Gut–Kidney–Heart: A Novel Trilogy
Abstract
:1. Introduction
2. Gut Microbiota and Immunity
| Roles of the Gut Microbiota | References |
|---|---|
| Digestion of indigestible plant polysaccharides | [22] |
| Synthesis of vitamins and necessary amino acids | [22] |
| Metabolism of drugs | [25] |
| Barrier on the apical surface of the intestinal epithelium against pathogens | [28] |
| Immune modulation: production of SCFAs, source of MAMPs, constitution of the GALT, induction of CCR-2 necessary for phagocytosis, differentiation and function of ILCs and lymphocytes | [29,31,35,40,42,43,44] |
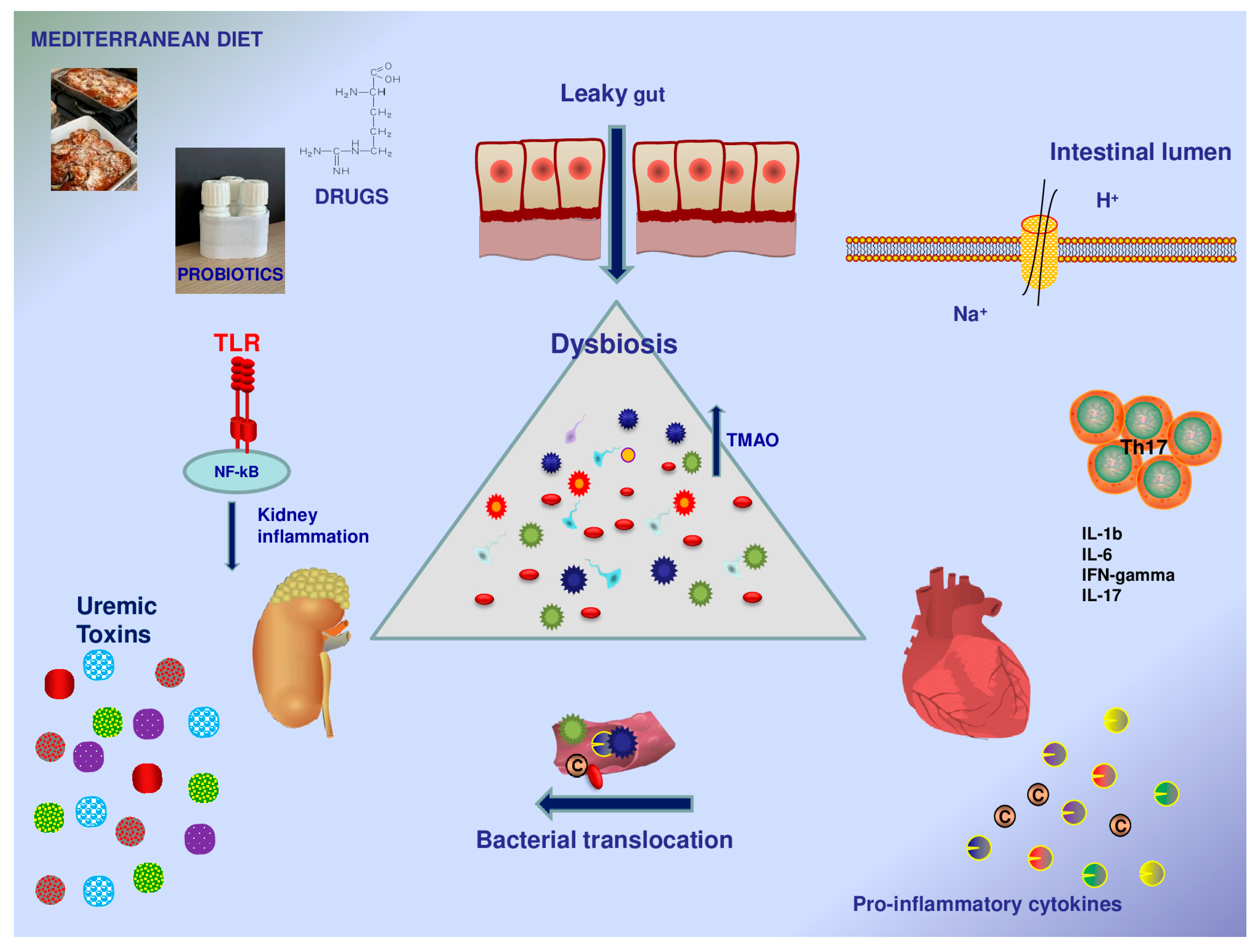
3. The Gut Hypothesis in Cardiovascular Disease
| Gut and Systemic Alterations | Cardiovascular Consequences | References |
|---|---|---|
| Dysbiosis; intestinal permeability Bacterial translocation; microbial metabolites Pro-inflammatory cytokines; chronic inflammation | Heart failure | [59,64,66] |
| Homeostasis of water and salts | [64,65] | |
| Atherosclerosis | [72,73] | |
| Myocardial fibrosis | [72,73] | |
| Coronary heart disease | [74,75,78] | |
| Hypertension | [77] | |
| Arrythmias | [79] |
4. Gut–Kidney Axis, a Bidirectional Talk
| Gut and Systemic Alterations | Kidney Disease | Microbial Changes | References |
|---|---|---|---|
| Uremic dysbiosis Leaky gut Hyperuricemia Uremic toxins Inflammation | CKD | Increased urease bacteria Increased pathogens (e.g., Enterobacteriaceae) producing uremic toxins Reduction in GM species diversity Increased Ruminococcus genus Increased Bifidobacteria Decreased Lactobacilli Prevalence of Veillonellaceae and Enterobacteriaceae and reduced presence of Eubacteriaceae (ESRD) | [90,92,95,99,100,101] |
| AKI | Increase in Escherichia spp. and Enterobacter spp. Decrease in Lactobacillus, Ruminococcaceae, Faecalibacterium, and Lachnospiraceae | [89,97] |
5. Gut, Kidney, and Heart: A Vicious Circle
6. Trimethylamine N-Oxide (TMAO) and Other GM Products
7. The Role of GM Modulation in the Gut–Kidney–Heart Axis
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| GM | Gut microbiota |
| GI | Gastrointestinal |
| LPS | Lipopolysaccharide |
| SCFAs | Short-chain fatty acids |
| GPCRs | G protein-coupled receptors |
| FFARs | Free fatty acid receptors |
| ROS | Reactive oxygen species |
| MAMPs | Microbe-associated molecular patterns |
| PRRs | Pattern recognition receptors |
| MALT | Mucosa-associated lymphoid tissue |
| GALT | Gut-associated lymphoid tissue |
| PAMPs | Pathogen-associated molecular patterns |
| TLRs | Toll-like receptors |
| APCs | Antigen presenting cells |
| CCR-2 | C-C chemokine receptor type 2 |
| HDACs | Histone deacetylases |
| IFNs | Interferons |
| IL | Interleukin |
| TNF | Tumor necrosis factor |
| ILCs | Innate lymphoid cells |
| HF | Heart failure |
| IP | Intestinal permeability |
| TMAO | Trimethylamine N-oxide |
| MMP | Matrix metalloproteinase |
| ICAM | Intercellular adhesion molecule |
| VCAM | Vascular cell adhesion molecule |
| CCR2 | Chemokine receptor type 2 |
| CCL2 | Chemokine ligand 2 |
| PAGln | Phenylacetyl glutamine |
| NT-proBNP | N-terminal pro-B-type natriuretic peptide |
| LVEF | Left ventricle ejection fraction |
| CHD | Coronary heart disease |
| NLRP3 | NOD-, LRR- and pyrin domain-containing protein 3 |
| CKD | Chronic kidney disease |
| TLR | Toll-like receptor |
| MyD88 | Myeloid differentiation primary response 88 |
| NF-kB | Nuclear factor kappa-light-chain-enhancer of activated B cells |
| MAP | Mitogen-activated protein |
| AKI | Acute kidney injury |
| ESRD | End-stage renal disease |
| NAFLD | Non-alcoholic fatty liver disease |
| JNK | C-Jun-N-terminal kinase |
| RAS | Renin angiotensin system |
| ACE | Angiotensin-converting enzyme |
| AT1R | Angiotensin II type 1 receptor |
| IAA | Indole acetic acid |
| IxS | Indoxyl sulfate |
| CAS | Carotid artery stenting |
| PAD | Peripheral artery disease |
| DMB | 3-dimethyl-1-butanol |
| MeD | Mediterranean diet |
| SGLT2i | Sodium glucose cotransporter 2 inhibitors |
| FMT | Fecal microbiota transplantation |
References
- Quigley, E.M.M. Microbiota-Brain-Gut Axis and Neurodegenerative Diseases. Curr. Neurol. Neurosci. Rep. 2017, 17, 94. [Google Scholar] [CrossRef]
- Huang, Y.; Xin, W.; Xiong, J.; Yao, M.; Zhang, B.; Zhao, J. The Intestinal Microbiota and Metabolites in the Gut-Kidney-Heart Axis of Chronic Kidney Disease. Front. Pharmacol. 2022, 13, 837500. [Google Scholar] [CrossRef]
- Rooks, M.G.; Garrett, W.S. Gut Microbiota, Metabolites and Host Immunity. Nat. Rev. Immunol. 2016, 16, 341–352. [Google Scholar] [CrossRef]
- Rivera, C.A.; Lennon-Duménil, A.-M. Gut Immune Cells and Intestinal Niche Imprinting. Semin. Cell Dev. Biol. 2023, 150–151, 50–57. [Google Scholar] [CrossRef]
- Cianci, R.; Franza, L.; Schinzari, G.; Rossi, E.; Ianiro, G.; Tortora, G.; Gasbarrini, A.; Gambassi, G.; Cammarota, G. The Interplay between Immunity and Microbiota at Intestinal Immunological Niche: The Case of Cancer. Int. J. Mol. Sci. 2019, 20, 501. [Google Scholar] [CrossRef]
- Doe, W.F. The Intestinal Immune System. Gut 1989, 30, 1679–1685. [Google Scholar] [CrossRef]
- Anders, H.-J.; Andersen, K.; Stecher, B. The Intestinal Microbiota, a Leaky Gut, and Abnormal Immunity in Kidney Disease. Kidney Int. 2013, 83, 1010–1016. [Google Scholar] [CrossRef]
- Cigarran Guldris, S.; González Parra, E.; Cases Amenós, A. Gut Microbiota in Chronic Kidney Disease. Nefrol. Publicacion Of. Soc. Esp. Nefrol. 2017, 37, 9–19. [Google Scholar] [CrossRef]
- Glorieux, G.; Nigam, S.K.; Vanholder, R.; Verbeke, F. Role of the Microbiome in Gut-Heart-Kidney Cross Talk. Circ. Res. 2023, 132, 1064–1083. [Google Scholar] [CrossRef]
- Suganya, K.; Son, T.; Kim, K.-W.; Koo, B.-S. Impact of Gut Microbiota: How It Could Play Roles beyond the Digestive System on Development of Cardiovascular and Renal Diseases. Microb. Pathog. 2021, 152, 104583. [Google Scholar] [CrossRef]
- Scarpellini, E.; Ianiro, G.; Attili, F.; Bassanelli, C.; De Santis, A.; Gasbarrini, A. The Human Gut Microbiota and Virome: Potential Therapeutic Implications. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2015, 47, 1007–1012. [Google Scholar] [CrossRef]
- Rinninella, E.; Raoul, P.; Cintoni, M.; Franceschi, F.; Miggiano, G.A.D.; Gasbarrini, A.; Mele, M.C. What Is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms 2019, 7, 14. [Google Scholar] [CrossRef]
