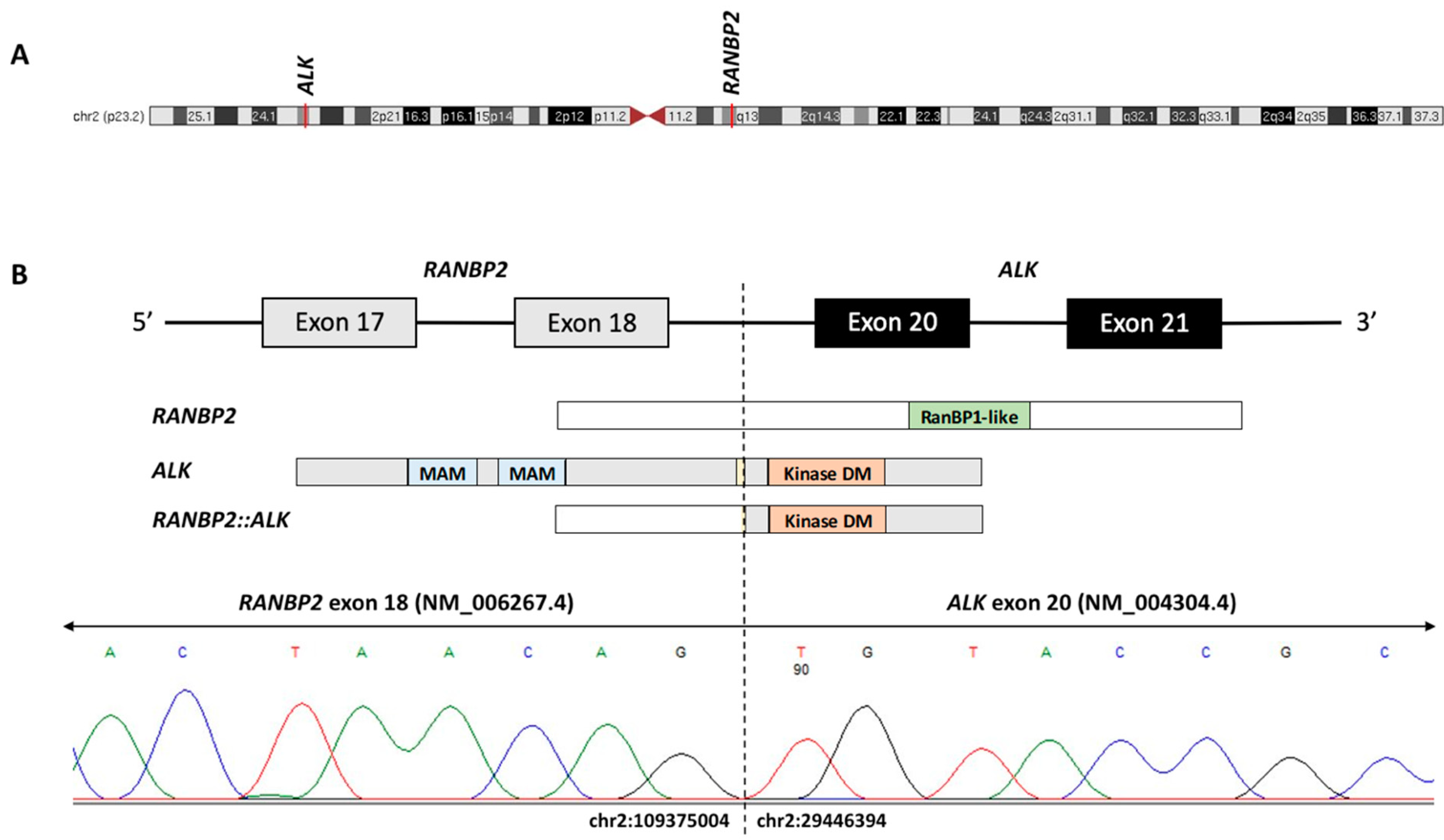
ALK Fusion in an Adolescent with Acute Myeloid Leukemia: A Case Report and Review of the Literature
Abstract
1. Introduction
2. Case Presentation
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benharroch, D.; Meguerian-Bedoyan, Z.; Lamant, L.; Amin, C.; Brugières, L.; Terrier-Lacombe, M.J.; Delsol, G. ALK-positive lymphoma: A single disease with a broad spectrum of morphology. Blood J. Am. Soc. Hematol. 1998, 91, 2076–2084. [Google Scholar]
- Morris, S.W.; Kirstein, M.N.; Valentine, M.B.; Dittmer, K.G.; Shapiro, D.N.; Saltman, D.L.; Look, A.T. Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin’s lymphoma. Science 1994, 263, 1281–1284. [Google Scholar] [CrossRef] [PubMed]
- Soda, M.; Choi, Y.L.; Enomoto, M.; Takada, S.; Yamashita, Y.; Ishikawa, S.; Fujiwara, S.-I.; Watanabe, H.; Kurashina, K.; Hatanaka, H.; et al. Identification of the transforming EML4–ALK fusion gene in non-small-cell lung cancer. Nature 2007, 448, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Griffin, C.A.; Hawkins, A.L.; Dvorak, C.; Henkle, C.; Ellingham, T.; Perlman, E. Recurrent involvement of 2p23 in inflammatory myofibroblastic tumors. Cancer Res. 1999, 59, 2776–2780. [Google Scholar] [PubMed]
- Carén, H.; Abel, F.; Kogner, P.; Martinsson, T. High incidence of DNA mutations and gene amplifications of the ALK gene in advanced sporadic neuroblastoma tumours. Biochem. J. 2008, 416, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Kwak, E.L.; Bang, Y.-J.; Camidge, D.R.; Shaw, A.T.; Solomon, B.; Maki, R.G.; Ou, S.-H.I.; Dezube, B.J.; Jänne, P.A.; Costa, D.B.; et al. Anaplastic Lymphoma Kinase Inhibition in Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2010, 363, 1693–1703. [Google Scholar] [CrossRef] [PubMed]
- Mossé, Y.P.; Voss, S.D.; Lim, M.S.; Rolland, D.; Minard, C.G.; Fox, E.; Adamson, P.; Wilner, K.; Blaney, S.M.; Weigel, B.J. Targeting ALK With Crizotinib in Pediatric Anaplastic Large Cell Lymphoma and Inflammatory Myofibroblastic Tumor: A Children’s Oncology Group Study. J. Clin. Oncol. 2017, 35, 3215–3221. [Google Scholar] [CrossRef] [PubMed]
