Anthropometric Measurements and Admission Parameters as Predictors of Acute Respiratory Distress Syndrome in Hospitalized COVID-19 Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
- (I)
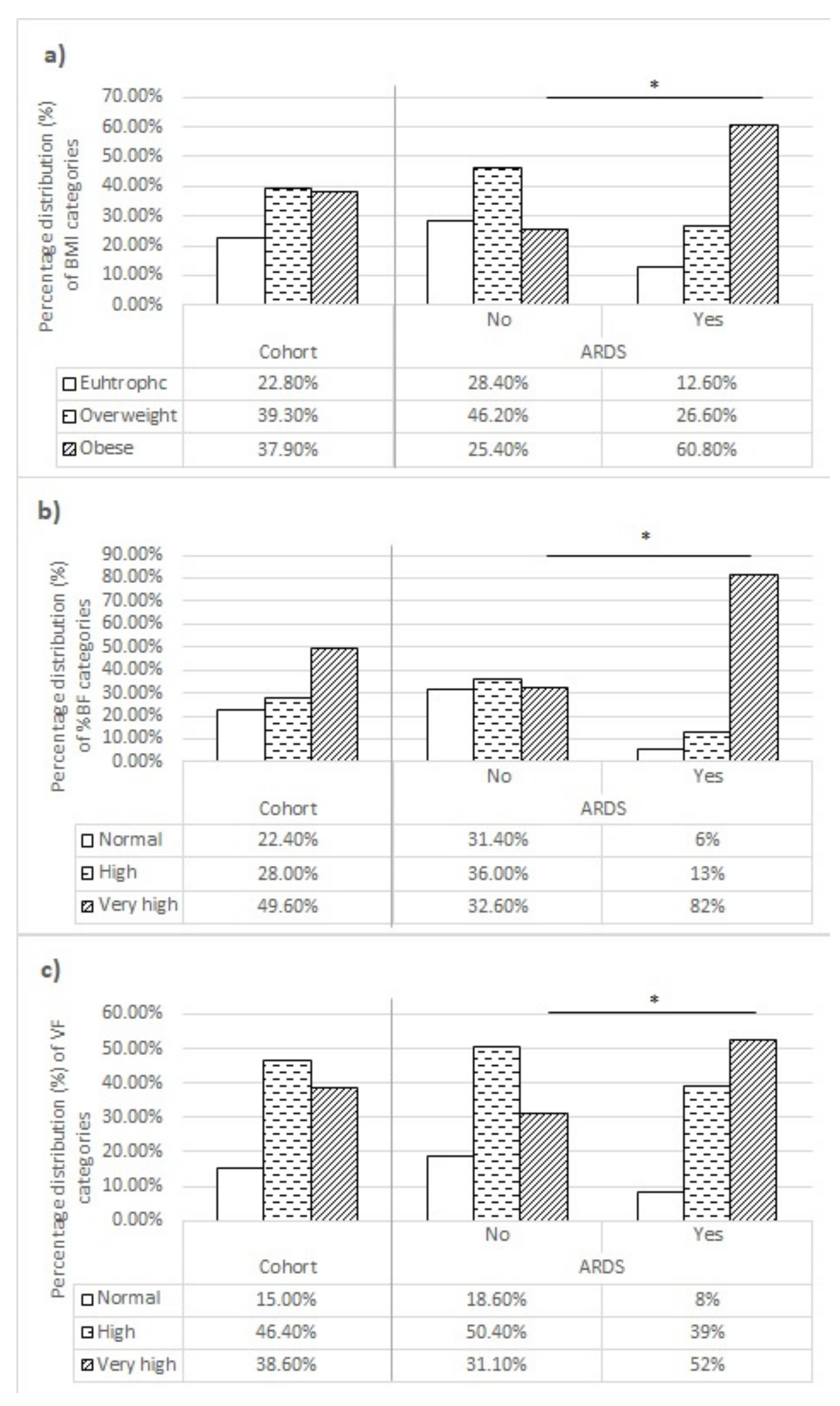
- BMI, calculated using the formula BMI [kg/m2] = BM [kg]/BH2 [m2], where BM is the body mass expressed in kg (with 0.1 kg precision), and BH is body height expressed in m (with 0.01 m precision). According to BMI values, patients were categorized as (I) underweight < 18.5 kg/m2, (II) normal weight 18.6–24.9 kg/m2, (III) overweight 25–29.9 kg/m2, (IV) class 1 obesity 30–34.9 kg/m2, (V) class 2 obesity 35–39.9 kg/m2, or (VI) class 3 obesity > 40 kg/m2 [22].