- Ramirez, J.; Guarner, F.; Bustos Fernandez, L.; Maruy, A.; Sdepanian, V.L.; Cohen, H. Antibiotics as Major Disruptors of Gut Microbiota. Front. Cell. Infect. Microbiol. 2020, 10, 572912. [Google Scholar] [CrossRef]
- Milani, C.; Duranti, S.; Bottacini, F.; Casey, E.; Turroni, F.; Mahony, J.; Belzer, C.; Delgado Palacio, S.; Arboleya Montes, S.; Mancabelli, L.; et al. The First Microbial Colonizers of the Human Gut: Composition, Activities, and Health Implications of the Infant Gut Microbiota. Microbiol. Mol. Biol. Rev. MMBR 2017, 81, e00036-17. [Google Scholar] [CrossRef]
- Cavalcanti Neto, M.P.; Aquino, J.d.S.; Romão da Silva, L.d.F.; de Oliveira Silva, R.; Guimarães, K.S.d.L.; de Oliveira, Y.; de Souza, E.L.; Magnani, M.; Vidal, H.; de Brito Alves, J.L. Gut Microbiota and Probiotics Intervention: A Potential Therapeutic Target for Management of Cardiometabolic Disorders and Chronic Kidney Disease? Pharmacol. Res. 2018, 130, 152–163. [Google Scholar] [CrossRef]
- Lu, J.; Zhang, L.; Zhai, Q.; Zhao, J.; Zhang, H.; Lee, Y.-K.; Lu, W.; Li, M.; Chen, W. Chinese Gut Microbiota and Its Associations with Staple Food Type, Ethnicity, and Urbanization. NPJ Biofilms Microbiomes 2021, 7, 71. [Google Scholar] [CrossRef]
- Dehingia, M.; Adak, A.; Khan, M.R. Ethnicity-Influenced Microbiota: A Future Healthcare Perspective. Trends Microbiol. 2019, 27, 191–193. [Google Scholar] [CrossRef]
- Bibbò, S.; Ianiro, G.; Giorgio, V.; Scaldaferri, F.; Masucci, L.; Gasbarrini, A.; Cammarota, G. The Role of Diet on Gut Microbiota Composition. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 4742–4749. [Google Scholar]
- Malesza, I.J.; Malesza, M.; Walkowiak, J.; Mussin, N.; Walkowiak, D.; Aringazina, R.; Bartkowiak-Wieczorek, J.; Mądry, E. High-Fat, Western-Style Diet, Systemic Inflammation, and Gut Microbiota: A Narrative Review. Cells 2021, 10, 3164. [Google Scholar] [CrossRef]
- Weiss, G.A.; Hennet, T. Mechanisms and Consequences of Intestinal Dysbiosis. Cell. Mol. Life Sci. CMLS 2017, 74, 2959–2977. [Google Scholar] [CrossRef]
- Martinez, J.E.; Kahana, D.D.; Ghuman, S.; Wilson, H.P.; Wilson, J.; Kim, S.C.J.; Lagishetty, V.; Jacobs, J.P.; Sinha-Hikim, A.P.; Friedman, T.C. Unhealthy Lifestyle and Gut Dysbiosis: A Better Understanding of the Effects of Poor Diet and Nicotine on the Intestinal Microbiome. Front. Endocrinol. 2021, 12, 667066. [Google Scholar] [CrossRef]
- Wang, X.; Yang, S.; Li, S.; Zhao, L.; Hao, Y.; Qin, J.; Zhang, L.; Zhang, C.; Bian, W.; Zuo, L.; et al. Aberrant Gut Microbiota Alters Host Metabolome and Impacts Renal Failure in Humans and Rodents. Gut 2020, 69, 2131–2142. [Google Scholar] [CrossRef]
- Christian, V.J.; Miller, K.R.; Martindale, R.G. Food Insecurity, Malnutrition, and the Microbiome. Curr. Nutr. Rep. 2020, 9, 356–360. [Google Scholar] [CrossRef]
- Liu, B.-N.; Liu, X.-T.; Liang, Z.-H.; Wang, J.-H. Gut Microbiota in Obesity. World J. Gastroenterol. 2021, 27, 3837–3850. [Google Scholar] [CrossRef]
- Javdan, B.; Lopez, J.G.; Chankhamjon, P.; Lee, Y.-C.J.; Hull, R.; Wu, Q.; Wang, X.; Chatterjee, S.; Donia, M.S. Personalized Mapping of Drug Metabolism by the Human Gut Microbiome. Cell 2020, 181, 1661–1679.e22. [Google Scholar] [CrossRef]
- Weersma, R.K.; Zhernakova, A.; Fu, J. Interaction between Drugs and the Gut Microbiome. Gut 2020, 69, 1510–1519. [Google Scholar] [CrossRef]
- Routy, B.; Le Chatelier, E.; Derosa, L.; Duong, C.P.M.; Alou, M.T.; Daillère, R.; Fluckiger, A.; Messaoudene, M.; Rauber, C.; Roberti, M.P.; et al. Gut Microbiome Influences Efficacy of PD-1-Based Immunotherapy against Epithelial Tumors. Science 2018, 359, 91–97. [Google Scholar] [CrossRef]
- McGuckin, M.A.; Lindén, S.K.; Sutton, P.; Florin, T.H. Mucin Dynamics and Enteric Pathogens. Nat. Rev. Microbiol. 2011, 9, 265–278. [Google Scholar] [CrossRef]
- Candelli, M.; Franza, L.; Pignataro, G.; Ojetti, V.; Covino, M.; Piccioni, A.; Gasbarrini, A.; Franceschi, F. Interaction between Lipopolysaccharide and Gut Microbiota in Inflammatory Bowel Diseases. Int. J. Mol. Sci. 2021, 22, 6242. [Google Scholar] [CrossRef]
- Tan, J.K.; Macia, L.; Mackay, C.R. Dietary Fiber and SCFAs in the Regulation of Mucosal Immunity. J. Allergy Clin. Immunol. 2023, 151, 361–370. [Google Scholar] [CrossRef]
- Ratajczak, W.; Rył, A.; Mizerski, A.; Walczakiewicz, K.; Sipak, O.; Laszczyńska, M. Immunomodulatory Potential of Gut Microbiome-Derived Short-Chain Fatty Acids (SCFAs). Acta Biochim. Pol. 2019, 66. [Google Scholar] [CrossRef]
- Tan, J.; McKenzie, C.; Potamitis, M.; Thorburn, A.N.; Mackay, C.R.; Macia, L. The Role of Short-Chain Fatty Acids in Health and Disease. Adv. Immunol. 2014, 121, 91–119. [Google Scholar] [CrossRef]
- Jiang, C.; Li, G.; Huang, P.; Liu, Z.; Zhao, B. The Gut Microbiota and Alzheimer’s Disease. J. Alzheimers Dis. JAD 2017, 58, 1–15. [Google Scholar] [CrossRef]
- Zanza, C.; Romenskaya, T.; Thangathurai, D.; Ojetti, V.; Saviano, A.; Abenavoli, L.; Robba, C.; Cammarota, G.; Franceschi, F.; Piccioni, A.; et al. Microbiome in Critical Care: An Unconventional and Unknown Ally. Curr. Med. Chem. 2022, 29, 3179–3188. [Google Scholar] [CrossRef]
- Martel, J.; Chang, S.-H.; Ko, Y.-F.; Hwang, T.-L.; Young, J.D.; Ojcius, D.M. Gut Barrier Disruption and Chronic Disease. Trends Endocrinol. Metab. TEM 2022, 33, 247–265. [Google Scholar] [CrossRef]
- Mörbe, U.M.; Jørgensen, P.B.; Fenton, T.M.; von Burg, N.; Riis, L.B.; Spencer, J.; Agace, W.W. Human Gut-Associated Lymphoid Tissues (GALT); Diversity, Structure, and Function. Mucosal Immunol. 2021, 14, 793–802. [Google Scholar] [CrossRef]
- Chandran, P.; Satthaporn, S.; Robins, A.; Eremin, O. Inflammatory Bowel Disease: Dysfunction of GALT and Gut Bacterial Flora (II). Surg. J. R. Coll. Surg. Edinb. Irel. 2003, 1, 125–136. [Google Scholar] [CrossRef]
- Lyu, M.; Suzuki, H.; Kang, L.; Gaspal, F.; Zhou, W.; Goc, J.; Zhou, L.; Zhou, J.; Zhang, W.; JRI Live Cell Bank; et al. ILC3s Select Microbiota-Specific Regulatory T Cells to Establish Tolerance in the Gut. Nature 2022, 610, 744–751. [Google Scholar] [CrossRef]
- Tang, D.; Kang, R.; Coyne, C.B.; Zeh, H.J.; Lotze, M.T. PAMPs and DAMPs: Signal 0s That Spur Autophagy and Immunity. Immunol. Rev. 2012, 249, 158–175. [Google Scholar] [CrossRef]
- Cario, E. Barrier-Protective Function of Intestinal Epithelial Toll-like Receptor 2. Mucosal Immunol. 2008, 1 (Suppl. 1), S62–S66. [Google Scholar] [CrossRef]
