Characterisation of Ferritin–Lymphocyte Ratio in COVID-19
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Data Collection
2.3. Ethical Approval
2.4. Study Endpoints
2.5. Statistical Analysis
3. Results
3.1. Baseline Patient Characteristics
3.2. Clinical and Laboratory Results
3.3. FLR Distributions and Correlations
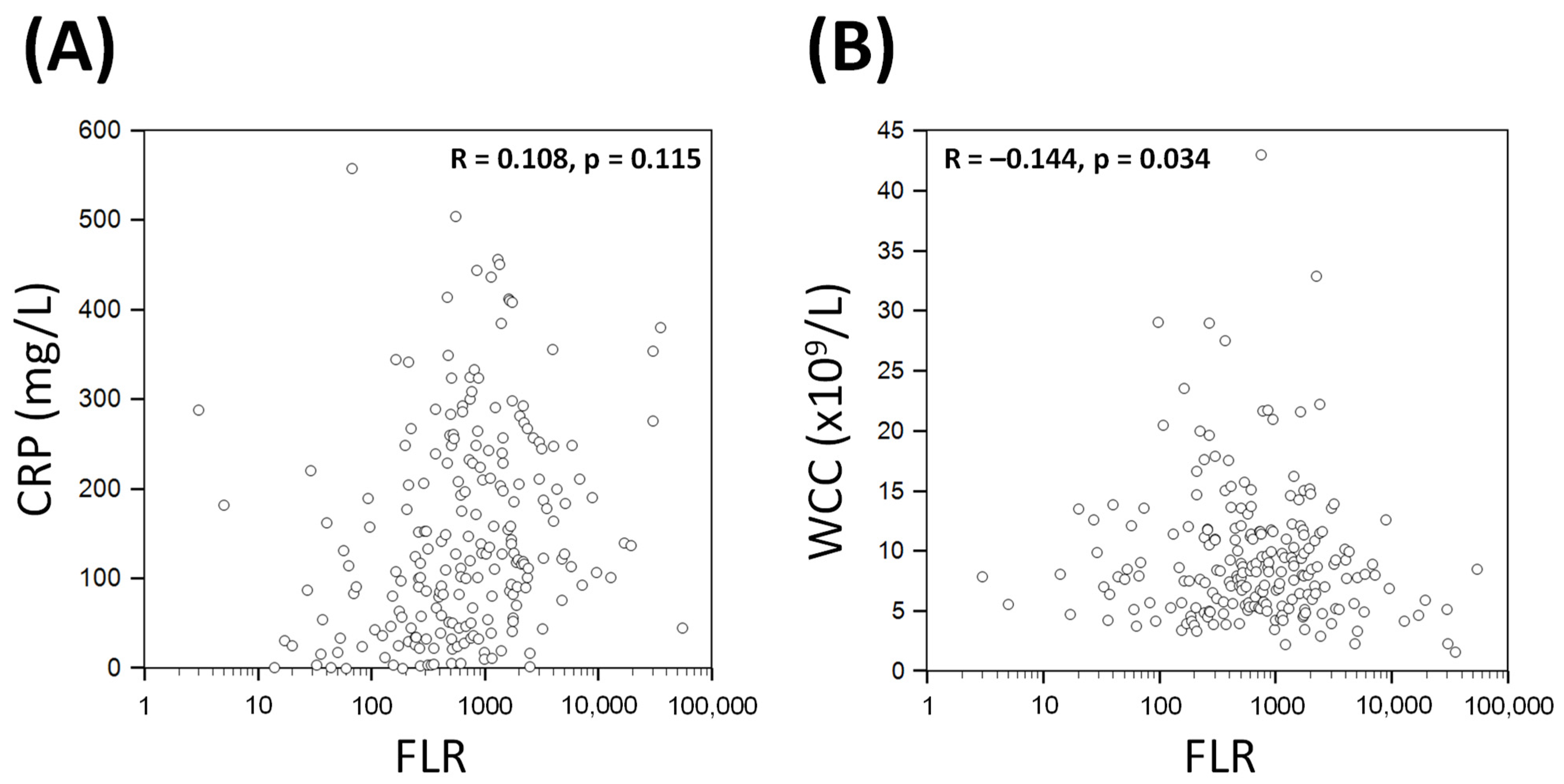
3.4. Diagnostic Performance for Predicting Clinical Outcomes
3.5. Survival Analysis
4. Discussion
4.1. FLR as a Rule-Out Test for Adverse Outcomes in COVID-19
4.2. FLR as a Combination Biomarker
4.3. Improving FLR
4.4. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singh, P.; Warren, K.; Adler, H.; Mangano, A.; Sansbury, J.; Duff, R. A Retrospective Review of Outcomes in Intensive Care Unit Patients Infected With SARS-Cov2 in Correlation to Admission Acute Physiologic Assessment and Chronic Health Evaluation II Scores. Cureus 2021, 13, e14051. [Google Scholar] [CrossRef]
- Botoș, I.D.; Pantiș, C.; Bodolea, C.; Nemes, A.; Crișan, D.; Avram, L.; Negrău, M.O.; Hirișcău, I.E.; Crăciun, R.; Puia, C.I. The Dynamics of the Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios Predict Progression to Septic Shock and Death in Patients with Prolonged Intensive Care Unit Stay. Medicina 2022, 59, 32. [Google Scholar] [CrossRef] [PubMed]
- Kosidło, J.W.; Wolszczak-Biedrzycka, B.; Matowicka-Karna, J.; Dymicka-Piekarska, V.; Dorf, J. Clinical Significance and Diagnostic Utility of NLR, LMR, PLR and SII in the Course of COVID-19: A Literature Review. J. Inflamm. Res. 2023, 16, 539–562. [Google Scholar] [CrossRef] [PubMed]
- Mayne, K.J.; Lees, J.S.; Rutherford, E.; Thomson, P.C.; Traynor, J.P.; Dey, V.; Lang, N.N.; Mark, P.B. Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios: Associations with mortality in a haemodialysis cohort. Clin. Kidney J. 2023, 16, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Liu, A.; Hammond, R.; Chan, K.; Chukwuenweniwe, C.; Johnson, R.; Khair, D.; Duck, E.; Olubodun, O.; Barwick, K.; Banya, W.; et al. Comparison of Lymphocyte-CRP Ratio to Conventional Inflammatory Markers for Predicting Clinical Outcomes in COVID-19. J. Pers. Med. 2023, 13, 909. [Google Scholar] [CrossRef] [PubMed]
- Aygun, H.; Eraybar, S. Can ferritin/lymphocyte percentage ratio, a new indicator, predict the clinical course of COVID-19 cases? Bratisl. Lek. Listy 2021, 122, 799–804. [Google Scholar] [CrossRef]
- Kernan, K.F.; Carcillo, J.A. Hyperferritinemia and inflammation. Int. Immunol. 2017, 29, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Li, H.; Li, L.; Liu, C.; Yan, S.; Chen, H.; Li, Y. Ferritin in the coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. J. Clin. Lab. Anal. 2020, 34, e23618. [Google Scholar] [CrossRef]
