METCAM Is a Potential Biomarker for Predicting the Malignant Propensity of and as a Therapeutic Target for Prostate Cancer
Abstract
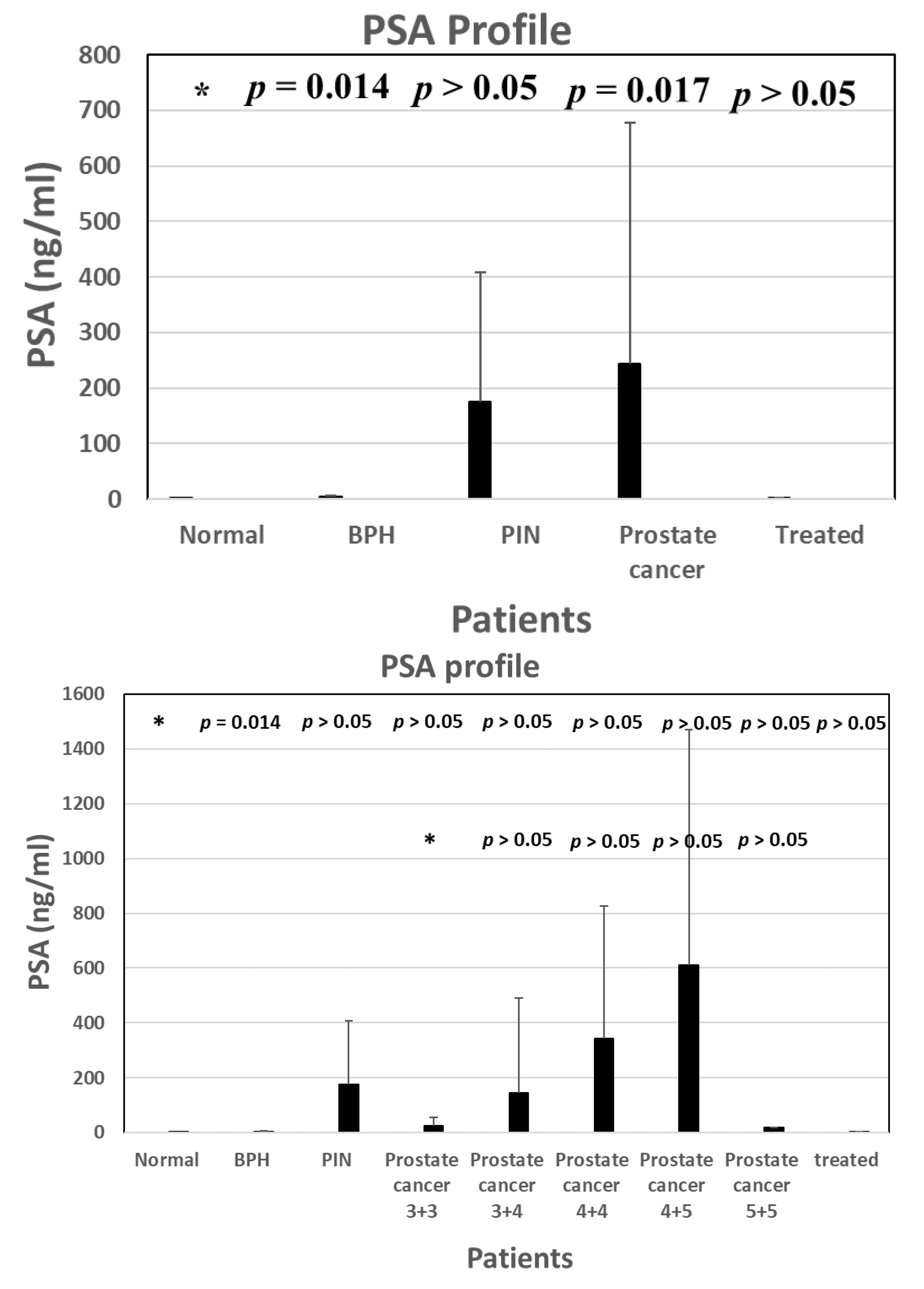
1. Current State of Clinical Diagnosis of Malignant Prostate Cancer
2. Human METCAM (huMETCAM) Is Overly Expressed in Prostate Cancer Tissues and in TRAMP, Suggesting That It May Serve as a Biomarker for Predicting the Malignant Potential of Prostatic Tumors
3. Using Various Immunological Methods to Validate METCAM as a Diagnostic Marker for Predicting the Malignant Propensity of Prostate Cancer
3.1. Use of Three Immunological Methods—Immunoblot (Western Blot), ELISA, and Traditional LFIA—To Test Whether METCAM May Serve as a Biomarker for the Malignant Potential of Prostate Cancer
3.2. Using a Magnetic Bead-Enriched Array Display Immunoassay (MBIA) Method also Supports the above Notion
3.3. Using a Modified LFIA Method Not only Supports the above Notion but also Further Shows That METCAM Can Be Used to Predict Malignant Propensity at the Pre-Malignant (Pin) Stage
3.4. Using Magnetic-Beads to Purify the METCAM from Serum Samples and, Subsequently, Subject Them to the Modified LFIA, which also Supports the above Notion
3.5. Direct Application of Triple Complexes to the Modified LFIA
4. METCAM Plays a Positive Role in the Malignant Progression of Most Prostate Carcinoma Cells
5. METCAM as a Therapeutic Target for Clinical Treatment of Patients with Malignant Prostate Cancer
6. Conclusions and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics CA Cancer. J. Clin. 2020, 70, 7–30. [Google Scholar]
- Catalona, W.J.; Scott, W.W. Carcinoma of the prostate: A review. J. Urol. 1978, 119, 1–8. [Google Scholar] [CrossRef]
- Wood Jr, D.P.; Banks, E.R.; Humphreys, S.; McRoberts, J.W.; Rangneker, V.M. Identification of bone marrow micro-metastases in patients with prostate cancer. Cancer 1994, 74, 2533–2540. [Google Scholar] [CrossRef]
- Liu, J.; Li, Y.; Yang, N.; Yang, C.; Mao, L. Current state of biomarkers for the diagnosis and assessment of treatment efficacy of prostate cancer. Discov. Med. 2019, 27, 235–243. [Google Scholar]
