Bacterial and Viral Co-Infections in COVID-19 Patients: Etiology and Clinical Impact
Abstract
1. Introduction
2. Materials and Methods
2.1. Population Survey and Sampling
2.2. Detection of Respiratory Co-Pathogens
2.2.1. Extraction
2.2.2. Detection of Bacterial Co-Pathogens
2.2.3. Detection of Viral Co-Pathogens
- (1)
- AdV, RSV, and PIV1;
- (2)
- BoV, RV, and PIV2;
- (3)
- HMPV and PIV3;
- (4)
- HCoV-229E and HCoV-HKU-1;
- (5)
- HCoV-NL63 and HCoV-OC43;
- (6)
- SARS-CoV-2 and influenza A and B viruses (FluSC2).
- Reverse transcription: 25 °C for 2 min and then 50 °C for 15 min;
- Initial denaturation: 95 °C for 2 min;
- Amplification for 45 cycles: 95 °C for 15 s and then 55 °C for 30 s.
2.3. Next-Generation Sequencing (NGS)
2.4. Definitions and Data
2.5. Statistical Analysis
3. Results
3.1. Population Characteristics
3.2. Detection of Co-Infections in COVID-19 Patients
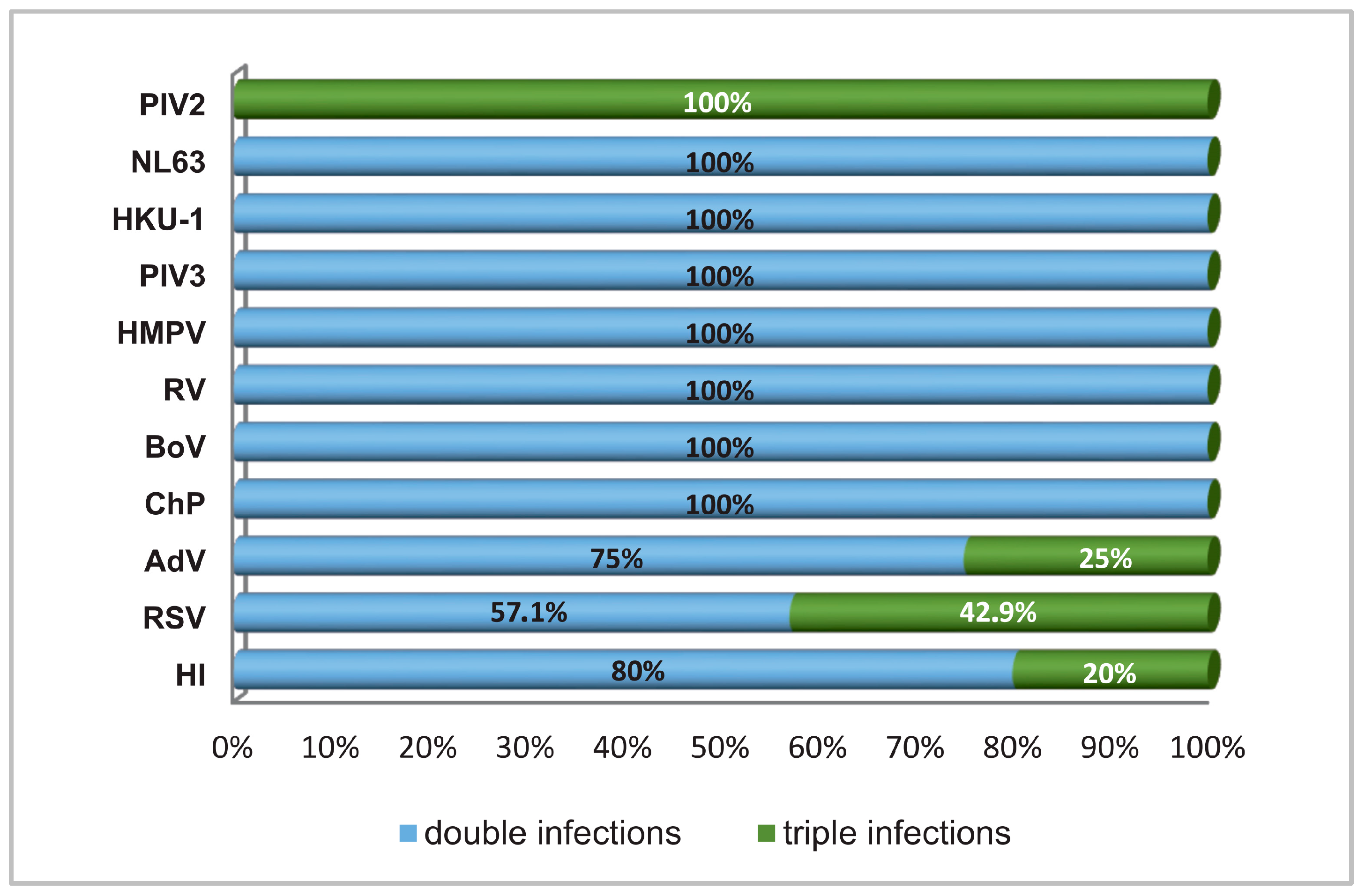
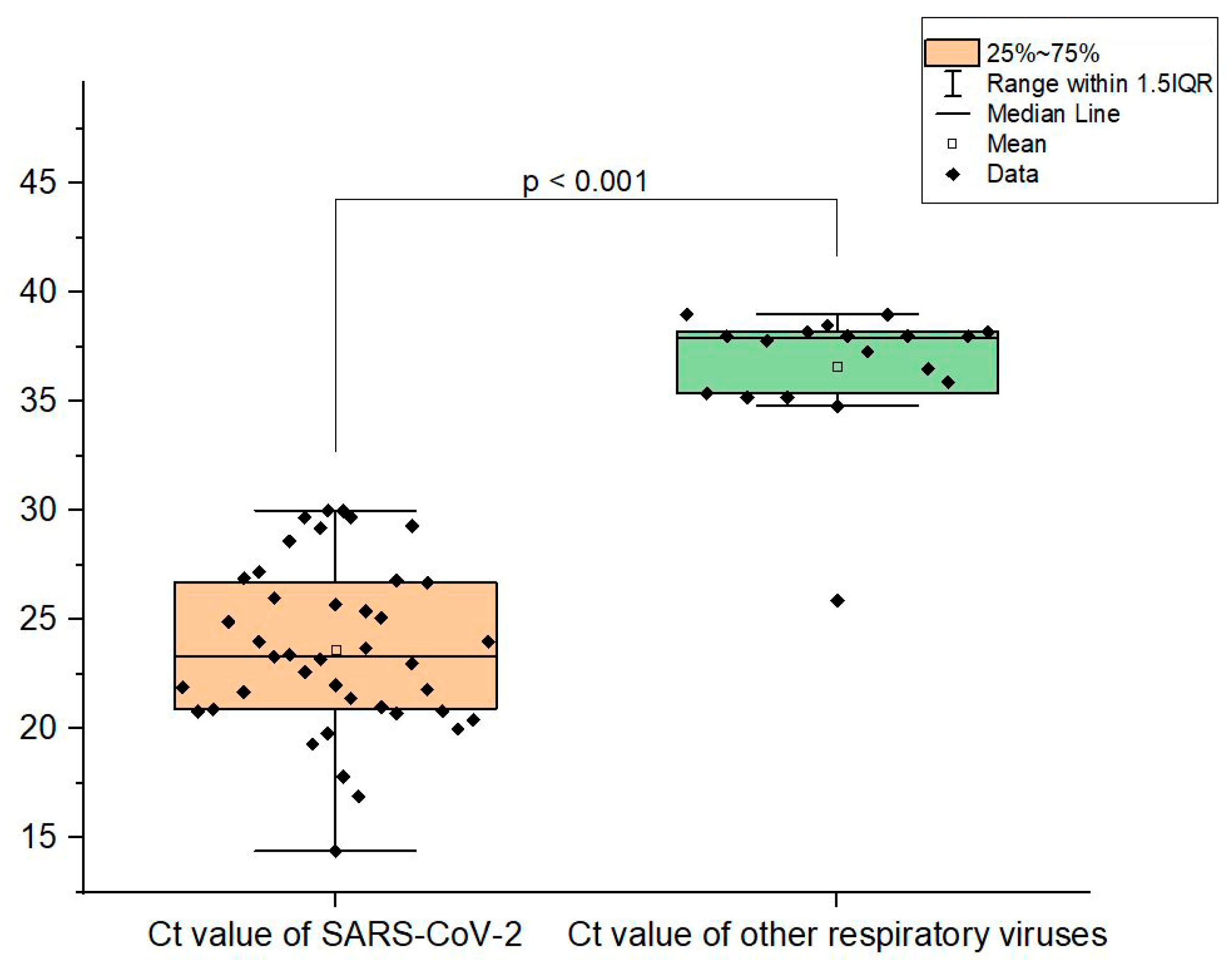
3.3. Viral Load of Respiratory Virus Co-Infections
3.4. Distribution of SARS-CoV-2 Variants in Individual Proven Co-Infections
3.5. Weekly and Seasonal Distribution of Confirmed Co-Infections
3.6. Clinical Data of the Investigated Patients
3.7. Age Characteristics of the Clinical Presentation of Respiratory Infection in Mono- and Co-Infected Patients
3.8. Vaccination Status
3.9. Determining the Clinical Severity of COVID-19 in Mono- and Co-Infections with Bacterial and Viral Co-Pathogens: Treatment
3.10. Treatment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Principi, N.; Autore, G.; Ramundo, G.; Esposito, S. Epidemiology of respiratory infections during the COVID-19 pandemic. Viruses 2023, 15, 1160. [Google Scholar] [CrossRef] [PubMed]
- Greene, S.K.; Levin-Rector, A.; Kyaw, N.T.; Luoma, E.; Amin, H.; McGibbon, E.; Mathes, R.W.; Ahuja, S.D. Comparative hospitalization risk for SARS-CoV-2 Omicron and Delta variant infections, by variant predominance periods and patient-level sequencing results, New York City, August 2021–January 2022. Influenza Other Respir. Viruses 2023, 17, e13062. [Google Scholar] [CrossRef] [PubMed]
- Olsen, S.J.; Azziz-Baumgartner, E.; Budd, A.P.; Brammer, L.; Sullivan, S.; Pineda, R.F.; Cohen, C.; Fry, A.M. Decreased influenza activity during the COVID-19 pandemic—United States, Australia, Chile, and South Africa. Am. J. Transplant. 2020, 20, 3681–3685. [Google Scholar] [CrossRef] [PubMed]
- Groves, H.E.; Papenburg, J.; Mehta, K.; Bettinger, J.A.; Sadarangani, M.; Halperin, S.A.; Morris, S.K.; Lefebvre, M.A. The effect of the COVID-19 pandemic on influenza-related hospitalization, intensive care admission and mortality in children in Canada: A population-based study. Lancet Reg. Health-Am. 2022, 7, 100132. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Wang, Y.; Shen, C.; Luo, J.; Yu, W. Decreased Incidence of Influenza During the COVID-19 Pandemic. Int. J. Gen. Med. 2022, 15, 2957. [Google Scholar] [CrossRef]
- Avolio, M.; Venturini, S.; De Rosa, R.; Crapis, M.; Basaglia, G. Epidemiology of respiratory virus before and during COVID-19 pandemic. Le Infez. Med. 2022, 30, 104. [Google Scholar]