- (II)
- Body fat percentage (BF%), expressed as a percentage of the total mass (with 0.1% precision). According to BF% values, regarding age and sex, patients were categorized as (I) low BF%, (II) normal BF%, (III) high BF%, or (IV) very high BF% (age- and sex-adjusted cutoff values are presented in Table 1) [23].
- (III)
- Visceral fat (VF) level, according to which patients were categorized as (I) normal (1–9), (II) high (10–14), or (III) very high (≥15) [24].
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rahman, S.; Montero, M.T.V.; Rowe, K.; Kirton, R.; Kunik, F., Jr. Epidemiology, pathogenesis, clinical presentations, diagnosis and treatment of COVID-19: A review of current evidence. Expert Rev. Clin. Pharmacol. 2021, 14, 601–621. [Google Scholar] [CrossRef] [PubMed]
- Knoll, R.; Schultze, J.L.; Schulte-Schrepping, J. Monocytes and Macrophages in COVID-19. Front. Immunol. 2021, 12, 720109. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Gallo Marin, B.; Aghagoli, G.; Lavine, K.; Yang, L.; Siff, E.J.; Chiang, S.S.; Salazar-Mather, T.P.; Dumenco, L.; Savaria, M.C.; Aung, S.N.; et al. Predictors of COVID-19 severity: A literature review. Rev. Med. Virol. 2021, 31, 1–10. [Google Scholar] [CrossRef]
- Masvekar, R.R.; Kosa, P.; Jin, K.; Dobbs, K.; Stack, M.A.; Castagnoli, R.; Quaresima, V.; Su, H.C.; Imberti, L.; Notarangelo, L.D.; et al. Prognostic value of serum/plasma neurofilament light chain for COVID-19-associated mortality. Ann. Clin. Transl. Neurol. 2022, 9, 622–632. [Google Scholar] [CrossRef]
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966. [Google Scholar] [CrossRef]
- Xu, W.; Sun, N.N.; Gao, H.N.; Chen, Z.Y.; Yang, Y.; Ju, B.; Tang, L.L. Risk factors analysis of COVID-19 patients with ARDS and prediction based on machine learning. Sci. Rep. 2021, 11, 2933. [Google Scholar] [CrossRef]
- Gujski, M.; Jankowski, M.; Rabczenko, D.; Gorynski, P.; Juszczyk, G. The Prevalence of Acute Respiratory Distress Syndrome (ARDS) and Outcomes in Hospitalized Patients with COVID-19-A Study Based on Data from the Polish National Hospital Register. Viruses 2022, 14, 76. [Google Scholar] [CrossRef]
- Mesas, A.E.; Cavero-Redondo, I.; Alvarez-Bueno, C.; Sarria Cabrera, M.A.; Maffei de Andrade, S.; Sequi-Dominguez, I.; Martinez-Vizcaino, V. Predictors of in-hospital COVID-19 mortality: A comprehensive systematic review and meta-analysis exploring differences by age, sex and health conditions. PLoS ONE 2020, 15, e0241742. [Google Scholar] [CrossRef]
- Statsenko, Y.; Al Zahmi, F.; Habuza, T.; Gorkom, K.N.; Zaki, N. Prediction of COVID-19 severity using laboratory findings on admission: Informative values, thresholds, ML model performance. BMJ Open 2021, 11, e044500. [Google Scholar] [CrossRef]
