The Future of Precision Medicine in the Cure of Alzheimer’s Disease
Abstract
1. Introduction
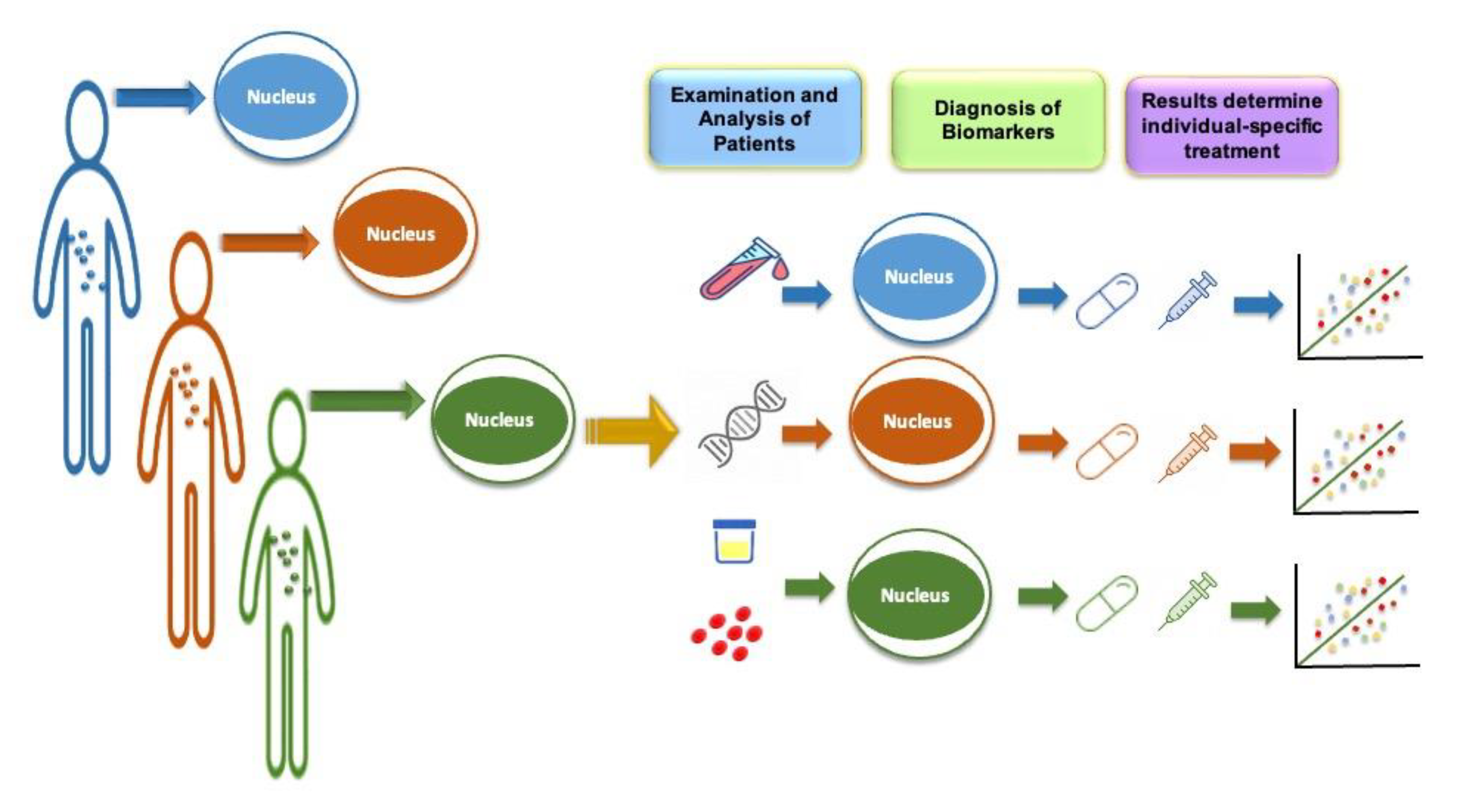
2. Concept of Precision Medicine
3. Alzheimer’s Disease and Other Related Disorders
3.1. Alzheimer’s Disease
3.2. Parkinson’s Disease
3.3. Dementia with Lewy Bodies
3.4. Amyotrophic Lateral Sclerosis
4. Precision Medicine Application to AD
4.1. Precision Medicine for AD and the Role of Genetics
4.1.1. APOE Gene
4.1.2. MTHFR Gene
4.1.3. Presenilin 1 and 2 Gene
4.1.4. Genome-Wide Significant (GWS) Susceptibility Loci
4.2. Role of Physiological Biomarkers in Precision Medicine for AD
4.3. Evolving Conception of Neuroimaging in AD Precision Medicine
4.4. Implementation of Artificial Intelligence as a Road to Precision Medicine
5. Limitation, Regulation, and Ethical and Societal Consideration of Precision Medicine
6. Future Prospective to the Usage of Precision Medicine
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sloane, P.D.; Zimmerman, S.; Suchindran, C.; Reed, P.; Wang, L.; Boustani, M.; Sudha, S. The Public Health Impact of Alzheimer’s Disease, 2000–2050: Potential Implication of Treatment Advances. Annu. Rev. Public Health 2002, 23, 213–231. [Google Scholar] [CrossRef] [PubMed]
- Siemieniuk, R.A.C.; Guyatt, G.H. Corticosteroids in the Treatment of Community-Acquired Pneumonia: An Evidence Summary. Pol. Arch. Med. Wewn. 2015, 125, 570–575. [Google Scholar] [CrossRef] [PubMed]
- Panza, F.; Lozupone, M.; Logroscino, G.; Imbimbo, B.P. A Critical Appraisal of Amyloid-β-Targeting Therapies for Alzheimer Disease. Nat. Rev. Neurol. 2019, 15, 73–88. [Google Scholar] [CrossRef] [PubMed]
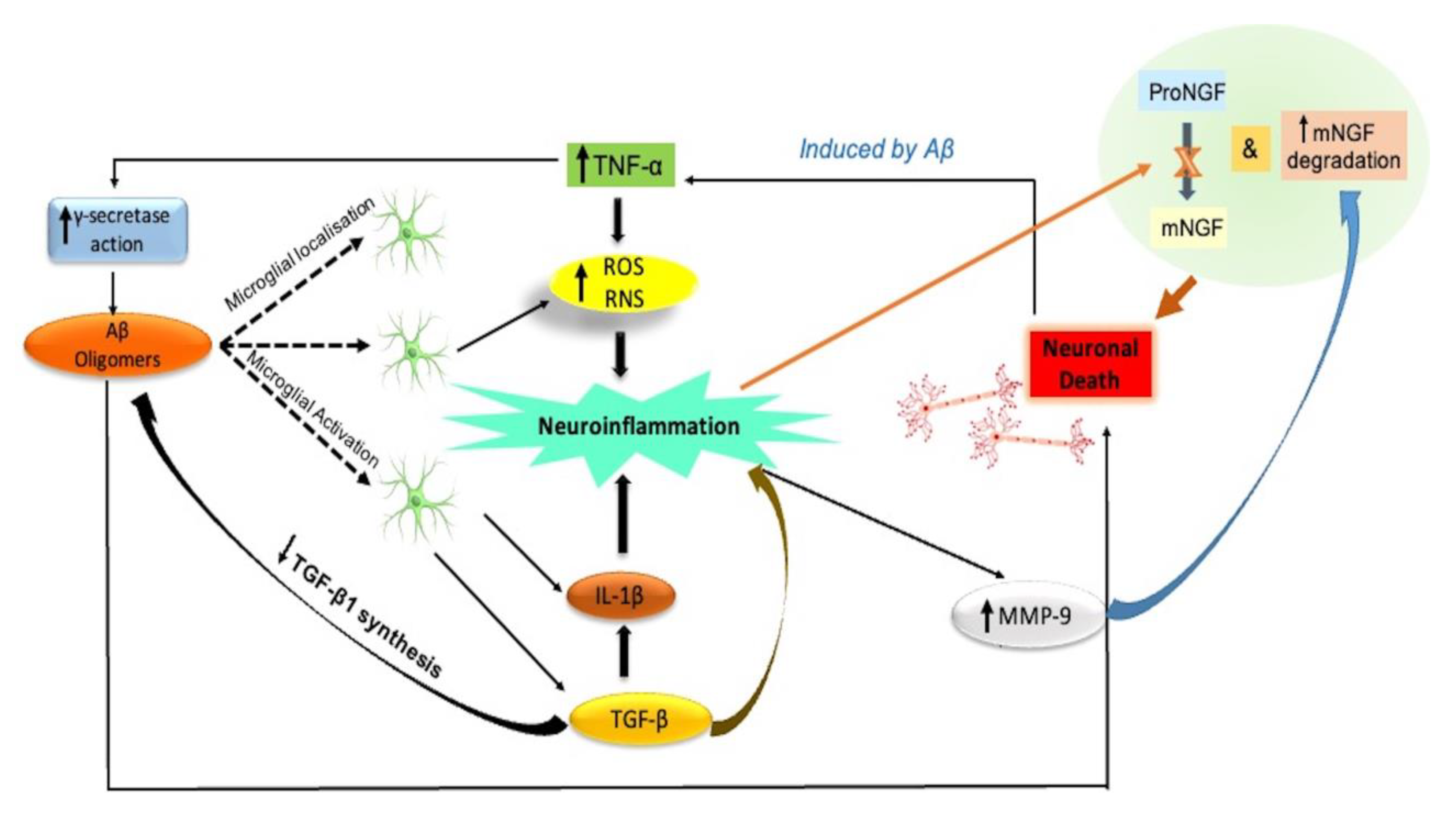
- Hampel, H.; Caraci, F.; Cuello, A.C.; Caruso, G.; Nisticò, R.; Corbo, M.; Baldacci, F.; Toschi, N.; Garaci, F.; Chiesa, P.A.; et al. A Path Toward Precision Medicine for Neuroinflammatory Mechanisms in Alzheimer’s Disease. Front. Immunol. 2020, 11, 456. [Google Scholar] [CrossRef] [PubMed]
- Ohm, D.T.; Fought, A.J.; Martersteck, A.; Coventry, C.; Sridhar, J.; Gefen, T.; Weintraub, S.; Bigio, E.; Mesulam, M.-M.; Rogalski, E.; et al. Accumulation of Neurofibrillary Tangles and Activated Microglia Is Associated with Lower Neuron Densities in the Aphasic Variant of Alzheimer’s Disease. Brain Pathol. 2021, 31, 189–204. [Google Scholar] [CrossRef]
- Heneka, M.T.; Carson, M.J.; El Khoury, J.; Landreth, G.E.; Brosseron, F.; Feinstein, D.L.; Jacobs, A.H.; Wyss-Coray, T.; Vitorica, J.; Ransohoff, R.M.; et al. Neuroinflammation in Alzheimer’s Disease. Lancet Neurol. 2015, 14, 388–405. [Google Scholar] [CrossRef]
- Nordengen, K.; Kirsebom, B.-E.; Henjum, K.; Selnes, P.; Gísladóttir, B.; Wettergreen, M.; Torsetnes, S.B.; Grøntvedt, G.R.; Waterloo, K.K.; Aarsland, D.; et al. Glial Activation and Inflammation along the Alzheimer’s Disease Continuum. J. Neuroinflammation 2019, 16, 46. [Google Scholar] [CrossRef]
- Hampel, H.; Frank, R.; Broich, K.; Teipel, S.J.; Katz, R.G.; Hardy, J.; Herholz, K.; Bokde, A.L.W.; Jessen, F.; Hoessler, Y.C.; et al. Biomarkers for Alzheimer’s Disease: Academic, Industry and Regulatory Perspectives. Nat. Rev. Drug Discov. 2010, 9, 560–574. [Google Scholar] [CrossRef]
- Chen, R.; Mias, G.I.; Li-Pook-Than, J.; Jiang, L.; Lam, H.Y.K.; Chen, R.; Miriami, E.; Karczewski, K.J.; Hariharan, M.; Dewey, F.E.; et al. Personal Omics Profiling Reveals Dynamic Molecular and Medical Phenotypes. Cell 2012, 148, 1293–1307. [Google Scholar] [CrossRef]
- Hampel, H.; O’Bryant, S.E.; Durrleman, S.; Younesi, E.; Rojkova, K.; Escott-Price, V.; Corvol, J.-C.; Broich, K.; Dubois, B.; Lista, S.; et al. A Precision Medicine Initiative for Alzheimer’s Disease: The Road Ahead to Biomarker-Guided Integrative Disease Modeling. Climacteric J. Int. Menopause Soc. 2017, 20, 107–118. [Google Scholar] [CrossRef]
- Berkowitz, C.; Mosconi, L.; Scheyer, O.; Rahman, A.; Hristov, H.; Isaacson, R. Precision Medicine for Alzheimer’s Disease Prevention. Healthcare 2018, 6, 82. [Google Scholar] [CrossRef] [PubMed]
- Antman, E.M.; Loscalzo, J. Precision Medicine in Cardiology. Nat. Rev. Cardiol. 2016, 13, 591–602. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.H.; Bode, A.M.; Dong, Z. Precision Medicine: The Foundation of Future Cancer Therapeutics. NPJ Precis. Oncol. 2017, 1, 12. [Google Scholar] [CrossRef] [PubMed]
- Reitz, C. Toward Precision Medicine in Alzheimer’s Disease. Ann. Transl. Med. 2016, 4, 107. [Google Scholar] [CrossRef] [PubMed]
- Ridge, P.G.; Hoyt, K.B.; Boehme, K.; Mukherjee, S.; Crane, P.K.; Haines, J.L.; Mayeux, R.; Farrer, L.A.; Pericak-Vance, M.A.; Schellenberg, G.D.; et al. Assessment of the Genetic Variance of Late-Onset Alzheimer’s Disease. Neurobiol. Aging 2016, 41, 200.e13–200.e20. [Google Scholar] [CrossRef]
- Bisht, K.; Sharma, K.; Tremblay, M.-È. Chronic Stress as a Risk Factor for Alzheimer’s Disease: Roles of Microglia-Mediated Synaptic Remodeling, Inflammation, and Oxidative Stress. Neurobiol. Stress 2018, 9, 9–21. [Google Scholar] [CrossRef]
- Decourt, B.; Lahiri, D.K.; Sabbagh, M.N. Targeting Tumor Necrosis Factor Alpha for Alzheimer’s Disease. Curr. Alzheimer Res. 2017, 14, 412–425. [Google Scholar] [CrossRef]
- Brosseron, F.; Krauthausen, M.; Kummer, M.; Heneka, M.T. Body Fluid Cytokine Levels in Mild Cognitive Impairment and Alzheimer’s Disease: A Comparative Overview. Mol. Neurobiol. 2014, 50, 534–544. [Google Scholar] [CrossRef]