- Ries, R.E.; Triche, T.J.; Smith, J.L.; Leonti, A.R.; Alonzo, T.A.; Farrar, J.E.; Chen, X.; Liu, Y.; Shaw, T.; Huang, B.J.; et al. Genome and Transcriptome Profiling of Monosomy 7 AML Defines Novel Risk and Therapeutic Cohorts. Blood 2020, 136 (Suppl. S1), 20–21. [Google Scholar] [CrossRef]
- Manselle, M.K.; Ries, R.E.; Hylkema, T.; Leonti, A.; Kirkey, D.C.; Furlan, S.N.; Meshinchi, S. Functional consequence and therapeutic targeting of cryptic ALK fusions in monosomy 7 acute myeloid leukemia. Pediatr. Blood Cancer 2023, 70, e30180. [Google Scholar] [CrossRef] [PubMed]
- Maesako, Y.; Izumi, K.; Okamori, S.; Takeoka, K.; Kishimori, C.; Okumura, A.; Ohno, H. inv (2)(p23q13)/RAN-binding protein 2 (RANBP2)–ALK fusion gene in myeloid leukemia that developed in an elderly woman. Int. J. Hematol. 2014, 99, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Takeoka, K.; Okumura, A.; Maesako, Y.; Akasaka, T.; Ohno, H. Crizotinib resistance in acute myeloid leukemia with inv (2)(p23q13)/RAN binding protein 2 (RANBP2) anaplastic lymphoma kinase (ALK) fusion and monosomy 7. Cancer Genet. 2015, 208, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.-H.; Jang, S.; Park, C.-J.; Cho, Y.-U.; Lee, J.-H.; Lee, K.-H.; Lee, J.-O.; Shin, J.-Y.; Kim, J.-I.; Huh, J.; et al. RANBP2-ALK fusion combined with monosomy 7 in acute myelomonocytic leukemia. Cancer Genet. 2014, 207, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Röttgers, S.; Gombert, M.; Teigler-Schlegel, A.; Busch, K.; Gamerdinger, U.; Slany, R.; Harbott, J.; Borkhardt, A. ALK fusion genes in children with atypical myeloproliferative leukemia. Leukemia 2010, 24, 1197–1200. [Google Scholar] [CrossRef]
- Bazarbachi, A.; Labopin, M.; Battipaglia, G.; Djabali, A.; Forcade, E.; Arcese, W.; Socié, G.; Blaise, D.; Passweg, J.R.; Cornelissen, J.J.; et al. Post-Transplant Sorafenib Improves Overall Survival in FLT3 Mutated AML: A Report from the EBMT Acute Leukemia Working Party. Blood 2018, 132 (Suppl. S1), 708. [Google Scholar] [CrossRef]
- Pollard, J.A.; Alonzo, T.A.; Gerbing, R.; Brown, P.; Fox, E.; Choi, J.; Aplenc, R. Sorafenib in combination with standard chemotherapy for children with high allelic ratio FLT3/ITD+ acute myeloid leukemia: A report from the children’s oncology group protocol AAML1031. J. Clin. Oncol. 2022, 40, 2023–2035. [Google Scholar] [CrossRef] [PubMed]
