Urinary Oxidative Stress Biomarkers in the Diagnosis of Detrusor Overactivity in Female Patients with Stress Urinary Incontinence
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Urinary Biomarker Analysis
2.3. Quantification of 8-OHdG, 8-Isoprostane, and TAC
2.4. Quantification of Inflammatory Cytokines
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yande, S.D.; Joglekar, O.V.; Joshi, M. Role of Urodynamics in Stress Urinary Incontinence: A Critical Appraisal. J. MidLife Health 2016, 7, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Kuo, H.-C. Effect of Detrusor Function on the Therapeutic Outcome of a Suburethral Sling Procedure Using a Polypropylene Sling for Stress Urinary Incontinence in Women. Scand. J. Urol. Nephrol. 2007, 41, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Stoffel, J.T.; Smith, J.J.; Crivellaro, S.; Bresette, J.F. Mixed Incontinence: Does Preoperative Urodynamic Detrusor Overactivity Affect Postoperative Quality of Life after Pubovaginal Sling? Int. Braz. J. Urol. 2008, 34, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Kobashi, K.C.; Albo, M.E.; Dmochowski, R.R.; Ginsberg, D.A.; Goldman, H.B.; Gomelsky, A.; Kraus, S.R.; Sandhu, J.S.; Shepler, T.; Treadwell, J.R.; et al. Surgical Treatment of Female Stress Urinary Incontinence: AUA/SUFU Guideline. J. Urol. 2017, 198, 875–883. [Google Scholar] [CrossRef]
- Nager, C.W.; FitzGerald, M.; Kraus, S.R.; Chai, T.C.; Zyczynski, H.; Sirls, L.; Lemack, G.E.; Lloyd, L.K.; Litman, H.J.; Stoddard, A.M.; et al. Urodynamic Measures Do Not Predict Stress Continence Outcomes after Surgery for Stress Urinary Incontinence in Selected Women. J. Urol. 2008, 179, 1470–1474. [Google Scholar] [CrossRef]
- Nager, C.W.; Sirls, L.; Litman, H.J.; Richter, H.; Nygaard, I.; Chai, T.; Kraus, S.; Zyczynski, H.; Kenton, K.; Huang, L.; et al. Baseline Urodynamic Predictors of Treatment Failure 1 Year after Mid Urethral Sling Surgery. J. Urol. 2011, 186, 597–603. [Google Scholar] [CrossRef]