- Eikelenboom, P.; Zhan, S.S.; van Gool, W.A.; Allsop, D. Inflammatory Mechanisms in Alzheimer’s Disease. Trends Pharmacol. Sci. 1994, 15, 447–450. [Google Scholar] [CrossRef]
- Caraci, F.; Gulisano, W.; Guida, C.A.; Impellizzeri, A.A.R.; Drago, F.; Puzzo, D.; Palmeri, A. A Key Role for TGF-Β1 in Hippocampal Synaptic Plasticity and Memory. Sci. Rep. 2015, 5, 11252. [Google Scholar] [CrossRef]
- Tong, L.; Balazs, R.; Soiampornkul, R.; Thangnipon, W.; Cotman, C.W. Interleukin-1 Beta Impairs Brain Derived Neurotrophic Factor-Induced Signal Transduction. Neurobiol. Aging 2008, 29, 1380–1393. [Google Scholar] [CrossRef]
- Bruno, M.A.; Leon, W.C.; Fragoso, G.; Mushynski, W.E.; Almazan, G.; Cuello, A.C. Amyloid Beta-Induced Nerve Growth Factor Dysmetabolism in Alzheimer Disease. J. Neuropathol. Exp. Neurol. 2009, 68, 857–869. [Google Scholar] [CrossRef]
- Iulita, M.F.; do Carmo, S.; Ower, A.K.; Fortress, A.M.; Flores Aguilar, L.; Hanna, M.; Wisniewski, T.; Granholm, A.-C.; Buhusi, M.; Busciglio, J.; et al. Nerve Growth Factor Metabolic Dysfunction in Down’s Syndrome Brains. Brain J. Neurol. 2014, 137, 860–872. [Google Scholar] [CrossRef]
- Agid, Y. Levodopa: Is Toxicity a Myth? Neurology 1998, 50, 858–863. [Google Scholar] [CrossRef]
- Dickson, D.W.; Braak, H.; Duda, J.E.; Duyckaerts, C.; Gasser, T.; Halliday, G.M.; Hardy, J.; Leverenz, J.B.; del Tredici, K.; Wszolek, Z.K.; et al. Neuropathological Assessment of Parkinson’s Disease: Refining the Diagnostic Criteria. Lancet Neurol. 2009, 8, 1150–1157. [Google Scholar] [CrossRef]
- Houlden, H.; Singleton, A.B. The Genetics and Neuropathology of Parkinson’s Disease. Acta Neuropathol. 2012, 124, 325–338. [Google Scholar] [CrossRef]
- Riederer, P.; Sofic, E.; Rausch, W.D.; Schmidt, B.; Reynolds, G.P.; Jellinger, K.; Youdim, M.B. Transition Metals, Ferritin, Glutathione, and Ascorbic Acid in Parkinsonian Brains. J. Neurochem. 1989, 52, 515–520. [Google Scholar] [CrossRef]
- Schapira, A.H.; Jenner, P. Etiology and Pathogenesis of Parkinson’s Disease. Mov. Disord. Off. J. Mov. Disord. Soc. 2011, 26, 1049–1055. [Google Scholar] [CrossRef]
- Tofaris, G.K.; Spillantini, M.G. Alpha-Synuclein Dysfunction in Lewy Body Diseases. Mov. Disord. Off. J. Mov. Disord. Soc. 2005, 20 (Suppl. S12), S37–S44. [Google Scholar] [CrossRef]
- Hernández-Romero, M.C.; Delgado-Cortés, M.J.; Sarmiento, M.; de Pablos, R.M.; Espinosa-Oliva, A.M.; Argüelles, S.; Bández, M.J.; Villarán, R.F.; Mauriño, R.; Santiago, M.; et al. Peripheral Inflammation Increases the Deleterious Effect of CNS Inflammation on the Nigrostriatal Dopaminergic System. Neurotoxicology 2012, 33, 347–360. [Google Scholar] [CrossRef]
- Armstrong, M.J. Advances in Dementia with Lewy Bodies. Ther. Adv. Neurol. Disord. 2021, 14, 17562864211057666. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Kordich, J.K.; Williams, E.T.; Levine, N.; Cole-Strauss, A.; Marshall, L.; Labrie, V.; Ma, J.; Lipton, J.W.; Moore, D.J. Parkinson’s Disease-Linked D620N VPS35 Knockin Mice Manifest Tau Neuropathology and Dopaminergic Neurodegeneration. Proc. Natl. Acad. Sci. USA 2019, 116, 5765–5774. [Google Scholar] [CrossRef] [PubMed]
- Boillée, S.; Vande Velde, C.; Cleveland, D.W. ALS: A Disease of Motor Neurons and Their Nonneuronal Neighbors. Neuron 2006, 52, 39–59. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, S.; Iwata, M. Mitochondrial Alterations in the Spinal Cord of Patients with Sporadic Amyotrophic Lateral Sclerosis. J. Neuropathol. Exp. Neurol. 2007, 66, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Magrané, J.; Manfredi, G. Mitochondrial Function, Morphology, and Axonal Transport in Amyotrophic Lateral Sclerosis. Antioxid. Redox Signal. 2009, 11, 1615–1626. [Google Scholar] [CrossRef]
- Higgins, C.M.J.; Jung, C.; Xu, Z. ALS-Associated Mutant SOD1G93A Causes Mitochondrial Vacuolation by Expansion of the Intermembrane Space and by Involvement of SOD1 Aggregation and Peroxisomes. BMC Neurosci. 2003, 4, 16. [Google Scholar] [CrossRef]
- Bacman, S.R.; Bradley, W.G.; Moraes, C.T. Mitochondrial Involvement in Amyotrophic Lateral Sclerosis: Trigger or Target? Mol. Neurobiol. 2006, 33, 113–131. [Google Scholar] [CrossRef]
- Tohgi, H.; Abe, T.; Yamazaki, K.; Murata, T.; Ishizaki, E.; Isobe, C. Remarkable Increase in Cerebrospinal Fluid 3-Nitrotyrosine in Patients with Sporadic Amyotrophic Lateral Sclerosis. Ann. Neurol. 1999, 46, 129–131. [Google Scholar] [CrossRef]
- Zarei, S.; Carr, K.; Reiley, L.; Diaz, K.; Guerra, O.; Altamirano, P.F.; Pagani, W.; Lodin, D.; Orozco, G.; Chinea, A. A Comprehensive Review of Amyotrophic Lateral Sclerosis. Surg. Neurol. Int. 2015, 6, 171. [Google Scholar] [CrossRef]
- Zhao, W.; Beers, D.R.; Appel, S.H. Immune-Mediated Mechanisms in the Pathoprogression of Amyotrophic Lateral Sclerosis. J. Neuroimmune Pharmacol. Off. J. Soc. NeuroImmune Pharmacol. 2013, 8, 888–899. [Google Scholar] [CrossRef]
- Hampel, H.; O’Bryant, S.E.; Castrillo, J.I.; Ritchie, C.; Rojkova, K.; Broich, K.; Benda, N.; Nisticò, R.; Frank, R.A.; Dubois, B.; et al. PRECISION MEDICINE—The Golden Gate for Detection, Treatment and Prevention of Alzheimer’s Disease. J. Prev. Alzheimer’s Dis. 2016, 3, 243–259. [Google Scholar] [CrossRef]
- National Research Council (US) Committee on A Framework for Developing a New Taxonomy of Disease toward Precision Medicine: Building a Knowledge Network for Biomedical Research and a New Taxonomy of Disease; The National Academies Collection: Reports Funded by National Institutes of Health; National Academies Press (US): Washington, DC, USA, 2011; ISBN 978-0-309-22222-8.