- Röllig, C.; Serve, H.; Hüttmann, A.; Noppeney, R.; Müller-Tidow, C.; Krug, U.; Ehninger, G. Addition of sorafenib versus placebo to standard therapy in patients aged 60 years or younger with newly diagnosed acute myeloid leukaemia (SORAML): A multicentre, phase 2, randomised controlled trial. Lancet Oncol. 2015, 16, 1691–1699. [Google Scholar] [CrossRef]
- Röllig, C.; Serve, H.; Noppeney, R.; Hanoun, M.; Krug, U.; Baldus, C.D.; Brandts, C.H.; Kunzmann, V.; Einsele, H.; Krämer, A.; et al. Sorafenib or placebo in patients with newly diagnosed acute myeloid leukaemia: Long-term follow-up of the randomized controlled SORAML trial. Leukemia 2021, 35, 2517–2525. [Google Scholar] [CrossRef]
- Gagelmann, N.; Wolschke, C.; Klyuchnikov, E.; Christopeit, M.; Ayuk, F.; Kröger, N. TKI maintenance after stem-cell transplantation for FLT3-ITD positive acute myeloid leukemia: A systematic review and meta-analysis. Front. Immunol. 2021, 12, 630429. [Google Scholar] [CrossRef]


| Literature Source | Patient Age and Disease | Peripheral Blood and Marrow Description | Flow Cytometry Markers | ISCN | RT-PCR |
|---|---|---|---|---|---|
| Maesako et al. [10] | 75 y, AML | WBC: 143.6 × 103/µL 38.6% monocytes; 13.6% immature granulocytes (including blasts) BM blasts: 32.1% BM morphology: > 90% cellularity; marked hyperplasia of myeloid-lineage cells and monocytes | Pos: CD34, CD13, CD33, CD116, CD123, CD11b, CD11c, CD45RA, and HLA-DR +/−: CD36 and CD117 Neg: CD7 and CD56 | 46,XX,inv(2)(p23q13)/,45,idem, −7/46,idem, −7, +mar[1].ish inv(2)(p23)(3’ALK+) (q13)(5’ALK+) | RANBP2::ALK |
| Manselle et al. [9] | 1.901 y, AML | WBC: 66.2 × 103/µL BM blasts: 68% | 45,XY,inv(2)(p13q14), −7[15]/46,XY[5] | RANBP2::ALK | |
| 1.51 y, AML | WBC: 175.7 × 103/µL BM blasts: 71.4% | 45,XY,−7[24] | SPTBN1::ALK | ||
| 9.044 y, AML | WBC: 104.1 × 103/µL BM blasts: 33% | 45,XX,inv(2)(p21q21) c,−7[20] | SPTBN1::ALK | ||
| 1.244 y, AML | WBC: 99.8 × 103/µL BM blasts: 49% | 45,XX, −7[20] | SPTBN1::ALK | ||