- Murphy, L.; Watson, R.W. Patented prostate cancer biomarkers. Nat. Rev. Urol. 2012, 9, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Ferro, M.; De Cobelli, O.; Lucarelli, G.; Porreca, A.; Busetto, G.M.; Cantiello, F.; Damiano, R.; Autorino, R.; Musi, G.; Vartolomei, M.D.; et al. Beyond PSA: The Role of Prostate Health Index (phi). Int. J. Mol. Sci. 2020, 21, 1184. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Cao, W.; Li, Q.; Shen, H.; Liu, C.; Deng, J.; Xu, J.; Shao, Q. Evaluation of prostate cancer antigen 3 for detecting prostate cancer: A systematic review and meta-analysis. Sci. Rep. 2016, 6, 25776. [Google Scholar] [CrossRef]
- Kohaar, I.; Petrovics, G.; Srivastava, S. A Rich Array of Prostate Cancer Molecular Biomarkers: Opportunities and Challenges. Int. J. Mol. Sci. 2019, 20, 1813. [Google Scholar] [CrossRef] [PubMed]
- Tomlins, S.A.; Day, J.R.; Lonigro, R.J.; Hovelson, D.H.; Siddiqui, J.; Kunju, L.P.; Dunn, R.L.; Meyer, S.; Hodge, P.; Groskopf, J.; et al. Urine TMPRSS2:ERG Plus PCA3 for Individualized Prostate Cancer Risk Assessment. Eur. Urol. 2015, 70, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Di Minno, A.; Aveta, A.; Gelzo, M.; Tripodi, L.; Pandolfo, S.D.; Crocetto, F.; Imbimbo, C.; Castaldo, G. 8-Hydroxy-2-Deoxyguanosine and 8-Iso-Prostaglandin F2α: Putative Biomarkers to assess Oxidative Stress Damage Following Robot-Assisted Radical Prostatectomy (RARP). J. Clin. Med. 2022, 11, 6102. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, J.M.; Reithmuller, G.; Johnson, J.P. MUC18, a marker of tumor progression in human melanoma. Proc. Natl. Acad. Sci. USA 1989, 86, 9891–9895. [Google Scholar] [CrossRef]
- Wu, G.-J.; Wu, M.-W.H.; Wang, S.-W.; Liu, Z.; Qu, P.; Peng, Q.; Yang, H.; Varma, V.A.; Sun, Q.C.; Petros, J.A.; et al. Isolation and characterization of the major form of human MUC18 cDNA gene and correlation of MUC18 over-expression in prostate cancer cell lines and tissues with malignant progression. Gene 2001, 279, 17–31. [Google Scholar] [CrossRef]
- Shih, I.M.; Elder, D.E.; Hsu, M.Y.; Herlyn, M. Regulation of Mel-CAM/MUC18 expression on melanocytes of different stages of tumor progression by normal keratinocytes. Am. J. Pathol. 1994, 145, 837–845. [Google Scholar] [PubMed]
- Xie, S.; Luca, M.; Huang, S.; Gutman, M.; Reich, R.; Johnson, J.P.; Bar-Eli, M. Expression of MCAM/MCU18 by human melanoma cells leads to increased tumor growth and metastasis. Cancer Res. 1997, 57, 2295–2303. [Google Scholar] [PubMed]