- Feld, J.; Tremblay, D.; Thibaud, S.; Kessler, A.; Naymagon, L. Ferritin levels in patients with COVID-19: A poor predictor of mortality and hemophagocytic lymphohistiocytosis. Int. J. Lab. Hematol. 2020, 42, 773–779. [Google Scholar] [CrossRef]
- Sharif, K.; Vieira Borba, V.; Zandman-Goddard, G.; Shoenfeld, Y. Eppur Si Muove: Ferritin is essential in modulating inflammation. Clin. Exp. Immunol. 2018, 191, 149–150. [Google Scholar] [CrossRef]
- Huang, I.; Pranata, R. Lymphopenia in severe coronavirus disease-2019 (COVID-19): Systematic review and meta-analysis. J. Intensive Care 2020, 8, 36. [Google Scholar] [CrossRef] [PubMed]
- Forman, D.T.; Parker, S.L. The measurement and interpretation of serum ferritin. Ann. Clin. Lab. Sci. 1980, 10, 345–350. [Google Scholar] [PubMed]
- Li, Y.; Yang, T.; Wang, S.; Zheng, J.; Zhou, J.; Jiang, M.; Zhou, T.; Cao, Y.; Wang, H. The value of lymphocyte count in determining the severity of COVID-19 and estimating the time for nucleic acid test results to turn negative. Bosn. J. Basic Med. Sci. 2021, 21, 235–241. [Google Scholar] [CrossRef]
- Dodge, Y. Kolmogorov–Smirnov Test. In The Concise Encyclopedia of Statistics; Springer: New York, NY, USA, 2008; pp. 283–287. [Google Scholar]
- Altman, D.G.; Gore, S.M.; Gardner, M.J.; Pocock, S.J. Statistical guidelines for contributors to medical journals. Br. Med. J. (Clin. Res. Ed.) 1983, 286, 1489–1493. [Google Scholar] [CrossRef]
- Campbell, I. Chi-squared and Fisher-Irwin tests of two-by-two tables with small sample recommendations. Stat. Med. 2007, 26, 3661–3675. [Google Scholar] [CrossRef]
- Kirch, W. (Ed.) Pearson’s Correlation Coefficient. In Encyclopedia of Public Health; Springer: Dordrecht, The Netherlands, 2008; pp. 1090–1091. [Google Scholar]
- Hanley, J.A. Receiver operating characteristic (ROC) methodology: The state of the art. Crit. Rev. Diagn. Imaging 1989, 29, 307–335. [Google Scholar]
- Fluss, R.; Faraggi, D.; Reiser, B. Estimation of the Youden Index and its associated cutoff point. Biom. J. Biom. Z. 2005, 47, 458–472. [Google Scholar] [CrossRef]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- Kaplan, E.L.; Meier, P. Nonparametric Estimation from Incomplete Observations. J. Am. Stat. Assoc. 1958, 53, 457–481. [Google Scholar] [CrossRef]
- Logothetis, C.N.; Weppelmann, T.A.; Jordan, A.; Hanna, C.; Zhang, S.; Charkowick, S.; Oxner, A. D-Dimer Testing for the Exclusion of Pulmonary Embolism Among Hospitalized Patients With COVID-19. JAMA Netw. Open 2021, 4, e2128802. [Google Scholar] [CrossRef]
- Liu, A.; Hammond, R.; Chan, K.; Chukwuenweniwe, C.; Johnson, R.; Khair, D.; Duck, E.; Olubodun, O.; Barwick, K.; Banya, W.; et al. Normal high-sensitivity cardiac troponin for ruling-out inpatient mortality in acute COVID-19. PLoS ONE 2023, 18, e0284523. [Google Scholar] [CrossRef] [PubMed]