- Hampel, H.; Lista, S.; Khachaturian, Z.S. Development of Biomarkers to Chart All Alzheimer’s Disease Stages: The Royal Road to Cutting the Therapeutic Gordian Knot. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2012, 8, 312–336. [Google Scholar] [CrossRef]
- Lista, S.; Khachaturian, Z.S.; Rujescu, D.; Garaci, F.; Dubois, B.; Hampel, H. Application of Systems Theory in Longitudinal Studies on the Origin and Progression of Alzheimer’s Disease. Methods Mol. Biol. Clifton NJ 2016, 1303, 49–67. [Google Scholar] [CrossRef]
- Dubois, B.; Feldman, H.H.; Jacova, C.; Hampel, H.; Molinuevo, J.L.; Blennow, K.; DeKosky, S.T.; Gauthier, S.; Selkoe, D.; Bateman, R.; et al. Advancing Research Diagnostic Criteria for Alzheimer’s Disease: The IWG-2 Criteria. Lancet Neurol. 2014, 13, 614–629. [Google Scholar] [CrossRef]
- Hampel, H.; Lista, S.; Teipel, S.J.; Garaci, F.; Nisticò, R.; Blennow, K.; Zetterberg, H.; Bertram, L.; Duyckaerts, C.; Bakardjian, H.; et al. Perspective on Future Role of Biological Markers in Clinical Therapy Trials of Alzheimer’s Disease: A Long-Range Point of View beyond 2020. Biochem. Pharmacol. 2014, 88, 426–449. [Google Scholar] [CrossRef]
- Hampel, H.; Lista, S. Use of Biomarkers and Imaging to Assess Pathophysiology, Mechanisms of Action and Target Engagement. J. Nutr. Health Aging 2013, 17, 54–63. [Google Scholar] [CrossRef]
- Zetzsche, T.; Rujescu, D.; Hardy, J.; Hampel, H. Advances and Perspectives from Genetic Research: Development of Biological Markers in Alzheimer’s Disease. Expert Rev. Mol. Diagn. 2010, 10, 667–690. [Google Scholar] [CrossRef]
- Hampel, H.; Lista, S. Alzheimer Disease: From Inherited to Sporadic AD-Crossing the Biomarker Bridge. Nat. Rev. Neurol. 2012, 8, 598–600. [Google Scholar] [CrossRef]
- Lista, S.; O’Bryant, S.E.; Blennow, K.; Dubois, B.; Hugon, J.; Zetterberg, H.; Hampel, H. Biomarkers in Sporadic and Familial Alzheimer’s Disease. J. Alzheimer’s Dis. 2015, 47, 291–317. [Google Scholar] [CrossRef]
- Blennow, K.; Hampel, H.; Weiner, M.; Zetterberg, H. Cerebrospinal Fluid and Plasma Biomarkers in Alzheimer Disease. Nat. Rev. Neurol. 2010, 6, 131–144. [Google Scholar] [CrossRef]
- Hampel, H.; Shen, Y.; Walsh, D.M.; Aisen, P.; Shaw, L.M.; Zetterberg, H.; Trojanowski, J.Q.; Blennow, K. Biological Markers of Amyloid Beta-Related Mechanisms in Alzheimer’s Disease. Exp. Neurol. 2010, 223, 334–346. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, K.; O’Bryant, S.E.; Hampel, H.; Trojanowski, J.Q.; Montine, T.J.; Jeromin, A.; Blennow, K.; Lönneborg, A.; Wyss-Coray, T.; Soares, H.; et al. The Future of Blood-Based Biomarkers for Alzheimer’s Disease. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2014, 10, 115–131. [Google Scholar] [CrossRef] [PubMed]
- O’Bryant, S.E.; Lista, S.; Rissman, R.A.; Edwards, M.; Zhang, F.; Hall, J.; Zetterberg, H.; Lovestone, S.; Gupta, V.; Graff-Radford, N.; et al. Comparing Biological Markers of Alzheimer’s Disease across Blood Fraction and Platforms: Comparing Apples to Oranges. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2016, 3, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Ewers, M.; Sperling, R.A.; Klunk, W.E.; Weiner, M.W.; Hampel, H. Neuroimaging Markers for the Prediction and Early Diagnosis of Alzheimer’s Disease Dementia. Trends Neurosci. 2011, 34, 430–442. [Google Scholar] [CrossRef]
- Teipel, S.J.; Grothe, M.; Lista, S.; Toschi, N.; Garaci, F.G.; Hampel, H. Relevance of Magnetic Resonance Imaging for Early Detection and Diagnosis of Alzheimer Disease. Med. Clin. N. Am. 2013, 97, 399–424. [Google Scholar] [CrossRef]
- Poil, S.-S.; de Haan, W.; van der Flier, W.M.; Mansvelder, H.D.; Scheltens, P.; Linkenkaer-Hansen, K. Integrative EEG Biomarkers Predict Progression to Alzheimer’s Disease at the MCI Stage. Front. Aging Neurosci. 2013, 5, 58. [Google Scholar] [CrossRef]
- Jørgensen, J.T. Companion Diagnostics: The Key to Personalized Medicine. Expert Rev. Mol. Diagn. 2015, 15, 153–156. [Google Scholar] [CrossRef]
- Lyman, G.H.; Moses, H.L. Biomarker Tests for Molecularly Targeted Therapies—The Key to Unlocking Precision Medicine. N. Engl. J. Med. 2016, 375, 4–6. [Google Scholar] [CrossRef]
- Ballard, C.; Gauthier, S.; Corbett, A.; Brayne, C.; Aarsland, D.; Jones, E. Alzheimer’s Disease. Lancet Lond. Engl. 2011, 377, 1019–1031. [Google Scholar] [CrossRef]
- Mahley, R.W. Apolipoprotein E: Cholesterol Transport Protein with Expanding Role in Cell Biology. Science 1988, 240, 622–630. [Google Scholar] [CrossRef]
- Corder, E.H.; Saunders, A.M.; Strittmatter, W.J.; Schmechel, D.E.; Gaskell, P.C.; Small, G.W.; Roses, A.D.; Haines, J.L.; Pericak-Vance, M.A. Gene Dose of Apolipoprotein E Type 4 Allele and the Risk of Alzheimer’s Disease in Late Onset Families. Science 1993, 261, 921–923. [Google Scholar] [CrossRef]
- Talbot, C.; Lendon, C.; Craddock, N.; Shears, S.; Morris, J.C.; Goate, A. Protection against Alzheimer’s Disease with ApoE Epsilon 2. Lancet Lond. Engl. 1994, 343, 1432–1433. [Google Scholar] [CrossRef]
- Farrer, L.A.; Cupples, L.A.; Haines, J.L.; Hyman, B.; Kukull, W.A.; Mayeux, R.; Myers, R.H.; Pericak-Vance, M.A.; Risch, N.; van Duijn, C.M. Effects of Age, Sex, and Ethnicity on the Association between Apolipoprotein E Genotype and Alzheimer Disease. A Meta-Analysis. APOE and Alzheimer Disease Meta Analysis Consortium. JAMA 1997, 278, 1349–1356. [Google Scholar] [CrossRef]
- Strittmatter, W.J.; Weisgraber, K.H.; Huang, D.Y.; Dong, L.M.; Salvesen, G.S.; Pericak-Vance, M.; Schmechel, D.; Saunders, A.M.; Goldgaber, D.; Roses, A.D. Binding of Human Apolipoprotein E to Synthetic Amyloid Beta Peptide: Isoform-Specific Effects and Implications for Late-Onset Alzheimer Disease. Proc. Natl. Acad. Sci. USA 1993, 90, 8098–8102. [Google Scholar] [CrossRef]
- Van Cauwenberghe, C.; van Broeckhoven, C.; Sleegers, K. The Genetic Landscape of Alzheimer Disease: Clinical Implications and Perspectives. Genet. Med. Off. J. Am. Coll. Med. Genet. 2016, 18, 421–430. [Google Scholar] [CrossRef]
- Solomon, A.; Turunen, H.; Ngandu, T.; Peltonen, M.; Levälahti, E.; Helisalmi, S.; Antikainen, R.; Bäckman, L.; Hänninen, T.; Jula, A.; et al. Effect of the Apolipoprotein E Genotype on Cognitive Change during a Multidomain Lifestyle Intervention: A Subgroup Analysis of a Randomized Clinical Trial. JAMA Neurol. 2018, 75, 462–470. [Google Scholar] [CrossRef]
- Masson, L.F.; McNeill, G.; Avenell, A. Genetic Variation and the Lipid Response to Dietary Intervention: A Systematic Review. Am. J. Clin. Nutr. 2003, 77, 1098–1111. [Google Scholar] [CrossRef]