- Anfosso, F.; Bardin, N.; Francès, V.; Vivier, E.; Camoin-Jau, L.; Sampol, J.; Dignat-George, F. Activation of Human Endothelial Cells via S-Endo-1 Antigen (CD146) Stimulates the Tyrosine Phosphorylation of Focal Adhesion Kinase p125FAK. J. Biol. Chem. 1998, 273, 26852–26856. [Google Scholar] [CrossRef]
- Shih, I.M.; Elder, D.E.; Speicher, D.; Johnson, J.P.; Herlyn, M. Isolation and functional characterization of the A32 melanoma-associated antigen. Cancer Res. 1994, 54, 2514–2520. [Google Scholar] [PubMed]
- Wu, G.J. METCAM/MUC18 and cancer metastasis. Curr. Genom. 2005, 6, 333–349. [Google Scholar] [CrossRef]
- Wu, G.J. Dual Roles of METCAM in the Progression of Different Cancers. J. Oncol. 2012, 2012, 853797. [Google Scholar] [CrossRef]
- Shih, I.-M. The role of CD146 (Mel-CAM) in biology and pathology. J. Pathol. 1999, 189, 4–11. [Google Scholar] [CrossRef]
- Wu, G.-J.; Dickerson, E.B. Frequent and increased expression of human METCAM/MUC18 in cancer tissues and metastatic lesions is associated with the clinical progression of human ovarian carcinoma. Taiwan. J. Obstet. Gynecol. 2014, 53, 509–517. [Google Scholar] [CrossRef]
- Lin, J.C.; Chiang, C.F.; Wang, S.W.; Wang, W.Y.; Kwuan, P.C.; Wu, G.J. Significance and expression of human METCAM/MUC18 in nasopharyngeal carcinoma (NPC) and metastatic lesions. Asian Pac. J. Cancer Prev. 2014, 15, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.-J.; Varma, V.A.; Wu, M.-W.H.; Wang, S.-W.; Qu, P.; Yang, H.; Petros, J.A.; Lim, S.D.; Amin, M.B. Expression of a human cell adhesion molecule, MUC18, in prostate cancer cell lines and tissues. Prostate 2001, 48, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Zeng, G.; Cai, S.; Liu, Y.; Wu, G.-J. METCAM/MUC18 augments migration, invasion, and tumorigenicity of human breast cancer SK-BR-3 cells. Gene 2012, 492, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Wang, S.W.C.; Liu, Z.; Wu, M.W.H.; Armstrong, C.; Wu, G.J. Isolation and characterization of murine MUC18 cDNA gene, and correlation of MUC18 expression in murine melanoma cell lines with metastatic ability. Gene 2001, 265, 133–145. [Google Scholar] [CrossRef]
- Wu, G.-J.; Fu, P.; Wang, S.-W.; Wu, M.-W.H. Enforced Expression of MCAM/MUC18 Increases In vitro Motility and Invasiveness and In vivo Metastasis of Two Mouse Melanoma K1735 Sublines in a Syngeneic Mouse Model. Mol. Cancer Res. 2008, 6, 1666–1677. [Google Scholar] [CrossRef]
