Modeling Electric Fields in Transcutaneous Spinal Direct Current Stimulation: A Clinical Perspective
Abstract
1. Introduction
2. tsDCS Modeling: Methods, Limitations, and Results
| Duke | Ella | Billie | Louis | |||
|---|---|---|---|---|---|---|
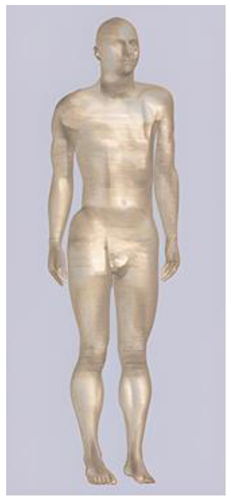 | 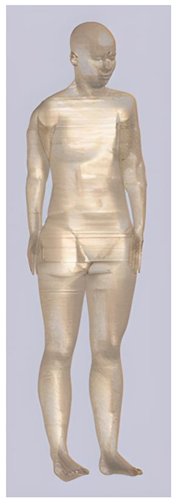 |  |  | |||
| Name | Age (Years) | Sex | Height (m) | Mass (kg) | BMI (kg/m2) | No. of Tissues |
| Duke | 34 | M | 1.74 | 70 | 23.1 | 77 |
| Ella | 26 | F | 1.60 | 58 | 22.7 | 74 |
| Billie | 11 | F | 1.47 | 35 | - | 75 |
| Louis | 14 | M | 1.69 | 50.4 | - | 77 |
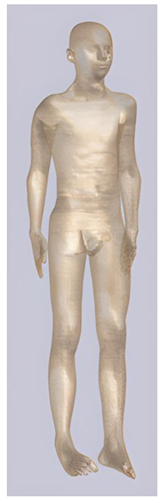
| Roberta | Thelonious | Eartha | Dizzy | |||
|---|---|---|---|---|---|---|
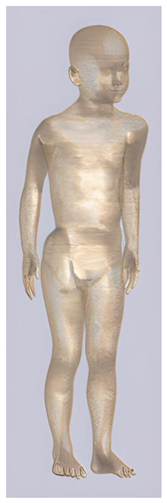 |  |  |  | |||
| Name | Age (Years) | Sex | Height (m) | Mass (kg) | BMI (kg/m2) | No. of Tissues |
| Roberta | 5 | F | 1.10 | 17.8 | 14.9 | 76 |
| Thelonious | 6 | M | 1.15 | 19.3 | 14.1 | 76 |
| Eartha | 8 | F | 1.36 | 30.7 | 16.6 | 76 |
| Dizzy | 8 | M | 1.37 | 26.0 | 13.8 | 76 |
| Computational Studies—Duke Model | |||||||
|---|---|---|---|---|---|---|---|
| Study | tsDCS Protocol | No. of Tissues Considered | ROIs | Induced J (A/m2) | Induced E (V/m) | ||
| Active Electrode | Reference Electrode | Intensity (mA) | |||||
| Miranda et al., 2016 [23] | SP of C7 1 | R deltoid 1 | 2.5 | 9 | C-SC | - | M = 0.27 |
| Bastos et al., 2016 [51] | SP of L2, L3, L4 1 | 4 cm above active electrode 1 | 3 | 8 | L-SC and S/C SC | - | M = 0.29 |
| 8 cm above active electrode 1 | - | M = 0.39 | |||||
| 12 cm above active electrode 1 | - | M = 0.47 | |||||
| 16 cm above active electrode 1 | - | M = 0.57 | |||||
| R deltoid 1 | - | M = 0.35 | |||||
| Fernandes et al., 2016 [45] | SP of C7 1 | R deltoid 1 | 2.5 | 9 | GM and WM in C-SC | - | WM: ≅ 0.15; M = 0.27; m = 0.10 GM: ≅ 0.13; M = 0.16; m = 0.11 |
| SP of C3 2 * | SP of T3 2 * | - | WM: ≅ 0.39; M = 0.69; m = 0.29 GM: ≅ 0.36; M = 0.43; m = 0.33 | ||||
| SP of C3 2 * | SP of T3 2 * | - | WM: ≅ 0.41; M = 0.71; m = 0.29 GM: ≅ 0.37; M = 0.44; m = 0.34 | ||||
| Fernandes et al., 2018 [26] | A: SP of T10 3 | C: R deltoid 3 | 2.5 | 13 | GM and WM in T-SC, L-SC, and S-SC | GM: M = 0.11–0.15 | M = 0.20–0.67 (T-SC) |
| C: umbilicus 3 | M = 0.2–0.44 (L/S-SC) | ||||||
| C: R iliac crest 3 | M = 0.25–0.56 (L/S-SC) | ||||||
| A: SP of T8 3 | C: umbilicus 3 | M = 0.20–0.63 (lower T-SC) | |||||
| C: R iliac crest 3 | M = 0.25–0.72 (lower T-SC) | ||||||
| A: SP of L2 3 | C: R deltoid 3 | M = 0.20–0.59 (T-SC and L/S-SC) | |||||
| C: SP of T8 3 | M = 0.25–0.76 (lower T-SC) | ||||||
| Pereira et al., 2018 [48] | A: between SPs of L1, L2 3 | C: L ASIC 3 | 2.5 | 13 | GM and WM in L-SC | WM: M = 0.078 GM: M = 0.040 | WM: M = 0.12 GM: M = 0.10 |
| Fernandes et al., 2019 [47] | A: SP of T3 3 | C: SP of C3 3 | 2.5 | 18 | GM and WM in C-SC | - | WM: M = 0.49 GM: M = 0.44 |
| Fernandes et al., 2019 [46] | SP of C7 3 | R deltoid 3 | 2.5 | 15 | GM and WM in C-SC | - | - |
| SP of C7 3 | cervicomental angle 3 | - | - | ||||
| SP of C4 3 | cervicomental angle 3 | - | - | ||||
| SP of C3 3 | SP of T3 3 | - | WM: M = 0.50 GM: M = 0.40 | ||||
| Computational Studies—Ella Model | |||||||
|---|---|---|---|---|---|---|---|
| Study | tsDCS Protocol | No. of Tissues Considered | ROIs | Induced J (A/m2) | Induced E (V/m) | ||
| Active Electrode | Reference Electrode | Intensity (mA) | |||||
| Parazzini et al., 2014 [21] | SP of T10 1 | R deltoid 2 | 3 | - | SC, CE, NRs, and muscles | C-SC: = 8.2 × 10−4; M = 6.4 × 10−3 T-SC: = 4.6 × 10−3; M = 1.4 × 10−2 | - |
| umbilicus 2 | C-SC: = 5.7 × 10−5; M = 3.2 × 10−4 T-SC: = 4.1 × 10−3; M = 1.4 × 10−2 | - | |||||
| head vertex 2 | C-SC: = 3.4 × 10−2; M = 8.5 × 10−2 T-SC: = 9.4 × 10−3; M = 2.8 × 10−2 | - | |||||
| Kuck et al., 2017 [22] | SP of T11 3 | L posterior shoulder 3 | 2.5 | - | GM and WM in L-SC | - | M = 0.47–0.82 |
| placed at equal distance, superior and inferior to T11 3 | - | ||||||
| SP of T11 3 | L and R ASIC 3 | - | |||||
| Kuck et al., 2019 [58] | SP of T11 3 | L posterior shoulder 3 | 2.5 | 22 | SC, soft tissues and vertebrae at representative levels (C2, T2, T6, T10) | without implants: Vertebrae: M = 0.11 (T6) Soft tissues: M = 0.55 (T6) SC: M = 0.4 (T6) with implants: Vertebrae: M = 0.11 (T6) Soft tissues: M = 0.37 (T16) SC: M = 0.11 (T6) | without implants: Vertebrae: M = 7.02 (T6) Soft tissues: M = 4.94 (T2) SC: M = 2.6 (T6) with implants: Vertebrae: M = 5.57 (T6) Soft tissues: M = 2.32 (T6) SC: M = 0.15 (T6) |
| Placed 7 cm superior and inferior to T11 3 | without implants: Vertebrae: M = 0.15 (T6) Soft tissues: M = 0.66 (T10) SC: M = 0.59 (T10) with implants: Vertebrae: M = 0.23 (T10) Soft tissues: M = 1.04 (T10) SC: M = N.R. | without implants: Vertebrae: M = 7.7 (T6) Soft tissues: M = 5.38 (T10) SC: M = 3.6 (T10) with implants: Vertebrae: M = 11.78 (T10) Soft tissues: M = 6.52 (T10) SC: M = N.R. | |||||
| Computational Studies—Billie and Louis Models | ||||||
|---|---|---|---|---|---|---|
