The Safe Values of Quantitative Perfusion Parameters of ICG Angiography Based on Tissue Oxygenation of Hyperspectral Imaging for Laparoscopic Colorectal Surgery: A Prospective Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. ICG Angiography
2.3. Hyperspectral Imaging (HSI)
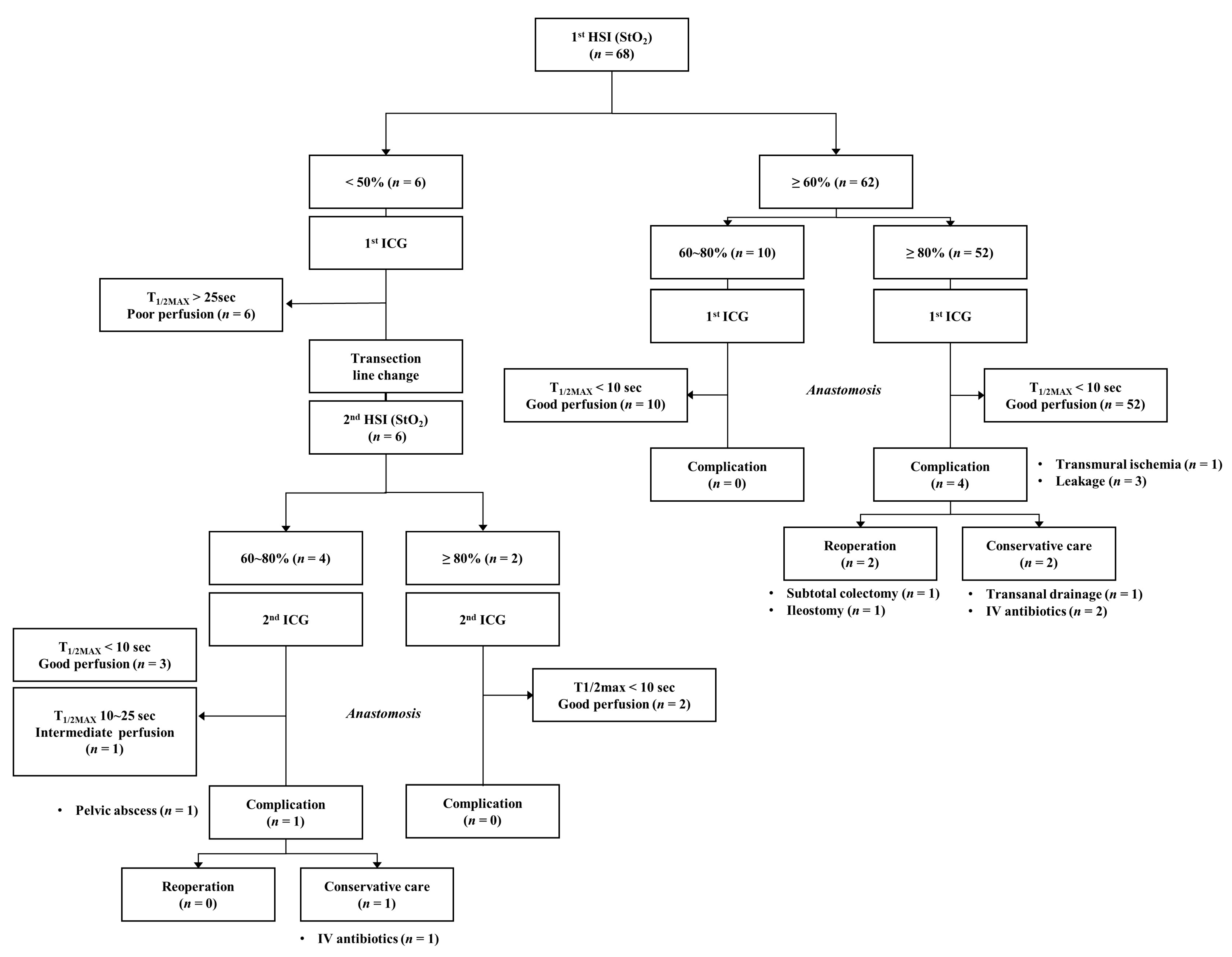
2.4. Colonic Perfusion Assessment Protocol
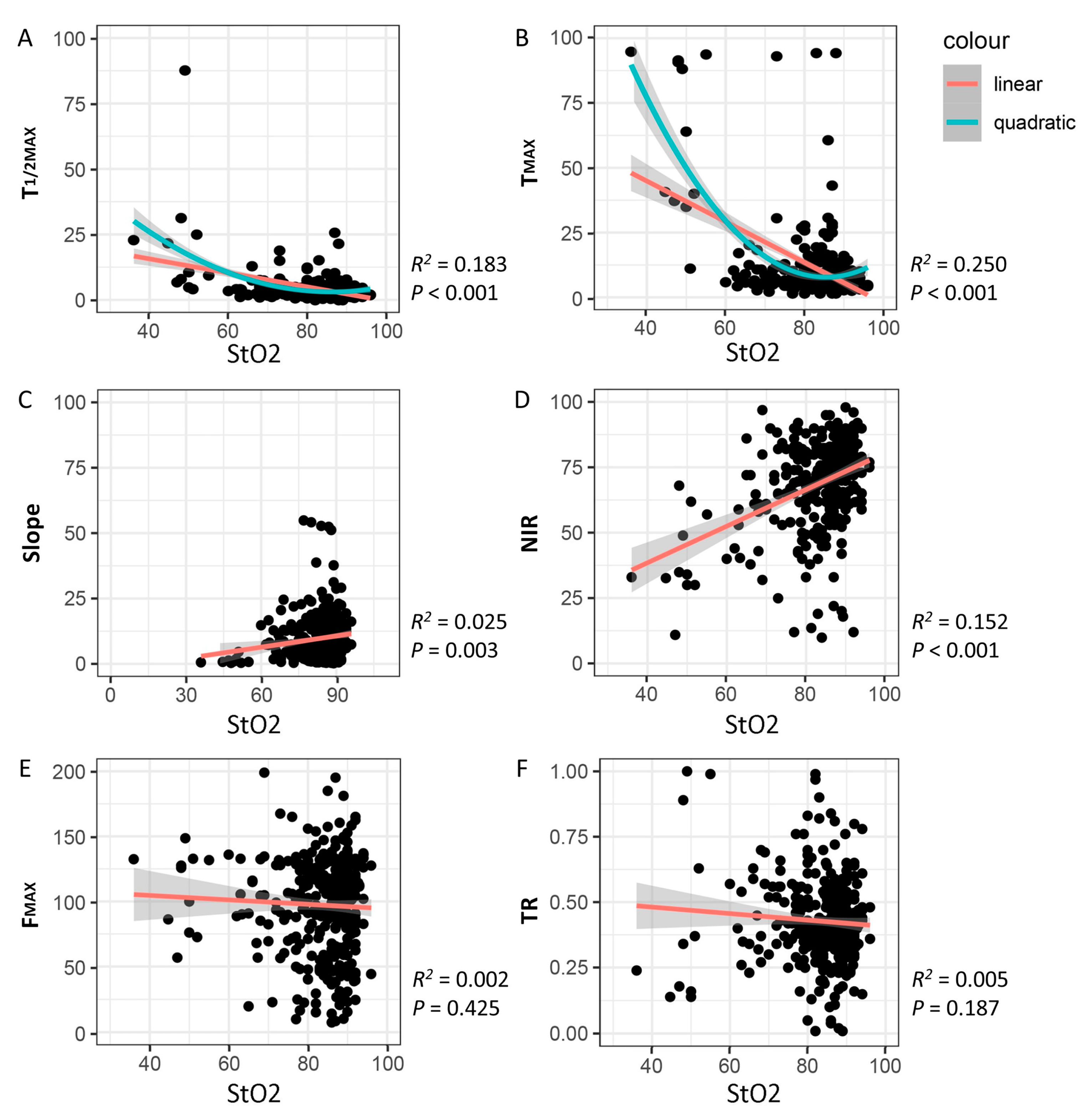
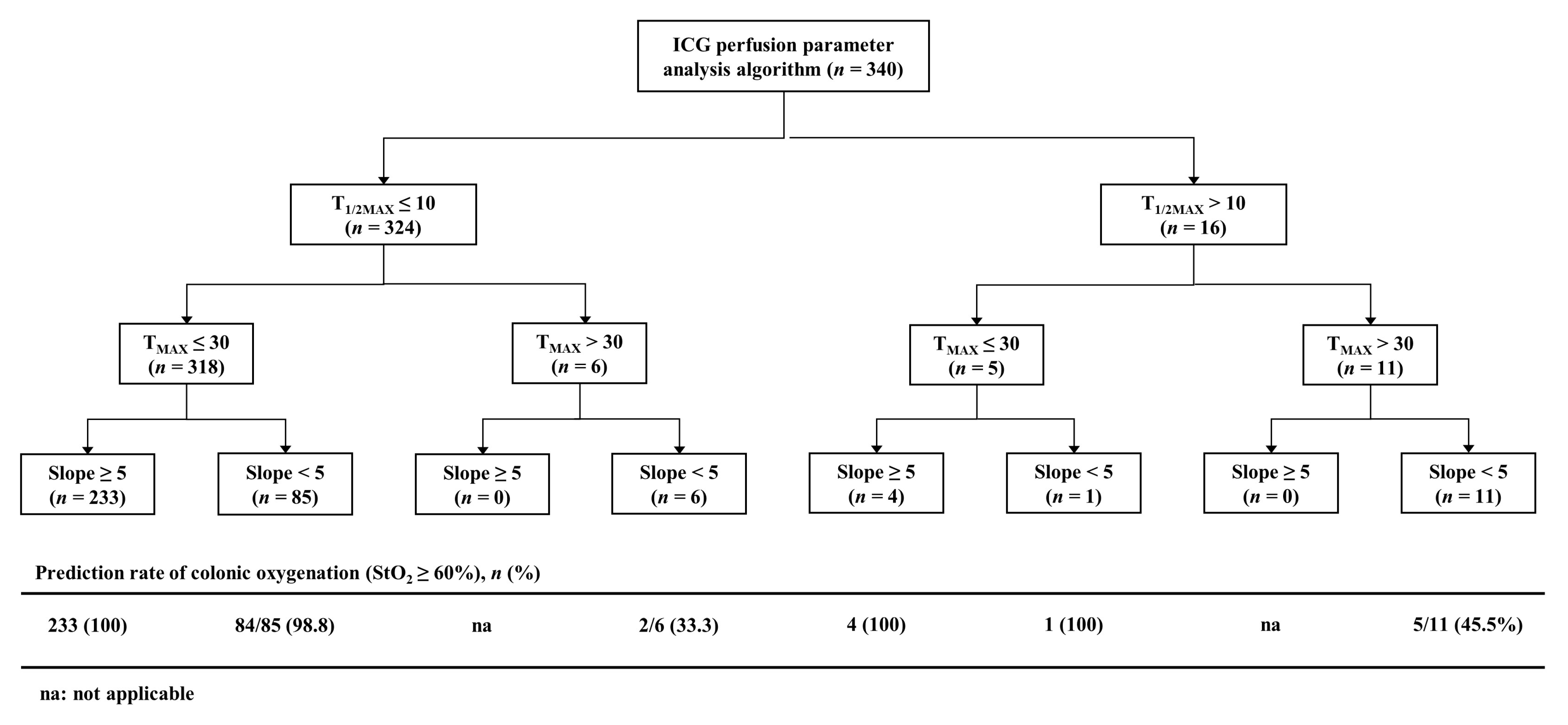
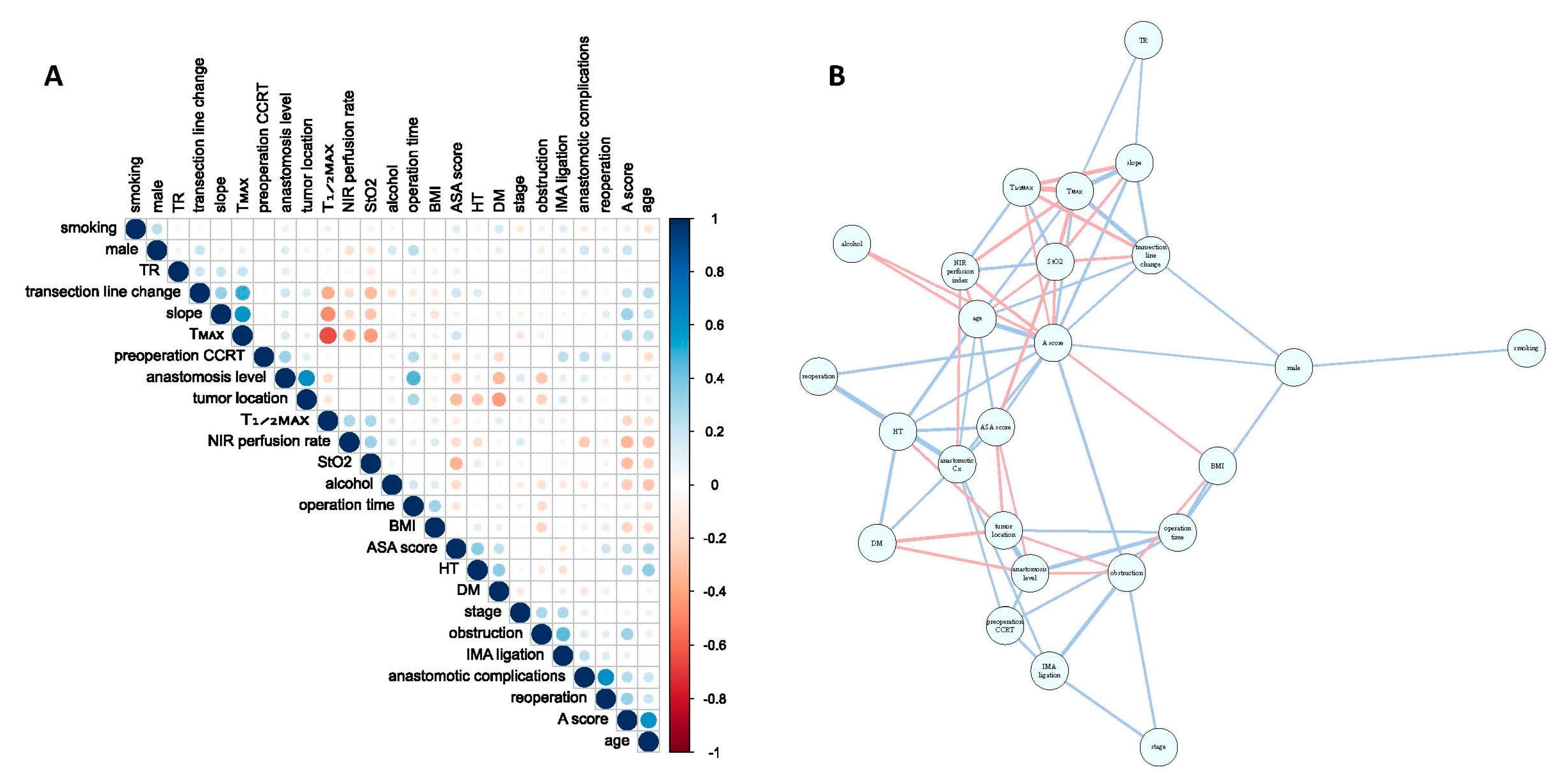
2.5. Comparison of StO2 Levels and Quantitative Perfusion Parameters
2.6. Anastomotic Complications
2.7. Statistical Analysis
3. Results
4. Discussion
4.1. Study Limitations
4.2. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Son, G.M.; Kwon, M.S.; Kim, Y.; Kim, J.; Kim, S.H.; Lee, J.W. Quantitative analysis of colon perfusion pattern using indocyanine green (ICG) angiography in laparoscopic colorectal surgery. Surg. Endosc. 2019, 33, 1640–1649. [Google Scholar] [CrossRef]
- Son, G.M.; Kim, T.U.; Park, B.S.; Jung, H.J.; Lee, S.S.; Yoon, J.U.; Lee, J.W. Colonic hypoperfusion following ligation of the inferior mesenteric artery in rectosigmoid colon cancer patients. Ann. Surg. Treat. Res. 2019, 97, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Son, G.M.; Ahn, H.M.; Lee, I.Y.; Ha, G.W. Multifunctional Indocyanine Green Applications for Fluorescence-Guided Laparoscopic Colorectal Surgery. Ann. Coloproctol. 2021, 37, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Son, G.M.; Ahn, H.M.; Lee, I.Y.; Lee, S.M.; Park, S.H.; Baek, K.R. Clinical effect and standardization of indocyanine green angiography in the laparoscopic colorectal surgery. J. Minim. Invasive Surg. 2021, 24, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Ahn, H.M.; Son, G.M.; Lee, I.Y.; Park, S.H.; Kim, N.S.; Baek, K.R. Optimization of indocyanine green angiography for colon perfusion during laparoscopic colorectal surgery. Color. Dis. 2021, 23, 1848–1859. [Google Scholar] [CrossRef] [PubMed]