- Popkin, B.M.; Du, S.; Green, W.D.; Beck, M.A.; Algaith, T.; Herbst, C.H.; Alsukait, R.F.; Alluhidan, M.; Alazemi, N.; Shekar, M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 2020, 21, e13128. [Google Scholar] [CrossRef]
- Pranata, R.; Lim, M.A.; Yonas, E.; Vania, R.; Lukito, A.A.; Siswanto, B.B.; Meyer, M. Body mass index and outcome in patients with COVID-19: A dose-response meta-analysis. Diabetes Metab. 2021, 47, 101178. [Google Scholar] [CrossRef]
- Chu, Y.; Yang, J.; Shi, J.; Zhang, P.; Wang, X. Obesity is associated with increased severity of disease in COVID-19 pneumonia: A systematic review and meta-analysis. Eur. J. Med. Res. 2020, 25, 64. [Google Scholar] [CrossRef]
- Yang, J.; Hu, J.; Zhu, C. Obesity aggravates COVID-19: A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 257–261. [Google Scholar] [CrossRef]
- Sattar, N.; McInnes, I.B.; McMurray, J.J.V. Obesity Is a Risk Factor for Severe COVID-19 Infection: Multiple Potential Mechanisms. Circulation 2020, 142, 4–6. [Google Scholar] [CrossRef]
- Kwok, S.; Adam, S.; Ho, J.H.; Iqbal, Z.; Turkington, P.; Razvi, S.; Le Roux, C.W.; Soran, H.; Syed, A.A. Obesity: A critical risk factor in the COVID-19 pandemic. Clin. Obes. 2020, 10, e12403. [Google Scholar] [CrossRef]
- Watanabe, M.; Caruso, D.; Tuccinardi, D.; Risi, R.; Zerunian, M.; Polici, M.; Pucciarelli, F.; Tarallo, M.; Strigari, L.; Manfrini, S.; et al. Visceral fat shows the strongest association with the need of intensive care in patients with COVID-19. Metabolism 2020, 111, 154319. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 Clinical Management: Living Guidance; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Battaglini, D.; Fazzini, B.; Silva, P.L.; Cruz, F.F.; Ball, L.; Robba, C.; Rocco, P.R.M.; Pelosi, P. Challenges in ARDS Definition, Management, and Identification of Effective Personalized Therapies. J. Clin. Med. 2023, 12, 1381. [Google Scholar] [CrossRef]
- Force, A.D.T.; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [CrossRef]
- Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation. In World Health Organization Technical Report Series; World Health Organization: Geneva, Switzerland, 2000; Volume 894, p. 252. [Google Scholar]
- Gallagher, D.; Heymsfield, S.B.; Heo, M.; Jebb, S.A.; Murgatroyd, P.R.; Sakamoto, Y. Healthy percentage body fat ranges: An approach for developing guidelines based on body mass index. Am. J. Clin. Nutr. 2000, 72, 694–701. [Google Scholar] [CrossRef] [PubMed]
- TANITA-Medical Product Guide; TANITA: Arlington Heights, IL, USA, 2021.
- Dreher, M.; Kersten, A.; Bickenbach, J.; Balfanz, P.; Hartmann, B.; Cornelissen, C.; Daher, A.; Stohr, R.; Kleines, M.; Lemmen, S.W.; et al. The Characteristics of 50 Hospitalized COVID-19 Patients with and Without ARDS. Dtsch. Arztebl. Int. 2020, 117, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Grujic, V.; Dragnic, N.; Radic, I.; Harhaji, S.; Susnjevic, S. Overweight and obesity among adults in Serbia: Results from the National Health Survey. Eat. Weight Disord. 2010, 15, e34–e42. [Google Scholar] [CrossRef] [PubMed]