- Wu, G.-J. Ectopic expression of MCAM/MUC18 increases in vitro motility and invasiveness, but decreases in vivo tumorigenesis and metastasis of a mouse melanoma K1735-9 subline in a syngeneic mouse model. Clin. Exp. Metastasis 2016, 33, 817–828. [Google Scholar] [CrossRef]
- Huang, C.-Y.; Wu, G.J. Mechanism of METCAM/MUC18-promoted progression of human breast cancer cells: METCAM/MUC18 promoted tumorigenesis of human breast cancer SK-BR-3 cells in a dosage-specific manner. Taiwan. J. Obstet. Gynecol. 2016, 55, 202–212. [Google Scholar] [CrossRef]
- Zeng, Q.; Li, W.; Lu, D.; Wu, Z.; Duan, H.; Luo, Y.; Feng, J.; Yang, D.; Fu, L.; Yan, X. CD146, an epithelial-mesenchymal transition inducer, is associated with triple-negative breast cancer. Proc. Natl. Acad. Sci. USA 2011, 109, 1127–1132. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.J. Chapter 7: The role of MUC18 in prostate carcinoma. In Immunohistochemistry and in Situ Hybridization of Human Carcinomas; Hayat, M.A., Ed.; Elsevier Sciences/Academic Press: New York, NY, USA, 2004; Volume 4, pp. 347–358. [Google Scholar]
- Wu, G.-J.; Peng, Q.; Fu, P.; Wang, S.-W.; Chiang, C.-F.; Dillehay, D.L.; Wu, M.-W.H. Ectopical expression of human MUC18 increases metastasis of human prostate cancer cells. Gene 2004, 327, 201–213. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.-J.; Wu, M.-W.H.; Wang, C.; Liu, Y. Enforced Expression of METCAM/MUC18 Increases Tumorigenesis of Human Prostate Cancer LNCaP Cells in Nude Mice. J. Urol. 2011, 185, 1504–1512. [Google Scholar] [CrossRef]
- Wu, G.-J. METCAM/MUC18 Decreases the Malignant Propensity of Human Ovarian Carcinoma Cells. Int. J. Mol. Sci. 2018, 19, 2976. [Google Scholar] [CrossRef]
- Liu, Y.-C.; Chen, Y.-J.; Wu, G.-J. METCAM/MUC18 Plays a Tumor Suppressor Role in the Development of Nasopharyngeal Carcinoma Type, I. Int. J. Mol. Sci. 2022, 23, 13389. [Google Scholar] [CrossRef]
- Liu, Y.C. The Putative Role of HuMETCAM in Modulating the Development and Progression of Nasopharyngeal Carcinoma. Master’s Thesis, Chung Yuan Christian University, Taoyuan, Taiwan, 2014. Available online: http://.www.lib.cycu.edu.tw/thesis (accessed on 1 January 2019).