- Jansen-Winkeln, B.; Germann, I.; Köhler, H.; Mehdorn, M.; Maktabi, M.; Sucher, R.; Barberio, M.; Chalopin, C.; Diana, M.; Moulla, Y.; et al. Comparison of hyperspectral imaging and fluorescence angiography for the determination of the transection margin in colorectal resections-a comparative study. Int. J. Color. Dis. 2021, 36, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Pfahl, A.; Radmacher, G.K.; Köhler, H.; Maktabi, M.; Neumuth, T.; Melzer, A.; Gockel, I.; Chalopin, C.; Jansen-Winkeln, B. Combined indocyanine green and quantitative perfusion assessment with hyperspectral imaging during colorectal resections. Biomed. Opt. Express 2022, 13, 3145–3160. [Google Scholar] [CrossRef]
- Sherwinter, D.; Chandler, P.; Martz, J. The use of tissue oxygen measurements compared to indocyanine green imaging for the assessment of intraoperative tissue viability of human bowel. Surg. Endosc. 2022, 36, 2192–2196. [Google Scholar] [CrossRef]
- Hennig, S.; Jansen-Winkeln, B.; Köhler, H.; Knospe, L.; Chalopin, C.; Maktabi, M.; Pfahl, A.; Hoffmann, J.; Kwast, S.; Gockel, I.; et al. Novel Intraoperative Imaging of Gastric Tube Perfusion during Oncologic Esophagectomy—A Pilot Study Comparing Hyperspectral Imaging (HSI) and Fluorescence Imaging (FI) with Indocyanine Green (ICG). Cancers 2021, 14, 97. [Google Scholar] [CrossRef]
- Soares, A.S.; Bano, S.; Clancy, N.T.; Stoyanov, D.; Lovat, L.B.; Chand, M. Multisensor perfusion assessment cohort study: Preliminary evidence toward a standardized assessment of indocyanine green fluorescence in colorectal surgery. Surgery 2022, 172, 69–73. [Google Scholar] [CrossRef]
- Park, S.H.; Park, H.M.; Baek, K.R.; Ahn, H.M.; Lee, I.Y.; Son, G.M. Artificial intelligence based real-time microcirculation analysis system for laparoscopic colorectal surgery. World J. Gastroenterol. 2020, 26, 6945–6962. [Google Scholar] [CrossRef] [PubMed]