| Study | Model | tsDCS Protocol | ROIs | Induced J (A/m2) | ||
| Active Electrode | Reference Electrode | Intensity (mA) | ||||
| Parazzini et al., 2014 [21] | Louis | SP of T10 1 | R deltoid 2 | 3 | SC, CE, NRs, and muscles | C-SC: = 3.6 × 10−4; M = 2.4 × 10−3 T-SC: = 5.4 × 10−3; M = 1.6 × 10−2 L-SC: = 3.9 × 10−3; M = 6.1 × 10−3 |
| umbilicus 2 | C-SC: = 4.7 × 10−5; M = 4.1 × 10−4 T-SC: = 4.9 × 10−3; M = 1.6 × 10−2 L-SC: = 1.2 × 10−2; M = 1.7 × 10−2 | |||||
| head vertex 2 | C-SC: = 3.4 × 10−2; M = 7.9 × 10−2 T-SC: = 1.6 × 10−2; M = 3.3 × 10−2 L-SC: = 3.8 × 10−3; M = 6.0 × 10−3 | |||||
| Billie | SP of T10 1 | R deltoid 2 | C-SC: = 6.5 × 10−4; M = 3.4 × 10−3 T-SC: = 6.3 × 10−3; M = 1.4 × 10−2 L-SC: = 2.3 × 10−3; M = 1.1 × 10−2 S/C-SC: = 9.2 × 10−4; M = 1.7 × 10−3 | |||
| umbilicus 2 | C-SC: = 1.5 × 10−4; M = 5.2 × 10−4 T-SC: = 5.8 × 10−3; M = 1.9 × 10−2 L-SC: = 1.0 × 10−2; M = 2.4 × 10−2 S/C-SC: = 2.3 × 10−3; M = 4.3 × 10−3 | |||||
| head vertex 2 | C-SC: = 4.0 × 10−2; M = 6.3 × 10−2 T-SC: = 1.4 × 10−2; M = 3.2 × 10−2 L-SC: = 1.6 × 10−3; M = 8.5 × 10−3 S/C-SC: = 2.5 × 10−4; M = 4.6 × 10−4 | |||||
| Computational Studies—Roberta, Thelonious, Eartha and Dizzy Models | ||||||
|---|---|---|---|---|---|---|
| Study | Model | tsDCS Protocol | ROIs | Induced E (V/m) | ||
| Active Electrode | Reference Electrode | Intensity (mA) | ||||
| Fiocchi et al., 2016 [41] | Roberta | SP of T10 1 | R deltoid 2 | 3 | SC, CE and NRs | C-SC: me ≅ 0.1; M ≅ 0.5; m ≅ 0.01 T-SC: me ≅ 1.6; M ≅ 2.7; m ≅ 0.3 L-SC: me ≅ 0.8; M ≅ 1.2; m ≅ 0.45 |
| Thelonious | SP of T10 1 | R deltoid 2 | C-SC: me ≅ 0.1; M ≅ 0.5; m ≅ 0.01 T-SC: me ≅ 1.6; M ≅ 2.7; m ≅ 0.3 L-SC: me ≅ 0.8; M ≅ 1.2; m ≅ 0.45 | |||
| Eartha | SP of T10 1 | R deltoid 2 | C-SC: me ≅ 0.15; M ≅ 0.25; m ≅ 0.01 T-SC: me ≅ 0.6; M ≅ 1.8; m ≅ 0.25 L-SC: me ≅ 0.25; M ≅ 0.3; m ≅ 0.15 | |||
| Dizzy | SP of T10 1 | R deltoid 2 | C-SC: me ≅ 0.1; M ≅ 0.25; m ≅ 0.01 T-SC: me ≅ 0.8; M ≅ 1.6; m ≅ 0.2 L-SC: me ≅ 0.25; M ≅ 0.4; m ≅ 0.15 | |||
3. Computational Insights for Clinical Studies
4. Insights for Clinical Studies from Animal Models
5. What Is Next? Role of Models for tsDCS Applications
6. Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fernandes, S.R.; Salvador, R.; de Carvalho, M.; Miranda, P.C. Modelling studies of non-invasive electric and magnetic stimulation of the spinal cord. In Brain and Human Body Modeling 2020; Makarov, S.N., Noetscher, G.M., Nummenmaa, A., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 139–165. ISBN 978-3-030-45622-1. [Google Scholar]
- Iglesias, C.; Nielsen, J.B.; Marchand-Pauvert, V. Corticospinal Inhibition of Transmission in Propriospinal-like Neurones during Human Walking. Eur. J. Neurosci. 2008, 28, 1351–1361. [Google Scholar] [CrossRef]
- Ahmed, Z.; Aguilar, J.; Pulecchi, F.; Dilena, R.; Oliviero, A.; Priori, A.; Foffani, G. Trans-Spinal Direct Current Stimulation Modulates Motor Cortex-Induced Muscle Contraction in Mice. J. Appl. Physiol. 2011, 110, 1414–1424. [Google Scholar] [CrossRef]
- Ahmed, Z. Effects of Cathodal Trans-Spinal Direct Current Stimulation on Mouse Spinal Network and Complex Multijoint Movements. J. Neurosci. 2013, 33, 14949–14957. [Google Scholar] [CrossRef] [PubMed]
- Eccles, J.C.; Kostyuk, P.G.; Schmidt, R.F. The Effect of Electric Polarization of the Spinal Cord on Central Afferent Fibres and on Their Excitatory Synaptic Action. J. Physiol. 1962, 162, 138–150. [Google Scholar] [CrossRef] [PubMed]
- Priori, A.; Ciocca, M.; Parazzini, M.; Vergari, M.; Ferrucci, R. Transcranial Cerebellar Direct Current Stimulation and Transcutaneous Spinal Cord Direct Current Stimulation as Innovative Tools for Neuroscientists. J. Physiol. 2014, 592, 3345–3369. [Google Scholar] [CrossRef]
- Cogiamanian, F.; Ardolino, G.; Vergari, M.; Ferrucci, R.; Ciocca, M.; Scelzo, E.; Barbieri, S.; Priori, A. Transcutaneous Spinal Direct Current Stimulation. Front. Psychiatry 2012, 3, 63. [Google Scholar] [CrossRef]
- Huang, Y.; Thomas, C.; Datta, A. Optimized Transcutaneous Spinal Cord Direct Current Stimulation Using Multiple Electrodes from 3/9/7 System. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 6290–6293. [Google Scholar]
- Cogiamanian, F.; Vergari, M.; Pulecchi, F.; Marceglia, S.; Priori, A. Effect of Spinal Transcutaneous Direct Current Stimulation on Somatosensory Evoked Potentials in Humans. Clin. Neurophysiol. 2008, 119, 2636–2640. [Google Scholar] [CrossRef] [PubMed]
- Winkler, T.; Hering, P.; Straube, A. Spinal DC Stimulation in Humans Modulates Post-Activation Depression of the H-Reflex Depending on Current Polarity. Clin. Neurophysiol. 2010, 121, 957–961. [Google Scholar] [CrossRef]
- Lim, C.-Y.; Shin, H.-I. Noninvasive DC Stimulation on Neck Changes MEP. Neuroreport 2011, 22, 819–823. [Google Scholar] [CrossRef]
- Cogiamanian, F.; Vergari, M.; Schiaffi, E.; Marceglia, S.; Ardolino, G.; Barbieri, S.; Priori, A. Transcutaneous Spinal Cord Direct Current Stimulation Inhibits the Lower Limb Nociceptive Flexion Reflex in Human Beings. Pain 2011, 152, 370–375. [Google Scholar] [CrossRef]