- Mandelia, Y.; Procop, G.W.; Richter, S.S.; Worley, S.; Liu, W.; Esper, F. Dynamics and predisposition of respiratory viral co-infections in children and adults. Clin. Microbiol. Infect. 2021, 27, 631.e1–631.e6. [Google Scholar] [CrossRef]
- Peci, A.; Tran, V.; Guthrie, J.L.; Li, Y.; Nelson, P.; Schwartz, K.L.; Eshaghi, A.; Buchan, S.A.; Gubbay, J.B. Prevalence of co-infections with respiratory viruses in individuals investigated for SARS-CoV-2 in Ontario. Canada. Viruses 2021, 13, 130. [Google Scholar] [CrossRef]
- Lansbury, L.; Lim, B.; Baskaran, V.; Lim, W.S. Co-infections in people with COVID-19: A systematic review and meta-analysis. J. Infect. 2020, 81, 266–275. [Google Scholar] [CrossRef]
- Krumbein, H.; Kümmel, L.S.; Fragkou, P.C.; Thölken, C.; Hünerbein, B.L.; Reiter, R.; Papathanasiou, K.A.; Renz, H.; Skevaki, C. Respiratory viral co-infections in patients with COVID-19 and associated outcomes: A systematic review and meta-analysis. Rev. Med. Virol. 2023, 33, e2365. [Google Scholar] [CrossRef]
- Bengoechea, J.A.; Bamford, C.G. SARS-CoV-2. bacterial co-infections. and AMR: The deadly trio in COVID-19? EMBO Mol. Med. 2020, 12, e12560. [Google Scholar] [CrossRef] [PubMed]
- Hoque, M.N.; Chaudhury, A.; Akanda, M.A.M.; Hossain, M.A.; Islam, M.T. Genomic diversity and evolution. diagnosis. prevention. and therapeutics of the pandemic COVID-19 disease. PeerJ 2020, 8, e9689. [Google Scholar] [CrossRef] [PubMed]
- Langford, B.J.; So, M.; Raybardhan, S.; Leung, V.; Westwood, D.; MacFadden, D.R.; Soucy, J.-P.R.; Daneman, N. Bacterial co-infection and secondary infection in patients with COVID-19: A living rapid review and meta-analysis. Clin. Microbiol. Infect. 2020, 26, 1622–1629. [Google Scholar] [CrossRef] [PubMed]
- Khatiwada, S.; Subedi, A. Lung microbiome and coronavirus disease 2019 (COVID-19): Possible link and implications. Hum. Microbiome J. 2020, 17, 100073. [Google Scholar] [CrossRef] [PubMed]
- Peddu, V.; Shean, R.C.; Xie, H.; Shrestha, L.; Perchetti, G.A.; Minot, S.S.; Roychoudhury, P.; Huang, M.; Nalla, A.; Reddy, S.B.; et al. Metagenomic analysis reveals clinical SARS-CoV-2 infection and bacterial or viral superinfection and colonization. Clin. Chem. 2020, 66, 966–972. [Google Scholar] [CrossRef] [PubMed]
- Nishiura, H.; Kobayashi, T.; Miyama, T.; Suzuki, A.; Jung, S.M.; Hayashi, K.; Kinoshita, R.; Yang, Y.; Yuan, B.; Akhmetzhanov, A.R.; et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int. J. Infect. Dis. 2020, 94, 154–155. [Google Scholar] [CrossRef]
- Yi, C.; Sun, X.; Ye, J.; Ding, L.; Liu, M.; Yang, Z.; Lu, X.; Zhang, Y.; Ma, L.; Gu, W.; et al. Key residues of the receptor binding motif in the spike protein of SARS-CoV-2 that interact with ACE2 and neutralizing antibodies. Cell. Mol. Immunol. 2020, 17, 621–630. [Google Scholar] [CrossRef]
- Trifonova, I.; Christova, I.; Madzharova, I.; Angelova, S.; Voleva, S.; Yordanova, R.; Tcherveniakova, T.; Krumova, S.; Korsun, N. Clinical significance and role of coinfections with respiratory pathogens among individuals with confirmed severe acute respiratory syndrome coronavirus-2 infection. Front Public Health 2022, 10, 959319. [Google Scholar] [CrossRef]