- Khosrawipour, T.; Li, S.; Steward, E.; Chaudhry, H.; Nguyen, D.; Khosrawipour, V.; Jafari, M.D.; Pigazzi, A. Assessment of Anastomotic Viability with Spectroscopic Real-time Oxygen Saturation Measurement in a Porcine Study. Surg. Innov. 2022, 30, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Thomaßen, M.T.; Köhler, H.; Pfahl, A.; Stelzner, S.; Mehdorn, M.; Thieme, R.; Jansen-Winkeln, B.; Gockel, I.; Chalopin, C.; Moulla, Y. In vivo evaluation of a hyperspectral imaging system for minimally invasive surgery (HSI-MIS). Surg. Endosc. 2023, 37, 3691–3700. [Google Scholar] [CrossRef] [PubMed]
- Wada, T.; Kawada, K.; Takahashi, R.; Yoshitomi, M.; Hida, K.; Hasegawa, S.; Sakai, Y. ICG fluorescence imaging for quantitative evaluation of colonic perfusion in laparoscopic colorectal surgery. Surg. Endosc. 2017, 31, 4184–4193. [Google Scholar] [CrossRef]
- Wada, T.; Kawada, K.; Hoshino, N.; Inamoto, S.; Yoshitomi, M.; Hida, K.; Sakai, Y. The effects of intraoperative ICG fluorescence angiography in laparoscopic low anterior resection: A propensity score-matched study. Int. J. Clin. Oncol. 2019, 24, 394–402. [Google Scholar] [CrossRef]
- Gonzalez-Jacobo, A.; Chandler, P.; Martz, J.; Sherwinter, D. Tissue Oximetry as a Potential Alternative to Indocyanine Green (ICG) Perfusion Assessment in Colorectal Anastomotic Cases. Surg. Laparosc. Endosc. Percutaneous Tech. 2023, 33, 207–210. [Google Scholar] [CrossRef]
- Gräfitsch, A.; Kirchhoff, P.; Soysal, S.D.; Däster, S.; Hoffmann, H. Dynamic Serosal Perfusion Assessment during Colorectal Resection Using Visible Light Spectroscopy. Eur. Surg. Res. 2021, 62, 25–31. [Google Scholar] [CrossRef]
- Tavy, A.L.; de Bruin, A.F.; Boerma, E.C.; Ince, C.; Hilty, M.P.; Noordzij, P.G.; Boerma, D.; van Iterson, M. Association between serosal intestinal microcirculation and blood pressure during major abdominal surgery. J. Intensive Med. 2021, 1, 59–64. [Google Scholar] [CrossRef]
- Seeliger, B.; Agnus, V.; Mascagni, P.; Barberio, M.; Longo, F.; Lapergola, A.; Mutter, D.; Klymchenko, A.S.; Chand, M.; Marescaux, J.; et al. Simultaneous computer-assisted assessment of mucosal and serosal perfusion in a model of segmental colonic ischemia. Surg. Endosc. 2020, 34, 4818–4827. [Google Scholar] [CrossRef]