- Truini, A.; Vergari, M.; Biasiotta, A.; La Cesa, S.; Gabriele, M.; Di Stefano, G.; Cambieri, C.; Cruccu, G.; Inghilleri, M.; Priori, A. Transcutaneous Spinal Direct Current Stimulation Inhibits Nociceptive Spinal Pathway Conduction and Increases Pain Tolerance in Humans. Eur. J. Pain 2011, 15, 1023–1027. [Google Scholar] [CrossRef]
- Lamy, J.-C.; Ho, C.; Badel, A.; Arrigo, R.T.; Boakye, M. Modulation of Soleus H Reflex by Spinal DC Stimulation in Humans. J. Neurophysiol. 2012, 108, 906–914. [Google Scholar] [CrossRef]
- Hubli, M.; Dietz, V.; Schrafl-Altermatt, M.; Bolliger, M. Modulation of Spinal Neuronal Excitability by Spinal Direct Currents and Locomotion after Spinal Cord Injury. Clin. Neurophysiol. 2013, 124, 1187–1195. [Google Scholar] [CrossRef]
- Guidetti, M.; Ferrucci, R.; Vergari, M.; Aglieco, G.; Naci, A.; Versace, S.; Pacheco-Barrios, K.; Giannoni-Luza, S.; Barbieri, S.; Priori, A.; et al. Effects of Transcutaneous Spinal Direct Current Stimulation (TsDCS) in Patients With Chronic Pain: A Clinical and Neurophysiological Study. Front. Neurol. 2021, 12, 695910. [Google Scholar] [CrossRef] [PubMed]
- Bocci, T.; Barloscio, D.; Vergari, M.; Di Rollo, A.; Rossi, S.; Priori, A.; Sartucci, F. Spinal Direct Current Stimulation Modulates Short Intracortical Inhibition. Neuromodul. Technol. Neural Interface 2015, 18, 686–693. [Google Scholar] [CrossRef]
- Bocci, T.; Caleo, M.; Vannini, B.; Vergari, M.; Cogiamanian, F.; Rossi, S.; Priori, A.; Sartucci, F. An Unexpected Target of Spinal Direct Current Stimulation: Interhemispheric Connectivity in Humans. J. Neurosci. Methods 2015, 254, 18–26. [Google Scholar] [CrossRef]
- Bocci, T.; Marceglia, S.; Vergari, M.; Cognetto, V.; Cogiamanian, F.; Sartucci, F.; Priori, A. Transcutaneous Spinal Direct Current Stimulation Modulates Human Corticospinal System Excitability. J. Neurophysiol. 2015, 114, 440–446. [Google Scholar] [CrossRef]
- Bocci, T.; Vannini, B.; Torzini, A.; Mazzatenta, A.; Vergari, M.; Cogiamanian, F.; Priori, A.; Sartucci, F. Cathodal Transcutaneous Spinal Direct Current Stimulation (TsDCS) Improves Motor Unit Recruitment in Healthy Subjects. Neurosci. Lett. 2014, 578, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Parazzini, M.; Fiocchi, S.; Liorni, I.; Rossi, E.; Cogiamanian, F.; Vergari, M.; Priori, A.; Ravazzani, P. Modeling the Current Density Generated by Transcutaneous Spinal Direct Current Stimulation (TsDCS). Clin. Neurophysiol. 2014, 125, 2260–2270. [Google Scholar] [CrossRef] [PubMed]
- Kuck, A.; Stegeman, D.F.; Asseldonk, E.H.F. van Modeling Trans-Spinal Direct Current Stimulation for the Modulation of the Lumbar Spinal Motor Pathways. J. Neural. Eng. 2017, 14, 056014. [Google Scholar] [CrossRef]
- Miranda, P.C.; Salvador, R.; Wenger, C.; Fernandes, S.R. Computational Models of Non-Invasive Brain and Spinal Cord Stimulation. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 6457–6460. [Google Scholar]
- Peterchev, A.V.; Wagner, T.A.; Miranda, P.C.; Nitsche, M.A.; Paulus, W.; Lisanby, S.H.; Pascual-Leone, A.; Bikson, M. Fundamentals of Transcranial Electric and Magnetic Stimulation Dose: Definition, Selection, and Reporting Practices. Brain Stimul. 2012, 5, 435–453. [Google Scholar] [CrossRef] [PubMed]
- Guidetti, M.; Arlotti, M.; Bocci, T.; Bianchi, A.M.; Parazzini, M.; Ferrucci, R.; Priori, A. Electric Fields Induced in the Brain by Transcranial Electric Stimulation: A Review of In Vivo Recordings. Biomedicines 2022, 10, 2333. [Google Scholar] [CrossRef]
- Fernandes, S.R.; Salvador, R.; Wenger, C.; de Carvalho, M.; Miranda, P.C. Transcutaneous Spinal Direct Current Stimulation of the Lumbar and Sacral Spinal Cord: A Modelling Study. J. Neural Eng. 2018, 15, 036008. [Google Scholar] [CrossRef]
- Bikson, M.; Rahman, A.; Datta, A. Computational Models of Transcranial Direct Current Stimulation. Clin. EEG Neurosci. 2012, 43, 176–183. [Google Scholar] [CrossRef]
- Albizu, A.; Fang, R.; Indahlastari, A.; O’Shea, A.; Stolte, S.E.; See, K.B.; Boutzoukas, E.M.; Kraft, J.N.; Nissim, N.R.; Woods, A.J. Machine Learning and Individual Variability in Electric Field Characteristics Predict TDCS Treatment Response. Brain Stimul. 2020, 13, 1753–1764. [Google Scholar] [CrossRef]
- Datta, A.; Krause, M.R.; Pilly, P.K.; Choe, J.; Zanos, T.P.; Thomas, C.; Pack, C.C. On Comparing in Vivo Intracranial Recordings in Non-Human Primates to Predictions of Optimized Transcranial Electrical Stimulation. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 1774–1777. [Google Scholar]
- Chhatbar, P.Y.; Kautz, S.A.; Takacs, I.; Rowland, N.C.; Revuelta, G.J.; George, M.S.; Bikson, M.; Feng, W. Evidence of Transcranial Direct Current Stimulation-Generated Electric Fields at Subthalamic Level in Human Brain in Vivo. Brain Stimul. 2018, 11, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Esmaeilpour, Z.; Milosevic, M.; Azevedo, K.; Khadka, N.; Navarro, J.; Brunoni, A.; Popovic, M.R.; Bikson, M.; Fonoff, E.T. Proceedings #21. Intracranial Voltage Recording during Transcranial Direct Current Stimulation (TDCS) in Human Subjects with Validation of a Standard Model. Brain Stimul. 2017, 10, e72–e75. [Google Scholar] [CrossRef]