- Wu, G.J. Chapter 13 Dual role of METCAM/MUC18 in the progression of cancer cells. In Gene Expression and Regulation in Mammalian Cells-Transcription from General Aspects; Uchiumi, F., Ed.; InTech-Open Access Publisher: Rijeka, Croatia, 2018; pp. 257–289. ISBN 978-953-51-3856-3. Print ISBN 978-953-51-3855-6. [Google Scholar]
- Wu, G.-J.; Fu, P.; Chiang, C.-F.; Huss, W.J.; Greenberg, N.M.; Wu, M.-W.H. Increased expression of MUC18 correlates with the metastatic progression of mouse prostate adenocarcinoma in the TRAMP model. J. Urol. 2005, 173, 1778–1783. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.J. Human METCAM/MUC18 as a Novel Biomarker to Drive and its Specific SiRNAs to Block the Malignant Progression of Prostate Cancer. J. Cell Sci. Ther. 2015, 6, 5–1000227. [Google Scholar] [CrossRef]
- Pong, Y.-H.; Su, Y.-R.; Lo, H.-W.; Ho, C.-K.; Hsieh, C.-C.; Chu, C.-T.; Chen-Yang, Y.W.; Tsai, V.F.; Wu, J.-C.; Wu, G.-J. METCAM/MUC18 is a new early diagnostic biomarker for the malignant potential of prostate cancer: Validation with Western blot method, enzyme-linked immunosorbent assay and lateral flow immunoassay. Cancer Biomark. 2020, 27, 377–387. [Google Scholar] [CrossRef] [PubMed]
- Bahadır, E.B.; Sezgintürk, M.K. Lateral flow assays: Principles, designs and labels. Trends Anal. Chem. 2016, 82, 286–306. [Google Scholar] [CrossRef]
- Parolo, C.; de la Escosura-Muñiz, A.; Merkoçi, A. Enhanced lateral flow immunoassay using gold nanoparticles loaded with enzymes. Biosens. Bioelectron. 2013, 40, 412–416. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.-C.; Chuang, Y.-H.; Wei, Y.-C.; Hsieh, C.-C.; Pong, Y.-H.; Su, Y.-R.; Tsai, V.; Wu, G.-J. Validating METCAM/MUC18 as a Novel Biomarker to Predict the Malignant Potential of Prostate Cancer at an Early Stage by Using a Modified Gold Nanoparticles-Based Lateral Flow Immunoassay. Diagnostics 2021, 11, 443. [Google Scholar] [CrossRef]
- Wu, G.J. Human METCAM/MUC18 is a New Diagnostic Marker of and a Driver for Promoting and its Specific SiRNAs, Derived Oligopeptides and Antibodies be used for Decreasing the Malignant Progression of Prostate Cancer. J. Stem Cell Res. Ther. 2016, 1, 00035. [Google Scholar] [CrossRef]
- Wei, Y.C. Comparing Magnetic Beads-Enriched Array Display Immunoassay with the Two Gold Nanoparticles-Based Lateral flow Immunoassay for Determination of the Prostate Cancer Biomarker-METCAM/MUC18 Concentration in Human Serum. Master’s Thesis, Chung Yuan Christian University, Taoyuan, Taiwan, 2018. [Google Scholar]
- Chuang, Y.H. Using Magnetic Beads-Enriched Array Display Immunoassay and the GOLD nanoparticles-Based Lateral Flow Immunoassay for Determination of the Prostate Cancer Biomarker-METCAM/MUC18 Concentration in Human Serum. Master’s Thesis, Chung Yuan Christian University, Taoyuan, Taiwan, 2019. [Google Scholar]
- Hsieh, C.C. Using a Gold Nanoparticles-Based Lateral Flow Immunoassay and a Magnetic Beads-Enriched Array Display Immunoassay with a High Affinity Bond for Determining the Prostate Cancer Biomarker-METCAM/MUC18 Concentration in Human Serum. Master’s Thesis, Chung Yuan Christian University, Taoyuan, Taiwan, 2020. [Google Scholar]
- Fu, Y.C. Using a Gold Nanoparticles-Based Lateral Flow IMMUNOASSAY to determine the Prostate Cancer Biomarker METCAM/MUC18 CONCENTRATION in human Serum That Was Purified by Magnetic Bead via a High Affinity Bond. Master’s Thesis, Chung Yuan Christian University, Taoyuan, Taiwan, 2021. [Google Scholar]
- Yan, X.; Lin, Y.; Yang, D.; Shen, Y.; Yuan, M.; Zhang, Z.; Li, P.; Xia, H.; Li, L.; Luo, D.; et al. A novel anti-CD146 monoclonal antibody, AA98, inhibits angiogenesis and tumor growth. Blood 2003, 102, 184–191. [Google Scholar] [CrossRef]