- Barberio, M.; Felli, E.; Pizzicannella, M.; Agnus, V.; Al-Taher, M.; Seyller, E.; Moulla, Y.; Jansen-Winkeln, B.; Gockel, I.; Marescaux, J.; et al. Quantitative serosal and mucosal optical imaging perfusion assessment in gastric conduits for esophageal surgery: An experimental study in enhanced reality. Surg. Endosc. 2021, 35, 5827–5835. [Google Scholar] [CrossRef]
- Gomez-Rosado, J.C.; Valdes-Hernandez, J.; Cintas-Catena, J.; Cano-Matias, A.; Perez-Sanchez, A.; Del Rio-Lafuente, F.J.; Torres-Arcos, C.; Lara-Fernandez, Y.; Capitan-Morales, L.C.; Oliva-Mompean, F. Feasibility of quantitative analysis of colonic perfusion using indocyanine green to prevent anastomotic leak in colorectal surgery. Surg. Endosc. 2022, 36, 1688–1695. [Google Scholar] [CrossRef] [PubMed]
- Garoufalia, Z.; Wexner, S.D. Indocyanine Green Fluorescence Guided Surgery in Colorectal Surgery. J. Clin. Med. 2023, 12, 494. [Google Scholar] [CrossRef] [PubMed]
- Flores-Rodríguez, E.; Garrido-López, L.; Sánchez-Santos, R.; Cano-Valderrama, O.; Rodríguez-Fernández, L.; Nogueira-Sixto, M.; Paniagua-García Señorans, M.; Vigorita, V.; Moncada-Iribarren, E. Is ICG essential in all colorectal surgery? A 3-year experience in a single center: A cohort study. Int. J. Color. Dis. 2023, 38, 67. [Google Scholar] [CrossRef] [PubMed]
- Kondo, A.; Kumamoto, K.; Asano, E.; Feng, D.; Kobara, H.; Okano, K. Indocyanine green fluorescence imaging during laparoscopic rectal cancer surgery could reduce the incidence of anastomotic leakage: A single institutional retrospective cohort study. World J. Surg. Oncol. 2022, 20, 397. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.B.; Stansby, G.; Bain, I.; Harrison, D.K. Intraoperative measurement of colonic oxygenation during bowel resection. Adv. Exp. Med. Biol. 2009, 645, 261–266. [Google Scholar]
- Lee, E.S.; Bass, A.; Arko, F.R.; Heikkinen, M.; Harris, E.J.; Zarins, C.K.; van der Starre, P.; Olcott, C. Intraoperative colon mucosal oxygen saturation during aortic surgery. J. Surg. Res. 2006, 136, 19–24. [Google Scholar] [CrossRef]