- Salimpour, Y.; Liu, C.-C.; Webber, W.R.; Mills, K.A.; Anderson, W.S. Subdural Recordings from an Awake Human Brain for Measuring Current Intensity during Transcranial Direct Current Stimulation. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju, Republic of Korea, 11–15 July 2017; pp. 1110–1113. [Google Scholar]
- Christ, A.; Kainz, W.; Hahn, E.G.; Honegger, K.; Zefferer, M.; Neufeld, E.; Rascher, W.; Janka, R.; Bautz, W.; Chen, J.; et al. The Virtual Family—Development of Surface-Based Anatomical Models of Two Adults and Two Children for Dosimetric Simulations. Phys. Med. Biol. 2010, 55, N23–N38. [Google Scholar] [CrossRef]
- Indahlastari, A.; Albizu, A.; Kraft, J.N.; O’Shea, A.; Nissim, N.R.; Dunn, A.L.; Carballo, D.; Gordon, M.P.; Taank, S.; Kahn, A.T.; et al. Individualized TDCS Modeling Predicts Functional Connectivity Changes within the Working Memory Network in Older Adults. Brain Stimul. 2021, 14, 1205–1215. [Google Scholar] [CrossRef] [PubMed]
- Cancelli, A.; Cottone, C.; Giordani, A.; Asta, G.; Lupoi, D.; Pizzella, V.; Tecchio, F. MRI-Guided Regional Personalized Electrical Stimulation in Multisession and Home Treatments. Front. Neurosci. 2018, 12, 284. [Google Scholar] [CrossRef]
- Reato, D.; Salvador, R.; Bikson, M.; Opitz, A.; Dmochowski, J.; Miranda, P.C. Principles of transcranial direct current Stimulation (TDCS): Introduction to the biophysics of TDCS. In Practical Guide to Transcranial Direct Current Stimulation: Principles, Procedures and Applications; Knotkova, H., Nitsche, M.A., Bikson, M., Woods, A.J., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 45–80. ISBN 978-3-319-95948-1. [Google Scholar]
- Opitz, A.; Yeagle, E.; Thielscher, A.; Schroeder, C.; Mehta, A.D.; Milham, M.P. On the Importance of Precise Electrode Placement for Targeted Transcranial Electric Stimulation. NeuroImage 2018, 181, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Gellner, A.-K.; Reis, J.; Fritsch, B. Glia: A Neglected Player in Non-Invasive Direct Current Brain Stimulation. Front. Cell. Neurosci. 2016, 10, 188. [Google Scholar] [CrossRef]
- Chhatbar, P.Y.; George, M.S.; Kautz, S.A.; Feng, W. Charge Density, Not Current Density, Is a More Comprehensive Safety Measure of Transcranial Direct Current Stimulation. Brain Behav. Immun. 2017, 66, 414–415. [Google Scholar] [CrossRef] [PubMed]
- Roche, N.; Geiger, M.; Bussel, B. Mechanisms Underlying Transcranial Direct Current Stimulation in Rehabilitation. Ann. Phys. Rehabil. Med. 2015, 58, 214–219. [Google Scholar] [CrossRef]
- Fiocchi, S.; Ravazzani, P.; Priori, A.; Parazzini, M. Cerebellar and Spinal Direct Current Stimulation in Children: Computational Modeling of the Induced Electric Field. Front. Hum. Neurosci. 2016, 10, 522. [Google Scholar] [CrossRef]
- Gabriel, S.; Lau, R.W.; Gabriel, C. The Dielectric Properties of Biological Tissues: II. Measurements in the Frequency Range 10 Hz to 20 GHz. Phys. Med. Biol. 1996, 41, 2251–2269. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, C.; Peyman, A.; Grant, E.H. Electrical Conductivity of Tissue at Frequencies below 1 MHz. Phys. Med. Biol. 2009, 54, 4863–4878. [Google Scholar] [CrossRef]
- Chen, X.-L.; Benkler, S.; Chavannes, N.; De Santis, V.; Bakker, J.; van Rhoon, G.; Mosig, J.; Kuster, N. Analysis of Human Brain Exposure to Low-Frequency Magnetic Fields: A Numerical Assessment of Spatially Averaged Electric Fields and Exposure Limits. Bioelectromagnetics 2013, 34, 375–384. [Google Scholar] [CrossRef]
- Fernandes, S.R.; Salvador, R.; Wenger, C.; de Carvalho, M.A.; Miranda, P.C. Influence of Electrode Configuration on the Electric Field Distribution during Transcutaneous Spinal Direct Current Stimulation of the Cervical Spine. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 3121–3124. [Google Scholar]
- Fernandes, S.R.; Pereira, M.; Salvador, R.; Miranda, P.C.; de Carvalho, M. Cervical Trans-Spinal Direct Current Stimulation: A Modelling-Experimental Approach. J. Neuroeng. Rehabil. 2019, 16, 123. [Google Scholar] [CrossRef]
- Fernandes, S.R.; Salvador, R.; de Carvalho, M.; Miranda, P.C. Electric Field Distribution during Non-Invasive Electric and Magnetic Stimulation of the Cervical Spinal Cord. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 5898–5901. [Google Scholar]
- Pereira, M.; Fernandes, S.R.; Miranda, P.C.; de Carvalho, M. Neuromodulation of Lower Limb Motor Responses with Transcutaneous Lumbar Spinal Cord Direct Current Stimulation. Clin. Neurophysiol. 2018, 129, 1999–2009. [Google Scholar] [CrossRef]
- Nitsche, M.A.; Cohen, L.G.; Wassermann, E.M.; Priori, A.; Lang, N.; Antal, A.; Paulus, W.; Hummel, F.; Boggio, P.S.; Fregni, F.; et al. Transcranial Direct Current Stimulation: State of the Art 2008. Brain Stimul. 2008, 1, 206–223. [Google Scholar] [CrossRef]