- Fernandez Crespo, S.; Perez-Matute, P.; Iniguez Martinez, M.; Fernandez-Villa, T.; Dominguez-Garrido, E.; Oteo, J.A.; Marcos-Delgado, A.; Flores, C.; Riancho, J.A.; Rojas-Martinez, A.; et al. Severity of COVID-19 attributable to obesity according to BMI and CUN-BAE. Semergen 2022, 48, 101840. [Google Scholar] [CrossRef] [PubMed]
- Ogata, H.; Mori, M.; Jingushi, Y.; Matsuzaki, H.; Katahira, K.; Ishimatsu, A.; Enokizu-Ogawa, A.; Taguchi, K.; Moriwaki, A.; Yoshida, M. Impact of visceral fat on the prognosis of coronavirus disease 2019: An observational cohort study. BMC Infect. Dis. 2021, 21, 1240. [Google Scholar] [CrossRef]
- Zhang, X.; Lewis, A.M.; Moley, J.R.; Brestoff, J.R. A systematic review and meta-analysis of obesity and COVID-19 outcomes. Sci. Rep. 2021, 11, 7193. [Google Scholar] [CrossRef]
- Favre, G.; Legueult, K.; Pradier, C.; Raffaelli, C.; Ichai, C.; Iannelli, A.; Redheuil, A.; Lucidarme, O.; Esnault, V. Visceral fat is associated to the severity of COVID-19. Metabolism 2021, 115, 154440. [Google Scholar] [CrossRef]
- Goehler, A.; Hsu, T.H.; Seiglie, J.A.; Siedner, M.J.; Lo, J.; Triant, V.; Hsu, J.; Foulkes, A.; Bassett, I.; Khorasani, R.; et al. Visceral Adiposity and Severe COVID-19 Disease: Application of an Artificial Intelligence Algorithm to Improve Clinical Risk Prediction. Open Forum Infect. Dis. 2021, 8, ofab275. [Google Scholar] [CrossRef]
- Bunnell, K.M.; Thaweethai, T.; Buckless, C.; Shinnick, D.J.; Torriani, M.; Foulkes, A.S.; Bredella, M.A. Body composition predictors of outcome in patients with COVID-19. Int. J. Obes. 2021, 45, 2238–2243. [Google Scholar] [CrossRef]
- Nikolic, M.; Simovic, S.; Novkovic, L.; Jokovic, V.; Djokovic, D.; Muric, N.; Bazic Sretenovic, D.; Jovanovic, J.; Pantic, K.; Cekerevac, I. Obesity and sleep apnea as a significant comorbidities in COVID-19—A case report. Obes. Res. Clin. Pract. 2021, 15, 281–284. [Google Scholar] [CrossRef]
- Chait, A.; den Hartigh, L.J. Adipose Tissue Distribution, Inflammation and Its Metabolic Consequences, Including Diabetes and Cardiovascular Disease. Front. Cardiovasc. Med. 2020, 7, 22. [Google Scholar] [CrossRef]
- Chaudry, O.; Grimm, A.; Friedberger, A.; Kemmler, W.; Uder, M.; Jakob, F.; Quick, H.H.; von Stengel, S.; Engelke, K. Magnetic Resonance Imaging and Bioelectrical Impedance Analysis to Assess Visceral and Abdominal Adipose Tissue. Obesity 2020, 28, 277–283. [Google Scholar] [CrossRef]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef]
- Pijls, B.G.; Jolani, S.; Atherley, A.; Derckx, R.T.; Dijkstra, J.I.R.; Franssen, G.H.L.; Hendriks, S.; Richters, A.; Venemans-Jellema, A.; Zalpuri, S.; et al. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: A meta-analysis of 59 studies. BMJ Open 2021, 11, e044640. [Google Scholar] [CrossRef]