- Köhler, H.; Pfahl, A.; Moulla, Y.; Thomaßen, M.T.; Maktabi, M.; Gockel, I.; Neumuth, T.; Melzer, A.; Chalopin, C. Comparison of image registration methods for combining laparoscopic video and spectral image data. Sci. Rep. 2022, 12, 16459. [Google Scholar] [CrossRef]
- Kim, J.C.; Lee, J.L.; Kim, C.W.; Kim, H.M.; Park, I.J.; Yoon, Y.S. Interpretation and clinical utility of indocyanine-green fluorescence imaging (IFI) in robot-assisted anorectal-function saving operations (ASOs): A propensity-score matched analysis of 872 prospectively enroled patients undergoing IFI. Int. J. Med. Robot. 2023, 19, e2515. [Google Scholar] [CrossRef]
- Kitaguchi, D.; Ito, M. Optimal anastomotic technique in rectal surgery to prevent anastomotic leakage. Ann. Coloproctol. 2023, 39, 97–105. [Google Scholar] [CrossRef]
- Alekseev, M.; Rybakov, E.; Khomyakov, E.; Zarodnyuk, I.; Shelygin, Y. Intraoperative fluorescence angiography as an independent factor of anastomotic leakage and a nomogram for predicting leak for colorectal anastomoses. Ann. Coloproctol. 2022, 38, 380–386. [Google Scholar] [CrossRef]
- Varela, C.; Kim, N.K. Surgical Treatment of Low-Lying Rectal Cancer: Updates. Ann. Coloproctol. 2021, 37, 395–424. [Google Scholar] [CrossRef] [PubMed]
- Faber, R.A.; Tange, F.P.; Galema, H.A.; Zwaan, T.C.; Holman, F.A.; Peeters, K.C.M.J.; Tanis, P.J.; Verhoef, C.; Burggraaf, J.; Mieog, J.S.D.; et al. Quantification of indocyanine green near-infrared fluorescence bowel perfusion assessment in colorectal surgery. Surg. Endosc. 2023; epub ahead of print. [Google Scholar] [CrossRef]


| Clinical Factor | Initial StO2, n (%) | p-Value † | |
|---|---|---|---|
| StO2 (≥60%), n = 62 | StO2 (<60%), n = 6 | ||
| Age (≥70 yr) | 25 (40.3) | 5 (83.3) | 0.080 |
| Male:Female | 41:21 | 6:0 | 0.186 |
| BMI (≥25 kg/m2) | 22 (35.5) | 1 (16.7) | 0.856 |
| ASA score (≥3) | 7 (11.3) | 2 (33.3) | 0.177 |
| Hypertension | 26 (41.9) | 4 (66.7) | 0.394 |
| Diabetes | 13 (21.0) | 1 (16.7) | 1.000 |
| Smoking | 7 (11.3) | 1 (16.7) | 0.543 |
| Alcohol drinking | 13 (100) | 0 (0) | 0.587 |
| Total cholesterol (≥220 mg/dL) | 11 (17.7) | 0 (0) | 0.579 |
| Atherosclerotic risk score (≥20) | 12 (19.4) | 3 (50.0) | 0.116 |