- Bellinghausen, C.; Gulraiz, F.; Heinzmann, A.C.; Dentener, M.A.; Savelkoul, P.H.; Wouters, E.F.; Rohde, G.G.; Stassen, F.R. Exposure to common respiratory bacteria alters the airway epithelial response to subsequent viral infection. Respir. Res. 2016, 17, 68. [Google Scholar] [CrossRef]
- Lalbiaktluangi, C.; Yadav, M.K.; Singh, P.K.; Singh, A.; Iyer, M.; Vellingiri, B.; Zomuansangi, R.; Zothanpuia; Ram, H. A cooperativity between virus and bacteria during respiratory infections. Front. Microbiol. 2023, 14, 1279159. [Google Scholar] [CrossRef]
- Ghoneim, H.E.; Thomas, G.; and McCullers, J.A. Depletion of alveolar macrophages during influenza infection facilitates bacterial superinfections. J. Immunol. 2013, 191, 1250–1259. [Google Scholar] [CrossRef] [PubMed]
- Short, J.L.; Toffel, M.W.; Hugill, A.R. Monitoring global supply chains. Strateg. Manag. J. 2016, 37, 1878–1897. [Google Scholar] [CrossRef]
- Avadhanula, V.; Rodriguez, C.A.; DeVincenzo, J.P.; Wang, Y.; Webby, R.J.; Ulett, G.C.; Adderson, E.E. Respiratory viruses augment the adhesion of bacterial pathogens to respiratory epithelium in a viral species-and cell type-dependent manner. J. Virol. 2006, 80, 1629–1636. [Google Scholar] [CrossRef] [PubMed]
- Giannakis, A.; Móré, D.; Erdmann, S.; Kintzelé, L.; Fischer, R.M.; Vogel, M.N.; Mangold, D.L.; von Stackelberg, O.; Schnitzler, P.; Zimmermann, S.; et al. COVID-19 pneumonia and its lookalikes: How radiologists perform in differentiating atypical pneumonias. Eur. J. Radiol. 2021, 144, 110002. [Google Scholar] [CrossRef] [PubMed]
- Chibabhai, V.; Duse, A.G.; Perovic, O.; Richards, G.A. Collateral damage of the COVID-19 pandemic: Exacerbation of antimicrobial resistance and disruptions to antimicrobial stewardship programmes? SAMJ S. Afr. Med. J. 2020, 110, 1–2. [Google Scholar] [CrossRef]
- Feldman, C.; Anderson, R. The role of co-infections and secondary infections in patients with COVID-19. Pneumonia 2021, 13, 5. [Google Scholar] [CrossRef]
- Jayyosi, M.G.; Khuri-Bulos, N.A.; Halasa, N.B.; Faouri, S.; Shehabi, A.A. Rare occurrence of Bordetella pertussis among Jordanian children younger than two years old with respiratory tract infections. J. Pediatr. Infect. Dis. 2015, 10, 053–056. [Google Scholar] [CrossRef][Green Version]
- Kodani, M.; Yang, G.; Conklin, L.M.; Travis, T.C.; Whitney, C.G.; Anderson, L.J.; Schrag, S.J.; Taylor, T.H., Jr.; Beall, B.W.; Breiman, R.F.; et al. Application of TaqMan low-density arrays for simultaneous detection of multiple respiratory pathogens. J. Clin. Microbiol. 2011, 49, 2175–2182. [Google Scholar] [CrossRef]
- Dare, R.K.; Fry, A.M.; Chittaganpitch, M.; Sawanpanyalert, P.; Olsen, S.J.; Erdman, D.D. Human coronavirus infections in rural Thailand: A comprehensive study using real-time reverse-transcription polymerase chain reaction assays. J. Infect. Dis. 2007, 196, 1321–1328. [Google Scholar] [CrossRef]
- ARDS Definition Task Force; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, N.; Campobasso, C.P.; Cocozza, S.; Conti, V.; Davinelli, S.; Costantino, M.; Cannavo, A.; Rengo, G.; Filippelli, A.; Corbi, G. Relationship between COVID-19 mortality, hospital beds, and primary care by Italian regions: A lesson for the future. J. Clin. Med. 2022, 11, 4196. [Google Scholar] [CrossRef] [PubMed]