- Morello, F.; Bima, P.; Giamello, J.D.; Baricocchi, D.; Risi, F.; Vesan, M.; Pivetta, E.E.; de Stefano, G.; Chiarlo, M.; Veglia, S.; et al. A 4C mortality score based dichotomic rule supports Emergency Department discharge of COVID-19 patients. Minerva Med. 2023, 113, 916–926. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.W.X.; Sutjipto, S.; Lee, P.H.; Dugan, C.; Khoo, B.Y.; Ren, D.; Young, B.E.; Lye, D.C. Validation of ISARIC 4C mortality and deterioration scores in a mixed vaccination status cohort of hospitalized COVID-19 patients in Singapore. Clin. Infect. Dis. 2022, 75, e874–e877. [Google Scholar] [CrossRef]
- Liu, A.; Hammond, R.; Donnelly, P.D.; Kaski, J.C.; Coates, A.R.M. Effective prognostic and clinical risk stratification in COVID-19 using multimodality biomarkers. J. Intern. Med. 2023, 294, 21–46. [Google Scholar] [CrossRef] [PubMed]
- Liu, A.; Hammond, R.; Chan, K.; Chukwuenweniwe, C.; Johnson, R.; Khair, D.; Duck, E.; Olubodun, O.; Barwick, K.; Banya, W.; et al. Low CRB-65 Scores Effectively Rule out Adverse Clinical Outcomes in COVID-19 Irrespective of Chest Radiographic Abnormalities. Biomedicines 2023, 11, 2423. [Google Scholar] [CrossRef]
- Coates, A.R.M.; Hu, Y.; Holt, J.; Yeh, P. Antibiotic combination therapy against resistant bacterial infections: Synergy, rejuvenation and resistance reduction. Expert Rev. Anti-Infect. Ther. 2020, 18, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Tonduangu, N.; Le Borgne, P.; Lefebvre, F.; Alame, K.; Berard, L.; Gottwalles, Y.; Cipolat, L.; Gennai, S.; Bilbault, P.; Lavoignet, C.E.; et al. Prognostic Value of C-Reactive Protein to Lymphocyte Ratio (CLR) in Emergency Department Patients with SARS-CoV-2 Infection. J. Pers. Med. 2021, 11, 1274. [Google Scholar] [CrossRef]
- Kang, D.; Kirienko, N.V. Interdependence between iron acquisition and biofilm formation in Pseudomonas aeruginosa. J. Microbiol. 2018, 56, 449–457. [Google Scholar] [CrossRef]
- Lin, M.H.; Shu, J.C.; Huang, H.Y.; Cheng, Y.C. Involvement of iron in biofilm formation by Staphylococcus aureus. PLoS ONE 2012, 7, e34388. [Google Scholar] [CrossRef]
- Shillitoe, A.J. The Common Causes of Lymphopenia. J. Clin. Pathol. 1950, 3, 321. [Google Scholar] [CrossRef]
- Huang, W.; Berube, J.; McNamara, M.; Saksena, S.; Hartman, M.; Arshad, T.; Bornheimer, S.J.; O’Gorman, M. Lymphocyte Subset Counts in COVID-19 Patients: A Meta-Analysis. Cytom. A 2020, 97, 772–776. [Google Scholar] [CrossRef] [PubMed]
- Bobcakova, A.; Petriskova, J.; Vysehradsky, R.; Kocan, I.; Kapustova, L.; Barnova, M.; Diamant, Z.; Jesenak, M. Immune Profile in Patients With COVID-19: Lymphocytes Exhaustion Markers in Relationship to Clinical Outcome. Front. Cell. Infect. Microbiol. 2021, 11, 646688. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Gao, Y.; Wang, G.; Song, G.; Liu, S.; Sun, D.; Xu, Y.; Tian, Z. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell. Mol. Immunol. 2020, 17, 533–535. [Google Scholar] [CrossRef]