- Farro, G.; Stakenborg, M.; Gomez-Pinilla, P.J.; Labeeuw, E.; Goverse, G.; Di Giovangiulio, M.; Stakenborg, N.; Meroni, E.; D’Errico, F.; Elkrim, Y.; et al. CCR2-Dependent Monocyte-Derived Macrophages Resolve Inflammation and Restore Gut Motility in Postoperative Ileus. Gut 2017, 66, 2098–2109. [Google Scholar] [CrossRef]
- Woo, V.; Alenghat, T. Epigenetic Regulation by Gut Microbiota. Gut Microbes 2022, 14, 2022407. [Google Scholar] [CrossRef]
- Jiao, Y.; Wu, L.; Huntington, N.D.; Zhang, X. Crosstalk Between Gut Microbiota and Innate Immunity and Its Implication in Autoimmune Diseases. Front. Immunol. 2020, 11, 282. [Google Scholar] [CrossRef]
- Panda, S.K.; Colonna, M. Innate Lymphoid Cells in Mucosal Immunity. Front. Immunol. 2019, 10, 861. [Google Scholar] [CrossRef]
- Wang, L.; Zhu, L.; Qin, S. Gut Microbiota Modulation on Intestinal Mucosal Adaptive Immunity. J. Immunol. Res. 2019, 2019, 4735040. [Google Scholar] [CrossRef]
- Fraser, J.D.; Proft, T. The Bacterial Superantigen and Superantigen-like Proteins. Immunol. Rev. 2008, 225, 226–243. [Google Scholar] [CrossRef]
- Saini, A.; Dalal, P.; Sharma, D. Deciphering the Interdependent Labyrinth between Gut Microbiota and the Immune System. Lett. Appl. Microbiol. 2022, 75, 1122–1135. [Google Scholar] [CrossRef]
- Takiishi, T.; Fenero, C.I.M.; Câmara, N.O.S. Intestinal Barrier and Gut Microbiota: Shaping Our Immune Responses throughout Life. Tissue Barriers 2017, 5, e1373208. [Google Scholar] [CrossRef]
- Luu, M.; Riester, Z.; Baldrich, A.; Reichardt, N.; Yuille, S.; Busetti, A.; Klein, M.; Wempe, A.; Leister, H.; Raifer, H.; et al. Microbial Short-Chain Fatty Acids Modulate CD8+ T Cell Responses and Improve Adoptive Immunotherapy for Cancer. Nat. Commun. 2021, 12, 4077. [Google Scholar] [CrossRef]
- Chen, P.; Tang, X. Gut Microbiota as Regulators of Th17/Treg Balance in Patients with Myasthenia Gravis. Front. Immunol. 2021, 12, 803101. [Google Scholar] [CrossRef]
- Manos, J. The Human Microbiome in Disease and Pathology. APMIS Acta Pathol. Microbiol. Immunol. Scand. 2022, 130, 690–705. [Google Scholar] [CrossRef]
- Jobin, C. Precision Medicine Using Microbiota. Science 2018, 359, 32–34. [Google Scholar] [CrossRef]
- Gilbert, J.A.; Lynch, S.V. Community Ecology as a Framework for Human Microbiome Research. Nat. Med. 2019, 25, 884–889. [Google Scholar] [CrossRef]
- Berg, G.; Rybakova, D.; Fischer, D.; Cernava, T.; Vergès, M.-C.C.; Charles, T.; Chen, X.; Cocolin, L.; Eversole, K.; Corral, G.H.; et al. Microbiome Definition Re-Visited: Old Concepts and New Challenges. Microbiome 2020, 8, 103. [Google Scholar] [CrossRef]
- Hou, K.; Wu, Z.-X.; Chen, X.-Y.; Wang, J.-Q.; Zhang, D.; Xiao, C.; Zhu, D.; Koya, J.B.; Wei, L.; Li, J.; et al. Microbiota in Health and Diseases. Signal Transduct. Target. Ther. 2022, 7, 135. [Google Scholar] [CrossRef]
- Sciarra, F.; Franceschini, E.; Campolo, F.; Venneri, M.A. The Diagnostic Potential of the Human Blood Microbiome: Are We Dreaming or Awake? Int. J. Mol. Sci. 2023, 24, 10422. [Google Scholar] [CrossRef]
- Bozkurt, B.; Coats, A.J.; Tsutsui, H.; Abdelhamid, M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Böhm, M.; Butler, J.; et al. Universal Definition and Classification of Heart Failure. J. Card. Fail. 2021, 27, 387–413. [Google Scholar] [CrossRef]
- Al-Ayadhi, L.; Zayed, N.; Bhat, R.S.; Moubayed, N.M.S.; Al-Muammar, M.N.; El-Ansary, A. The Use of Biomarkers Associated with Leaky Gut as a Diagnostic Tool for Early Intervention in Autism Spectrum Disorder: A Systematic Review. Gut Pathog. 2021, 13, 54. [Google Scholar] [CrossRef]
- Tang, W.H.W.; Li, D.Y.; Hazen, S.L. Dietary Metabolism, the Gut Microbiome, and Heart Failure. Nat. Rev. Cardiol. 2019, 16, 137–154. [Google Scholar] [CrossRef]
- Barbaresko, J.; Koch, M.; Schulze, M.B.; Nöthlings, U. Dietary Pattern Analysis and Biomarkers of Low-Grade Inflammation: A Systematic Literature Review. Nutr. Rev. 2013, 71, 511–527. [Google Scholar] [CrossRef]
- Kawano, Y.; Edwards, M.; Huang, Y.; Bilate, A.M.; Araujo, L.P.; Tanoue, T.; Atarashi, K.; Ladinsky, M.S.; Reiner, S.L.; Wang, H.H.; et al. Microbiota Imbalance Induced by Dietary Sugar Disrupts Immune-Mediated Protection from Metabolic Syndrome. Cell 2022, 185, 3501–3519.e20. [Google Scholar] [CrossRef]
- Wang, P.-X.; Deng, X.-R.; Zhang, C.-H.; Yuan, H.-J. Gut Microbiota and Metabolic Syndrome. Chin. Med. J. 2020, 133, 808–816. [Google Scholar] [CrossRef]
- Lupu, V.V.; Adam Raileanu, A.; Mihai, C.M.; Morariu, I.D.; Lupu, A.; Starcea, I.M.; Frasinariu, O.E.; Mocanu, A.; Dragan, F.; Fotea, S. The Implication of the Gut Microbiome in Heart Failure. Cells 2023, 12, 1158. [Google Scholar] [CrossRef]
- Riehle, C.; Bauersachs, J. Key Inflammatory Mechanisms Underlying Heart Failure. Herz 2019, 44, 96–106. [Google Scholar] [CrossRef]
- Harrison, C.A.; Laubitz, D.; Ohland, C.L.; Midura-Kiela, M.T.; Patil, K.; Besselsen, D.G.; Jamwal, D.R.; Jobin, C.; Ghishan, F.K.; Kiela, P.R. Microbial Dysbiosis Associated with Impaired Intestinal Na+/H+ Exchange Accelerates and Exacerbates Colitis in Ex-Germ Free Mice. Mucosal Immunol. 2018, 11, 1329–1341. [Google Scholar] [CrossRef]
- Hayashi, T.; Yamashita, T.; Takahashi, T.; Tabata, T.; Watanabe, H.; Gotoh, Y.; Shinohara, M.; Kami, K.; Tanaka, H.; Matsumoto, K.; et al. Uncovering the Role of Gut Microbiota in Amino Acid Metabolic Disturbances in Heart Failure Through Metagenomic Analysis. Front. Cardiovasc. Med. 2021, 8, 789325. [Google Scholar] [CrossRef]
- Pasini, E.; Aquilani, R.; Testa, C.; Baiardi, P.; Angioletti, S.; Boschi, F.; Verri, M.; Dioguardi, F. Pathogenic Gut Flora in Patients with Chronic Heart Failure. JACC Heart Fail. 2016, 4, 220–227. [Google Scholar] [CrossRef]
- Kim, M.; Huda, M.N.; Bennett, B.J. Sequence Meets Function-Microbiota and Cardiovascular Disease. Cardiovasc. Res. 2022, 118, 399–412. [Google Scholar] [CrossRef]
- Cianci, R.; Franza, L.; Borriello, R.; Pagliari, D.; Gasbarrini, A.; Gambassi, G. The Role of Gut Microbiota in Heart Failure: When Friends Become Enemies. Biomedicines 2022, 10, 2712. [Google Scholar] [CrossRef]
- Romano, K.A.; Nemet, I.; Prasad Saha, P.; Haghikia, A.; Li, X.S.; Mohan, M.L.; Lovano, B.; Castel, L.; Witkowski, M.; Buffa, J.A.; et al. Gut Microbiota-Generated Phenylacetylglutamine and Heart Failure. Circ. Heart Fail. 2023, 16, e009972. [Google Scholar] [CrossRef]