- Saeed, N.K.; Al-Khawaja, S.; Alsalman, J.; Almusawi, S.; Albalooshi, N.A.; Al-Biltagi, M. Bacterial co-infection in patients with SARS-CoV-2 in the Kingdom of Bahrain. World J. Virol. 2021, 10, 168. [Google Scholar] [CrossRef] [PubMed]
- Sahu, C.; Singh, S.; Pathak, A.; Singh, S.; Patel, S.S.; Ghoshal, U.; Garg, A. Bacterial coinfections in COVID: Prevalence. antibiotic sensitivity patterns and clinical outcomes from a tertiary institute of Northern India. J. Fam. Med. Prim. Care 2022, 11, 4473–4478. [Google Scholar] [CrossRef] [PubMed]
- Yan, X.; Li, K.; Lei, Z.; Luo, J.; Wang, Q.; Wei, S. Prevalence and associated outcomes of co-infection between SARS-CoV-2 and influenza: A systematic review and meta-analysis. Int. J. Infect. Dis. 2023, 136, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Fan, H.; Zhou, L.; Lv, J.; Yang, S.; Chen, G.; Liu, X.; Han, C.; Tan, X.; Qian, S.; Wu, Z.; et al. Bacterial coinfections contribute to severe COVID-19 in winter. Cell Res. 2023, 33, 562–564. [Google Scholar] [CrossRef]
- Alhumaid, S.; Al Mutair, A.; Al Alawi, Z.; Alshawi, A.M.; Alomran, S.A.; Almuhanna, M.S.; Almuslim, A.A.; Bu Shafia, A.H.; Alotaibi, A.M.; Ahmed, G.Y.; et al. Coinfections with bacteria. fungi. and respiratory viruses in patients with SARS-CoV-2: A systematic review and meta-analysis. Pathogens 2021, 10, 809. [Google Scholar] [CrossRef]
- Singh, V.; Upadhyay, P.; Reddy, J.; Granger, J. SARS-CoV-2 respiratory co-infections: Incidence of viral and bacterial co-pathogens. Int. J. Infect. Dis. 2021, 105, 617–620. [Google Scholar] [CrossRef]
- Contou, D.; Claudinon, A.; Pajot, O.; Micaëlo, M.; Longuet Flandre, P.; Dubert, M.; Cally, R.; Logre, E.; Fraissé, M.; Mentec, H. Bacterial and viral co-infections in patients with severe SARS-CoV-2 pneumonia admitted to a French ICU. Ann. Intensive Care 2020, 10, 119. [Google Scholar] [CrossRef]
- Borkakoty, B.; Bali, N.K. Haemophilus influenzae and SARS-CoV-2: Is there a role for investigation? Indian J. Med. Microbiol. 2021, 39, 240–244. [Google Scholar] [CrossRef]
- Davies-Bolorunduro, O.F.; Fowora, M.A.; Amoo, O.S.; Adeniji, E.; Osuolale, K.A.; Oladele, O.; Onuigbo, T.I.; Obi, J.C.; Oraegbu, J.; Ogundepo, O.; et al. Evaluation of respiratory tract bacterial co-infections in SARS-CoV-2 patients with mild or asymptomatic infection in Lagos. Nigeria. Bull. Natl. Res. Cent. 2022, 46, 115. [Google Scholar] [CrossRef]
- Swets, M.C.; Russell, C.D.; Harrison, E.M.; Docherty, A.B.; Lone, N.; Girvan, M.; Hardwick, H.E.; ISARIC4C Investigators; Visser, L.G.; Openshaw, P.J.M.; et al. SARS-CoV-2 co-infection with influenza viruses, respiratory syncytial virus. or adenoviruses. Lancet 2022, 399, 1463–1464. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Quinn, J.; Pinsky, B.; Shah, N.H.; Brown, I. Rates of co-infection between SARS-CoV-2 and other respiratory pathogens. JAMA 2020, 323, 2085–2086. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, P.P.; Dawson, P.; Wadhwa, A.; Rabold, E.M.; Buono, S.; Dietrich, E.A.; Reses, H.E.; Vuong, J.; Pawloski, L.; Dasu, T.; et al. Epidemiological correlates of polymerase chain reaction cycle threshold values in the detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Clin. Infect. Dis. 2021, 72, e761–e767. [Google Scholar] [CrossRef] [PubMed]