- Miranda, P.C.; Mekonnen, A.; Salvador, R.; Ruffini, G. The Electric Field in the Cortex during Transcranial Current Stimulation. NeuroImage 2013, 70, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Bastos, R.; Fernandes, S.R.; Salvador, R.; Wenger, C.; de Carvalho, M.A.; Miranda, P.C. The Effect of Inter-Electrode Distance on the Electric Field Distribution during Transcutaneous Lumbar Spinal Cord Direct Current Stimulation. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 1754–1757. [Google Scholar]
- Fritsch, B.; Reis, J.; Martinowich, K.; Schambra, H.M.; Ji, Y.; Cohen, L.G.; Lu, B. Direct Current Stimulation Promotes BDNF-Dependent Synaptic Plasticity: Potential Implications for Motor Learning. Neuron 2010, 66, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Law, S.K. Thickness and Resistivity Variations over the Upper Surface of the Human Skull. Brain Topogr. 1993, 6, 99–109. [Google Scholar] [CrossRef]
- Choi, Y.-A.; Kim, Y.; Shin, H.-I. Pilot Study of Feasibility and Effect of Anodal Transcutaneous Spinal Direct Current Stimulation on Chronic Neuropathic Pain after Spinal Cord Injury. Spinal Cord 2019, 57, 461–470. [Google Scholar] [CrossRef]
- Williams, P.T.J.A.; Truong, D.Q.; Seifert, A.C.; Xu, J.; Bikson, M.; Martin, J.H. Selective Augmentation of Corticospinal Motor Drive with Trans-Spinal Direct Current Stimulation in the Cat. Brain Stimul. 2022, 15, 624–634. [Google Scholar] [CrossRef]
- Saywell, S.A.; Ford, T.W.; Kirkwood, P.A.; Kirkwood, P.A. Axonal Projections of Renshaw Cells in the Thoracic Spinal Cord. Physiol. Rep. 2013, 1, 161. [Google Scholar] [CrossRef]
- Parazzini, M.; Rossi, E.; Ferrucci, R.; Liorni, I.; Priori, A.; Ravazzani, P. Modelling the Electric Field and the Current Density Generated by Cerebellar Transcranial DC Stimulation in Humans. Clin. Neurophysiol. 2014, 125, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Kuck, A.; Stegeman, D.F.; van Asseldonk, E.H.F. Modeling Trans-Spinal Direct Current Stimulation in the Presence of Spinal Implants. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 790–797. [Google Scholar] [CrossRef]
- Wang, L.; Liu, C.; Hou, Y.; Zhan, S.; Zhang, Z.; Wang, J.; Wang, Y. Altered Cortical Gray Matter Volume and Functional Connectivity after Transcutaneous Spinal Cord Direct Current Stimulation in Idiopathic Restless Legs Syndrome. Sleep Med. 2020, 74, 254–261. [Google Scholar] [CrossRef]
- Alhassani, G.; Treleaven, J.; Schabrun, S.S.M. Combined Transcranial and Trans-Spinal Direct Current Stimulation in Chronic Headache: A Feasibility and Safety Trial for a Novel Intervention. Hong Kong Physiother. J. 2017, 37, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lamy, J.-C.; Varriale, P.; Apartis, E.; Mehdi, S.; Blancher-Meinadier, A.; Kosutzka, Z.; Degos, B.; Frismand, S.; Simonetta-Moreau, M.; Meunier, S.; et al. Trans-Spinal Direct Current Stimulation for Managing Primary Orthostatic Tremor. Mov. Disord. 2021, 36, 1835–1842. [Google Scholar] [CrossRef]
- Heide, A.C.; Winkler, T.; Helms, H.J.; Nitsche, M.A.; Trenkwalder, C.; Paulus, W.; Bachmann, C.G. Effects of Transcutaneous Spinal Direct Current Stimulation in Idiopathic Restless Legs Patients. Brain Stimul. 2014, 7, 636–642. [Google Scholar] [CrossRef]
- Berra, E.; Bergamaschi, R.; De Icco, R.; Dagna, C.; Perrotta, A.; Rovaris, M.; Grasso, M.G.; Anastasio, M.G.; Pinardi, G.; Martello, F.; et al. The Effects of Transcutaneous Spinal Direct Current Stimulation on Neuropathic Pain in Multiple Sclerosis: Clinical and Neurophysiological Assessment. Front. Hum. Neurosci. 2019, 13, 31. [Google Scholar] [CrossRef]
- Marangolo, P.; Fiori, V.; Shofany, J.; Gili, T.; Caltagirone, C.; Cucuzza, G.; Priori, A. Moving Beyond the Brain: Transcutaneous Spinal Direct Current Stimulation in Post-Stroke Aphasia. Front. Neurol. 2017, 8, 400. [Google Scholar] [CrossRef]
- Pisano, F.; Caltagirone, C.; Incoccia, C.; Marangolo, P. Spinal or Cortical Direct Current Stimulation: Which Is the Best? Evidence from Apraxia of Speech in Post-Stroke Aphasia. Behav. Brain Res. 2021, 399, 113019. [Google Scholar] [CrossRef]
- Pisano, F.; Caltagirone, C.; Satriano, F.; Perri, R.; Fadda, L.; Marangolo, P. Can Alzheimer’s Disease Be Prevented? First Evidence from Spinal Stimulation Efficacy on Executive Functions. J. Alzheimer Dis. 2020, 77, 1755–1764. [Google Scholar] [CrossRef]
- Powell, E.S.; Carrico, C.; Salyers, E.; Westgate, P.M.; Sawaki, L. The Effect of Transcutaneous Spinal Direct Current Stimulation on Corticospinal Excitability in Chronic Incomplete Spinal Cord Injury. NeuroRehabilitation 2018, 43, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Ardolino, G.; Bocci, T.; Nigro, M.; Vergari, M.; Di Fonzo, A.; Bonato, S.; Cogiamanian, F.; Cortese, F.; Cova, I.; Barbieri, S.; et al. Spinal Direct Current Stimulation (TsDCS) in Hereditary Spastic Paraplegias (HSP): A Sham-Controlled Crossover Study. J. Spinal Cord Med. 2021, 44, 46–53. [Google Scholar] [CrossRef]