- Nager, C.W.; Brubaker, L.; Litman, H.J.; Zyczynski, H.M.; Varner, R.E.; Amundsen, C.; Sirls, L.T.; Norton, P.A.; Arisco, A.M.; Chai, T.C.; et al. A Randomized Trial of Urodynamic Testing before Stress-Incontinence Surgery. N. Engl. J. Med. 2012, 366, 1987–1997. [Google Scholar] [CrossRef]
- McLennan, M.T.; Melick, C.; Bent, A.E. Urethral Instability: Clinical and Urodynamic Characteristics. Neurourol. Urodyn. 2001, 20, 653–660. [Google Scholar] [CrossRef]
- Jiang, Y.-H.; Chen, S.-F.; Kuo, H.-C. Role of Videourodynamic Study in Precision Diagnosis and Treatment for Lower Urinary Tract Dysfunction. Tzu Chi Med. J. 2020, 32, 121–130. [Google Scholar]
- Jiang, Y.-H.; Jhang, J.-F.; Hsu, Y.-H.; Ho, H.-C.; Wu, Y.-H.; Kuo, H.-C. Urine Biomarkers in ESSIC Type 2 Interstitial Cystitis/bladder Pain Syndrome and Overactive Bladder with Developing a Novel Diagnostic Algorithm. Sci. Rep. 2021, 11, 914. [Google Scholar] [CrossRef]
- D’Ancona, C.; Haylen, B.; Oelke, M.; Abranches-Monteiro, L.; Arnold, E.; Goldman, H.; Hamid, R.; Homma, Y.; Marcelissen, T.; Rademakers, K.; et al. The International Continence Society (ICS) Report on the Terminology for Adult Male Lower Urinary Tract and Pelvic Floor Symptoms and Dysfunction. Neurourol. Urodyn. 2019, 38, 433–477. [Google Scholar] [CrossRef]
- Rosier, P.F.W.M.; Schaefer, W.; Lose, G.; Goldman, H.B.; Guralnick, M.; Eustice, S.; Dickinson, T.; Hashim, H. International Continence Society Good Urodynamic Practices and Terms 2016: Urodynamics, Uroflowmetry, Cystometry, and Pressure-Flow Study. Neurourol. Urodyn. 2017, 36, 1243–1260. [Google Scholar] [CrossRef]
- Jiang, Y.-H.; Jhang, J.-F.; Ho, H.-C.; Chiou, D.-Y.; Kuo, H.-C. Urine Oxidative Stress Biomarkers as Novel Biomarkers in Interstitial Cystitis/Bladder Pain Syndrome. Biomedicines 2022, 10, 1701. [Google Scholar] [CrossRef]
- Jiang, Y.-H.; Jhang, J.-F.; Ho, H.-C.; Hsu, Y.-H.; Kuo, H.-C. Diagnostic and Prognostic Value of Urine Biomarkers among Women with Dysfunctional Voiding. Sci. Rep. 2022, 12, 1–8. [Google Scholar]
- Schaefer, W. Re: Is the Bladder a Reliable Witness for Predicting Detrusor Overactivity? H. Hashim and P. Abrams. J Urol, 175: 191–195, 2006. J. Urol. 2006, 176, 1256–1257, author reply 1256–1257. [Google Scholar] [CrossRef]