- Nowak, M.D.; Sordillo, E.M.; Gitman, M.R.; Mondolfi, A.E.P. Coinfection in SARS-CoV-2 infected patients: Where are influenza virus and rhinovirus/enterovirus? J. Med. Virol. 2020, 92, 1699. [Google Scholar] [CrossRef]
- Wade, S.F.; Diouara, A.A.M.; Ngom, B.; Thiam, F.; Dia, N. SARS-CoV-2 and Other Respiratory Viruses in Human Olfactory Pathophysiology. Microorganisms 2024, 12, 540. [Google Scholar] [CrossRef]
- Trifonova, I.; Korsun, N.; Madzharova, I.; Alexiev, I.; Ivanov, I.; Levterova, V.; Grigorova, L.; Stoikov, I.; Donchev, D.; Christova, I. Epidemiological and Genetic Characteristics of Respiratory Viral Coinfections with Different Variants of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Viruses 2024, 16, 958. [Google Scholar] [CrossRef]
- Babawale, P.I.; Guerrero-Plata, A. Respiratory Viral Coinfections: Insights into Epidemiology, Immune Response. Pathology. and Clinical Outcomes. Pathogens 2024, 13, 316. [Google Scholar] [CrossRef]
- AlBahrani, S.; AlZahrani, S.J.; Al-Maqati, T.N.; Almehbash, A.; Alshammari, A.; Bujlai, R.; Taweel, S.B.; Almasabi, F.; AlAmari, A.; Al-Tawfiq, J.A. Dynamic Patterns and Predominance of Respiratory Pathogens Post-COVID-19: Insights from a Two-Year Analysis. J. Epidemiol. Glob. Health 2024, 14, 311–318. [Google Scholar] [CrossRef]
- Pattemore, P.K.; Jennings, L.C. Chapter 31—Epidemiology of respiratory infections. In Pediatric Respiratory Medicine, 2nd ed.; Mosby: Maryland Heights, MO, USA, 2008; pp. 435–452. [Google Scholar] [CrossRef]
- Felsenstein, S.; Hedrich, C.M. SARS-CoV-2 infections in children and young people. Clin. Immunol. 2020, 220, 108588. [Google Scholar] [CrossRef]
- Li, Y.; Wang, H.; Wang, F.; Lu, X.; Du, H.; Xu, J.; Han, F.; Zhang, L.; Zhang, M. Co-infections of SARS-CoV-2 with multiple common respiratory pathogens in infected children: A retrospective study. Medicine 2021, 100, e24315. [Google Scholar] [CrossRef]
- Karaaslan, A.; Çetin, C.; Akın, Y.; Tekol, S.D.; Söbü, E.; Demirhan, R. Coinfection in SARS-CoV-2 infected children patients. J. Infect. Dev. Ctries. 2021, 15, 761–765. [Google Scholar] [CrossRef] [PubMed]
- Nieto-Rivera, B.; Saldaña-Ahuactzi, Z.; Parra-Ortega, I.; Flores-Alanis, A.; Carbajal-Franco, E.; Cruz-Rangel, A.; Galaviz-Hernández, S.; Romero-Navarro, B.; de la Rosa-Zamboni, D.; Salazar-García, M.; et al. Frequency of respiratory virus-associated infection among children and adolescents from a tertiary-care hospital in Mexico City. Sci. Rep. 2023, 13, 19763. [Google Scholar] [CrossRef] [PubMed]
- El-Koofy, N.M.; El-Shabrawi, M.H.; Abd El-alim, B.A.; Zein, M.M.; Badawi, N.E. Patterns of respiratory tract infections in children under 5 years of age in a low–middle-income country. J. Egypt. Public Health Assoc. 2022, 97, 22. [Google Scholar] [CrossRef] [PubMed]
- Solito, C.; Hernández-García, M.; Casamayor, N.A.; Ortiz, A.P.; Pino, R.; Alsina, L.; de Sevilla, M.F. COVID-19 admissions: Trying to define the real impact of infection in hospitalized patients. An. Pediatría 2024, 100, 342–351. [Google Scholar] [CrossRef]