- Awosika, O.O.; Matthews, S.; Staggs, E.J.; Boyne, P.; Song, X.; Rizik, B.A.; Sucharew, H.J.; Zhang, C.; Mungcal, G.; Moudgal, R.; et al. Backward Locomotor Treadmill Training Combined with Transcutaneous Spinal Direct Current Stimulation in Stroke: A Randomized Pilot Feasibility and Safety Study. Brain Commun. 2020, 2, fcaa045. [Google Scholar] [CrossRef] [PubMed]
- Picelli, A.; Chemello, E.; Castellazzi, P.; Roncari, L.; Waldner, A.; Saltuari, L.; Smania, N. Combined Effects of Transcranial Direct Current Stimulation (TDCS) and Transcutaneous Spinal Direct Current Stimulation (TsDCS) on Robot-Assisted Gait Training in Patients with Chronic Stroke: A Pilot, Double Blind, Randomized Controlled Trial. Restor. Neurol. Neurosci. 2015, 33, 357–368. [Google Scholar] [CrossRef]
- Bikson, M.; Datta, A.; Elwassif, M. Establishing Safety Limits for Transcranial Direct Current Stimulation. Clin. Neurophysiol. 2009, 120, 1033–1034. [Google Scholar] [CrossRef]
- Nitsche, M.A.; Liebetanz, D.; Lang, N.; Antal, A.; Tergau, F.; Paulus, W. Safety Criteria for Transcranial Direct Current Stimulation (TDCS) in Humans. Clin. Neurophysiol. 2003, 114, 2220–2222. [Google Scholar] [CrossRef]
- McCaig, C.D.; Rajnicek, A.M.; Song, B.; Zhao, M. Controlling Cell Behavior Electrically: Current Views and Future Potential. Physiol. Rev. 2005, 85, 943–978. [Google Scholar] [CrossRef]
- Heo, C.; Yoo, J.; Lee, S.; Jo, A.; Jung, S.; Yoo, H.; Lee, Y.H.; Suh, M. The Control of Neural Cell-to-Cell Interactions through Non-Contact Electrical Field Stimulation Using Graphene Electrodes. Biomaterials 2011, 32, 19–27. [Google Scholar] [CrossRef]
- Hernández-Labrado, G.R.; Polo, J.L.; López-Dolado, E.; Collazos-Castro, J.E. Spinal Cord Direct Current Stimulation: Finite Element Analysis of the Electric Field and Current Density. Med. Biol. Eng. Comput. 2011, 49, 417–429. [Google Scholar] [CrossRef]
- Bedlack, R.S.; Wei, M.D.; Loew, L.M. Localized Membrane Depolarizations and Localized Calcium Influx during Electric Field-Guided Neurite Growth. Neuron 1992, 9, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Erskine, L.; Stewart, R.; McCaig, C.D. Electric Field-Directed Growth and Branching of Cultured Frog Nerves: Effects of Aminoglycosides and Polycations. J. Neurobiol. 1995, 26, 523–536. [Google Scholar] [CrossRef] [PubMed]
- Rajnicek, A.M.; Foubister, L.E.; McCaig, C.D. Growth Cone Steering by a Physiological Electric Field Requires Dynamic Microtubules, Microfilaments and Rac-Mediated Filopodial Asymmetry. J. Cell Sci. 2006, 119, 1736–1745. [Google Scholar] [CrossRef]
- Rajnicek, A.M.; Foubister, L.E.; McCaig, C.D. Temporally and Spatially Coordinated Roles for Rho, Rac, Cdc42 and Their Effectors in Growth Cone Guidance by a Physiological Electric Field. J. Cell Sci. 2006, 119, 1723–1735. [Google Scholar] [CrossRef] [PubMed]
- Borgens, R.B. Electrically Mediated Regeneration and Guidance of Adult Mammalian Spinal Axons into Polymeric Channels. Neuroscience 1999, 91, 251–264. [Google Scholar] [CrossRef] [PubMed]
- Agboada, D.; Mosayebi-Samani, M.; Kuo, M.-F.; Nitsche, M.A. Induction of Long-Term Potentiation-like Plasticity in the Primary Motor Cortex with Repeated Anodal Transcranial Direct Current Stimulation—Better Effects with Intensified Protocols? Brain Stimul. 2020, 13, 987–997. [Google Scholar] [CrossRef]
- Wenderoth, N.; Debaere, F.; Sunaert, S.; Swinnen, S.P. The Role of Anterior Cingulate Cortex and Precuneus in the Coordination of Motor Behaviour. Eur. J. Neurosci. 2005, 22, 235–246. [Google Scholar] [CrossRef]
- Veasey, S.C.; Fornal, C.A.; Metzler, C.W.; Jacobs, B.L. Response of Serotonergic Caudal Raphe Neurons in Relation to Specific Motor Activities in Freely Moving Cats. J. Neurosci. 1995, 15, 5346–5359. [Google Scholar] [CrossRef] [PubMed]
- Zeng, M.; Wang, L.; Cheng, B.; Qi, G.; He, J.; Xu, Z.; Han, T.; Liu, C.; Wang, Y. Transcutaneous Spinal Cord Direct-Current Stimulation Modulates Functional Activity and Integration in Idiopathic Restless Legs Syndrome. Front. Neurosci. 2020, 14, 873. [Google Scholar] [CrossRef]
- Bhadra, N.; Kilgore, K.L. Direct Current Electrical Conduction Block of Peripheral Nerve. IEEE Trans. Neural Syst. Rehabil. Eng. 2004, 12, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Schweizer, L.; Meyer-Frießem, C.H.; Zahn, P.K.; Tegenthoff, M.; Schmidt-Wilcke, T. Transcutaneous Spinal Direct Current Stimulation Alters Resting-State Functional Connectivity. Brain Connect. 2017, 7, 357–365. [Google Scholar] [CrossRef]
- Schweizer, L.M.; Zahn, P.K.; Pogatzki-Zahn, E.M.; Magerl, W.; Tegenthoff, M.; Meyer-Frießem, C.H. Influence of Transcutaneous Spinal Stimulation on Human LTP-like Pain Amplification. A Randomized, Double-Blind Study in Volunteers. Clin. Neurophysiol. 2017, 128, 1413–1420. [Google Scholar] [CrossRef]
- Bocci, T.; De Carolis, G.; Paroli, M.; Barloscio, D.; Parenti, L.; Tollapi, L.; Valeriani, M.; Sartucci, F. Neurophysiological Comparison Among Tonic, High Frequency, and Burst Spinal Cord Stimulation: Novel Insights Into Spinal and Brain Mechanisms of Action. Neuromodul. Technol. Neural Interface 2018, 21, 480–488. [Google Scholar] [CrossRef]