- Chu, F.M.; Dmochowski, R. Pathophysiology of Overactive Bladder. Am. J. Med. 2006, 119, 3–8. [Google Scholar] [CrossRef]
- Yokoyama, T.; Nozaki, K.; Fujita, O.; Nose, H.; Inoue, M.; Kumon, H. Role of C Afferent Fibers and Monitoring of Intravesical Resiniferatoxin Therapy for Patients with Idiopathic Detrusor Overactivity. J. Urol. 2004, 172, 596–600. [Google Scholar] [CrossRef]
- Wu, Y.-H.; Chueh, K.-S.; Chuang, S.-M.; Long, C.-Y.; Lu, J.-H.; Juan, Y.-S. Bladder Hyperactivity Induced by Oxidative Stress and Bladder Ischemia: A Review of Treatment Strategies with Antioxidants. Int. J. Mol. Sci. 2021, 22, 6014. [Google Scholar] [CrossRef]
- Charrua, A.; Cruz, C.D.; Cruz, F. 365 TRPV1 and TRPV4 Antagonists Have Synergistic Effect for Treating Bladder Overactivity in Rats. Eur. Urol. Suppl. 2012, 11, e365. [Google Scholar] [CrossRef]
- Yamaguchi, O.; Honda, K.; Nomiya, M.; Shishido, K.; Kakizaki, H.; Tanaka, H.; Yamanishi, T.; Homma, Y.; Takeda, M.; Araki, I.; et al. Defining Overactive Bladder as Hypersensitivity. Neurourol. Urodyn. 2007, 26, 904–907. [Google Scholar] [CrossRef]
- Brierley, S.M.; Goh, K.G.K.; Sullivan, M.J.; Moore, K.H.; Ulett, G.C.; Grundy, L. Innate Immune Response to Bacterial Urinary Tract Infection Sensitises High-Threshold Bladder Afferents and Recruits Silent Nociceptors. Pain 2020, 161, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Graille, M.; Wild, P.; Sauvain, J.-J.; Hemmendinger, M.; Canu, I.G.; Hopf, N.B. Urinary 8-Isoprostane as a Biomarker for Oxidative Stress. A Systematic Review and Meta-Analysis. Toxicol. Lett. 2020, 328, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Molnár, P.J.; Dér, B.; Borsodi, K.; Balla, H.; Borbás, Z.; Molnár, K.; Ruisanchez, É.; Kenessey, I.; Horváth, A.; Keszthelyi, A.; et al. Isoprostanes Evoke Contraction of the Murine and Human Detrusor Muscle via Activation of the Thromboxane Prostanoid TP Receptor and Rho Kinase. Am. J. Physiol. Ren. Physiol. 2021, 320, F537–F547. [Google Scholar] [CrossRef] [PubMed]
- Il’yasova, D.; Scarbrough, P.; Spasojevic, I. Urinary Biomarkers of Oxidative Status. Clin. Chim. Acta 2012, 413, 1446–1453. [Google Scholar] [CrossRef]