| Stage (≥III) | 26 (41.9) | 2 (33.3) | 1.000 |
| Cancer location | |||
| Sigmoid | 25 (96.2) | 1 (3.8) | 0.395 |
| Rectum | 37 (88.1) | 5 (11.9) | |
| PCRT | 8 (12.9) | 1 (16.7) | 1.000 |
| Cancer obstruction | 14 (22.6) | 1 (16.7) | 1.000 |
| Operation (LAR) | 41 (66.1) | 5 (83.3) | 0.656 |
| Anastomotic level (<5 cm) | 22 (35.5) | 4 (66.7) | 0.193 |
| Diverting ileostomy | 20 (32.3) | 4 (66.7) | 0.175 |
| IMA ligation (high) | 36 (58.1) | 4 (66.7) | 1.000 |
| Anastomotic complication | 4 (6.5) | 1 (16.7) | 0.379 |
| Reoperation | 2 (3.2) | 0 | 1.000 |
| Regression Analysis | Cutoff Value, Mean (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|
| Model (n) | Equation | R2 | StO2 60% | StO2 65% | StO2 70% | StO2 75% | StO2 80% | |
| T1/2MAX (s) | linear (n = 340) | T1/2MAX = 26.351 − 0.267 × StO2 | 0.183 | 10.31 | 8.98 | 7.64 | 6.30 | 4.97 |
| (8.79, 11.83) | (7.73, 10.22) | (96.66, 8.63) | (5.55, 7.06) | (4.37, 5.57) | ||||
| quadratic (n = 340) | T1/2MAX = 82.801 − 1.851 × StO2 + 0.011(StO2)2 | 0.260 | 10.40 | 7.86 | 5.85 | 4.39 | 3.46 | |
| (8.95, 11.85) | (6.61, 9.10) | (4.74, 6.97) | (3.42, 5.35) | (2.70, 4.22) | ||||
| TMAX (s) | linear (n = 340) | TMAX = 76.287 − 0.785 × StO2 | 0.250 | 29.18 | 25.25 | 21.33 | 17.40 | 13.48 |
| (25.52, 32.84) | (22.26, 28.25) | (18.96, 23.70) | (15.58, 19.22) | (12.03, 14.92) | ||||
| quadratic (n = 340) | T MAX = 252.715 − 5.736 × StO2 + 0.034(StO2)2 | 0.369 | 29.45 | 21.76 | 15.74 | 11.41 | 8.76 | |
| (26.09, 32.81) | (18.87, 24.64) | (13.17, 18.32) | (9.18, 13.65) | (6.99, 10.52) | ||||
| Slope (s/AU) | linear (n = 340) | Slope = −2.236 + 0.144 × StO2 | 0.025 | 6.38 | 7.10 | 7.82 | 8.54 | 9.26 |
| (3.98, 8.79) | (5.13, 9.07) | (6.26, 9.38) | (7.34, 9.73) | (8.31, 10.20) | ||||
| linear (n = 335) | Slope = −3.087 + 0.146 × StO2 | 0.043 | 5.68 | 6.41 | 7.14 | 7.87 | 8.60 | |
| (3.81, 7.55) | (4.88, 7.94) | (5.92, 8.35) | (6.93, 8.80) | (7.86, 9.34) | ||||
| NIR perfusion index | linear (n = 340) | NIR = 10.515 + 0.699 × StO2 | 0.152 | 52.48 | 55.98 | 59.48 | 62.98 | 66.47 |