- De Ridder, D.; Vanneste, S. Burst and Tonic Spinal Cord Stimulation: Different and Common Brain Mechanisms. Neuromodul. J. Int. Neuromodul. Soc. 2016, 19, 47–59. [Google Scholar] [CrossRef]
- Aguilar, J.; Pulecchi, F.; Dilena, R.; Oliviero, A.; Priori, A.; Foffani, G. Spinal Direct Current Stimulation Modulates the Activity of Gracile Nucleus and Primary Somatosensory Cortex in Anaesthetized Rats. J. Physiol. 2011, 589, 4981–4996. [Google Scholar] [CrossRef]
- Ahmed, Z. Effects of Cathodal Trans-Spinal Direct Current Stimulation on Lower Urinary Tract Function in Normal and Spinal Cord Injury Mice with Overactive Bladder. J. Neural Eng. 2017, 14, 056002. [Google Scholar] [CrossRef]
- Ahmed, Z. Electrophysiological Characterization of Spino-Sciatic and Cortico-Sciatic Associative Plasticity: Modulation by Trans-Spinal Direct Current and Effects on Recovery after Spinal Cord Injury in Mice. J. Neurosci. 2013, 33, 4935. [Google Scholar] [CrossRef]
- Zareen, N.; Shinozaki, M.; Ryan, D.; Alexander, H.; Amer, A.; Truong, D.Q.; Khadka, N.; Sarkar, A.; Naeem, S.; Bikson, M.; et al. Motor Cortex and Spinal Cord Neuromodulation Promote Corticospinal Tract Axonal Outgrowth and Motor Recovery after Cervical Contusion Spinal Cord Injury. Exp. Neurol. 2017, 297, 179–189. [Google Scholar] [CrossRef]
- Yang, Q.; Ramamurthy, A.; Lall, S.; Santos, J.; Ratnadurai-Giridharan, S.; Zareen, N.; Alexander, H.; Ryan, D.; Martin, J.H.; Carmel, J.B. Independent Replication of Motor Cortex and Cervical Spinal Cord Electrical Stimulation to Promote Forelimb Motor Function after Spinal Cord Injury in Rats. Exp. Neurol. 2019, 320, 112962. [Google Scholar] [CrossRef]
- Elbasiouny, S.M.; Moroz, D.; Bakr, M.M.; Mushahwar, V.K. Management of Spasticity After Spinal Cord Injury: Current Techniques and Future Directions. Neurorehabilit. Neural Repair 2010, 24, 23. [Google Scholar] [CrossRef] [PubMed]
- Mekhael, W.; Begum, S.; Samaddar, S.; Hassan, M.; Toruno, P.; Ahmed, M.; Gorin, A.; Maisano, M.; Ayad, M.; Ahmed, Z. Repeated Anodal Trans-Spinal Direct Current Stimulation Results in Long-Term Reduction of Spasticity in Mice with Spinal Cord Injury. J. Physiol. 2019, 597, 2201–2223. [Google Scholar] [CrossRef]
- Ahmed, Z.; Wieraszko, A. Trans-Spinal Direct Current Enhances Corticospinal Output and Stimulation-Evoked Release of Glutamate Analog, D-2,3-3H-Aspartic Acid. J. Appl. Physiol. 2012, 112, 1576–1592. [Google Scholar] [CrossRef] [PubMed]
- Lodge, D.; Anis, N.A. Effects of Ketamine and Three Other Anaesthetics on Spinal Reflexes and Inhibitions in the Cat. Br. J. Anaesth. 1984, 56, 1143–1151. [Google Scholar] [CrossRef]
- Zandieh, S.; Hopf, R.; Redl, H.; Schlag, M.G. The Effect of Ketamine/Xylazine Anesthesia on Sensory and Motor Evoked Potentials in the Rat. Spinal Cord 2002, 41, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Liebetanz, D.; Koch, R.; Mayenfels, S.; König, F.; Paulus, W.; Nitsche, M.A. Safety Limits of Cathodal Transcranial Direct Current Stimulation in Rats. Clin. Neurophysiol. 2009, 120, 1161–1167. [Google Scholar] [CrossRef]
- Ranger, M.R.B.; Irwin, G.J.; Bunbury, K.M.; Peutrell, J.M. Changing Body Position Alters the Location of the Spinal Cord within the Vertebral Canal: A Magnetic Resonance Imaging Study. Br. J. Anaesth. 2008, 101, 804–809. [Google Scholar] [CrossRef]
- Perrotta, A.; Bolla, M.; Anastasio, M.G.; Serrao, M.; Sandrini, G.; Pierelli, F. Modulation of Temporal Summation Threshold of the Nociceptive Withdrawal Reflex by Transcutaneous Spinal Direct Current Stimulation in Humans. Clin. Neurophysiol. 2016, 127, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Stagg, C.J.; Antal, A.; Nitsche, M.A. Physiology of Transcranial Direct Current Stimulation. J. ECT 2018, 34, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Paget-Blanc, A.; Chang, J.L.; Saul, M.; Lin, R.; Ahmed, Z.; Volpe, B.T. Non-Invasive Treatment of Patients with Upper Extremity Spasticity Following Stroke Using Paired Trans-Spinal and Peripheral Direct Current Stimulation. Bioelectron. Med. 2019, 5, 11. [Google Scholar] [CrossRef]
- Cash, R.F.H.; Udupa, K.; Gunraj, C.A.; Mazzella, F.; Daskalakis, Z.J.; Wong, A.H.C.; Kennedy, J.L.; Chen, R. Influence of BDNF Val66Met Polymorphism on Excitatory-Inhibitory Balance and Plasticity in Human Motor Cortex. Clin. Neurophysiol. Off. J. Int. Fed. Clin. Neurophysiol. 2021, 132, 2827–2839. [Google Scholar] [CrossRef] [PubMed]
- Cheeran, B.; Talelli, P.; Mori, F.; Koch, G.; Suppa, A.; Edwards, M.; Houlden, H.; Bhatia, K.; Greenwood, R.; Rothwell, J.C. A Common Polymorphism in the Brain-Derived Neurotrophic Factor Gene (BDNF) Modulates Human Cortical Plasticity and the Response to RTMS. J. Physiol. 2008, 586, 5717–5725. [Google Scholar] [CrossRef]
- Cirillo, J.; Hughes, J.; Ridding, M.; Thomas, P.Q.; Semmler, J.G. Differential Modulation of Motor Cortex Excitability in BDNF Met Allele Carriers Following Experimentally Induced and Use-Dependent Plasticity. Eur. J. Neurosci. 2012, 36, 2640–2649. [Google Scholar] [CrossRef]