- Attaway, A.H.; Scheraga, R.G.; Bhimraj, A.; Biehl, M.; Hatipoglu, U. Severe covid-19 pneumonia: Pathogenesis and clinical management. BMJ 2021, 372, n436. [Google Scholar] [CrossRef]
- Sharma, G.; Volgman, A.S.; Michos, E.D. Sex Differences in Mortality From COVID-19 Pandemic: Are Men Vulnerable and Women Protected? JACC Case Rep. 2020, 2, 1407–1410. [Google Scholar] [CrossRef]
- Salah, H.M.; Mehta, J.L. Hypothesis: Sex-Related Differences in ACE2 Activity May Contribute to Higher Mortality in Men Versus Women With COVID-19. J. Cardiovasc. Pharmacol. Ther. 2021, 26, 114–118. [Google Scholar] [CrossRef]
- Jimenez-Solem, E.; Petersen, T.S.; Hansen, C.; Hansen, C.; Lioma, C.; Igel, C.; Boomsma, W.; Krause, O.; Lorenzen, S.; Selvan, R.; et al. Developing and validating COVID-19 adverse outcome risk prediction models from a bi-national European cohort of 5594 patients. Sci. Rep. 2021, 11, 3246. [Google Scholar] [CrossRef]
- Mejia, F.; Medina, C.; Cornejo, E.; Morello, E.; Vasquez, S.; Alave, J.; Schwalb, A.; Malaga, G. Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima, Peru. PLoS ONE 2020, 15, e0244171. [Google Scholar] [CrossRef]
- Ostergaard, L. SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: Consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiol. Rep. 2021, 9, e14726. [Google Scholar] [CrossRef]
- Del Valle, D.M.; Kim-Schulze, S.; Huang, H.H.; Beckmann, N.D.; Nirenberg, S.; Wang, B.; Lavin, Y.; Swartz, T.H.; Madduri, D.; Stock, A.; et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 2020, 26, 1636–1643. [Google Scholar] [CrossRef] [PubMed]
- Leisman, D.E.; Ronner, L.; Pinotti, R.; Taylor, M.D.; Sinha, P.; Calfee, C.S.; Hirayama, A.V.; Mastroiani, F.; Turtle, C.J.; Harhay, M.O.; et al. Cytokine elevation in severe and critical COVID-19: A rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes. Lancet Respir. Med. 2020, 8, 1233–1244. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.; Wang, Q.; Zhang, D.; Ding, J.; Huang, Q.; Tang, Y.Q.; Wang, Q.; Miao, H. Lymphopenia predicts disease severity of COVID-19: A descriptive and predictive study. Signal Transduct. Target Ther. 2020, 5, 33. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Ramirez, D.C.; Normand, K.; Zhaoyun, Y.; Torres-Castro, R. Long-Term Impact of COVID-19: A Systematic Review of the Literature and Meta-Analysis. Biomedicines 2021, 9, 900. [Google Scholar] [CrossRef]
- Pelosi, P.; Tonelli, R.; Torregiani, C.; Baratella, E.; Confalonieri, M.; Battaglini, D.; Marchioni, A.; Confalonieri, P.; Clini, E.; Salton, F.; et al. Different Methods to Improve the Monitoring of Noninvasive Respiratory Support of Patients with Severe Pneumonia/ARDS Due to COVID-19: An Update. J. Clin. Med. 2022, 11, 1704. [Google Scholar] [CrossRef]