- Kuchar, E.; Załęski, A.; Wronowski, M.; Krankowska, D.; Podsiadły, E.; Brodaczewska, K.; Lewicka, A.; Lewicki, S.; Kieda, C.; Horban, A.; et al. Children were less frequently infected with SARS-CoV-2 than adults during 2020 COVID-19 pandemic in Warsaw, Poland. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 541–547. [Google Scholar] [CrossRef]
- Latouche, M.; Ouafi, M.; Engelmann, I.; Becquart, A.; Alidjinou, E.K.; Mitha, A.; Dubos, F. Frequency and burden of disease for SARS-CoV-2 and other viral respiratory tract infections in children under the age of 2 months. Pediatr. Pulmonol. 2024, 59, 101–110. [Google Scholar] [CrossRef]
- Luan, Y.Y.; Yin, C.H.; Yao, Y.M. Update advances on C-reactive protein in COVID-19 and other viral infections. Front. Immunol. 2021, 12, 720363. [Google Scholar] [CrossRef]
- Ali, N. Elevated level of C-reactive protein may be an early marker to predict risk for severity of COVID-19. J. Med. Virol. 2020, 92, 2409. [Google Scholar] [CrossRef]
- Taylor, C.A. COVID-19–Associated Hospitalizations among US Adults Aged ≥ 65 Years—COVID-NET. 13 States, January–August 2023. MMWR. Morb. Mortal. Wkly. Rep. 2023, 72, 1089–1094. [Google Scholar] [CrossRef]
- Inaida, S.; Paul, R.E.; Matsuno, S. Viral transmissibility of SARS-CoV-2 accelerates in the winter. similarly to influenza epidemics. Am. J. Infect. Control 2022, 50, 1070–1076. [Google Scholar] [CrossRef]
- Rezaei-Tavabe, N.; Kheiri, S.; Mousavi, M.S.; Mohammadian-Hafshejani, A. The Effect of Monovalent Influenza Vaccine on the Risk of Hospitalization and All-Cause Mortality According to the Results of Randomized Clinical Trials: A Systematic Review and Meta-Analysis. Iran. J. Public Health 2023, 52, 924. [Google Scholar] [PubMed]
- Thompson, M.G.; Stenehjem, E.; Grannis, S.; Ball, S.W.; Naleway, A.L.; Ong, T.C.; DeSilva, M.B.; Natarajan, N.; Bozio, C.H.; Lewis, N.; et al. Effectiveness of COVID-19 vaccines in ambulatory and inpatient care settings. N. Engl. J. Med. 2021, 385, 1355–1371. [Google Scholar] [CrossRef] [PubMed]
- Franco-Paredes, C. Transmissibility of SARS-CoV-2 among fully vaccinated individuals. Lancet. Infect. Dis. 2022, 22, 16. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi-Haddad-Zavareh, M.; Bayani, M.; Shokri, M.; Ebrahimpour, S.; Babazadeh, A.; Mehraeen, R.; Moudi, E.; Rostami, A.; Barary, M.; Hosseini, A.; et al. C-reactive protein as a prognostic indicator in COVID-19 patients. Interdiscip. Perspect. Infect. Dis. 2021, 2021, 5557582. [Google Scholar] [CrossRef]
- Mphekgwana, P.M.; Sono-Setati, M.E.; Maluleke, A.F.; Matlala, S.F. Low Oxygen Saturation of COVID-19 in Patient Case Fatalities. Limpopo Province. South Africa. J. Respir. 2022, 2, 77–86. [Google Scholar] [CrossRef]
- Wu, H.; Zhou, H.Y.; Zheng, H.; Wu, A. Towards Understanding and Identification of Human Viral Co-Infections. Viruses 2024, 16, 673. [Google Scholar] [CrossRef]
- Stefanidis, K.; Konstantelou, E.; Yusuf, G.T.; Oikonomou, A.; Tavernaraki, K.; Karakitsos, D.; Loukides, S.; Vlahos, I. Radiological. epidemiological and clinical patterns of pulmonary viral infections. Eur. J. Radiol. 2021, 136, 109548. [Google Scholar] [CrossRef]



| Co-Infection | n | % |
|---|---|---|
| SARS-CoV-2 + HI | 20 | 47.62% |
| SARS-CoV-2 + RSV | 4 | 9.52% |