- Wei, H.; Wu, J.; Wang, H.; Huang, J.; Li, C.; Zhang, Y.; Song, Y.; Zhou, Z.; Sun, Y.; Xiao, L.; et al. Increased Circulating Phenylacetylglutamine Concentration Elevates the Predictive Value of Cardiovascular Event Risk in Heart Failure Patients. J. Intern. Med. 2023, 294, 515–530. [Google Scholar] [CrossRef]
- Kurmani, S.; Squire, I. Acute Heart Failure: Definition, Classification and Epidemiology. Curr. Heart Fail. Rep. 2017, 14, 385–392. [Google Scholar] [CrossRef]
- Sethwala, A.M.; Goh, I.; Amerena, J.V. Combating Inflammation in Cardiovascular Disease. Heart Lung Circ. 2021, 30, 197–206. [Google Scholar] [CrossRef]
- Rahman, M.M.; Islam, F.; Or-Rashid, M.H.; Mamun, A.A.; Rahaman, M.S.; Islam, M.M.; Meem, A.F.K.; Sutradhar, P.R.; Mitra, S.; Mimi, A.A.; et al. The Gut Microbiota (Microbiome) in Cardiovascular Disease and Its Therapeutic Regulation. Front. Cell. Infect. Microbiol. 2022, 12, 903570. [Google Scholar] [CrossRef]
- Wang, Z.; Klipfell, E.; Bennett, B.J.; Koeth, R.; Levison, B.S.; DuGar, B.; Feldstein, A.E.; Britt, E.B.; Fu, X.; Chung, Y.-M.; et al. Gut Flora Metabolism of Phosphatidylcholine Promotes Cardiovascular Disease. Nature 2011, 472, 57–63. [Google Scholar] [CrossRef]
- Tang, W.H.W.; Wang, Z.; Levison, B.S.; Koeth, R.A.; Britt, E.B.; Fu, X.; Wu, Y.; Hazen, S.L. Intestinal Microbial Metabolism of Phosphatidylcholine and Cardiovascular Risk. N. Engl. J. Med. 2013, 368, 1575–1584. [Google Scholar] [CrossRef]
- Koeth, R.A.; Wang, Z.; Levison, B.S.; Buffa, J.A.; Org, E.; Sheehy, B.T.; Britt, E.B.; Fu, X.; Wu, Y.; Li, L.; et al. Intestinal Microbiota Metabolism of L-Carnitine, a Nutrient in Red Meat, Promotes Atherosclerosis. Nat. Med. 2013, 19, 576–585. [Google Scholar] [CrossRef]
- Marques, F.Z.; Nelson, E.; Chu, P.Y.; Horlock, D.; Fiedler, A.; Ziemann, M.; Tan, J.K.; Kuruppu, S.; Rajapakse, N.W.; El-Osta, A.; et al. High-Fiber Diet and Acetate Supplementation Change the Gut Microbiota and Prevent the Development of Hypertension and Heart Failure in Hypertensive Mice. Circulation 2017, 135, 964–977. [Google Scholar] [CrossRef]
- Liu, H.; Zhuang, J.; Tang, P.; Li, J.; Xiong, X.; Deng, H. The Role of the Gut Microbiota in Coronary Heart Disease. Curr. Atheroscler. Rep. 2020, 22, 77. [Google Scholar] [CrossRef]
- Gawałko, M.; Agbaedeng, T.A.; Saljic, A.; Müller, D.N.; Wilck, N.; Schnabel, R.; Penders, J.; Rienstra, M.; van Gelder, I.; Jespersen, T.; et al. Gut Microbiota, Dysbiosis and Atrial Fibrillation. Arrhythmogenic Mechanisms and Potential Clinical Implications. Cardiovasc. Res. 2021, 118, 2415–2427. [Google Scholar] [CrossRef]
- Evenepoel, P.; Poesen, R.; Meijers, B. The Gut-Kidney Axis. Pediatr. Nephrol. Berl. Ger. 2017, 32, 2005–2014. [Google Scholar] [CrossRef]
- Mafra, D.; Borges, N.; Alvarenga, L.; Esgalhado, M.; Cardozo, L.; Lindholm, B.; Stenvinkel, P. Dietary Components That May Influence the Disturbed Gut Microbiota in Chronic Kidney Disease. Nutrients 2019, 11, 496. [Google Scholar] [CrossRef]
- Cianci, R.; Franza, L.; Massaro, M.G.; Borriello, R.; Tota, A.; Pallozzi, M.; De Vito, F.; Gambassi, G. The Crosstalk between Gut Microbiota, Intestinal Immunological Niche and Visceral Adipose Tissue as a New Model for the Pathogenesis of Metabolic and Inflammatory Diseases: The Paradigm of Type 2 Diabetes Mellitus. Curr. Med. Chem. 2022, 29, 3189–3201. [Google Scholar] [CrossRef]
- Wang, J.; Chen, Y.; Zhong, H.; Chen, F.; Regenstein, J.; Hu, X.; Cai, L.; Feng, F. The Gut Microbiota as a Target to Control Hyperuricemia Pathogenesis: Potential Mechanisms and Therapeutic Strategies. Crit. Rev. Food Sci. Nutr. 2022, 62, 3979–3989. [Google Scholar] [CrossRef]
- Halimulati, M.; Wang, R.; Aihemaitijiang, S.; Huang, X.; Ye, C.; Zhang, Z.; Li, L.; Zhu, W.; Zhang, Z.; He, L. Anti-Hyperuricemic Effect of Anserine Based on the Gut-Kidney Axis: Integrated Analysis of Metagenomics and Metabolomics. Nutrients 2023, 15, 969. [Google Scholar] [CrossRef]
- Castillo-Rodriguez, E.; Fernandez-Prado, R.; Esteras, R.; Perez-Gomez, M.V.; Gracia-Iguacel, C.; Fernandez-Fernandez, B.; Kanbay, M.; Tejedor, A.; Lazaro, A.; Ruiz-Ortega, M.; et al. Impact of Altered Intestinal Microbiota on Chronic Kidney Disease Progression. Toxins 2018, 10, 300. [Google Scholar] [CrossRef]
- Vaziri, N.D.; Wong, J.; Pahl, M.; Piceno, Y.M.; Yuan, J.; DeSantis, T.Z.; Ni, Z.; Nguyen, T.-H.; Andersen, G.L. Chronic Kidney Disease Alters Intestinal Microbial Flora. Kidney Int. 2013, 83, 308–315. [Google Scholar] [CrossRef]
- Huang, W.; Zhou, L.; Guo, H.; Xu, Y.; Xu, Y. The Role of Short-Chain Fatty Acids in Kidney Injury Induced by Gut-Derived Inflammatory Response. Metabolism. 2017, 68, 20–30. [Google Scholar] [CrossRef]
- Watanabe, I.K.M.; Andrade-Silva, M.; Foresto-Neto, O.; Felizardo, R.J.F.; Matheus, M.A.C.; Silva, R.C.; Cenedeze, M.A.; Honda, T.S.B.; Perandini, L.A.B.; Volpini, R.A.; et al. Gut Microbiota and Intestinal Epithelial Myd88 Signaling Are Crucial for Renal Injury in UUO Mice. Front. Immunol. 2020, 11, 578623. [Google Scholar] [CrossRef]
- Stavropoulou, E.; Kantartzi, K.; Tsigalou, C.; Konstantinidis, T.; Romanidou, G.; Voidarou, C.; Bezirtzoglou, E. Focus on the Gut-Kidney Axis in Health and Disease. Front. Med. 2020, 7, 620102. [Google Scholar] [CrossRef]
- Ramos, C.I.; Armani, R.G.; Canziani, M.E.F.; Dalboni, M.A.; Dolenga, C.J.R.; Nakao, L.S.; Campbell, K.L.; Cuppari, L. Effect of Prebiotic (Fructooligosaccharide) on Uremic Toxins of Chronic Kidney Disease Patients: A Randomized Controlled Trial. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc.-Eur. Ren. Assoc. 2019, 34, 1876–1884. [Google Scholar] [CrossRef]
- Rukavina Mikusic, N.L.; Kouyoumdzian, N.M.; Choi, M.R. Gut Microbiota and Chronic Kidney Disease: Evidences and Mechanisms That Mediate a New Communication in the Gastrointestinal-Renal Axis. Pflugers Arch. 2020, 472, 303–320. [Google Scholar] [CrossRef]
- Xi, Y.; Yan, J.; Li, M.; Ying, S.; Shi, Z. Gut Microbiota Dysbiosis Increases the Risk of Visceral Gout in Goslings through Translocation of Gut-Derived Lipopolysaccharide. Poult. Sci. 2019, 98, 5361–5373. [Google Scholar] [CrossRef]
- Hartwich, K.; Poehlein, A.; Daniel, R. The Purine-Utilizing Bacterium Clostridium Acidurici 9a: A Genome-Guided Metabolic Reconsideration. PLoS ONE 2012, 7, e51662. [Google Scholar] [CrossRef]