- Ambrosino, P.; Lanzillo, A.; Maniscalco, M. COVID-19 and Post-Acute COVID-19 Syndrome: From Pathophysiology to Novel Translational Applications. Biomedicines 2021, 10, 47. [Google Scholar] [CrossRef]
- Marini, E.; Buffa, R.; Contreras, M.; Magris, M.; Hidalgo, G.; Sanchez, W.; Ortiz, V.; Urbaez, M.; Cabras, S.; Blaser, M.J.; et al. Effect of influenza-induced fever on human bioimpedance values. PLoS ONE 2015, 10, e0125301. [Google Scholar] [CrossRef]
- Xu, Z.; Liu, Y.; Yan, C.; Yang, R.; Xu, L.; Guo, Z.; Yu, A.; Cheng, X.; Ma, L.; Hu, C.; et al. Measurement of visceral fat and abdominal obesity by single-frequency bioelectrical impedance and CT: A cross-sectional study. BMJ Open 2021, 11, e048221. [Google Scholar] [CrossRef]

| Sex | Age (Years) | BF% Categories | |||
|---|---|---|---|---|---|
| Low | Normal | High (Overweight) | Very High (Obesity) | ||
| Female | 20–39 | <21% | 21–32.9% | 33–39.5% | >39.5% |
| 40–59 | <23% | 23–33.9% | 34–40% | >40% | |
| ≥60 | 24% | 24–35.9% | 36–41.5% | >41.5% | |
| Male | 20–39 | <7% | 7–19.9% | 20–25% | >25% |
| 40–59 | <10.5% | 10.5–21.9% | 22–27.5% | >27.5% | |
| ≥60 | <12% | 12–24.9% | 25–30% | >30% | |
| Cohort Characteristics | Frequency (Number of Cases) or Median Value (with IQR) | p-Value | |||
|---|---|---|---|---|---|
| Cohort | No ARDS | ARDS | |||
| Age [years] | 68.0 (IQR 17.0) | 68.5 (IQR 16.0) | 66.0 (IQR 19.0) | 0.006 * | |
| Sex | Male | 62.9% (n = 256) | 68.9% (n = 182) | 51.7% (n = 74) | 0.001 * |
| Female | 37.1% (n = 151) | 31.1% (n = 82) | 48.3% (n = 69) | ||
| COMORBIDITIES | |||||
| Arterial hypertension | 68.1% (n = 277) | 70.5% (n = 186) | 63.6% (n = 91) | 0.182 | |
| Diabetes mellitus | 26.5% (n = 108) | 25.4% (n = 67) | 28.7% (n = 41) | 0.482 | |
| Chronic kidney disease | 14.7% (n = 60) | 14.8% (n = 39) | 14.7% (n = 21) | 1.000 | |
| Neurological condition 1 | 3.4% (n = 14) | 3.8% (n = 10) | 2.8% (n = 4) | 0.778 | |
| Previous myocardial infarction | 3.9% (n = 16) | 3.8% (n = 10) | 4.2% (n = 6) | 0.797 | |
| Malignancy | 6.1% (n = 25) | 7.2% (n = 19) | 4.2% (n = 6) | 0.283 | |
| Obstructive lung disease 2 | 3.2% (n = 13) | 3.4% (n = 9) | 2.8% (n = 4) | 1.000 | |
| Charlson Comorbidity Index | 3.0 (IQR 2.0) | 3.0 (IQR 2.0) | 3.0 (IQR 3.0) | 0.052 | |
| DISEASE COURSE AND OUTCOME | |||||
| Time from disease onset to hospital admission [days] | 6.0 (IQR 6.0) | 7.0 (IQR 7.0) | 6.0 (IQR 5.0) | 0.003 * | |
| ARDS development | 35.1% (n = 143) | / | / | / | |
| Mortality | 17.4% (n = 71) | 9% (n = 24) | 44.1% (n = 63) | <0.001 * | |
| Hospital stay [days] | 17.0 (IQR 11.0) | 14.5 (IQR 9.75) | 21.0 (IQR 14.0) | <0.001 * | |
| Oxygen support requirement on admission | 92.9% (n = 378) | 90.5% (n = 239) | 97.2% (n = 139) | 0.014 * | |
| Blood Gas and Laboratory Analysis | Median Values (IQR) | p-Value | ||
|---|---|---|---|---|
| Cohort | No ARDS | ARDS | ||
| PaO2 [kPa] | 6.9 (IQR 1.4) | 14.5 (IQR 9.75) | 6.4 (IQR 1.2) | <0.001 * |