| SARS-CoV-2 + ChP | 3 | 7.14% |
| SARS-CoV-2 + AdV | 3 | 7.14% |
| SARS-CoV-2 + HI + RSV | 3 | 7.14% |
| SARS-CoV-2 + BoV | 2 | 4.76% |
| SARS-CoV-2 + RV | 1 | 2.38% |
| SARS-CoV-2 + HMPV | 1 | 2.38% |
| SARS-CoV-2 + PIV3 | 1 | 2.38% |
| SARS-CoV-2 + HKU-1 | 1 | 2.38% |
| SARS-CoV-2 + NL63 | 1 | 2.38% |
| SARS-CoV-2 + HI + AdV | 1 | 2.38% |
| SARS-CoV-2 + HI + PIV2 | 1 | 2.38% |
| SARS-CoV-2 + MP | 0 | 0% |
| SARS-CoV-2 + PIV1 | 0 | 0% |
| SARS-CoV-2 + PIV2 | 0 | 0% |
| SARS-CoV-2 + 229E | 0 | 0% |
| SARS-CoV-2 + OC43 | 0 | 0% |
| SARS-CoV-2 + Influenza A | 0 | 0% |
| SARS-CoV-2 + Influenza B | 0 | 0% |
| Delta | ||
|---|---|---|
| Tested: 119 | ||
| Co-infections: 2 | ||
| Positive rate: 1.7% | ||
| AY.75.1 | + BoV | n = 1 |
| AY.4.4 | + RSV | n = 1 |
| Omicron | ||
| Tested: 186 | ||
| Co-infections: 32 (29 + 3 triple) | ||
| Positive rate: 17.2% | ||
| BA.1 | + AdV | n = 1 |
| + RSV | n = 1 | |
| BA.1.1 | + HI | n = 2 |
| BA.2 | + HI | n = 13 |
| + HI + RSV | n = 1 | |
| + HI +PIV2 | n = 1 | |
| + HI + AdV | n = 1 | |
| + ChP | n = 2 | |
| + RSV | n = 1 | |
| + BoV | n = 1 | |
| + PIV3 | n = 1 | |
| + NL63 | n = 1 | |
| + AdV | n = 2 | |
| BA.2.12 | + RV | n = 1 |
| BA.2.9 | + HI | n = 2 |
| + ChP | n = 1 | |
| Age Group (Years Old) | 0–5 | 6–16 | 17–64 | >65 |
|---|---|---|---|---|
| Co-infected * (n) | 5 | 2 | 7 | 17 |
| Symptom | ||||
| Fever, n (%) | 4 (80) | 1 (50) | 7 (100) | 13 (76.5) |
| Fatigue, n (%) | 4 (80) | 2 (100) | 7 (100) | 11 (64.7) |
| Cough, n (%) | 2 (40) | 0 (0) | 7 (100) | 14 (82.4) |
| Diarrhea, n (%) | 1 (20) | 1 (50) | 2 (28.6) | 0 (0) |
| Headache, n (%) | 0 (0) | 0 (0) | 0 (0) | 3 (17.6) |
| Rhinitis, n (%) | 3 (60) | 1 (50) | 2 (28.6) | 4 (23.5) |
| Pneumonia, n (%) | 2 (40) | 2 (100) | 5 (71.4) | 15 (88.2) |
| Laboratory results | ||||
| Oxygen saturation, mean % | 93.2 | 90.5 | 91.7 | 89.5 |
| Lym **,mean × 109/L | 2.73 | 2.1 | 2.1 | 2.3 |
| WBC **, mean × 109/L | 5.1 | 9.7 | 4.9 | 5.4 |
| CRP **, mean mg/L | 16.2 | 56 | 42.9 | 78.1 |
| Hospital stay, mean/SD ** (days) | 3.1/2.2 | 6/5.6 | 5.2/2.3 | 8.1/3.7 |
| Hospital stay, median (days) | 3 | 6 | 6 | 9 |
| Clinical outcome | ||||
| ICU ** stay, n (%) | 1 (20) | 0 (0) | 1 (14.3) | 1 (20) |
| Fatal outcome, n (%) | 0 | 0 | 1 (14.3) | 2 (11.8) |
| SARS-CoV-2 Mono-Infection | Viral SARS-CoV-2 Co-Infection | Bacterial SARS-CoV-2 Co-Infection | SARS-CoV-2 Triple Infection | p-Value: Viral vs. Bacterial Co-Infection | p-Value: Co- vs. Triple Infection | p-Value: Mono- vs. Co-Infection | p-Value: Mono- vs. Triple Infection | |
|---|---|---|---|---|---|---|---|---|
| Distribution, n (%) | 295 (87.5) | 14 (4.2) | 23 (6.8) | 5 (1.5) | – | – | – | – |
| With clinical data, n | 141 | 9 | 19 | 5 | – | – | – | – |
| Symptoms, n (%) | ||||||||
| Fever | 110 (78) | 8 (88.9) | 15 (78.9) | 4 (80) | 1 | 1 | 0.8138 | 1 |
| Fatigue | 111 (78.8) | 7 (77.8) | 14 (73.7) | 4 (80) | 1 | 1 | 0.8151 | 1 |
| Cough | 107 (75.9) | 7 (77.8) | 14 (73.7) | 3 (60) | 1 | 0.5971 | 0.8228 | 0.5971 |
| Diarrhea | 22 (15.6) | 1 (11.7) | 2 (10.5) | 2 (40) | 1 | 0.1546 | 1 | 0.1895 |
| Headache | 39 (27.7) | 4 (44.4) | 1 (5.3) | – | 0.0256 | 0.5686 | 0.1825 | 0.3247 |
| Rhinitis | 50 (35.5) | 3 (33.3) | 4 (21.1) | 2 (40) | 0.6465 | 0.5971 | 0.4198 | 1 |