- Martínez-Lapiscina, E.H.; Galbete, C.; Corella, D.; Toledo, E.; Buil-Cosiales, P.; Salas-Salvado, J.; Ros, E.; Martinez-Gonzalez, M.A. Genotype Patterns at CLU, CR1, PICALM and APOE, Cognition and Mediterranean Diet: The PREDIMED-NAVARRA Trial. Genes Nutr. 2014, 9, 393. [Google Scholar] [CrossRef]
- Etnier, J.L.; Caselli, R.J.; Reiman, E.M.; Alexander, G.E.; Sibley, B.A.; Tessier, D.; McLemore, E.C. Cognitive Performance in Older Women Relative to ApoE-Epsilon4 Genotype and Aerobic Fitness. Med. Sci. Sports Exerc. 2007, 39, 199–207. [Google Scholar] [CrossRef]
- Yassine, H.N.; Braskie, M.N.; Mack, W.J.; Castor, K.J.; Fonteh, A.N.; Schneider, L.S.; Harrington, M.G.; Chui, H.C. Association of Docosahexaenoic Acid Supplementation with Alzheimer Disease Stage in Apolipoprotein E Ε4 Carriers: A Review. JAMA Neurol. 2017, 74, 339–347. [Google Scholar] [CrossRef]
- Sibani, S.; Christensen, B.; O’Ferrall, E.; Saadi, I.; Hiou-Tim, F.; Rosenblatt, D.S.; Rozen, R. Characterization of Six Novel Mutations in the Methylenetetrahydrofolate Reductase (MTHFR) Gene in Patients with Homocystinuria. Hum. Mutat. 2000, 15, 280–287. [Google Scholar] [CrossRef]
- Román, G.C. MTHFR Gene Mutations: A Potential Marker of Late-Onset Alzheimer’s Disease? J. Alzheimer’s Dis. 2015, 47, 323–327. [Google Scholar] [CrossRef] [PubMed]
- Romero-Sánchez, C.; Gómez-Gutierrez, A.; Gómez, P.E.; Casas-Gomez, M.C.; Briceño, I. C677T (RS1801133) MTHFR Gene Polymorphism Frequency in a Colombian Population. Colomb. Medica Cali Colomb. 2015, 46, 75–79. [Google Scholar] [CrossRef]
- McCaddon, A.; Hudson, P.; Davies, G.; Hughes, A.; Williams, J.H.; Wilkinson, C. Homocysteine and Cognitive Decline in Healthy Elderly. Dement. Geriatr. Cogn. Disord. 2001, 12, 309–313. [Google Scholar] [CrossRef]
- Seshadri, S.; Beiser, A.; Selhub, J.; Jacques, P.F.; Rosenberg, I.H.; D’Agostino, R.B.; Wilson, P.W.F.; Wolf, P.A. Plasma Homocysteine as a Risk Factor for Dementia and Alzheimer’s Disease. N. Engl. J. Med. 2002, 346, 476–483. [Google Scholar] [CrossRef]
- Clarke, R.; Birks, J.; Nexo, E.; Ueland, P.M.; Schneede, J.; Scott, J.; Molloy, A.; Evans, J.G. Low Vitamin B-12 Status and Risk of Cognitive Decline in Older Adults. Am. J. Clin. Nutr. 2007, 86, 1384–1391. [Google Scholar] [CrossRef]
- Weisberg, I.; Tran, P.; Christensen, B.; Sibani, S.; Rozen, R. A Second Genetic Polymorphism in Methylenetetrahydrofolate Reductase (MTHFR) Associated with Decreased Enzyme Activity. Mol. Genet. Metab. 1998, 64, 169–172. [Google Scholar] [CrossRef]
- Mansouri, L.; Fekih-Mrissa, N.; Klai, S.; Mansour, M.; Gritli, N.; Mrissa, R. Association of Methylenetetrahydrofolate Reductase Polymorphisms with Susceptibility to Alzheimer’s Disease. Clin. Neurol. Neurosurg. 2013, 115, 1693–1696. [Google Scholar] [CrossRef]
- Wakutani, Y.; Kowa, H.; Kusumi, M.; Nakaso, K.; Yasui, K.-I.; Isoe-Wada, K.; Yano, H.; Urakami, K.; Takeshima, T.; Nakashima, K. A Haplotype of the Methylenetetrahydrofolate Reductase Gene Is Protective against Late-Onset Alzheimer’s Disease. Neurobiol. Aging 2004, 25, 291–294. [Google Scholar] [CrossRef]
- Smith, A.D.; Smith, S.M.; de Jager, C.A.; Whitbread, P.; Johnston, C.; Agacinski, G.; Oulhaj, A.; Bradley, K.M.; Jacoby, R.; Refsum, H. Homocysteine-Lowering by B Vitamins Slows the Rate of Accelerated Brain Atrophy in Mild Cognitive Impairment: A Randomized Controlled Trial. PLoS ONE 2010, 5, e12244. [Google Scholar] [CrossRef]
- Douaud, G.; Refsum, H.; de Jager, C.A.; Jacoby, R.; Nichols, T.E.; Smith, S.M.; Smith, A.D. Preventing Alzheimer’s Disease-Related Gray Matter Atrophy by B-Vitamin Treatment. Proc. Natl. Acad. Sci. USA 2013, 110, 9523–9528. [Google Scholar] [CrossRef]
- Hekmatdoost, A.; Vahid, F.; Yari, Z.; Sadeghi, M.; Eini-Zinab, H.; Lakpour, N.; Arefi, S. Methyltetrahydrofolate vs. Folic Acid Supplementation in Idiopathic Recurrent Miscarriage with Respect to Methylenetetrahydrofolate Reductase C677T and A1298C Polymorphisms: A Randomized Controlled Trial. PLoS ONE 2015, 10, e0143569. [Google Scholar] [CrossRef]
- Schellenberg, G.D.; Bird, T.D.; Wijsman, E.M.; Orr, H.T.; Anderson, L.; Nemens, E.; White, J.A.; Bonnycastle, L.; Weber, J.L.; Alonso, M.E. Genetic Linkage Evidence for a Familial Alzheimer’s Disease Locus on Chromosome 14. Science 1992, 258, 668–671. [Google Scholar] [CrossRef]
- Van Broeckhoven, C.; Backhovens, H.; Cruts, M.; de Winter, G.; Bruyland, M.; Cras, P.; Martin, J.J. Mapping of a Gene Predisposing to Early-Onset Alzheimer’s Disease to Chromosome 14q24.3. Nat. Genet. 1992, 2, 335–339. [Google Scholar] [CrossRef]
- Sherrington, R.; Rogaev, E.I.; Liang, Y.; Rogaeva, E.A.; Levesque, G.; Ikeda, M.; Chi, H.; Lin, C.; Li, G.; Holman, K.; et al. Cloning of a Gene Bearing Missense Mutations in Early-Onset Familial Alzheimer’s Disease. Nature 1995, 375, 754–760. [Google Scholar] [CrossRef]
- Steiner, H.; Fluhrer, R.; Haass, C. Intramembrane Proteolysis by Gamma-Secretase. J. Biol. Chem. 2008, 283, 29627–29631. [Google Scholar] [CrossRef]
- Scheuner, D.; Eckman, C.; Jensen, M.; Song, X.; Citron, M.; Suzuki, N.; Bird, T.D.; Hardy, J.; Hutton, M.; Kukull, W.; et al. Secreted Amyloid Beta-Protein Similar to That in the Senile Plaques of Alzheimer’s Disease Is Increased in Vivo by the Presenilin 1 and 2 and APP Mutations Linked to Familial Alzheimer’s Disease. Nat. Med. 1996, 2, 864–870. [Google Scholar] [CrossRef]
- Levy-Lahad, E.; Wasco, W.; Poorkaj, P.; Romano, D.M.; Oshima, J.; Pettingell, W.H.; Yu, C.E.; Jondro, P.D.; Schmidt, S.D.; Wang, K. Candidate Gene for the Chromosome 1 Familial Alzheimer’s Disease Locus. Science 1995, 269, 973–977. [Google Scholar] [CrossRef]
- Campion, D.; Dumanchin, C.; Hannequin, D.; Dubois, B.; Belliard, S.; Puel, M.; Thomas-Anterion, C.; Michon, A.; Martin, C.; Charbonnier, F.; et al. Early-Onset Autosomal Dominant Alzheimer Disease: Prevalence, Genetic Heterogeneity, and Mutation Spectrum. Am. J. Hum. Genet. 1999, 65, 664–670. [Google Scholar] [CrossRef]
- Jiang, H.; Jayadev, S.; Lardelli, M.; Newman, M. A Review of the Familial Alzheimer’s Disease Locus PRESENILIN 2 and Its Relationship to PRESENILIN 1. J. Alzheimer’s Dis. 2018, 66, 1323–1339. [Google Scholar] [CrossRef]
- De Strooper, B.; Iwatsubo, T.; Wolfe, M.S. Presenilins and -Secretase: Structure, Function, and Role in Alzheimer Disease. Cold Spring Harb. Perspect. Med. 2012, 2, a006304. [Google Scholar] [CrossRef] [PubMed]
- Jayadev, S.; Leverenz, J.B.; Steinbart, E.; Stahl, J.; Klunk, W.; Yu, C.-E.; Bird, T.D. Alzheimer’s Disease Phenotypes and Genotypes Associated with Mutations in Presenilin 2. Brain J. Neurol. 2010, 133, 1143–1154. [Google Scholar] [CrossRef] [PubMed]