- Dubbioso, R.; Pellegrino, G.; Ranieri, F.; Di Pino, G.; Capone, F.; Dileone, M.; Iodice, R.; Ruggiero, L.; Tozza, S.; Uncini, A.; et al. BDNF Polymorphism and Interhemispheric Balance of Motor Cortex Excitability: A Preliminary Study. J. Neurophysiol. 2022, 127, 204–212. [Google Scholar] [CrossRef]
- Puri, R.; Hinder, M.R.; Fujiyama, H.; Gomez, R.; Carson, R.G.; Summers, J.J. Duration-Dependent Effects of the BDNF Val66Met Polymorphism on Anodal TDCS Induced Motor Cortex Plasticity in Older Adults: A Group and Individual Perspective. Front. Aging Neurosci. 2015, 7, 107. [Google Scholar] [CrossRef]
- Lamy, J.-C.; Boakye, M. BDNF Val66Met Polymorphism Alters Spinal DC Stimulation-Induced Plasticity in Humans. J. Neurophysiol. 2013, 110, 109–116. [Google Scholar] [CrossRef]
- Manto, M.; Argyropoulos, G.P.D.; Bocci, T.; Celnik, P.A.; Corben, L.A.; Guidetti, M.; Koch, G.; Priori, A.; Rothwell, J.C.; Sadnicka, A.; et al. Consensus Paper: Novel Directions and Next Steps of Non-Invasive Brain Stimulation of the Cerebellum in Health and Disease. Cerebellum 2021, 21, 1092–1122. [Google Scholar] [CrossRef]
- Schuman, C.D.; Kulkarni, S.R.; Parsa, M.; Mitchell, J.P.; Date, P.; Kay, B. Opportunities for Neuromorphic Computing Algorithms and Applications. Nat. Comput. Sci 2022, 2, 10–19. [Google Scholar] [CrossRef]
- Schuman, C.D.; Potok, T.E.; Patton, R.M.; Birdwell, J.D.; Dean, M.E.; Rose, G.S.; Plank, J.S. A Survey of Neuromorphic Computing and Neural Networks in Hardware. arXiv 2017, arXiv:1705.06963. [Google Scholar]
- Sala, G.; Bocci, T.; Borzì, V.; Parazzini, M.; Priori, A.; Ferrarese, C. Direct Current Stimulation Enhances Neuronal Alpha-Synuclein Degradation in Vitro. Sci. Rep. 2021, 11, 2197. [Google Scholar] [CrossRef]
- Pelletier, S.J.; Cicchetti, F. Cellular and Molecular Mechanisms of Action of Transcranial Direct Current Stimulation: Evidence from In Vitro and In Vivo Models. Int. J. Neuropsychopharmacol. 2015, 18, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Silva, S.P.; Martins, O.G.; Medeiros, L.F.; Crespo, P.C.; Do Couto, C.A.T.; De Freitas, J.S.; De Souza, A.; Morastico, A.; Cruz, L.A.X.; Sanches, P.R.S.; et al. Evidence of Anti-Inflammatory Effect of Transcranial Direct Current Stimulation in a CFA-Induced Chronic Inflammatory Pain Model in Wistar Rats. Neuroimmunomodulation 2022, 29, 500–514. [Google Scholar] [CrossRef] [PubMed]
- Callai, E.M.M.; Zin, L.E.F.; Catarina, L.S.; Ponzoni, D.; Gonçalves, C.A.S.; Vizuete, A.F.K.; Cougo, M.C.; Boff, J.; Puricelli, E.; Fernandes, E.K.; et al. Evaluation of the Immediate Effects of a Single Transcranial Direct Current Stimulation Session on Astrocyte Activation, Inflammatory Response, and Pain Threshold in Naïve Rats. Behav. Brain Res. 2022, 428, 113880. [Google Scholar] [CrossRef] [PubMed]
- Guidetti, M.; Bertini, A.; Pirone, F.; Sala, G.; Signorelli, P.; Ferrarese, C.; Priori, A.; Bocci, T. Neuroprotection and Non-Invasive Brain Stimulation: Facts or Fiction? Int. J. Mol. Sci. 2022, 23, 13775. [Google Scholar] [CrossRef] [PubMed]
- Komine, O.; Yamanaka, K. Neuroinflammation in Motor Neuron Disease. Nagoya J. Med. Sci. 2015, 77, 537. [Google Scholar] [PubMed]
- Cristofani, R.; Crippa, V.; Cicardi, M.E.; Tedesco, B.; Ferrari, V.; Chierichetti, M.; Casarotto, E.; Piccolella, M.; Messi, E.; Galbiati, M.; et al. A Crucial Role for the Protein Quality Control System in Motor Neuron Diseases. Front. Aging Neurosci. 2020, 12, 191. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guidetti, M.; Giannoni-Luza, S.; Bocci, T.; Pacheco-Barrios, K.; Bianchi, A.M.; Parazzini, M.; Ionta, S.; Ferrucci, R.; Maiorana, N.V.; Verde, F.; et al. Modeling Electric Fields in Transcutaneous Spinal Direct Current Stimulation: A Clinical Perspective. Biomedicines 2023, 11, 1283. https://doi.org/10.3390/biomedicines11051283
Guidetti M, Giannoni-Luza S, Bocci T, Pacheco-Barrios K, Bianchi AM, Parazzini M, Ionta S, Ferrucci R, Maiorana NV, Verde F, et al. Modeling Electric Fields in Transcutaneous Spinal Direct Current Stimulation: A Clinical Perspective. Biomedicines. 2023; 11(5):1283. https://doi.org/10.3390/biomedicines11051283
Chicago/Turabian StyleGuidetti, Matteo, Stefano Giannoni-Luza, Tommaso Bocci, Kevin Pacheco-Barrios, Anna Maria Bianchi, Marta Parazzini, Silvio Ionta, Roberta Ferrucci, Natale Vincenzo Maiorana, Federico Verde, and et al. 2023. "Modeling Electric Fields in Transcutaneous Spinal Direct Current Stimulation: A Clinical Perspective" Biomedicines 11, no. 5: 1283. https://doi.org/10.3390/biomedicines11051283
APA StyleGuidetti, M., Giannoni-Luza, S., Bocci, T., Pacheco-Barrios, K., Bianchi, A. M., Parazzini, M., Ionta, S., Ferrucci, R., Maiorana, N. V., Verde, F., Ticozzi, N., Silani, V., & Priori, A. (2023). Modeling Electric Fields in Transcutaneous Spinal Direct Current Stimulation: A Clinical Perspective. Biomedicines, 11(5), 1283. https://doi.org/10.3390/biomedicines11051283