| Pneumonia | 83 (58.9) | 6 (66.7) | 12 (63.2) | 3 (60) | 1 | 1 | 0.6955 | 1 |
| Laboratory results, mean | ||||||||
| Oxygen saturation (%) | 91.8 | 93.4 | 90.4 | 87.8 | n.s * | n.s | n.s | n.s |
| Lym **, (×109/L) | 1.76 | 0.88 | 3.1 | 1.5 | n.s | n.s | n.s | n.s |
| WBC **, (×109/L) | 6.9 | 5.4 | 5.4 | 8.7 | n.s | 0.02 | n.s | n.s |
| CRP **, (mg/L) | 65.5 | 86.7 | 48.3 | 109.6 | n.s | n.s | n.s | n.s |
| Treatment, n (%) | ||||||||
| Antibiotics | 96 (68.1) | 7 (77.8) | 12 (63.2) | 4 (80) | 0.67 | 1 | 1 | 1 |
| Antiviral drugs | 14 (9.9) | – | 1 (5.3) | – | 1 | 1 | 0.3086 | 1 |
| Corticosteroids | 44 (31.2) | 3 (33.3) | 9 (47.4) | 3 (60) | 0.687 | 0.639 | 0.1525 | 0.3283 |
| Vasodilators | 10 (7.1) | – | 1 (5.3) | – | 1 | 1 | 0.6925 | 1 |
| Heparin | 73 (51.8) | 6 (66.7) | 11 (57.9) | 2 (40) | 1 | 0.6285 | 0.5658 | 0.3595 |
| Oxygen therapy | 60 (42.6) | 3 (33.3) | 10 (52.3) | 4 (80) | 0.4348 | 0.3353 | 0.4367 | 0.1687 |
| Clinical outcome | ||||||||
| Hospital stay, mean/SD ** (days) | 6.1/4.2 | 7.8/3.4 | 5.3/3.3 | 6.3/2.4 | n.s | n.s | n.s | n.s |
| Hospital stay, median (days) | 5 | 8 | 4 | 7 | ||||
| ICU ** stay, n (%) | 1 (0.7) | – | 1 (5.3) | 2 (40) | 1 | 0.0501 | 0.3129 | 0.0028 |
| Fatal outcome, n (%) | 14 (9.9) | – | 2 (10.5) | 1 (20) | 1 | 0.3996 | 1 | 0.4493 |
| Factor | Coefficients | Lower 95% CI | Upper 95% CI | Std. Error | z | p | Exp(B) | Lower 95% CI | Upper 95% CI |
|---|---|---|---|---|---|---|---|---|---|
| Co-infection with two viruses | 2.5 | 0.09 | 4.9 | 1.23 | 2.04 | 0.042 | 12.14 | 1.1 | 134.26 |
| Co-infection with three viruses | 4.55 | 1.51 | 7.58 | 1.55 | 2.94 | 0.003 | 94.5 | 4.54 | 1967.29 |
| Days from the onset of symptoms before hospitalization | 0.25 | -0.08 | 0.58 | 0.17 | 1.51 | 0.131 | 1.29 | 0.93 | 1.79 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trifonova, I.; Madzharova, I.; Korsun, N.; Levterova, V.; Velikov, P.; Voleva, S.; Ivanov, I.; Ivanov, D.; Yordanova, R.; Tcherveniakova, T.; et al. Bacterial and Viral Co-Infections in COVID-19 Patients: Etiology and Clinical Impact. Biomedicines 2024, 12, 2210. https://doi.org/10.3390/biomedicines12102210
Trifonova I, Madzharova I, Korsun N, Levterova V, Velikov P, Voleva S, Ivanov I, Ivanov D, Yordanova R, Tcherveniakova T, et al. Bacterial and Viral Co-Infections in COVID-19 Patients: Etiology and Clinical Impact. Biomedicines. 2024; 12(10):2210. https://doi.org/10.3390/biomedicines12102210
Chicago/Turabian StyleTrifonova, Ivelina, Iveta Madzharova, Neli Korsun, Viktoria Levterova, Petar Velikov, Silvya Voleva, Ivan Ivanov, Daniel Ivanov, Ralitsa Yordanova, Tatiana Tcherveniakova, and et al. 2024. "Bacterial and Viral Co-Infections in COVID-19 Patients: Etiology and Clinical Impact" Biomedicines 12, no. 10: 2210. https://doi.org/10.3390/biomedicines12102210
APA StyleTrifonova, I., Madzharova, I., Korsun, N., Levterova, V., Velikov, P., Voleva, S., Ivanov, I., Ivanov, D., Yordanova, R., Tcherveniakova, T., Angelova, S., & Christova, I. (2024). Bacterial and Viral Co-Infections in COVID-19 Patients: Etiology and Clinical Impact. Biomedicines, 12(10), 2210. https://doi.org/10.3390/biomedicines12102210