- Finckh, U.; Alberici, A.; Antoniazzi, M.; Benussi, L.; Fedi, V.; Giannini, C.; Gal, A.; Nitsch, R.M.; Binetti, G. Variable Expression of Familial Alzheimer Disease Associated with Presenilin 2 Mutation M239I. Neurology 2000, 54, 2006–2008. [Google Scholar] [CrossRef] [PubMed]
- Blauwendraat, C.; Wilke, C.; Jansen, I.E.; Schulte, C.; Simón-Sánchez, J.; Metzger, F.G.; Bender, B.; Gasser, T.; Maetzler, W.; Rizzu, P.; et al. Pilot Whole-Exome Sequencing of a German Early-Onset Alzheimer’s Disease Cohort Reveals a Substantial Frequency of PSEN2 Variants. Neurobiol. Aging 2016, 37, 208.e11–208.e17. [Google Scholar] [CrossRef] [PubMed]
- Yan, L.; Li, L.; Han, W.; Pan, B.; Xue, X.; Mei, B. Age-Related Neuropsychiatric Symptoms in Presenilins Conditional Double Knockout Mice. Brain Res. Bull. 2013, 97, 104–111. [Google Scholar] [CrossRef]
- Jayadev, S.; Case, A.; Alajajian, B.; Eastman, A.J.; Möller, T.; Garden, G.A. Presenilin 2 Influences MiR146 Level and Activity in Microglia. J. Neurochem. 2013, 127, 592–599. [Google Scholar] [CrossRef]
- Jayadev, S.; Case, A.; Eastman, A.J.; Nguyen, H.; Pollak, J.; Wiley, J.C.; Möller, T.; Morrison, R.S.; Garden, G.A. Presenilin 2 Is the Predominant γ-Secretase in Microglia and Modulates Cytokine Release. PLoS ONE 2010, 5, e15743. [Google Scholar] [CrossRef]
- Jun, G.R.; Chung, J.; Mez, J.; Barber, R.; Beecham, G.W.; Bennett, D.A.; Buxbaum, J.D.; Byrd, G.S.; Carrasquillo, M.M.; Crane, P.K.; et al. Transethnic Genome-Wide Scan Identifies Novel Alzheimer’s Disease Loci. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2017, 13, 727–738. [Google Scholar] [CrossRef]
- Patel, D.; Zhang, X.; Farrell, J.J.; Chung, J.; Stein, T.D.; Lunetta, K.L.; Farrer, L.A. Cell-Type-Specific Expression Quantitative Trait Loci Associated with Alzheimer Disease in Blood and Brain Tissue. Transl. Psychiatry 2021, 11, 250. [Google Scholar] [CrossRef]
- Moingeon, P. Biomarkers for Allergen Immunotherapy: A “Panoromic” View. Immunol. Allergy Clin. N. Am. 2016, 36, 161–179. [Google Scholar] [CrossRef]
- Currie, G.; Delles, C. Use of Biomarkers in the Evaluation and Treatment of Hypertensive Patients. Curr. Hypertens. Rep. 2016, 18, 54. [Google Scholar] [CrossRef]
- Comabella, M.; Sastre-Garriga, J.; Montalban, X. Precision Medicine in Multiple Sclerosis: Biomarkers for Diagnosis, Prognosis, and Treatment Response. Curr. Opin. Neurol. 2016, 29, 254–262. [Google Scholar] [CrossRef]
- Hambly, N.; Shimbori, C.; Kolb, M. Molecular Classification of Idiopathic Pulmonary Fibrosis: Personalized Medicine, Genetics and Biomarkers. Respirol. Carlton Vic 2015, 20, 1010–1022. [Google Scholar] [CrossRef]
- Pearson, E.R. Personalized Medicine in Diabetes: The Role of “omics” and Biomarkers. Diabet. Med. J. Br. Diabet. Assoc. 2016, 33, 712–717. [Google Scholar] [CrossRef]
- O’Bryant, S.E.; Xiao, G.; Zhang, F.; Edwards, M.; German, D.C.; Yin, X.; Como, T.; Reisch, J.; Huebinger, R.M.; Graff-Radford, N.; et al. Validation of a Serum Screen for Alzheimer’s Disease across Assay Platforms, Species, and Tissues. J. Alzheimer’s Dis. 2014, 42, 1325–1335. [Google Scholar] [CrossRef]
- DeMarshall, C.A.; Nagele, E.P.; Sarkar, A.; Acharya, N.K.; Godsey, G.; Goldwaser, E.L.; Kosciuk, M.; Thayasivam, U.; Han, M.; Belinka, B.; et al. Detection of Alzheimer’s Disease at Mild Cognitive Impairment and Disease Progression Using Autoantibodies as Blood-Based Biomarkers. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2016, 3, 51–62. [Google Scholar] [CrossRef]
- Winston, C.N.; Goetzl, E.J.; Akers, J.C.; Carter, B.S.; Rockenstein, E.M.; Galasko, D.; Masliah, E.; Rissman, R.A. Prediction of Conversion from Mild Cognitive Impairment to Dementia with Neuronally Derived Blood Exosome Protein Profile. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2016, 3, 63–72. [Google Scholar] [CrossRef]
- Guedes, J.R.; Santana, I.; Cunha, C.; Duro, D.; Almeida, M.R.; Cardoso, A.M.; de Lima, M.C.P.; Cardoso, A.L. MicroRNA Deregulation and Chemotaxis and Phagocytosis Impairment in Alzheimer’s Disease. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2016, 3, 7–17. [Google Scholar] [CrossRef]
- Tampubolon, G. Repeated Systemic Inflammation Was Associated with Cognitive Deficits in Older Britons. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2016, 3, 1–6. [Google Scholar] [CrossRef]
- Hu, W.T.; Chen-Plotkin, A.; Arnold, S.E.; Grossman, M.; Clark, C.M.; Shaw, L.M.; McCluskey, L.; Elman, L.; Karlawish, J.; Hurtig, H.I.; et al. Biomarker Discovery for Alzheimer’s Disease, Frontotemporal Lobar Degeneration, and Parkinson’s Disease. Acta Neuropathol. 2010, 120, 385–399. [Google Scholar] [CrossRef]
- Henchcliffe, C.; Dodel, R.; Beal, M.F. Biomarkers of Parkinson’s Disease and Dementia with Lewy Bodies. Prog. Neurobiol. 2011, 95, 601–613. [Google Scholar] [CrossRef] [PubMed]
- Heneka, M.T.; Kummer, M.P.; Latz, E. Innate Immune Activation in Neurodegenerative Disease. Nat. Rev. Immunol. 2014, 14, 463–477. [Google Scholar] [CrossRef] [PubMed]
- Durrenberger, P.F.; Fernando, F.S.; Kashefi, S.N.; Bonnert, T.P.; Seilhean, D.; Nait-Oumesmar, B.; Schmitt, A.; Gebicke-Haerter, P.J.; Falkai, P.; Grünblatt, E.; et al. Common Mechanisms in Neurodegeneration and Neuroinflammation: A BrainNet Europe Gene Expression Microarray Study. J. Neural Transm. 2015, 122, 1055–1068. [Google Scholar] [CrossRef] [PubMed]
- Duong, T.; Nikolaeva, M.; Acton, P.J. C-Reactive Protein-like Immunoreactivity in the Neurofibrillary Tangles of Alzheimer’s Disease. Brain Res. 1997, 749, 152–156. [Google Scholar] [CrossRef]
- O’Bryant, S.E.; Johnson, L.; Edwards, M.; Soares, H.; Devous, M.D.; Ross, S.; Rohlfing, G.; Hall, J.; Texas Alzheimer’s Research & Care Consortium. The Link between C-Reactive Protein and Alzheimer’s Disease among Mexican Americans. J. Alzheimer’s Dis. 2013, 34, 701–706. [Google Scholar] [CrossRef]
- Glass, C.K.; Saijo, K.; Winner, B.; Marchetto, M.C.; Gage, F.H. Mechanisms Underlying Inflammation in Neurodegeneration. Cell 2010, 140, 918–934. [Google Scholar] [CrossRef]
- Wyss-Coray, T.; Rogers, J. Inflammation in Alzheimer Disease—A Brief Review of the Basic Science and Clinical Literature. Cold Spring Harb. Perspect. Med. 2012, 2, a006346. [Google Scholar] [CrossRef]
- In’T Veld, B.A.; Ruitenberg, A.; Hofman, A.; Launer, L.J.; van Duijn, C.M.; Stijnen, T.; Breteler, M.M.; Stricker, B.H. Nonsteroidal Antiinflammatory Drugs and the Risk of Alzheimer’s Disease. N. Engl. J. Med. 2001, 345, 1515–1521. [Google Scholar] [CrossRef]