- Leslie, M.C.; Zhao, Y.J.; Lachman, L.B.; Hwu, P.; Wu, G.J.; Bar-Eli, M. Immunization against MUC18/MCAM, a novel antigen that drives melanoma invasion and metastasis. Gene Ther. 2007, 14, 316–323 and 382. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.J.; Son, E.L. Soluble METCAM/MUC18 blocks angiogenesis during tumor formation of human prostate cancer cells. In Proceedings of the 97th Annual Meeting of American Association for the Cancer Research, Washington DC, USA, 1–5 April 2006; Volume 47, p. 252. [Google Scholar]
- Wu, G.J. Chapter METCAM/MUC18 promotes tumor progression and metastasis in most human cancers. In Tumor Progression and Metastasis; Lasfar, A., Ed.; InTech-Open Access Publisher: London, UK, 2020; pp. 1–29. ISBN 978-1-78985-350-6. [Google Scholar]
- Santana-Codina, N.; Mancias, J.D.; Kimmelman, A.C. The Role of Autophagy in Cancer. Annu. Rev. Cancer Biol. 2017, 1, 19–39. [Google Scholar] [CrossRef] [PubMed]
- Yun, C.W.; Lee, S.H. The Roles of Autophagy in Cancer. Int. J. Mol. Sci. 2018, 19, 3466. [Google Scholar] [CrossRef] [PubMed]
- Loizzo, D.; Pandolfo, S.D.; Rogers, D.; Cerrato, C.; di Meo, N.A.; Autorino, R.; Mirone, V.; Ferro, M.; Porta, C.; Stella, A.; et al. Novel Insights into Autophagy and Prostate Cancer: A Comprehensive Review. Int. J. Mol. Sci. 2022, 23, 3826. [Google Scholar] [CrossRef]










| Detection Method | Advantages | Disadvantages |
|---|---|---|
| Western blot analysis | Molecular sizes can be determined | Labor-intensive and results may vary depending on workers. Electrophoresis and electric-blotting equipment are needed. Not sensitive enough. |
| ELISA | More sensitive than WB | Labor-intensive, results vary depending on workers, expensive reader and other equipment for quantitation is needed. |
| Traditional LFIA | More sensitive, accurate, and reproducible than WB and ELISA | Not labor-intensive, results were not easily reproducible. |
| MBIA | Many samples can be quantitated easily on a single glass slide | Results vary among different workers; results were not easily reproducible |
| Modified LFIA | More sensitive and accurate than traditional LFIA; results are easily reproducible | Not many |
| Magnetic bead-purified serum + modified LFIA | Purification step can be used to remove interfering contaminants in the serum samples | Purification step may not be easily reproducible |
| Triple complexes + modified LFIA | More sensitive and accurate than traditional LFIA, results are easily reproducible, simple, inexpensive | Not many |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, J.-C.; Wu, G.-J. METCAM Is a Potential Biomarker for Predicting the Malignant Propensity of and as a Therapeutic Target for Prostate Cancer. Biomedicines 2023, 11, 205. https://doi.org/10.3390/biomedicines11010205
Wu J-C, Wu G-J. METCAM Is a Potential Biomarker for Predicting the Malignant Propensity of and as a Therapeutic Target for Prostate Cancer. Biomedicines. 2023; 11(1):205. https://doi.org/10.3390/biomedicines11010205
Chicago/Turabian StyleWu, Jui-Chuang, and Guang-Jer Wu. 2023. "METCAM Is a Potential Biomarker for Predicting the Malignant Propensity of and as a Therapeutic Target for Prostate Cancer" Biomedicines 11, no. 1: 205. https://doi.org/10.3390/biomedicines11010205
APA StyleWu, J.-C., & Wu, G.-J. (2023). METCAM Is a Potential Biomarker for Predicting the Malignant Propensity of and as a Therapeutic Target for Prostate Cancer. Biomedicines, 11(1), 205. https://doi.org/10.3390/biomedicines11010205