- Dokumacioglu, E.; Demiray, O.; Dokumacioglu, A.; Sahin, A.; Sen, T.M.; Cankaya, S. Measuring Urinary 8-Hydroxy-2′-Deoxyguanosine and Malondialdehyde Levels in Women with Overactive Bladder. Investig. Clin. Urol. 2018, 59, 252–256. [Google Scholar] [CrossRef]
- Jiménez-Cidre, M.A.; López-Fando, L.; Mora, A.M. Grupo de Investigación de Resultados de Salud en Urología Funcional y Urodinámica Clinical and Urodynamic Impact of Detrusor Overactivity in Women with Overactive Bladder. Actas Urol. Esp. 2019, 43, 221–227. [Google Scholar] [CrossRef]
- Chiang, C.-Y.; Fan, Y.-H.; Lin, A.T.-L.; Chen, K.-K. First Morning Voided Volume as a Valuable Tool for Evaluating Patients with Overactive Bladder. Urol. Sci. 2014, 25, 79–82. [Google Scholar] [CrossRef]
| Parameter | (A) USI + DO | (B) USI + HSB | (C) Control | Total | p-Value | Post Hoc |
|---|---|---|---|---|---|---|
| (N = 31) | (N = 28) | (N = 34) | ||||
| Age (years) | 61.9 ± 11.4 | 59.6 ± 10.5 | 60.6 ± 10.5 | 60.8 ± 10.7 | 0.714 | |
| BMI | 27.5 ± 5.12 | 25.9 ± 4.52 | 24.6 ± 4.71 | 26.0 ± 4.90 | 0.06 | |
| Previous SUI surgery | 6 (19.40%) | 1 (3.60%) | 0 (0.00%) | 7 (7.50%) | 0.005 | |
| HTN | 17 (54.8%) | 9 (32.1%) | 12 (35.3%) | 38 (40.9%) | 0.148 | |
| DM | 11 (35.5%) | 4 (14.3%) | 3 (8.8%) | 18 (19.4%) | 0.018 | |
| CVA | 5 (16.1%) | 4 (14.3%) | 0 (0%) | 9 (9.7%) | 0.012 | |
| Cancer | 3 (9.7%) | 2 (7.1%) | 1 (2.9%) | 6 (6.5%) | 0.535 | |
| Autoimmune diseases | 1 (3.2%) | 0 (0%) | 2 (5.9%) | 3 (3.2%) | 0.293 | |
| Urgency | 25 (80.6%) | 17 (63.0%) | 16 (47.1%) | 58 (62.4%) | 0.020 | |
| Pdet (cmH2O) | 23.0 ± 16.3 | 16.6 ± 9.9 | 13.3 ± 8.3 | 17.7 ± 12.7 | 0.008 | A vs. C |
| Qmax (mL/s) | 14.5 ± 7.5 | 13.5 ± 6.2 | 20.2 ± 7.3 | 16.2 ± 7.6 | 0.001 | A vs.C, B vs. C |
| Volume (mL) | 262 ± 85.0 | 267 ± 115 | 446 ± 122 | 330 ± 139 | <0.001 | A vs. C, B vs. C |
| PVR (mL) | 36.7 ± 61.1 | 38.5 ± 86.5 | 6.9 ± 14.2 | 27.2 ± 62.0 | 0.094 | |
| FSF (mL) | 121 ± 37.1 | 145 ± 54.2 | 166 ± 69.1 | 145 ± 58.1 | 0.007 | A vs. C |
| FS (mL) | 200 ± 65.0 | 236 ± 79.9 | 298 ± 97.7 | 247 ± 91.7 | <0.001 | A vs. C, B vs. C |