- Habib, H.M.; Ibrahim, S.; Zaim, A.; Ibrahim, W.H. The role of iron in the pathogenesis of COVID-19 and possible treatment with lactoferrin and other iron chelators. Biomed. Pharmacother. Biomed. Pharmacother. 2021, 136, 111228. [Google Scholar] [CrossRef] [PubMed]
- Zachary, H.; Emily, M. Hereditary haemochromatosis discovered after COVID-19 hospitalisation. BMJ Case Rep. 2023, 16, e253023. [Google Scholar] [CrossRef]
- Lee, J.X.; Chieng, W.K.; Lau, S.C.D.; Tan, C.E. COVID-19 and Hemoglobinopathies: A Systematic Review of Clinical Presentations, Investigations, and Outcomes. Front. Med. 2021, 8, 757510. [Google Scholar] [CrossRef]



| All Patients (n = 217) | Survivors (n = 159) | Non-Survivors (n = 58) | p Value | |
|---|---|---|---|---|
| Age (years) | 69 (55–82) | 64 (52–80) | 75 (66–83) | 0.001 |
| Male (%) | 130 (60) | 95 (60) | 35 (60) | 0.937 |
| BMI (kg/m2) | 26 (22–31) | 26 (22–31) | 26 (23–35) | 0.478 |
| Symptoms | ||||
| Chest pain | 23 (11) | 19 (12) | 4 (7) | 0.285 |
| Cough | 123 (57) | 92 (58) | 31 (53) | 0.561 |
| Dyspnoea | 123 (57) | 86 (54) | 37 (64) | 0.202 |
| Fatigue | 55 (25) | 40 (25) | 15 (26) | 0.916 |
| Fever | 112 (52) | 87 (55) | 25 (43) | 0.130 |
| Comorbidities | ||||
| Atrial fibrillation | 30 (14) | 19 (11) | 11 (19) | 0.185 |
| Ischaemic heart disease | 33 (15) | 15 (9) | 18 (31) | <0.001 |
| Heart failure | 27 (12) | 15 (9) | 12 (21) | 0.026 |
| Hypertension | 101 (47) | 73 (46) | 28 (48) | 0.757 |
| Diabetes | 77 (35) | 52 (33) | 25 (43) | 0.157 |
| Dyslipidaemia | 26 (12) | 17 (11) | 9 (16) | 0.341 |
| Current/ex-smoker | 66 (32) | 44/153 (29) | 22/53 (42) | 0.086 |
| CKD | 74 (34) | 49 (31) | 25 (43) | 0.091 |
| COPD | 27 (12) | 14 (9) | 13 (22) | 0.007 |
| Asthma | 23 (11) | 16 (10) | 7 (12) | 0.671 |
| CVA/TIA | 24 (11) | 15 (9) | 9 (16) | 0.206 |
| Medications | ||||
| ACEi/ARB | 57 (26) | 40 (25) | 17 (29) | 0.532 |
| Aspirin | 40 (18) | 26 (16) | 14 (24) | 0.191 |
| Beta-blockers | 49 (23) | 29 (18) | 20 (34) | 0.011 |
| Statins | 91 (42) | 59 (37) | 32 (55) | 0.017 |
| All Patients (n = 217) | Survivors (n = 159) | Non-Survivors (n = 58) | p Value | |
|---|---|---|---|---|
| Observations on admission | ||||
| Temperature (°C) | 37.2 (36.6–37.9) | 37.1 (36.6–38.0) | 37.2 (36.7–37.9) | 0.792 |
| SBP (mmHg) | 130 (116–146) | 131 (117–147) | 127 (111–138) | 0.033 |
| DBP (mmHg) | 75 ± 14 | 76 ± 14 | 71 ± 16 | 0.014 |
| Respiratory rate (/min) | 22 (19–28) | 20 (19–26) | 23 (20–30) | 0.053 |
| Laboratory results | ||||
| FLR | 711 (272–1722) | 662 (250–1543) | 848 (447–2157) | 0.026 |