| (48.05, 56.92) | (52.35, 59.62) | (56.60, 62.35) | (60.77, 65.19) | (64.72, 68.23) | ||||
| linear (n = 332) | NIR = 13.125 + 0.683 × StO2 | 0.185 | 54.12 | 57.54 | 60.96 | 64.37 | 67.79 | |
| (50.22, 58.03) | (54.35, 60.73) | (58.43, 63.48) | (62.44, 66.31) | (66.27, 69.31) | ||||
| Perfusion Parameter | Mean ± SD | Range | 95% CI of Mean | Cutoff Level (StO2 ≥ 60%) |
|---|---|---|---|---|
| T1/2MAX (s) | 4.07 ± 5.85 | 0.03–87.67 | 3.45–4.70 | ≤10 s a |
| TMAX (s) | 10.85 ± 14.68 | 1.57–94.77 | 9.28–12.41 | ≤30 s a |
| Perfusion TR | 0.43 ± 0.16 | 0.01–1.00 | 0.41–0.44 | ≤0.8 b |
| FMAX (AU) | 97.21 ± 37.00 | 7.62–199.01 | 93.26–101.16 | ≥25 b |
| Slope (AU/s) | 9.74 ± 8.46 | 0.33–54.95 | 8.83–10.64 | ≥5 a |
| NIR perfusion index | 68.82 ± 16.76 | 10.0–98.0 | 67.03–70.60 | ≥50 a |
| Perfusion Parameter | Cut Off Level | StO2, n (%) | p-Value | |
|---|---|---|---|---|
| <60% | ≥60% | |||
| T1/2MAX (s) | ≤10 | 5 (1.5) | 319 (98.5) | <0.001 |
| >10 | 6 (37.5) | 10 (62.5) | ||
| TMAX (s) | ≤30 | 1 (0.3) | 322 (99.7) | <0.001 |
| >30 | 10 (58.8) | 7 (41.2) | ||
| Perfusion TR | ≤0.8 | 8 (2.4) | 322 (97.6) | <0.001 |
| >0.8 | 3 (30.0) | 7 (70.0) | ||
| FMAX (AU) | ≤25 | 0 (0) | 15 (100) | 0.469 |
| >25 | 11 (3.4) | 314 (96.6) | ||
| Slope (s/AU) | <5 | 11 (10.4) | 95 (89.6) | <0.001 |
| ≥5 | 0 (0) | 234 (100) | ||
| NIR perfusion index | <50 | 8 (18.6) | 35 (81.4) | <0.001 |
| ≥50 | 3 (1.0) | 294 (99.0) | ||
| Total | 11 (3.2) | 329 (96.8) | ||
| Perfusion Parameter | Cutoff Level | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|---|---|---|---|---|---|
| T1/2MAX (s) | ≤10 | 97.0 | 54.5 | 98.5 | 37.5 | 95.6 |
| (94.5, 98.5) | (23.4, 83.3) | (96.4, 99.5) | (15.2, 64.6) | (92.8. 97.5) | ||
| TMAX (s) | ≤30 | 97.9 | 90.9 | 99.7 | 58.8 | 97.6 |
| (95.7, 99.1) | (58.7, 99.8) | (98.3, 100) | (32.9, 81.6) | (95.4, 98.9) | ||
| Perfusion TR | ≤0.8 | 97.9 | 27.3 | 97.6 | 30.0 | 95.6 |
| (95.7, 99.1) | (6.0, 61.0) | (95.3, 98.9) | (6.7, 65.2) | (92.8, 97.5) | ||
| FMAX (AU) | >25 | 95.4 | 0 | 96.6 | 0 | 92.4 |