| SaO2 [%] | 88 (IQR 6) | 89 (IQR 5) | 86 (IQR 5) | <0.001 * |
| WBC [109/L] | 8.2 (IQR 4.8) | 8.2 (IQR 4.5) | 8.3 (IQR 6.6) | 0.751 |
| Granulocyte count [109/L] | 6.9 (IQR 4.9) | 6.5 (IQR 4.85) | 7.4 (IQR 4.1) | 0.710 |
| Granulocytes [%] | 84.2 (IQR 11.7) | 83 (IQR 12.2) | 85.9 (IQR 10.8) | 0.001 * |
| Lymphocyte count [109/L] | 0.7 (IQR 0.5) | 0.73 (IQR 0.57) | 0.69 (IQR 0.43) | 0.009 * |
| Lymphocytes [%] | 9.1 (IQR 8.5) | 9.5 (IQR 8.6) | 8.5 (IQR 6.4) | 0.036 * |
| RBC [1012/L] | 4.5 (IQR 0.7) | 4.48 (IQR 0.81) | 4.47 (IQR 0.69) | 0.968 |
| HGB [g/L] | 134 (IQR 21) | 134.5 (IQR 21.75) | 133 (IQR 21) | 0.081 |
| PLT [109/L] | 201 (IQR 113) | 203.5 (IQR 108) | 199 (IQR 115) | 0.771 |
| INR | 1.08 (IQR 0.18) | 1.08 (IQR 0.16) | 1.07 (IQR 0.19) | 0.079 |
| aPTT [s] | 31.4 (IQR 6.85) | 31.5 (IQR 7) | 33.3 (IQR 6.3) | 0.917 |
| Fibrinogen [g/L] | 6.5 (IQR 2.15) | 6.26 (IQR 2.06) | 6.22 (IQR 2.09) | 0.485 |
| D-dimer [ug/mL] | 0.93 (IQR 0.97) | 0.97 (IQR 1.25) | 0.85 (IQR 0.76) | 0.159 |
| Albumin [g/L] | 36 (IQR 4) | 36 (IQR 4) | 36 (IQR 5) | 0.337 |
| AST [IU/L] | 42 (IQR 35) | 41 (IQR 31) | 43 (IQR 41) | 0.271 |
| ALT [IU/L] | 36 (IQR 36) | 36 (IQR 38.25) | 41 (IQR 40) | 0.830 |
| GGT [IU/L] | 41 (IQR 65) | 42 (IQR 65) | 41 (IQR 64) | 0.819 |
| BUN [mmol/L] | 7.8 (IQR 5.3) | 8.4 (IQR 5.5) | 7.1 (IQR 4.2) | 0.054 |
| Creatinine [mmol/L] | 92 (IQR 41) | 91 (IQR 42) | 94 (IQR 40) | 0.216 |
| LDH [U/L] | 773 (IQR 382) | 702 (IQR 388) | 890 (IQR 242) | <0.001 * |
| Ferritin [ug/L] | 838 (IQR 745) | 815 (IQR 792) | 877 (IQR 746) | 0.335 |
| CK [U/L] | 107(IQR 166) | 91.5 (IQR 152.75) | 156 (IQR 179) | 0.001 * |
| CKMB [U/L] | 18 (IQR 10) | 18 (IQR 9) | 18 (IQR 11) | 0.386 |
| CRP [mg/L] | 99 (IQR 96.1) | 96.6 (IQR 92.5) | 108.7 (IQR 99.8) | 0.009 * |
| PCT [ng/mL] | 0.11 (IQR 0.18) | 0.1 (IQR 0.17) | 0.114 (IQR 0.18) | 0.413 |
| cTnI [ng/mL] | 0.0038 (IQR 0.014) | 0.00145 (IQR 0.0145) | 0.006 (IQR 0.0127) | 0.637 |
| pro-BNP [pg/mL] | 559 (IQR 880) | 604 (IQR 959) | 389 (IQR 895) | 0.066 |
| IL-6 [pg/mL] | 58.7 (IQR 97) | 47.4 (IQR 89.15) | 89.8 (IQR 119.3) | <0.001 * |
| Variable | Frequency of ARDS | Crude OR | Adjusted OR | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |||
| PaO2 [kPa] | ≥6.85 | 20.5% | 1 | / | Excluded for multicollinearity ** | |
| <6.85 | 52.4% | 4.282 (2.770–6.619) | <0.001 * | |||
| SaO2 [kPa] | ≥87.5 | 18.9% | 1 | / | 1 | / |
| <87.5 | 56.9% | 5.670 (3.635–8.844) | <0.001 * | 5.120 (2.758–9.505) | <0.001 * | |
| Lymphocyte count [109/L] | ≥1.20 | 14.9% | 1 | / | 1 | / |
| <1.20 | 39.1% | 3.662 (1.807–7.422) | <0.001 * | 2.880 (1.218–6.809) | 0.016 * | |
| LDH [U/L] | ≤793.5 | 24.8% | 1 | / | 1 | / |
| >793.5 | 49.1% | 2.934 (1.898–4.538) | <0.001 * | 1.078 (0.580–2.002) | 0.812 | |
| CK [U/L] | ≤171 | 29.8% | 1 | / | 1 | / |