- Pan, L.; Han, P.; Ma, S.; Peng, R.; Wang, C.; Kong, W.; Cong, L.; Fu, J.; Zhang, Z.; Yu, H.; et al. Abnormal Metabolism of Gut Microbiota Reveals the Possible Molecular Mechanism of Nephropathy Induced by Hyperuricemia. Acta Pharm. Sin. B 2020, 10, 249–261. [Google Scholar] [CrossRef]
- Ni, J.; Shen, T.-C.D.; Chen, E.Z.; Bittinger, K.; Bailey, A.; Roggiani, M.; Sirota-Madi, A.; Friedman, E.S.; Chau, L.; Lin, A.; et al. A Role for Bacterial Urease in Gut Dysbiosis and Crohn’s Disease. Sci. Transl. Med. 2017, 9, eaah6888. [Google Scholar] [CrossRef]
- Chen, H.; Wang, J.; Ouyang, Q.; Peng, X.; Yu, Z.; Wang, J.; Huang, J. Alterations of Gut Microbes and Their Correlation with Clinical Features in Middle and End-Stages Chronic Kidney Disease. Front. Cell. Infect. Microbiol. 2023, 13, 1105366. [Google Scholar] [CrossRef]
- Voroneanu, L.; Burlacu, A.; Brinza, C.; Covic, A.; Balan, G.G.; Nistor, I.; Popa, C.; Hogas, S.; Covic, A. Gut Microbiota in Chronic Kidney Disease: From Composition to Modulation towards Better Outcomes-A Systematic Review. J. Clin. Med. 2023, 12, 1948. [Google Scholar] [CrossRef]
- Yang, J.; Kim, C.J.; Go, Y.S.; Lee, H.Y.; Kim, M.-G.; Oh, S.W.; Cho, W.Y.; Im, S.-H.; Jo, S.K. Intestinal Microbiota Control Acute Kidney Injury Severity by Immune Modulation. Kidney Int. 2020, 98, 932–946. [Google Scholar] [CrossRef]
- Hu, Q.; Wu, K.; Pan, W.; Zeng, Y.; Hu, K.; Chen, D.; Huang, X.; Zhang, Q. Intestinal Flora Alterations in Patients with Early Chronic Kidney Disease: A Case-Control Study among the Han Population in Southwestern China. J. Int. Med. Res. 2020, 48, 300060520926033. [Google Scholar] [CrossRef]
- Gao, B.; Jose, A.; Alonzo-Palma, N.; Malik, T.; Shankaranarayanan, D.; Regunathan-Shenk, R.; Raj, D.S. Butyrate Producing Microbiota Are Reduced in Chronic Kidney Diseases. Sci. Rep. 2021, 11, 23530. [Google Scholar] [CrossRef]
- Wang, H.; Ainiwaer, A.; Song, Y.; Qin, L.; Peng, A.; Bao, H.; Qin, H. Perturbed Gut Microbiome and Fecal and Serum Metabolomes Are Associated with Chronic Kidney Disease Severity. Microbiome 2023, 11, 3. [Google Scholar] [CrossRef]
- Raj, D.; Tomar, B.; Lahiri, A.; Mulay, S.R. The Gut-Liver-Kidney Axis: Novel Regulator of Fatty Liver Associated Chronic Kidney Disease. Pharmacol. Res. 2020, 152, 104617. [Google Scholar] [CrossRef]
- Padda, J.; Khalid, K.; Khedr, A.; Tasnim, F.; Al-Ewaidat, O.A.; Cooper, A.C.; Jean-Charles, G. Non-Alcoholic Fatty Liver Disease and Its Association With Diabetes Mellitus. Cureus 2021, 13, e17321. [Google Scholar] [CrossRef]
- Sharma, N.; Sircar, A.; Anders, H.-J.; Gaikwad, A.B. Crosstalk between Kidney and Liver in Non-Alcoholic Fatty Liver Disease: Mechanisms and Therapeutic Approaches. Arch. Physiol. Biochem. 2022, 128, 1024–1038. [Google Scholar] [CrossRef]
- Golab, F.; Kadkhodaee, M.; Zahmatkesh, M.; Hedayati, M.; Arab, H.; Schuster, R.; Zahedi, K.; Lentsch, A.B.; Soleimani, M. Ischemic and Non-Ischemic Acute Kidney Injury Cause Hepatic Damage. Kidney Int. 2009, 75, 783–792. [Google Scholar] [CrossRef]
- Feltenberger, J.D.; Andrade, J.M.O.; Paraíso, A.; Barros, L.O.; Filho, A.B.M.; Sinisterra, R.D.M.; Sousa, F.B.; Guimarães, A.L.S.; de Paula, A.M.B.; Campagnole-Santos, M.J.; et al. Oral Formulation of Angiotensin-(1-7) Improves Lipid Metabolism and Prevents High-Fat Diet-Induced Hepatic Steatosis and Inflammation in Mice. Hypertens. Dallas Tex 1979 2013, 62, 324–330. [Google Scholar] [CrossRef]
- Gryp, T.; Vanholder, R.; Vaneechoutte, M.; Glorieux, G. P-Cresyl Sulfate. Toxins 2017, 9, 52. [Google Scholar] [CrossRef]
- Pletinck, A.; Glorieux, G.; Schepers, E.; Cohen, G.; Gondouin, B.; Van Landschoot, M.; Eloot, S.; Rops, A.; Van de Voorde, J.; De Vriese, A.; et al. Protein-Bound Uremic Toxins Stimulate Crosstalk between Leukocytes and Vessel Wall. J. Am. Soc. Nephrol. JASN 2013, 24, 1981–1994. [Google Scholar] [CrossRef]
- Han, H.; Zhu, J.; Zhu, Z.; Ni, J.; Du, R.; Dai, Y.; Chen, Y.; Wu, Z.; Lu, L.; Zhang, R. P-Cresyl Sulfate Aggravates Cardiac Dysfunction Associated with Chronic Kidney Disease by Enhancing Apoptosis of Cardiomyocytes. J. Am. Heart Assoc. 2015, 4, e001852. [Google Scholar] [CrossRef]
- Liu, J.-R.; Miao, H.; Deng, D.-Q.; Vaziri, N.D.; Li, P.; Zhao, Y.-Y. Gut Microbiota-Derived Tryptophan Metabolism Mediates Renal Fibrosis by Aryl Hydrocarbon Receptor Signaling Activation. Cell. Mol. Life Sci. CMLS 2021, 78, 909–922. [Google Scholar] [CrossRef]
- Gatarek, P.; Kaluzna-Czaplinska, J. Trimethylamine N-Oxide (TMAO) in Human Health. EXCLI J. 2021, 20, 301–319. [Google Scholar] [CrossRef]
- Chen, K.; Zheng, X.; Feng, M.; Li, D.; Zhang, H. Gut Microbiota-Dependent Metabolite Trimethylamine N-Oxide Contributes to Cardiac Dysfunction in Western Diet-Induced Obese Mice. Front. Physiol. 2017, 8, 139. [Google Scholar] [CrossRef]
- Ma, G.; Pan, B.; Chen, Y.; Guo, C.; Zhao, M.; Zheng, L.; Chen, B. Trimethylamine N-Oxide in Atherogenesis: Impairing Endothelial Self-Repair Capacity and Enhancing Monocyte Adhesion. Biosci. Rep. 2017, 37, BSR20160244. [Google Scholar] [CrossRef]
- Masenga, S.K.; Povia, J.P.; Lwiindi, P.C.; Kirabo, A. Recent Advances in Microbiota-Associated Metabolites in Heart Failure. Biomedicines 2023, 11, 2313. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, H.; Ren, S.; Ding, Y.; Remex, N.S.; Bhuiyan, M.S.; Qu, J.; Tang, X. Gut Microbiota and Microbiota-Derived Metabolites in Cardiovascular Diseases. Chin. Med. J. 2023, 136, 2269–2284. [Google Scholar] [CrossRef]
- Kamo, T.; Akazawa, H.; Suda, W.; Saga-Kamo, A.; Shimizu, Y.; Yagi, H.; Liu, Q.; Nomura, S.; Naito, A.T.; Takeda, N.; et al. Dysbiosis and Compositional Alterations with Aging in the Gut Microbiota of Patients with Heart Failure. PLoS ONE 2017, 12, e0174099. [Google Scholar] [CrossRef]
- Kummen, M.; Mayerhofer, C.C.K.; Vestad, B.; Broch, K.; Awoyemi, A.; Storm-Larsen, C.; Ueland, T.; Yndestad, A.; Hov, J.R.; Trøseid, M. Gut Microbiota Signature in Heart Failure Defined from Profiling of 2 Independent Cohorts. J. Am. Coll. Cardiol. 2018, 71, 1184–1186. [Google Scholar] [CrossRef]
- Suzuki, T.; Yazaki, Y.; Voors, A.A.; Jones, D.J.L.; Chan, D.C.S.; Anker, S.D.; Cleland, J.G.; Dickstein, K.; Filippatos, G.; Hillege, H.L.; et al. Association with Outcomes and Response to Treatment of Trimethylamine N-Oxide in Heart Failure: Results from BIOSTAT-CHF. Eur. J. Heart Fail. 2019, 21, 877–886. [Google Scholar] [CrossRef]