| Compliance | 73.5 ± 61.7 | 95.2 ± 55.1 | 178 ± 111 | 118 ± 93.1 | <0.001 | A vs. C, B vs. C |
| BCI | 95.2 ± 36.6 | 82.7 ± 34.6 | 109.9 ± 40.5 | 96.8 ± 38.8 | 0.02 | B vs. C |
| CBC (mL) | 298 ± 90.0 | 304 ± 93.1 | 439 ± 141.2 | 351 ± 130 | <0.001 | A vs. C, B vs. C |
| cQmax | 0.86 ± 0.42 | 0.76 ± 0.32 | 0.95 ± 0.31 | 0.86 ± 0.36 | 0.118 | |
| VE | 0.90 ± 0.17 | 0.87 ± 0.28 | 0.98 ± 0.04 | 0.92 ± 0.19 | 0.046 | A vs. C |
| Urinary Biomarkers @ | (A) USI + DO | (B) USI + HSB | (C) Control | Total | p-Value | Post Hoc |
|---|---|---|---|---|---|---|
| (N = 31) | (N = 28) | (N = 34) | ||||
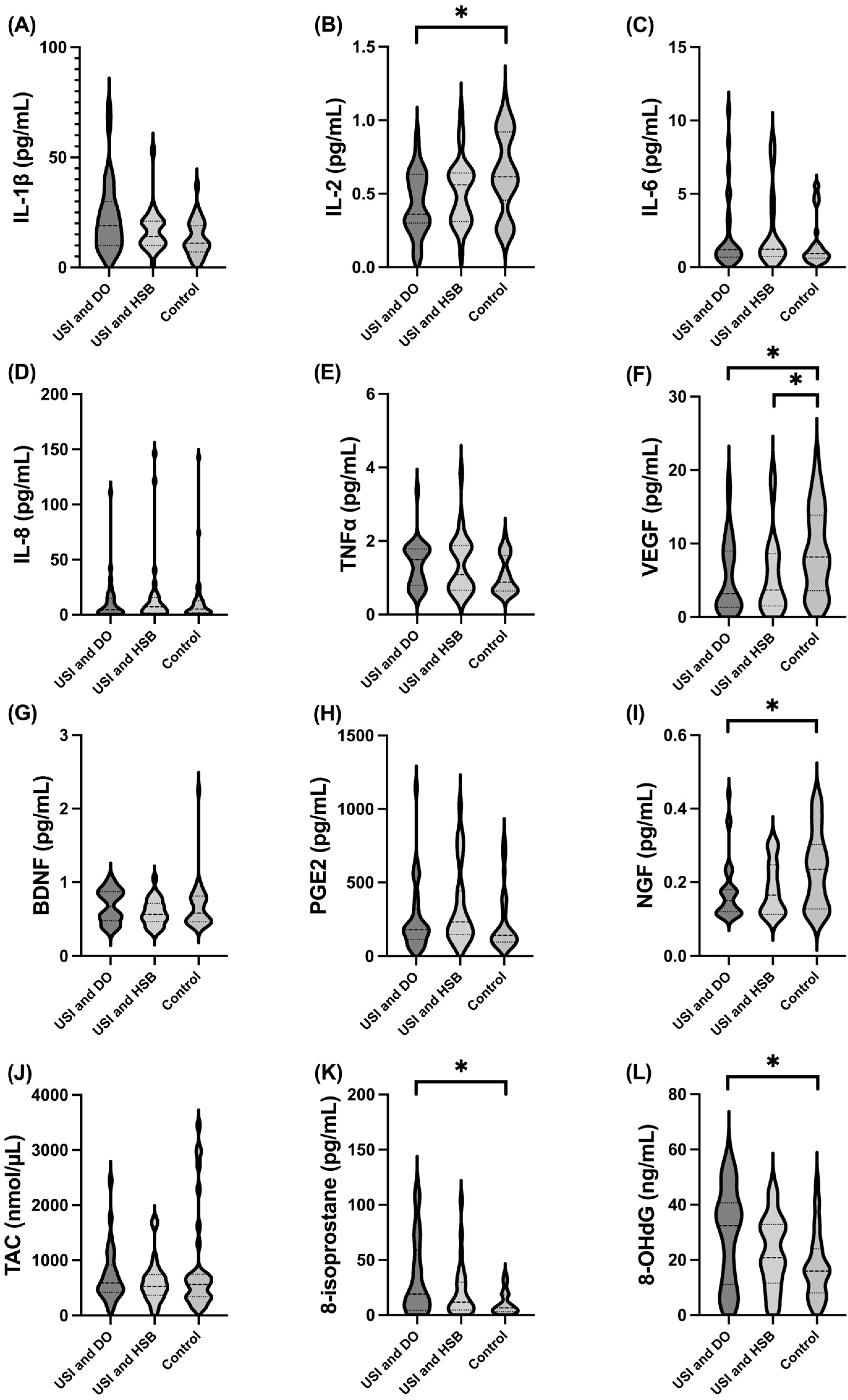
| IL-1β | 0.722 ± 0.229 (1) | 0.717 ± 0.287 (0) | 0.599 ± 0.235 (2) | 0.677 ± 0.255 (3) | 0.043 | |
| IL-2 | 0.433 ± 0.212 (0) | 0.516 ± 0.222 (1) | 0.638 ± 0.272 (0) | 0.533 ± 0.252 (1) | 0.021 | A vs. C |
| IL-6 | 2.15 ± 2.61 (0) | 2.41 ± 2.60 (0) | 1.62 ± 1.67 (0) | 2.03 ± 2.30 (0) | 0.312 | |
| IL-8 | 12.4 ± 21.3 (1) | 17.8 ± 34.2 (0) | 13.3 ± 26.8 (1) | 14.4 ± 27.5 (2) | 0.867 | |
| TNFα | 1.37 ± 0.621 (1) | 1.37 ± 0.795 (0) | 1.06 ± 0.509 (1) | 1.26 ± 0.655 (2) | 0.128 | |
| VEGF | 5.51 ± 4.99 (0) | 5.68 ± 5.42 (0) | 8.99 ± 5.834 (0) | 6.81 ± 5.62 (0) | 0.015 | A vs. C, B vs. C |
| BDNF | 0.678 ± 0.220 (1) | 0.588 ± 0.177 (0) | 0.674 ± 0.334 (1) | 0.649 ± 0.257 (2) | 0.272 | |
| TAC | 725 ± 496 (1) | 611 ± 388 (1) | 878 ± 911 (0) | 748 ± 663 (2) | 0.791 | |
| PGE2 | 256 ± 236 (1) | 335 ± 270 (0) | 221 ± 200 (0) | 267± 237 (1) | 0.063 | |
| NGF | 0.175 ± 0.083 (0) | 0.183 ± 0.072 (1) | 0.235 ± 0.103 (0) | 0.199 ± 0.091 (1) | 0.027 | A vs. C |
| 8-Isoprostane | 33.3 ± 34.6 (2) | 21.5 ± 24.5 (0) | 10.8 ± 10.5 (0) | 21.5 ± 26.4 (2) | 0.014 | A vs. C |
| 8-OHdG | 28.9 ± 17.3 (0) | 22.4 ± 12.9 (0) | 17.4 ± 11.7 (0) | 22.6 ± 14.7 (0) | 0.021 | A vs. C |
| Urinary Biomarkers @ | AUC | Cutoff Value @ | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|
| IL-1β | 0.680 | >0.665 | 63.33% | 68.75% | 66% | 67% |
| IL-2 | 0.698 | <0.545 | 67.74% | 67.65% | 66% | 70% |
| IL-6 | 0.555 | >1.175 | 51.72% | 66.67% | 58% | 61% |
| IL-8 | 0.506 | <1.795 | 33.33% | 78.79% | 59% | 57% |