- Aisen, P.S.; Schafer, K.A.; Grundman, M.; Pfeiffer, E.; Sano, M.; Davis, K.L.; Farlow, M.R.; Jin, S.; Thomas, R.G.; Thal, L.J.; et al. Effects of Rofecoxib or Naproxen vs. Placebo on Alzheimer Disease Progression: A Randomized Controlled Trial. JAMA 2003, 289, 2819–2826. [Google Scholar] [CrossRef]
- Thal, L.J.; Ferris, S.H.; Kirby, L.; Block, G.A.; Lines, C.R.; Yuen, E.; Assaid, C.; Nessly, M.L.; Norman, B.A.; Baranak, C.C.; et al. A Randomized, Double-Blind, Study of Rofecoxib in Patients with Mild Cognitive Impairment. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2005, 30, 1204–1215. [Google Scholar] [CrossRef]
- Jones, L.; Holmans, P.A.; Hamshere, M.L.; Harold, D.; Moskvina, V.; Ivanov, D.; Pocklington, A.; Abraham, R.; Hollingworth, P.; Sims, R.; et al. Genetic Evidence Implicates the Immune System and Cholesterol Metabolism in the Aetiology of Alzheimer’s Disease. PLoS ONE 2010, 5, e13950. [Google Scholar] [CrossRef]
- O’Bryant, S.E.; Gupta, V.; Henriksen, K.; Edwards, M.; Jeromin, A.; Lista, S.; Bazenet, C.; Soares, H.; Lovestone, S.; Hampel, H.; et al. Guidelines for the Standardization of Preanalytic Variables for Blood-Based Biomarker Studies in Alzheimer’s Disease Research. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2015, 11, 549–560. [Google Scholar] [CrossRef]
- Li, M.; Yu, T.; Hu, Y.-F. The Impact of Companion Diagnostic Device Measurement Performance on Clinical Validation of Personalized Medicine. Stat. Med. 2015, 34, 2222–2234. [Google Scholar] [CrossRef]
- Li, M. Statistical Consideration and Challenges in Bridging Study of Personalized Medicine. J. Biopharm. Stat. 2015, 25, 397–407. [Google Scholar] [CrossRef]
- Hampel, H.; Vassar, R.; de Strooper, B.; Hardy, J.; Willem, M.; Singh, N.; Zhou, J.; Yan, R.; Vanmechelen, E.; de Vos, A.; et al. The β-Secretase BACE1 in Alzheimer’s Disease. Biol. Psychiatry 2021, 89, 745–756. [Google Scholar] [CrossRef]
- Janeiro, M.H.; Ardanaz, C.G.; Sola-Sevilla, N.; Dong, J.; Cortés-Erice, M.; Solas, M.; Puerta, E.; Ramírez, M.J. Biomarkers in Alzheimer’s Disease. Adv. Lab. Med. Av. En Med. Lab. 2021, 2, 27–37. [Google Scholar] [CrossRef]
- Urbanelli, L.; Magini, A.; Ciccarone, V.; Trivelli, F.; Polidoro, M.; Tancini, B.; Emiliani, C. New Perspectives for the Diagnosis of Alzheimer’s Disease. Recent Patents CNS Drug Discov. 2009, 4, 160–181. [Google Scholar] [CrossRef]
- Brier, M.R.; Gordon, B.; Friedrichsen, K.; McCarthy, J.; Stern, A.; Christensen, J.; Owen, C.; Aldea, P.; Su, Y.; Hassenstab, J.; et al. Tau and Aβ Imaging, CSF Measures, and Cognition in Alzheimer’s Disease. Sci. Transl. Med. 2016, 8, 338ra66. [Google Scholar] [CrossRef]
- Ferreira, L.K.; Busatto, G.F. Neuroimaging in Alzheimer’s Disease: Current Role in Clinical Practice and Potential Future Applications. Clin. Sao Paulo Braz. 2011, 66 (Suppl. S1), 19–24. [Google Scholar] [CrossRef]
- Herholz, K.; Ebmeier, K. Clinical Amyloid Imaging in Alzheimer’s Disease. Lancet Neurol. 2011, 10, 667–670. [Google Scholar] [CrossRef]
- Isaac, M.; Vamvakas, S.; Abadie, E.; Jonsson, B.; Gispen, C.; Pani, L. Qualification Opinion of Novel Methodologies in the Predementia Stage of Alzheimer’s Disease: Cerebro-Spinal-Fluid Related Biomarkers for Drugs Affecting Amyloid Burden—Regulatory Considerations by European Medicines Agency Focusing in Improving Benefit/Risk in Regulatory Trials. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2011, 21, 781–788. [Google Scholar] [CrossRef]
- Shaw, L.M.; Vanderstichele, H.; Knapik-Czajka, M.; Clark, C.M.; Aisen, P.S.; Petersen, R.C.; Blennow, K.; Soares, H.; Simon, A.; Lewczuk, P.; et al. Cerebrospinal Fluid Biomarker Signature in Alzheimer’s Disease Neuroimaging Initiative Subjects. Ann. Neurol. 2009, 65, 403–413. [Google Scholar] [CrossRef] [PubMed]
- Mulder, C.; Verwey, N.A.; van der Flier, W.M.; Bouwman, F.H.; Kok, A.; van Elk, E.J.; Scheltens, P.; Blankenstein, M.A. Amyloid-Beta(1-42), Total Tau, and Phosphorylated Tau as Cerebrospinal Fluid Biomarkers for the Diagnosis of Alzheimer Disease. Clin. Chem. 2010, 56, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Buchhave, P.; Minthon, L.; Zetterberg, H.; Wallin, A.K.; Blennow, K.; Hansson, O. Cerebrospinal Fluid Levels of β-Amyloid 1-42, but Not of Tau, Are Fully Changed Already 5 to 10 Years before the Onset of Alzheimer Dementia. Arch. Gen. Psychiatry 2012, 69, 98–106. [Google Scholar] [CrossRef]
- Bateman, R.J.; Xiong, C.; Benzinger, T.L.S.; Fagan, A.M.; Goate, A.; Fox, N.C.; Marcus, D.S.; Cairns, N.J.; Xie, X.; Blazey, T.M.; et al. Clinical and Biomarker Changes in Dominantly Inherited Alzheimer’s Disease. N. Engl. J. Med. 2012, 367, 795–804. [Google Scholar] [CrossRef]
- Wong, D.F.; Rosenberg, P.B.; Zhou, Y.; Kumar, A.; Raymont, V.; Ravert, H.T.; Dannals, R.F.; Nandi, A.; Brasić, J.R.; Ye, W.; et al. In Vivo Imaging of Amyloid Deposition in Alzheimer Disease Using the Radioligand 18F-AV-45 (Florbetapir [Corrected] F 18). J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2010, 51, 913–920. [Google Scholar] [CrossRef]
- Fleisher, A.S.; Chen, K.; Liu, X.; Roontiva, A.; Thiyyagura, P.; Ayutyanont, N.; Joshi, A.D.; Clark, C.M.; Mintun, M.A.; Pontecorvo, M.J.; et al. Using Positron Emission Tomography and Florbetapir F18 to Image Cortical Amyloid in Patients with Mild Cognitive Impairment or Dementia Due to Alzheimer Disease. Arch. Neurol. 2011, 68, 1404–1411. [Google Scholar] [CrossRef]
- Rodrigue, K.M.; Kennedy, K.M.; Devous, M.D.; Rieck, J.R.; Hebrank, A.C.; Diaz-Arrastia, R.; Mathews, D.; Park, D.C. β-Amyloid Burden in Healthy Aging: Regional Distribution and Cognitive Consequences. Neurology 2012, 78, 387–395. [Google Scholar] [CrossRef]
- Quigley, H.; Colloby, S.J.; O’Brien, J.T. PET Imaging of Brain Amyloid in Dementia: A Review. Int. J. Geriatr. Psychiatry 2011, 26, 991–999. [Google Scholar] [CrossRef]
- Grundman, M.; Pontecorvo, M.J.; Salloway, S.P.; Doraiswamy, P.M.; Fleisher, A.S.; Sadowsky, C.H.; Nair, A.K.; Siderowf, A.; Lu, M.; Arora, A.K.; et al. Potential Impact of Amyloid Imaging on Diagnosis and Intended Management in Patients with Progressive Cognitive Decline. Alzheimer Dis. Assoc. Disord. 2013, 27, 4–15. [Google Scholar] [CrossRef]
- Doraiswamy, P.M.; Sperling, R.A.; Johnson, K.; Reiman, E.M.; Wong, T.Z.; Sabbagh, M.N.; Sadowsky, C.H.; Fleisher, A.S.; Carpenter, A.; Joshi, A.D.; et al. Florbetapir F 18 Amyloid PET and 36-Month Cognitive Decline: A Prospective Multicenter Study. Mol. Psychiatry 2014, 19, 1044–1051. [Google Scholar] [CrossRef]