- Paraskevaidis, I.; Xanthopoulos, A.; Tsougos, E.; Triposkiadis, F. Human Gut Microbiota in Heart Failure: Trying to Unmask an Emerging Organ. Biomedicines 2023, 11, 2574. [Google Scholar] [CrossRef]
- Zong, X.; Fan, Q.; Yang, Q.; Pan, R.; Zhuang, L.; Tao, R. Phenylacetylglutamine as a Risk Factor and Prognostic Indicator of Heart Failure. ESC Heart Fail. 2022, 9, 2645–2653. [Google Scholar] [CrossRef]
- Li, Y.; Lu, H.; Guo, J.; Zhang, M.; Zheng, H.; Liu, Y.; Liu, W. Gut Microbiota-Derived Trimethylamine N-Oxide Is Associated with the Risk of All-Cause and Cardiovascular Mortality in Patients with Chronic Kidney Disease: A Systematic Review and Dose-Response Meta-Analysis. Ann. Med. 2023, 55, 2215542. [Google Scholar] [CrossRef]
- Noce, A.; Tranchita, E.; Marrone, G.; Grazioli, E.; Lauro, M.D.; Murri, A.; Vanni, G.; Parisi, A.; Tesauro, M.; Cerulli, C. The Possible Role of Physical Activity in the Modulation of Gut Microbiota in Chronic Kidney Disease and Its Impact on Cardiovascular Risk: A Narrative Review. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 3733–3746. [Google Scholar] [PubMed]
- Pelletier, C.C.; Croyal, M.; Ene, L.; Aguesse, A.; Billon-Crossouard, S.; Krempf, M.; Lemoine, S.; Guebre-Egziabher, F.; Juillard, L.; Soulage, C.O. Elevation of Trimethylamine-N-Oxide in Chronic Kidney Disease: Contribution of Decreased Glomerular Filtration Rate. Toxins 2019, 11, 635. [Google Scholar] [CrossRef]
- Gryp, T.; De Paepe, K.; Vanholder, R.; Kerckhof, F.-M.; Van Biesen, W.; Van de Wiele, T.; Verbeke, F.; Speeckaert, M.; Joossens, M.; Couttenye, M.M.; et al. Gut Microbiota Generation of Protein-Bound Uremic Toxins and Related Metabolites Is Not Altered at Different Stages of Chronic Kidney Disease. Kidney Int. 2020, 97, 1230–1242. [Google Scholar] [CrossRef]
- Noce, A.; Marchetti, M.; Marrone, G.; Di Renzo, L.; Di Lauro, M.; Di Daniele, F.; Albanese, M.; Di Daniele, N.; Di Lorenzo, A. Link between Gut Microbiota Dysbiosis and Chronic Kidney Disease. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 2057–2074. [Google Scholar] [PubMed]
- Saranya, G.; Viswanathan, P. Gut Microbiota Dysbiosis in AKI to CKD Transition. Biomed. Pharmacother. 2023, 161, 114447. [Google Scholar] [CrossRef]
- Glassock, R.J.; Massry, S.G. Chapter 6-Uremic Toxins: An Integrated Overview of Classification and Pathobiology. In Nutritional Management of Renal Disease, 4th ed; Kopple, J.D., Massry, S.G., Kalantar-Zadeh, K., Fouque, D., Eds.; Academic Press: Cambridge, MA, USA, 2022; pp. 77–89. ISBN 978-0-12-818540-7. [Google Scholar]
- Falconi, C.A.; Junho, C.V.d.C.; Fogaça-Ruiz, F.; Vernier, I.C.S.; da Cunha, R.S.; Stinghen, A.E.M.; Carneiro-Ramos, M.S. Uremic Toxins: An Alarming Danger Concerning the Cardiovascular System. Front. Physiol. 2021, 12, 686249. [Google Scholar] [CrossRef]
- Rosner, M.H.; Reis, T.; Husain-Syed, F.; Vanholder, R.; Hutchison, C.; Stenvinkel, P.; Blankestijn, P.J.; Cozzolino, M.; Juillard, L.; Kashani, K.; et al. Classification of Uremic Toxins and Their Role in Kidney Failure. Clin. J. Am. Soc. Nephrol. CJASN 2021, 16, 1918–1928. [Google Scholar] [CrossRef]
- Xu, Y.; Bi, W.-D.; Shi, Y.-X.; Liang, X.-R.; Wang, H.-Y.; Lai, X.-L.; Bian, X.-L.; Guo, Z.-Y. Derivation and Elimination of Uremic Toxins from Kidney-Gut Axis. Front. Physiol. 2023, 14, 1123182. [Google Scholar] [CrossRef]
- Koshida, T.; Gohda, T.; Sugimoto, T.; Asahara, T.; Asao, R.; Ohsawa, I.; Gotoh, H.; Murakoshi, M.; Suzuki, Y.; Yamashiro, Y. Gut Microbiome and Microbiome-Derived Metabolites in Patients with End-Stage Kidney Disease. Int. J. Mol. Sci. 2023, 24, 11456. [Google Scholar] [CrossRef]
- Evenepoel, P.; Meijers, B.K.I.; Bammens, B.R.M.; Verbeke, K. Uremic Toxins Originating from Colonic Microbial Metabolism. Kidney Int. Suppl. 2009, 76, S12–S19. [Google Scholar] [CrossRef]
- Arcidiacono, T.; Macrina, L.; Premaschi, S.; Bologna, A.; Magni, G.; Foligno, N.; Avino, M.; Belloni, C.; Palmieri, N.; Conte, F.; et al. Serum Concentrations of Free Indoxyl and P-Cresyl Sulfate Are Associated with Mineral Metabolism Variables and Cardiovascular Risk in Hemodialysis Patients. J. Nephrol. 2022, 35, 1457–1465. [Google Scholar] [CrossRef]
- Kar, E.; Kar, F.; Can, B.; Çakır Gündoğdu, A.; Özbayer, C.; Koçak, F.E.; Şentürk, H. Prophylactic and Therapeutic Efficacy of Boric Acid on Lipopolysaccharide-Induced Liver and Kidney Inflammation in Rats. Biol. Trace Elem. Res. 2023. [Google Scholar] [CrossRef]
- Jiao, Y.; Li, W.; Zhang, Q.; Jiang, Q. Gut Microbiota and Hypertension: A Bibliometric Analysis of Recent Research (2014–2023). Front. Nutr. 2023, 10, 1253803. [Google Scholar] [CrossRef]
- Shi, L.; Li, C.; Wang, J.; Zhong, H.; Wei, T.; Fan, W.; Li, Z. The Intellectual Base and Global Trends in Inflammation of Diabetic Kidney Disease: A Bibliometric Analysis. Ren. Fail. 2023, 45, 2270061. [Google Scholar] [CrossRef]
- Tang, Z.; Yu, S.; Pan, Y. The Gut Microbiome Tango in the Progression of Chronic Kidney Disease and Potential Therapeutic Strategies. J. Transl. Med. 2023, 21, 689. [Google Scholar] [CrossRef]
- Janeiro, M.H.; Ramírez, M.J.; Milagro, F.I.; Martínez, J.A.; Solas, M. Implication of Trimethylamine N-Oxide (TMAO) in Disease: Potential Biomarker or New Therapeutic Target. Nutrients 2018, 10, 1398. [Google Scholar] [CrossRef]
- Mafra, D.; Borges, N.A.; Cardozo, L.F.M.d.F.; Anjos, J.S.; Black, A.P.; Moraes, C.; Bergman, P.; Lindholm, B.; Stenvinkel, P. Red Meat Intake in Chronic Kidney Disease Patients: Two Sides of the Coin. Nutr. Burbank Los Angel. Cty. Calif 2018, 46, 26–32. [Google Scholar] [CrossRef]
- Zeisel, S.H.; Warrier, M. Trimethylamine N-Oxide, the Microbiome, and Heart and Kidney Disease. Annu. Rev. Nutr. 2017, 37, 157–181. [Google Scholar] [CrossRef]
- Thomas, M.S.; Fernandez, M.L. Trimethylamine N-Oxide (TMAO), Diet and Cardiovascular Disease. Curr. Atheroscler. Rep. 2021, 23, 12. [Google Scholar] [CrossRef]
- Schuett, K.; Kleber, M.E.; Scharnagl, H.; Lorkowski, S.; März, W.; Niessner, A.; Marx, N.; Meinitzer, A. Trimethylamine-N-Oxide and Heart Failure with Reduced Versus Preserved Ejection Fraction. J. Am. Coll. Cardiol. 2017, 70, 3202–3204. [Google Scholar] [CrossRef]
- Chen, M.-L.; Zhu, X.-H.; Ran, L.; Lang, H.-D.; Yi, L.; Mi, M.-T. Trimethylamine-N-Oxide Induces Vascular Inflammation by Activating the NLRP3 Inflammasome Through the SIRT3-SOD2-mtROS Signaling Pathway. J. Am. Heart Assoc. 2017, 6, e006347. [Google Scholar] [CrossRef]