| TNFα | 0.644 | >0.940 | 70% | 57.58% | 60% | 78% |
| VEGF | 0.690 | <2.090 | 41.94% | 90.91% | 81% | 63% |
| BDNF | 0.558 | >0.515 | 73.33% | 45.45% | 55% | 65% |
| TAC | 0.528 | >354.480 | 86.67% | 38.24% | 55% | 76% |
| PGE2 | 0.680 | <0.190 | 77.42% | 58.82% | 63% | 74% |
| NGF | 0.569 | >157.555 | 66.67% | 64.71% | 63% | 69% |
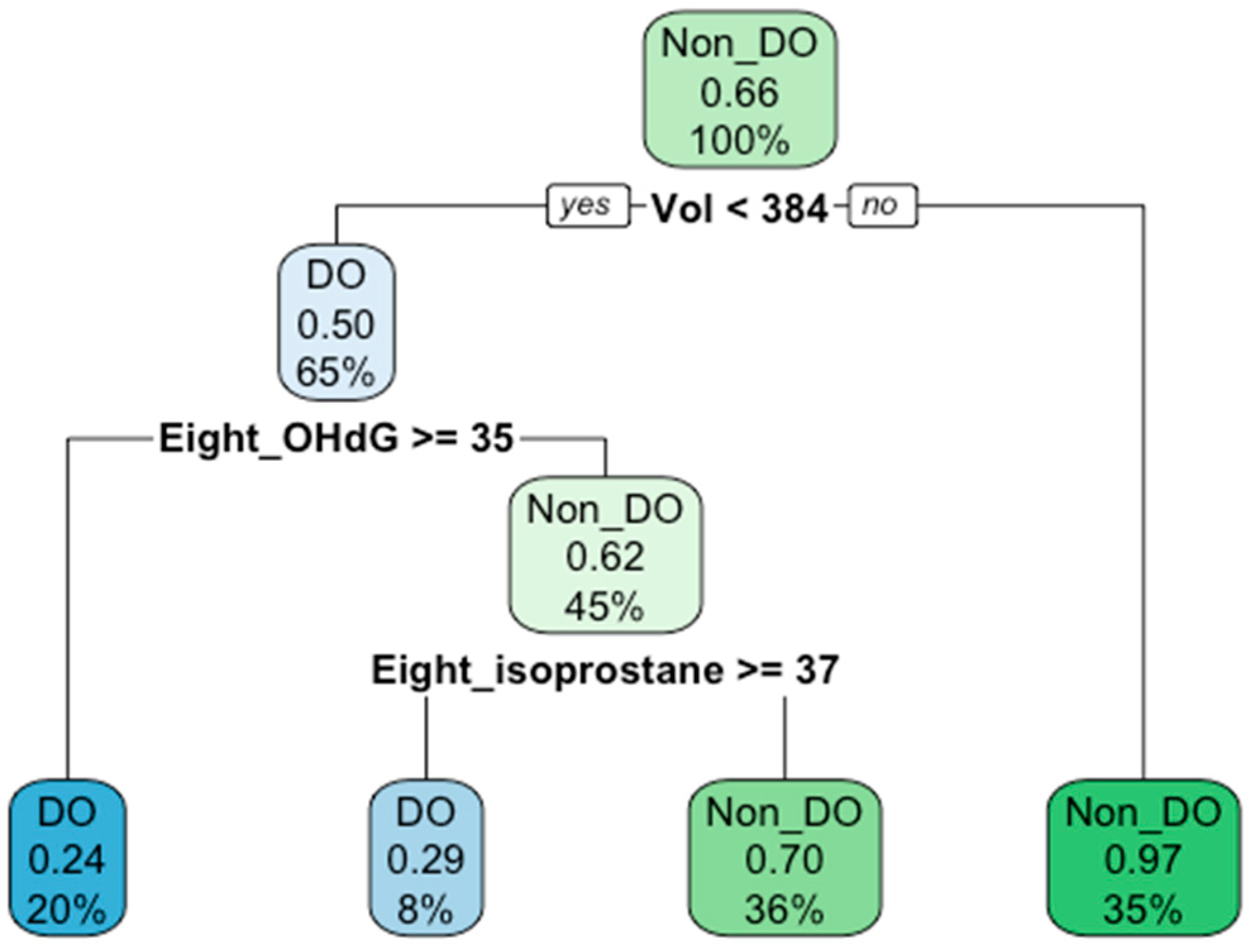
| 8-Isoprostane | 0.705 | >12.005 | 67.74% | 70.59% | 68% | 71% |
| 8-OHdG | 0.684 | >24.855 | 62.07% | 82.35% | 75% | 72% |
| Voided volume | 0.915 | <384.0 | 96.77 | 87.88 | 88% | 97% |
| Urinary Biomarkers @ | AUC | Cutoff Value @ | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|
| IL-1β | 0.606 | >0.695 | 56.7% | 66.7% | 45.9% | 75.5% |
| IL-2 | 0.655 | <0.515 | 61.3% | 65.6% | 47.5% | 76.9% |
| IL-6 | 0.506 | >1.180 | 51.7% | 58.3% | 37.5% | 71.4% |
| IL-8 | 0.519 | <1.785 | 33.3% | 77.1% | 41.7% | 70.1% |
| TNFα | 0.578 | >0.940 | 70.0% | 54.1% | 42.9% | 78.6% |
| VEGF | 0.604 | <2.090 | 41.9% | 80.3% | 52.0% | 73.1% |
| BDNF | 0.588 | >0.745 | 50.0% | 72.1% | 46.9% | 74.6% |
| TAC | 0.539 | >365.889 | 86.7% | 31.2% | 38.2% | 82.6% |
| PGE2 | 0.507 | <71.440 | 20.0% | 93.6% | 60.0% | 70.7% |
| NGF | 0.618 | <0.190 | 77.40% | 50% | 43.6% | 81.6% |
| 8-Isoprostane | 0.654 | >12.495 | 62.3% | 67.7% | 48.0% | 79.0% |
| 8-OHdG | 0.657 | >33.955 | 48.3% | 88.7% | 66.7% | 78.6% |
| Voided volume | 0.750 | <384.0 | 96.8% | 54.1% | 51.7% | 97.1% |
| Urinary Biomarkers @ | p-Value | Odds Ratio | 95% CI |
|---|---|---|---|
| USI + DO vs. control | |||
| IL-1β | 0.607 | 2.656 | 0.064–110.6 |
| IL-2 | 0.093 | 0.024 | 0.000–1.851 |
| VEGF | 0.452 | 0.934 | 0.780–1.117 |
| NGF | 0.230 | 3386.128 | 0.006–1000 |
| 8-Isoprostane | 0.038 | 1.046 | 1.002–1.090 |
| 8-OHdG | 0.019 | 1.064 | 1.010–1.120 |
| USI + DO vs. USI + non-DO | |||
| IL-1β | 0.700 | 1.566 | 0.159–15.40 |
| IL-2 | 0.183 | 0.111 | 0.004–2.819 |
| VEGF | 0.585 | 1.035 | 0.916–1.169 |
| NGF | 0.920 | 0.623 | 0.000–1000 |
| 8-Isoprostane | 0.262 | 1.013 | 0.990–1.037 |
| 8-OHdG | 0.097 | 1.032 | 0.994–1.071 |