- Johnson, K.A.; Schultz, A.; Betensky, R.A.; Becker, J.A.; Sepulcre, J.; Rentz, D.; Mormino, E.; Chhatwal, J.; Amariglio, R.; Papp, K.; et al. Tau Positron Emission Tomographic Imaging in Aging and Early Alzheimer Disease. Ann. Neurol. 2016, 79, 110–119. [Google Scholar] [CrossRef]
- Schwarz, A.J.; Yu, P.; Miller, B.B.; Shcherbinin, S.; Dickson, J.; Navitsky, M.; Joshi, A.D.; Devous, M.D.; Mintun, M.S. Regional Profiles of the Candidate Tau PET Ligand 18F-AV-1451 Recapitulate Key Features of Braak Histopathological Stages. Brain J. Neurol. 2016, 139, 1539–1550. [Google Scholar] [CrossRef]
- Vineis, P.; Chadeau-Hyam, M.; Gmuender, H.; Gulliver, J.; Herceg, Z.; Kleinjans, J.; Kogevinas, M.; Kyrtopoulos, S.; Nieuwenhuijsen, M.; Phillips, D.H.; et al. The Exposome in Practice: Design of the EXPOsOMICS Project. Int. J. Hyg. Environ. Health 2017, 220, 142–151. [Google Scholar] [CrossRef]
- Van Assen, M.; Lee, S.J.; de Cecco, C.N. Artificial Intelligence from A to Z: From Neural Network to Legal Framework. Eur. J. Radiol. 2020, 129, 109083. [Google Scholar] [CrossRef]
- He, J.; Baxter, S.L.; Xu, J.; Xu, J.; Zhou, X.; Zhang, K. The Practical Implementation of Artificial Intelligence Technologies in Medicine. Nat. Med. 2019, 25, 30–36. [Google Scholar] [CrossRef]
- Ehteshami Bejnordi, B.; Veta, M.; Johannes van Diest, P.; van Ginneken, B.; Karssemeijer, N.; Litjens, G.; van der Laak, J.A.W.M.; the CAMELYON16 Consortium; Hermsen, M.; Manson, Q.F.; et al. Diagnostic Assessment of Deep Learning Algorithms for Detection of Lymph Node Metastases in Women With Breast Cancer. JAMA 2017, 318, 2199–2210. [Google Scholar] [CrossRef]
- Esteva, A.; Kuprel, B.; Novoa, R.A.; Ko, J.; Swetter, S.M.; Blau, H.M.; Thrun, S. Dermatologist-Level Classification of Skin Cancer with Deep Neural Networks. Nature 2017, 542, 115–118. [Google Scholar] [CrossRef]
- Poplin, R.; Varadarajan, A.V.; Blumer, K.; Liu, Y.; McConnell, M.V.; Corrado, G.S.; Peng, L.; Webster, D.R. Prediction of Cardiovascular Risk Factors from Retinal Fundus Photographs via Deep Learning. Nat. Biomed. Eng. 2018, 2, 158–164. [Google Scholar] [CrossRef]
- Ardila, D.; Kiraly, A.P.; Bharadwaj, S.; Choi, B.; Reicher, J.J.; Peng, L.; Tse, D.; Etemadi, M.; Ye, W.; Corrado, G.; et al. End-to-End Lung Cancer Screening with Three-Dimensional Deep Learning on Low-Dose Chest Computed Tomography. Nat. Med. 2019, 25, 954–961. [Google Scholar] [CrossRef]
- Yala, A.; Lehman, C.; Schuster, T.; Portnoi, T.; Barzilay, R. A Deep Learning Mammography-Based Model for Improved Breast Cancer Risk Prediction. Radiology 2019, 292, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Gerke, S.; Babic, B.; Evgeniou, T.; Cohen, I.G. The Need for a System View to Regulate Artificial Intelligence/Machine Learning-Based Software as Medical Device. NPJ Digit. Med. 2020, 3, 53. [Google Scholar] [CrossRef] [PubMed]
- Ho, D.; Quake, S.R.; McCabe, E.R.B.; Chng, W.J.; Chow, E.K.; Ding, X.; Gelb, B.D.; Ginsburg, G.S.; Hassenstab, J.; Ho, C.-M.; et al. Enabling Technologies for Personalized and Precision Medicine. Trends Biotechnol. 2020, 38, 497–518. [Google Scholar] [CrossRef] [PubMed]
- Zitnik, M.; Nguyen, F.; Wang, B.; Leskovec, J.; Goldenberg, A.; Hoffman, M.M. Machine Learning for Integrating Data in Biology and Medicine: Principles, Practice, and Opportunities. Int. J. Inf. Fusion 2019, 50, 71–91. [Google Scholar] [CrossRef] [PubMed]
- Bycroft, C.; Freeman, C.; Petkova, D.; Band, G.; Elliott, L.T.; Sharp, K.; Motyer, A.; Vukcevic, D.; Delaneau, O.; O’Connell, J.; et al. The UK Biobank Resource with Deep Phenotyping and Genomic Data. Nature 2018, 562, 203–209. [Google Scholar] [CrossRef]
- Perkins, B.A.; Caskey, C.T.; Brar, P.; Dec, E.; Karow, D.S.; Kahn, A.M.; Hou, Y.-C.C.; Shah, N.; Boeldt, D.; Coughlin, E.; et al. Precision Medicine Screening Using Whole-Genome Sequencing and Advanced Imaging to Identify Disease Risk in Adults. Proc. Natl. Acad. Sci. USA 2018, 115, 3686–3691. [Google Scholar] [CrossRef]
- Price, N.D.; Magis, A.T.; Earls, J.C.; Glusman, G.; Levy, R.; Lausted, C.; McDonald, D.T.; Kusebauch, U.; Moss, C.L.; Zhou, Y.; et al. A Wellness Study of 108 Individuals Using Personal, Dense, Dynamic Data Clouds. Nat. Biotechnol. 2017, 35, 747–756. [Google Scholar] [CrossRef]
- Schüssler-Fiorenza Rose, S.M.; Contrepois, K.; Moneghetti, K.J.; Zhou, W.; Mishra, T.; Mataraso, S.; Dagan-Rosenfeld, O.; Ganz, A.B.; Dunn, J.; Hornburg, D.; et al. A Longitudinal Big Data Approach for Precision Health. Nat. Med. 2019, 25, 792–804. [Google Scholar] [CrossRef]
- Ahmed, Z.; Mohamed, K.; Zeeshan, S.; Dong, X. Artificial Intelligence with Multi-Functional Machine Learning Platform Development for Better Healthcare and Precision Medicine. Database J. Biol. Databases Curation 2020, 2020, baaa010. [Google Scholar] [CrossRef]
- Ashkenazy, R. Precision Medical Communication to Optimize Stakeholder Information Exchange: A “4M-Quadrant” Approach. Drug Discov. Today 2016, 21, 1039–1041. [Google Scholar] [CrossRef]
- Walter, W.; Pfarr, N.; Meggendorfer, M.; Jost, P.; Haferlach, T.; Weichert, W. Next-Generation Diagnostics for Precision Oncology: Preanalytical Considerations, Technical Challenges, and Available Technologies. Semin. Cancer Biol. 2022, 84, 3–15. [Google Scholar] [CrossRef]
- Hammack, C.M.; Brelsford, K.M.; Beskow, L.M. Thought Leader Perspectives on Participant Protections in Precision Medicine Research. J. Law Med. Ethics J. Am. Soc. Law Med. Ethics 2019, 47, 134–148. [Google Scholar] [CrossRef]
- Shomron, N. Prioritizing Personalized Medicine. Genet. Res. 2014, 96, e007. [Google Scholar] [CrossRef]
- Thomas, S.M. Society and Ethics—The Genetics of Disease. Curr. Opin. Genet. Dev. 2004, 14, 287–291. [Google Scholar] [CrossRef]
- Gurwitz, D.; Lunshof, J.E.; Altman, R.B. A Call for the Creation of Personalized Medicine Databases. Nat. Rev. Drug Discov. 2006, 5, 23–26. [Google Scholar] [CrossRef]
- Simmons, S.; Sahinalp, C.; Berger, B. Enabling Privacy-Preserving GWASs in Heterogeneous Human Populations. Cell Syst. 2016, 3, 54–61. [Google Scholar] [CrossRef]
- McGonigle, I.V. The Collective Nature of Personalized Medicine. Genet. Res. 2016, 98, e3. [Google Scholar] [CrossRef]
- OECD. Dementia Research and Care: Can Big Data Help? Anderson, G., Oderkirk, J., Eds.; OECD: Paris, France, 2015; ISBN 978-92-64-22841-2. [Google Scholar]
- Collins, F.S.; Varmus, H. A New Initiative on Precision Medicine. N. Engl. J. Med. 2015, 372, 793–795. [Google Scholar] [CrossRef]
- Enhancing Translational Research and Clinical Development for Alzheimer’s Disease and Other Dementias; OECD Science, Technology and Industry Policy Papers; OECD: Paris, France, 2015; Volume 22.