- Randrianarisoa, E.; Lehn-Stefan, A.; Wang, X.; Hoene, M.; Peter, A.; Heinzmann, S.S.; Zhao, X.; Königsrainer, I.; Königsrainer, A.; Balletshofer, B.; et al. Relationship of Serum Trimethylamine N-Oxide (TMAO) Levels with Early Atherosclerosis in Humans. Sci. Rep. 2016, 6, 26745. [Google Scholar] [CrossRef]
- Wu, C.; Li, C.; Zhao, W.; Xie, N.; Yan, F.; Lian, Y.; Zhou, L.; Xu, X.; Liang, Y.; Wang, L.; et al. Elevated Trimethylamine N-Oxide Related to Ischemic Brain Lesions after Carotid Artery Stenting. Neurology 2018, 90, e1283–e1290. [Google Scholar] [CrossRef]
- Senthong, V.; Wang, Z.; Fan, Y.; Wu, Y.; Hazen, S.L.; Tang, W.H.W. Trimethylamine N-Oxide and Mortality Risk in Patients with Peripheral Artery Disease. J. Am. Heart Assoc. 2016, 5, e004237. [Google Scholar] [CrossRef]
- Roncal, C.; Martínez-Aguilar, E.; Orbe, J.; Ravassa, S.; Fernandez-Montero, A.; Saenz-Pipaon, G.; Ugarte, A.; Estella-Hermoso de Mendoza, A.; Rodriguez, J.A.; Fernández-Alonso, S.; et al. Trimethylamine-N-Oxide (TMAO) Predicts Cardiovascular Mortality in Peripheral Artery Disease. Sci. Rep. 2019, 9, 15580. [Google Scholar] [CrossRef]
- Sheng, Z.; Tan, Y.; Liu, C.; Zhou, P.; Li, J.; Zhou, J.; Chen, R.; Chen, Y.; Song, L.; Zhao, H.; et al. Relation of Circulating Trimethylamine N-Oxide with Coronary Atherosclerotic Burden in Patients With ST-Segment Elevation Myocardial Infarction. Am. J. Cardiol. 2019, 123, 894–898. [Google Scholar] [CrossRef]
- Cañadas-Garre, M.; Anderson, K.; McGoldrick, J.; Maxwell, A.P.; McKnight, A.J. Proteomic and Metabolomic Approaches in the Search for Biomarkers in Chronic Kidney Disease. J. Proteomics 2019, 193, 93–122. [Google Scholar] [CrossRef]
- Zhang, W.; Miikeda, A.; Zuckerman, J.; Jia, X.; Charugundla, S.; Zhou, Z.; Kaczor-Urbanowicz, K.E.; Magyar, C.; Guo, F.; Wang, Z.; et al. Inhibition of Microbiota-Dependent TMAO Production Attenuates Chronic Kidney Disease in Mice. Sci. Rep. 2021, 11, 518. [Google Scholar] [CrossRef]
- Tang, W.H.W.; Wang, Z.; Kennedy, D.J.; Wu, Y.; Buffa, J.A.; Agatisa-Boyle, B.; Li, X.S.; Levison, B.S.; Hazen, S.L. Gut Microbiota-Dependent Trimethylamine N-Oxide (TMAO) Pathway Contributes to Both Development of Renal Insufficiency and Mortality Risk in Chronic Kidney Disease. Circ. Res. 2015, 116, 448–455. [Google Scholar] [CrossRef]
- Schluter, J.; Peled, J.U.; Taylor, B.P.; Markey, K.A.; Smith, M.; Taur, Y.; Niehus, R.; Staffas, A.; Dai, A.; Fontana, E.; et al. The Gut Microbiota Is Associated with Immune Cell Dynamics in Humans. Nature 2020, 588, 303–307. [Google Scholar] [CrossRef]
- Zmora, N.; Suez, J.; Elinav, E. You Are What You Eat: Diet, Health and the Gut Microbiota. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 35–56. [Google Scholar] [CrossRef]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean Diet; a Literature Review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Rio, P.; Massaro, M.G.; Caldarelli, M.; Frank, G.; Della-Morte, D.; Gasbarrini, A.; Gambassi, G.; De Lorenzo, A.; et al. Role of Nutrients in Modulating Microbiota and Immunity in COVID-19 Disease. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 5927–5945. [Google Scholar] [CrossRef]
- De Filippis, F.; Pellegrini, N.; Vannini, L.; Jeffery, I.B.; La Storia, A.; Laghi, L.; Serrazanetti, D.I.; Di Cagno, R.; Ferrocino, I.; Lazzi, C.; et al. High-Level Adherence to a Mediterranean Diet Beneficially Impacts the Gut Microbiota and Associated Metabolome. Gut 2016, 65, 1812–1821. [Google Scholar] [CrossRef]
- Sumida, K.; Lau, W.L.; Kovesdy, C.P.; Kalantar-Zadeh, K.; Kalantar-Zadeh, K. Microbiome Modulation as a Novel Therapeutic Approach in Chronic Kidney Disease. Curr. Opin. Nephrol. Hypertens. 2021, 30, 75–84. [Google Scholar] [CrossRef]
- Kasubuchi, M.; Hasegawa, S.; Hiramatsu, T.; Ichimura, A.; Kimura, I. Dietary Gut Microbial Metabolites, Short-Chain Fatty Acids, and Host Metabolic Regulation. Nutrients 2015, 7, 2839–2849. [Google Scholar] [CrossRef]
- Ko, G.-J.; Rhee, C.M.; Kalantar-Zadeh, K.; Joshi, S. The Effects of High-Protein Diets on Kidney Health and Longevity. J. Am. Soc. Nephrol. JASN 2020, 31, 1667–1679. [Google Scholar] [CrossRef]
- Ang, Q.Y.; Alexander, M.; Newman, J.C.; Tian, Y.; Cai, J.; Upadhyay, V.; Turnbaugh, J.A.; Verdin, E.; Hall, K.D.; Leibel, R.L.; et al. Ketogenic Diets Alter the Gut Microbiome Resulting in Decreased Intestinal Th17 Cells. Cell 2020, 181, 1263–1275.e16. [Google Scholar] [CrossRef]
- Kim, S.M.; Song, I.H. The Clinical Impact of Gut Microbiota in Chronic Kidney Disease. Korean J. Intern. Med. 2020, 35, 1305–1316. [Google Scholar] [CrossRef]
- Zhao, X.; Zhang, Z.; Hu, B.; Huang, W.; Yuan, C.; Zou, L. Response of Gut Microbiota to Metabolite Changes Induced by Endurance Exercise. Front. Microbiol. 2018, 9, 765. [Google Scholar] [CrossRef]
- Branchereau, M.; Burcelin, R.; Heymes, C. The Gut Microbiome and Heart Failure: A Better Gut for a Better Heart. Rev. Endocr. Metab. Disord. 2019, 20, 407–414. [Google Scholar] [CrossRef]
- Lam, V.; Su, J.; Koprowski, S.; Hsu, A.; Tweddell, J.S.; Rafiee, P.; Gross, G.J.; Salzman, N.H.; Baker, J.E. Intestinal microbiota determine severity of myocardial infarction in rats. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2012, 26, 1727–1735. [Google Scholar] [CrossRef]
- Gan, X.T.; Ettinger, G.; Huang, C.X.; Burton, J.P.; Haist, J.V.; Rajapurohitam, V.; Sidaway, J.E.; Martin, G.; Gloor, G.B.; Swann, J.R.; et al. Probiotic administration attenuates myocardial hypertrophy and heart failure after myocardial infarction in the rat. Circulation. Heart Fail. 2014, 7, 491–499. [Google Scholar] [CrossRef]
- Costanza, A.C.; Moscavitch, S.D.; Faria Neto, H.C.C.; Mesquita, E.T. Probiotic Therapy with Saccharomyces Boulardii for Heart Failure Patients: A Randomized, Double-Blind, Placebo-Controlled Pilot Trial. Int. J. Cardiol. 2015, 179, 348–350. [Google Scholar] [CrossRef]
- Dobrek, Ł. Potential therapeutic options targeting the gut dysbiosis in chronic kidney disease. Wiadomosci Lek. Wars. Pol. 1960 2022, 75, 1757–1764. [Google Scholar] [CrossRef]
- Ranganathan, N.; Ranganathan, P.; Friedman, E.A.; Joseph, A.; Delano, B.; Goldfarb, D.S.; Tam, P.; Rao, A.V.; Anteyi, E.; Musso, C.G. Pilot Study of Probiotic Dietary Supplementation for Promoting Healthy Kidney Function in Patients with Chronic Kidney Disease. Adv. Ther. 2010, 27, 634–647. [Google Scholar] [CrossRef]