| (96.2, 99.4) | (0, 28.5) | (94.6, 98.3) | (0, 21.8) | (89.0, 94.9) | ||
| Slope (AU/s) | ≥5 | 71.1 | 100 | 100 | 10.4 | 72.1 |
| (65.9, 76.0) | (71.5, 100) | (98.4, 100) | (5.3, 17.8) | (67.0, 76.8) |
| Perfusion Parameter | AUC | 95% CI | p-Value |
|---|---|---|---|
| T1/2MAX (s) | 0.944 | 0.894–0.994 | <0.001 |
| TMAX (s) | 0.976 | 0.949–1.000 | <0.001 |
| Perfusion TR | 0.428 | 0.176–0.679 | 0.415 |
| FMAX (AU) | 0.404 | 0.234–0.579 | 0.277 |
| Slope (AU/s) | 0.948 | 0.905–0.991 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Son, G.M.; Nazir, A.M.; Yun, M.S.; Lee, I.Y.; Im, S.B.; Kwak, J.Y.; Park, S.-H.; Baek, K.-R.; Gockel, I. The Safe Values of Quantitative Perfusion Parameters of ICG Angiography Based on Tissue Oxygenation of Hyperspectral Imaging for Laparoscopic Colorectal Surgery: A Prospective Observational Study. Biomedicines 2023, 11, 2029. https://doi.org/10.3390/biomedicines11072029
Son GM, Nazir AM, Yun MS, Lee IY, Im SB, Kwak JY, Park S-H, Baek K-R, Gockel I. The Safe Values of Quantitative Perfusion Parameters of ICG Angiography Based on Tissue Oxygenation of Hyperspectral Imaging for Laparoscopic Colorectal Surgery: A Prospective Observational Study. Biomedicines. 2023; 11(7):2029. https://doi.org/10.3390/biomedicines11072029
Chicago/Turabian StyleSon, Gyung Mo, Armaan M. Nazir, Mi Sook Yun, In Young Lee, Sun Bin Im, Jae Yeong Kwak, Sang-Ho Park, Kwang-Ryul Baek, and Ines Gockel. 2023. "The Safe Values of Quantitative Perfusion Parameters of ICG Angiography Based on Tissue Oxygenation of Hyperspectral Imaging for Laparoscopic Colorectal Surgery: A Prospective Observational Study" Biomedicines 11, no. 7: 2029. https://doi.org/10.3390/biomedicines11072029
APA StyleSon, G. M., Nazir, A. M., Yun, M. S., Lee, I. Y., Im, S. B., Kwak, J. Y., Park, S.-H., Baek, K.-R., & Gockel, I. (2023). The Safe Values of Quantitative Perfusion Parameters of ICG Angiography Based on Tissue Oxygenation of Hyperspectral Imaging for Laparoscopic Colorectal Surgery: A Prospective Observational Study. Biomedicines, 11(7), 2029. https://doi.org/10.3390/biomedicines11072029