- Chun, M.Y.; Park, C.J.; Kim, J.; Jeong, J.H.; Jang, H.; Kim, K.; Seo, S.W. Prediction of Conversion to Dementia Using Interpretable Machine Learning in Patients with Amnestic Mild Cognitive Impairment. Front. Aging Neurosci. 2022, 14, 898940. [Google Scholar] [CrossRef]
- Fowler, C.; Rainey-Smith, S.R.; Bird, S.; Bomke, J.; Bourgeat, P.; Brown, B.M.; Burnham, S.C.; Bush, A.I.; Chadunow, C.; Collins, S.; et al. Fifteen Years of the Australian Imaging, Biomarkers and Lifestyle (AIBL) Study: Progress and Observations from 2359 Older Adults Spanning the Spectrum from Cognitive Normality to Alzheimer’s Disease. J. Alzheimer’s Dis. Rep. 2021, 5, 443–468. [Google Scholar] [CrossRef]
- Lombardi, G.; Crescioli, G.; Cavedo, E.; Lucenteforte, E.; Casazza, G.; Bellatorre, A.-G.; Lista, C.; Costantino, G.; Frisoni, G.; Virgili, G.; et al. Structural Magnetic Resonance Imaging for the Early Diagnosis of Dementia Due to Alzheimer’s Disease in People with Mild Cognitive Impairment. Cochrane Database Syst. Rev. 2020, 3, CD009628. [Google Scholar] [CrossRef] [PubMed]
- La Joie, R.; Visani, A.V.; Baker, S.L.; Brown, J.A.; Bourakova, V.; Cha, J.; Chaudhary, K.; Edwards, L.; Iaccarino, L.; Janabi, M.; et al. Prospective Longitudinal Atrophy in Alzheimer’s Disease Correlates with the Intensity and Topography of Baseline Tau-PET. Sci. Transl. Med. 2020, 12, eaau5732. [Google Scholar] [CrossRef] [PubMed]
- Ginsburg, G.S.; Phillips, K.A. Precision Medicine: From Science to Value. Health Aff. 2018, 37, 694–701. [Google Scholar] [CrossRef] [PubMed]

| S.No. | Biological Marker | Description | Depiction | Cerebrospinal Fluid | Diagnostic Efficiency |
|---|---|---|---|---|---|
| 1. | Aβ42/Aβ40 | Aβ involves the processing of the amyloid precursor protein (APP) by enzymes called β-secretase and γ-secretase. These enzymes cleave APP to form Aβ peptides of varying lengths, with the most common being Aβ40 and Aβ42. The Aβ peptides can then aggregate to form amyloid plaques. | APP metabolism marker | A lower level is present in AD patients. | Indicated for diagnosing CSF. |
| 2. | Aβ38 | Aβ38 is a specific form of the Aβ peptide. Aβ peptides are generated through the cleavage of the APP by enzymes called beta-secretase and gamma-secretase. Aβ38 is a less common form of the Aβ peptide compared to the more prevalent Aβ40 and Aβ42. | APP metabolism marker. | No variations between groups. | Not really helpful on its own. May be useful in separating AD from dementias that are closely similar to AD. |
| 3. | sAPPα | sAPPα (soluble amyloid precursor protein alpha) is a fragment of the APP that is generated by the action of the α-secretase enzyme. This enzyme cleaves APP at a different site than the β-secretase and γ-secretase enzymes, which results in the production of different set of peptides. | APP cleavage product. | No variations between groups. | Not really helpful on its own. |
| 4. | sAPPβ | sAPPβ (soluble amyloid precursor protein beta) is a fragment of the APP that is generated by the action of the beta-secretase enzyme. This enzyme cleaves APP at a specific site, releasing sAPPβ and the C-terminal fragment (CTF) of APP. | APP cleavage product. | No variations between groups. | Not really helpful on its own. |
| 5. | t-Tau and p-Tau | Tau protein is a microtubule-associated protein that is found in neurons and is important for the stability and function of microtubules. | Markers connected to memory difficulties. | A higher level is present in AD patients. | P-tau is a hallmark of AD. Indicated for diagnosing CSF. |
| 6. | NFL | NFL protein is a type of intermediate filament protein that is found in the neurons of the nervous system. It is an important component of the cytoskeleton, which provides structural support for the cell. NFL protein is part of a group of neurofilament proteins that also includes neurofilament medium chain (NFM) and neurofilament heavy chain (NFH) proteins. | Neurodegeneration-related biomarker. | A higher level is present in AD patients. | Indicated for diagnosing CSF. |
| 7. | NSE | NSE is a protein that is found in high concentrations in neurons and neuroendocrine cells. It is an enzyme that plays a role in the metabolism of glucose and is considered to be a marker of neuronal damage. | Neurodegeneration-related biomarker. | A higher level is present in AD patients. | Possibly helpful for diagnosing CSF. |
| 8. | MCP-1 | MCP-1 is a small protein that is known to be involved in the recruitment of immune cells, specifically monocytes, to sites of inflammation and injury. MCP-1 may contribute to the accumulation of amyloid beta, which is a hallmark of AD. | Glial activation marker. | A higher level is present in AD patients. | Not really helpful on its own. |
| 9. | VLP-1 | VLP-1 1 is a protein that is found in the retina and is a member of the visinin-like protein family. VLP-1 is expressed in the inner segments of rod and cone photoreceptor cells, where it is involved in the regulation of intracellular calcium levels. VLP-1 is also found in the brain, where it may have a role in synaptic plasticity and learning. | Neurodegeneration-related biomarker. | A higher level is present in AD patients. | Possibly helpful for diagnosing CSF. |
| 10. | HFABP | HFABP is a small, cytosolic protein that is found in high concentrations in the heart and other tissues. It binds long-chain fatty acids and is involved in the intracellular transport and metabolism of fatty acids. | Neurodegeneration-related biomarker. | A higher level is present in AD patients. | Possibly helpful for diagnosing CSF. |
| 11. | GFAP | The accumulation of Aβ and tau protein, which are the hallmarks of AD, are known to cause astrocyte activation and increase the expression of GFAP. This suggests that astrocyte activation may play a role in the development of AD. | Glial activation marker. | No variations between groups. | Not really helpful on its own. |
| 12. | Neurogranin | Neurogranin is a protein that is primarily found in the brain and is thought to play a role in synaptic plasticity and memory formation. It’s a postsynaptic protein and is found to be associated with N-methyl-D-aspartate (NMDA) receptors, which are important for synaptic plasticity and memory formation. | Synapse degeneration marker. | A higher level is present in AD patients. | Particular to AD. High potential but little published studies. |
| 13. | α-Synuclein | α-synuclein is a protein primarily found in the brain and it’s known to be involved in the regulation of neurotransmitters release and synaptic function. | Protein at presynapse. | A higher level is present in AD patients. | Not really helpful on its own. Most studies are carried out with likely AD individuals. |
| 14. | sTREM2 | The accumulation of Aβ, which is a hallmark of AD, is known to activate microglia, and it is thought that the increased sTREM2 levels may be a result of this activation. | Neurodegeneration-related biomarker. | A higher level is present in AD patients. | Possibly helpful for diagnosing CSF. Little published studies |
| Name of the Project | Objective | Country |
|---|---|---|
| Australian Genomics Health Alliance | Create a national framework for integrating guidance on reporting results from clinical testing and genomics research into clinical study and experimentation. | Australia |
| Belgian Medical Genomics Initiative | Anticipate health outcomes using genomic data and carry out a pilot project in Belgium to integrate genomic data into clinical care. | Belgium |
| Genome Canada | Conduct extensive studies examining the use of genomics in the field of precision medicine. A decision-based, evidence-based strategy to healthcare and general health might be described as precision health. | Canada |
| Estonian Program for Personal Medicine | Sequence 5000 individuals, create an Estonian genotyping array, test it on 50,000 Estonian Biobank participants, make it available to all adults aged 35 to 65 (about 500,000 individuals), and connect it to the EMR. | Estonia |
| Plan France Medecine Genomique 2025 | Utilize the combination of patient care, education, and research to provide everyone with access to genetic medicine. | France |
| Bench-to-Bedside Project | 100,000 Israeli genomes from chosen patients will be sequenced. | Israel |
| Implementation of Genomic Medicine Project | Utilize genomics for the best possible diagnosis, care, and prevention. | Japan |
| Genome Technology to Business Translation Program | Subsequent developments treatment and diagnosis methods for personalised and preventive medicine using genomes. | Korea |
| Centre for Systems Biomedicine | Prioritize early Parkinson disease diagnosis and classification. | Luxembourg |
| Personalized OMIC Lattice for Advanced Research and Improving Stratification | Develop a 90-gene panel for gastrointestinal malignancies after implementing a TGFBI gene testing pilot for diagnosis of diseases and family risk evaluation in stromal corneal dystrophies. | Singapore |
| Pharmacogenomics Network | Use pharmacogenomics cards in conjunction with a national pharmacovigilance programme to determine the risks. | Thailand |
| Genomics England | To better comprehend cancer, uncommon disorders, and infectious diseases, 100,000 whole genomes will be sequenced and linked to National Health Service information. | United Kingdom |
| All of Us Research Program | To advance scientific research and clinical treatment, enrol one million participants who are representative of the community and share data from their EMRs, digital health technologies, and genomics. | United States |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arafah, A.; Khatoon, S.; Rasool, I.; Khan, A.; Rather, M.A.; Abujabal, K.A.; Faqih, Y.A.H.; Rashid, H.; Rashid, S.M.; Bilal Ahmad, S.; et al. The Future of Precision Medicine in the Cure of Alzheimer’s Disease. Biomedicines 2023, 11, 335. https://doi.org/10.3390/biomedicines11020335
Arafah A, Khatoon S, Rasool I, Khan A, Rather MA, Abujabal KA, Faqih YAH, Rashid H, Rashid SM, Bilal Ahmad S, et al. The Future of Precision Medicine in the Cure of Alzheimer’s Disease. Biomedicines. 2023; 11(2):335. https://doi.org/10.3390/biomedicines11020335
Chicago/Turabian StyleArafah, Azher, Saima Khatoon, Iyman Rasool, Andleeb Khan, Mashoque Ahmad Rather, Khaled Abdullah Abujabal, Yazid Abdullilah Hassan Faqih, Hina Rashid, Shahzada Mudasir Rashid, Sheikh Bilal Ahmad, and et al. 2023. "The Future of Precision Medicine in the Cure of Alzheimer’s Disease" Biomedicines 11, no. 2: 335. https://doi.org/10.3390/biomedicines11020335
APA StyleArafah, A., Khatoon, S., Rasool, I., Khan, A., Rather, M. A., Abujabal, K. A., Faqih, Y. A. H., Rashid, H., Rashid, S. M., Bilal Ahmad, S., Alexiou, A., & Rehman, M. U. (2023). The Future of Precision Medicine in the Cure of Alzheimer’s Disease. Biomedicines, 11(2), 335. https://doi.org/10.3390/biomedicines11020335