| Urinary Biomarkers @ | Pdet | Qmax | Vol | PVR | FSF | FS | Compliance | BCI | CBC | cQmax | VE |
|---|---|---|---|---|---|---|---|---|---|---|---|
| IL-1β | n.s. | n.s. | −0.218 | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. |
| IL-2 | −0.220 | 0.223 | 0.377 | n.s. | n.s. | n.s. | n.s. | n.s. | 0.329 | n.s. | n.s. |
| IL-6 | n.s. | n.s. | n.s. | n.s. | n.s. | −0.271 | n.s. | n.s. | n.s. | n.s. | n.s. |
| IL-8 | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. |
| TNFα | 0.212 | −0.261 | −0.337 | 0.416 | n.s. | n.s. | n.s. | n.s. | n.s. | −0.213 | −0.391 |
| VEGF | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | 0.208 | n.s. | n.s. |
| BDNF | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. |
| TAC | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. |
| PGE2 | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. |
| NGF | −0.247 | 0.212 | 0.335 | n.s. | n.s. | 0.216 | n.s. | n.s. | 0.259 | n.s. | n.s. |
| 8-Isoprostane | n.s. | n.s. | −0.391 | n.s. | n.s. | n.s. | n.s. | n.s. | −0.333 | n.s. | −0.256 |
| 8-OHdG | n.s. | n.s. | −0.249 | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, W.-H.; Jiang, Y.-H.; Kuo, H.-C. Urinary Oxidative Stress Biomarkers in the Diagnosis of Detrusor Overactivity in Female Patients with Stress Urinary Incontinence. Biomedicines 2023, 11, 357. https://doi.org/10.3390/biomedicines11020357
Chen W-H, Jiang Y-H, Kuo H-C. Urinary Oxidative Stress Biomarkers in the Diagnosis of Detrusor Overactivity in Female Patients with Stress Urinary Incontinence. Biomedicines. 2023; 11(2):357. https://doi.org/10.3390/biomedicines11020357
Chicago/Turabian StyleChen, Wei-Hsin, Yuan-Hong Jiang, and Hann-Chorng Kuo. 2023. "Urinary Oxidative Stress Biomarkers in the Diagnosis of Detrusor Overactivity in Female Patients with Stress Urinary Incontinence" Biomedicines 11, no. 2: 357. https://doi.org/10.3390/biomedicines11020357
APA StyleChen, W.-H., Jiang, Y.-H., & Kuo, H.-C. (2023). Urinary Oxidative Stress Biomarkers in the Diagnosis of Detrusor Overactivity in Female Patients with Stress Urinary Incontinence. Biomedicines, 11(2), 357. https://doi.org/10.3390/biomedicines11020357