| Ferritin (ng/mL) | 697 (265–1236) | 663 (226–1216) | 843 (392–1493) | 0.108 |
| Lymphocyte count (×109/L) | 0.87 (0.63–1.21) | 0.90 (0.64–1.31) | 0.73 (0.50–1.04) | 0.015 |
| CRP (mg/L) | 123 (53–229) | 111 (44–208) | 159 (101–282) | 0.001 |
| Haemoglobin (g/L) | 123 ± 24 | 125 ± 25 | 118 ± 20 | 0.027 |
| WCC (109/L) | 8.1 (5.5–11.5) | 7.9 (5.7–11.6) | 8.6 (5.3–11.2) | 0.815 |
| Platelet Count (109/L) | 234 (183–300) | 238 (194–292) | 221 (160–314) | 0.344 |
| Sodium (mmol/L) | 138 (134–140) | 137 (134–140) | 138 (134–141) | 0.635 |
| Potassium (mmol/L) | 4.3 (3.9–4.7) | 4.3 (3.9–4.6) | 4.5 (4.0–5.0) | 0.028 |
| Creatinine (μmol/L) | 96 (75–185) | 91 (72–153) | 123 (83–241) | 0.055 |
| Complications | ||||
| NIV requirement | 48 (22) | 26 (16) | 22 (38) | 0.001 |
| ICU admission | 35 (16) | 24 (15) | 11 (19) | 0.493 |
| Intubation | 18 (8) | 13 (8) | 5 (9) | 1.000 |
| Mortality | NIV Requirement | Intubation/ICU | |
|---|---|---|---|
| AUC | 0.60 | 0.55 | 0.58 |
| AUC 95% CI | 0.53–0.67 | 0.48–0.62 | 0.52–0.65 |
| AUC p-value | 0.023 | 0.312 | 0.098 |
| Optimal cut-off (Youden; [19]) | 286 | 356 | 368 |
| Sensitivity (95% CI) | 86% (75–94) | 79% (65–90) | 86% (70–95) |
| Specificity (95% CI) | 30% (23–38) | 33% (26–40) | 34% (27–41) |
| Positive LR (95% CI) | 1.2 (1.1–1.4) | 1.2 (1.0–1.4) | 1.3 (1.1–1.5) |
| Negative LR (95% CI) | 0.5 (0.2–0.9) | 0.6 (0.4–1.2) | 0.4 (0.2–1.0) |
| PPV (95% CI) | 31% (28–34) | 25% (22–29) | 20% (17–23) |
| NPV (95% CI) | 86% (75–92) | 85% (75–91) | 93% (84–97) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, A.; Hammond, R.; Chan, K.; Chukwuenweniwe, C.; Johnson, R.; Khair, D.; Duck, E.; Olubodun, O.; Barwick, K.; Banya, W.; et al. Characterisation of Ferritin–Lymphocyte Ratio in COVID-19. Biomedicines 2023, 11, 2819. https://doi.org/10.3390/biomedicines11102819
Liu A, Hammond R, Chan K, Chukwuenweniwe C, Johnson R, Khair D, Duck E, Olubodun O, Barwick K, Banya W, et al. Characterisation of Ferritin–Lymphocyte Ratio in COVID-19. Biomedicines. 2023; 11(10):2819. https://doi.org/10.3390/biomedicines11102819
Chicago/Turabian StyleLiu, Alexander, Robert Hammond, Kenneth Chan, Chukwugozie Chukwuenweniwe, Rebecca Johnson, Duaa Khair, Eleanor Duck, Oluwaseun Olubodun, Kristian Barwick, Winston Banya, and et al. 2023. "Characterisation of Ferritin–Lymphocyte Ratio in COVID-19" Biomedicines 11, no. 10: 2819. https://doi.org/10.3390/biomedicines11102819
APA StyleLiu, A., Hammond, R., Chan, K., Chukwuenweniwe, C., Johnson, R., Khair, D., Duck, E., Olubodun, O., Barwick, K., Banya, W., Stirrup, J., Donnelly, P. D., Kaski, J. C., & Coates, A. R. M. (2023). Characterisation of Ferritin–Lymphocyte Ratio in COVID-19. Biomedicines, 11(10), 2819. https://doi.org/10.3390/biomedicines11102819