| Lim et al. [12] | 31.4 y, AML | WBC: 55.6 × 103/µL; 11% blasts, 20 × 103/µL monocytes BM blasts: 21.5% BM morphology: dramatically increased cellularity; increased myeloblasts and granulocytic hyperplasia | Pos: CD13, CD33, CD15, CD65, and CD14 Neg: CD117, CD41, CD7, CD34, TdT, and all B and T cell antigens | 45,XX,inv(2)(p23q13),–7[20] | RANBP2::ALK |
| Rottgers et al. [13] | 8.0 y, MDS or JMML | WBC: 84 × 103/µL; 10% blasts; 34.5 × 103/µL monocytes BM morphology: dramatically increased cellularity; hyperplasia and dysplasia of granulopoiesis | 45,XY,inv(2)(p23q13), −7/46,XY[5] | RANBP2::ALK | |
| 16.3 y, AML | WBC: 85.3K; 40% blasts; 22.5 × 103/µL monocytes BM morphology: slightly increased cellularity; trilineage dysplasia | 45,XY,inv(2)(p23q13), −7[8]/46,XY,inv(2)(p23q13)[3] | RANBP2::ALK | ||
| 3.5 y, JMML | WBC: 88 × 103/µL; 20% blasts; 27 × 103/µL monocytes BM morphology: dramatically increased cellularity; granulocytic hyperplasia | 45,XY,t(2;2)(p23;q11~ 13), −7 | RANBP2::ALK |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shekar, M.; Llaurador Caraballo, G.; Punia, J.N.; Curry, C.V.; Fisher, K.E.; Redell, M.S. ALK Fusion in an Adolescent with Acute Myeloid Leukemia: A Case Report and Review of the Literature. Biomedicines 2023, 11, 1842. https://doi.org/10.3390/biomedicines11071842
Shekar M, Llaurador Caraballo G, Punia JN, Curry CV, Fisher KE, Redell MS. ALK Fusion in an Adolescent with Acute Myeloid Leukemia: A Case Report and Review of the Literature. Biomedicines. 2023; 11(7):1842. https://doi.org/10.3390/biomedicines11071842
Chicago/Turabian StyleShekar, Meghan, Gabriela Llaurador Caraballo, Jyotinder N. Punia, Choladda V. Curry, Kevin E. Fisher, and Michele S. Redell. 2023. "ALK Fusion in an Adolescent with Acute Myeloid Leukemia: A Case Report and Review of the Literature" Biomedicines 11, no. 7: 1842. https://doi.org/10.3390/biomedicines11071842
APA StyleShekar, M., Llaurador Caraballo, G., Punia, J. N., Curry, C. V., Fisher, K. E., & Redell, M. S. (2023). ALK Fusion in an Adolescent with Acute Myeloid Leukemia: A Case Report and Review of the Literature. Biomedicines, 11(7), 1842. https://doi.org/10.3390/biomedicines11071842