- Yao, S.; Zhao, Y.; Chen, H.; Sun, R.; Chen, L.; Huang, J.; Yu, Z.; Chen, S. Exploring the Plasticity of Diet on Gut Microbiota and Its Correlation with Gut Health. Nutrients 2023, 15, 3460. [Google Scholar] [CrossRef]
- Coss-Adame, E.; Remes-Troche, J.M.; Flores Rendón, R.; Tamayo de la Cuesta, J.L.; Valdovinos Díaz, M.A. Efficacy and Safety of Lubiprostone for the Treatment of Chronic Idiopathic Constipation: A Phase 3, Randomized, Placebo-Controlled Study. Rev. Gastroenterol. Mex. Engl. 2023, in press. [CrossRef]
- Cha, R.R.; Park, S.-Y.; Camilleri, M. Constipation in Patients with Chronic Kidney Disease. J. Neurogastroenterol. Motil. 2023, 29, 428–435. [Google Scholar] [CrossRef]
- Caggiano, G.; Cosola, C.; Di Leo, V.; Gesualdo, M.; Gesualdo, L. Microbiome Modulation to Correct Uremic Toxins and to Preserve Kidney Functions. Curr. Opin. Nephrol. Hypertens. 2020, 29, 49–56. [Google Scholar] [CrossRef]
- Lee, D.M.; Battson, M.L.; Jarrell, D.K.; Hou, S.; Ecton, K.E.; Weir, T.L.; Gentile, C.L. SGLT2 Inhibition via Dapagliflozin Improves Generalized Vascular Dysfunction and Alters the Gut Microbiota in Type 2 Diabetic Mice. Cardiovasc. Diabetol. 2018, 17, 62. [Google Scholar] [CrossRef]
- McDonald, L.C.; Gerding, D.N.; Johnson, S.; Bakken, J.S.; Carroll, K.C.; Coffin, S.E.; Dubberke, E.R.; Garey, K.W.; Gould, C.V.; Kelly, C.; et al. Clinical Practice Guidelines for Clostridium Difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2018, 66, e1–e48. [Google Scholar] [CrossRef]
- Bica, I.-C.; Pietroșel, V.-A.; Salmen, T.; Diaconu, C.-T.; Fierbinteanu Braticevici, C.; Stoica, R.-A.; Suceveanu, A.I.; Pantea Stoian, A. The Effects of Cardioprotective Antidiabetic Therapy on Microbiota in Patients with Type 2 Diabetes Mellitus-A Systematic Review. Int. J. Mol. Sci. 2023, 24, 7184. [Google Scholar] [CrossRef]
- Bao, N.; Liu, X.; Zhong, X.; Jia, S.; Hua, N.; Zhang, L.; Mo, G. Dapagliflozin-Affected Endothelial Dysfunction and Altered Gut Microbiota in Mice with Heart Failure. PeerJ 2023, 11, e15589. [Google Scholar] [CrossRef]
- Milosevic, I.; Vujovic, A.; Barac, A.; Djelic, M.; Korac, M.; Radovanovic Spurnic, A.; Gmizic, I.; Stevanovic, O.; Djordjevic, V.; Lekic, N.; et al. Gut-Liver Axis, Gut Microbiota, and Its Modulation in the Management of Liver Diseases: A Review of the Literature. Int. J. Mol. Sci. 2019, 20, 395. [Google Scholar] [CrossRef]
- Jiang, S.; Shui, Y.; Cui, Y.; Tang, C.; Wang, X.; Qiu, X.; Hu, W.; Fei, L.; Li, Y.; Zhang, S.; et al. Gut Microbiota Dependent Trimethylamine N-Oxide Aggravates Angiotensin II-Induced Hypertension. Redox Biol. 2021, 46, 102115. [Google Scholar] [CrossRef]
- Cammarota, G.; Ianiro, G.; Tilg, H.; Rajilić-Stojanović, M.; Kump, P.; Satokari, R.; Sokol, H.; Arkkila, P.; Pintus, C.; Hart, A.; et al. European Consensus Conference on Faecal Microbiota Transplantation in Clinical Practice. Gut 2017, 66, 569–580. [Google Scholar] [CrossRef]
- Wu, L.; Lu, X.-J.; Lin, D.-J.; Chen, W.-J.; Xue, X.-Y.; Liu, T.; Xu, J.-T.; Xie, Y.-T.; Li, M.-Q.; Lin, W.-Y.; et al. Washed Microbiota Transplantation Improves Patients with Metabolic Syndrome in South China. Front. Cell. Infect. Microbiol. 2022, 12, 1044957. [Google Scholar] [CrossRef]
- Stachowska, E.; Wiśniewska, M.; Dzieżyc, A.; Bohatyrewicz, A. Could the Use of Butyric Acid Have a Positive Effect on Microbiota and Treatment of Type 2 Diabetes? Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 4570–4578. [Google Scholar] [CrossRef]
- Ponziani, F.R.; Coppola, G.; Rio, P.; Caldarelli, M.; Borriello, R.; Gambassi, G.; Gasbarrini, A.; Cianci, R. Factors Influencing Microbiota in Modulating Vaccine Immune Response: A Long Way to Go. Vaccines 2023, 11, 1609. [Google Scholar] [CrossRef]
- Airola, C.; Severino, A.; Porcari, S.; Fusco, W.; Mullish, B.H.; Gasbarrini, A.; Cammarota, G.; Ponziani, F.R.; Ianiro, G. Future Modulation of Gut Microbiota: From Eubiotics to FMT, Engineered Bacteria, and Phage Therapy. Antibiotics 2023, 12, 868. [Google Scholar] [CrossRef]
- Triposkiadis, F.; Xanthopoulos, A.; Parissis, J.; Butler, J.; Farmakis, D. Pathogenesis of Chronic Heart Failure: Cardiovascular Aging, Risk Factors, Comorbidities, and Disease Modifiers. Heart Fail. Rev. 2022, 27, 337–344. [Google Scholar] [CrossRef]
- Proctor, L. Priorities for the next 10 Years of Human Microbiome Research. Nature 2019, 569, 623–625. [Google Scholar] [CrossRef]
| Metabolites | Microbial Origin | Consequences | References |
|---|---|---|---|
| LPS | Component of gut microbiota, constituent of Gram-negative bacteria | Gut and systemic inflammation | [29,82] |
| SCFAs | Microbial products from fiber fermentation, energy source of gut microbiota | Immune modulation: phagocytosis, ROS production, integrity of the gut barrier, HDAC inhibition and GPCR activation, differentiation of T-lymphocytes | [29,30,31,48] |
| TMAO | Microbial product deriving from the oxidation of TMA, produced from the metabolism of choline-containing products | Inflammation, plaque instability, MACE, NLRP3 inflammasome activation, cardiac inflammation and fibrosis, kidney damage | [74,106,109,120] |
| PAGln | Microbial product, phenylalanine metabolite | Heart failure, increase in NT-proBNP, negative inotropic effect | [64,65] |
| IxS pCS IAA | Microbial products Uremic toxins | NLRP3 inflammasome activation, cardiac inflammation and fibrosis, endothelial damage, kidney damage with tubulointerstitial fibrosis and glomerular sclerosis, uremic dysbiosis | [74,79,103,104] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caldarelli, M.; Franza, L.; Rio, P.; Gasbarrini, A.; Gambassi, G.; Cianci, R. Gut–Kidney–Heart: A Novel Trilogy. Biomedicines 2023, 11, 3063. https://doi.org/10.3390/biomedicines11113063
Caldarelli M, Franza L, Rio P, Gasbarrini A, Gambassi G, Cianci R. Gut–Kidney–Heart: A Novel Trilogy. Biomedicines. 2023; 11(11):3063. https://doi.org/10.3390/biomedicines11113063
Chicago/Turabian StyleCaldarelli, Mario, Laura Franza, Pierluigi Rio, Antonio Gasbarrini, Giovanni Gambassi, and Rossella Cianci. 2023. "Gut–Kidney–Heart: A Novel Trilogy" Biomedicines 11, no. 11: 3063. https://doi.org/10.3390/biomedicines11113063
APA StyleCaldarelli, M., Franza, L., Rio, P., Gasbarrini, A., Gambassi, G., & Cianci, R. (2023). Gut–Kidney–Heart: A Novel Trilogy. Biomedicines, 11(11), 3063. https://doi.org/10.3390/biomedicines11113063