| >171 | 45.0% | 1.927 (1.257–2.955) | 0.003 * | 1.911 (0.978–3.733) | 0.058 | |
| CRP [mg/L] | ≤108.5 | 30.6% | 1 | / | 1 | / |
| >108.5 | 40.9% | 1.572 (1.039–2.376) | 0.032 * | 1.096 (0.594–2.024) | 0.768 | |
| IL-6 [pg/mL] | ≤59.75 | 21.6% | 1 | / | 1 | / |
| >59.75 | 49.7% | 3.586 (2.327–5.525) | <0.001 * | 4.089 (2.136–7.826) | <0.001 * | |
| Age [years] | ≥68.5 | 29.8% | 1 | / | 1 | / |
| <68.5 | 39.7% | 1.554 (1.027–2.349) | 0.037 * | 1.976 (1.038–3.762) | 0.038 * | |
| Sex | Male | 28.9% | 1 | / | 1 | / |
| Female | 45.7% | 2.070 (1.361–3.147) | 0.001 * | 2.290 (1.158–4.529) | 0.017 * | |
| Need for oxygen therapy upon admission | No | 13.8% | 1 | / | Excluded for multicollinearity ** | |
| Yes | 36.8% | 3.635 (1.239–10.661) | 0.019 * | |||
| BMI | <30 | 22.1% | 1 | / | Excluded for multicollinearity ** | |
| ≥30 | 56.5% | 4.568 (2.955–7.060) | <0.001 * | |||
| BF% | Normal/High | 13.2% | 1 | / | 1 | / |
| Very high | 57.4% | 8.892 (5.439–14.538) | <0.001 * | 8.059 (3.990–16.276) | <0.001 * | |
| VF | Normal/High | 27.2% | 1 | / | 1 | / |
| Very high | 47.8% | 2.448 (1.610–3.722) | <0.001 * | 1.159 (0.566–2.372) | 0.686 | |
| Time from disease onset [days] | / | / | 0.923 (0.877–0.970) | 0.002 * | 0.941 (0.867–1.020) | 0.140 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zdravković, V.; Stevanović, Đ.; Ćićarić, N.; Zdravković, N.; Čekerevac, I.; Poskurica, M.; Simić, I.; Stojić, V.; Nikolić, T.; Marković, M.; et al. Anthropometric Measurements and Admission Parameters as Predictors of Acute Respiratory Distress Syndrome in Hospitalized COVID-19 Patients. Biomedicines 2023, 11, 1199. https://doi.org/10.3390/biomedicines11041199
Zdravković V, Stevanović Đ, Ćićarić N, Zdravković N, Čekerevac I, Poskurica M, Simić I, Stojić V, Nikolić T, Marković M, et al. Anthropometric Measurements and Admission Parameters as Predictors of Acute Respiratory Distress Syndrome in Hospitalized COVID-19 Patients. Biomedicines. 2023; 11(4):1199. https://doi.org/10.3390/biomedicines11041199
Chicago/Turabian StyleZdravković, Vladimir, Đorđe Stevanović, Neda Ćićarić, Nemanja Zdravković, Ivan Čekerevac, Mina Poskurica, Ivan Simić, Vladislava Stojić, Tomislav Nikolić, Marina Marković, and et al. 2023. "Anthropometric Measurements and Admission Parameters as Predictors of Acute Respiratory Distress Syndrome in Hospitalized COVID-19 Patients" Biomedicines 11, no. 4: 1199. https://doi.org/10.3390/biomedicines11041199
APA StyleZdravković, V., Stevanović, Đ., Ćićarić, N., Zdravković, N., Čekerevac, I., Poskurica, M., Simić, I., Stojić, V., Nikolić, T., Marković, M., Popović, M., Divjak, A., Todorović, D., & Petrović, M. (2023). Anthropometric Measurements and Admission Parameters as Predictors of Acute Respiratory Distress Syndrome in Hospitalized COVID-19 Patients. Biomedicines, 11(4), 1199. https://doi.org/10.3390/biomedicines11041199






