Pancreatic Pathological Changes in Murine Toxoplasmosis and Possible Association with Diabetes Mellitus
Abstract
1. Introduction
2. Materials and Methods
2.1. Animal Experiment
2.1.1. Infection with Me49 Strain of T. gondii
2.1.2. Infection with Virulent RH Strain of T. gondii
2.2. Histopathological Examination
2.2.1. Hematoxylin and Eosin Staining
2.2.2. Immunohistochemistry
2.3. Statistical Analysis
3. Results
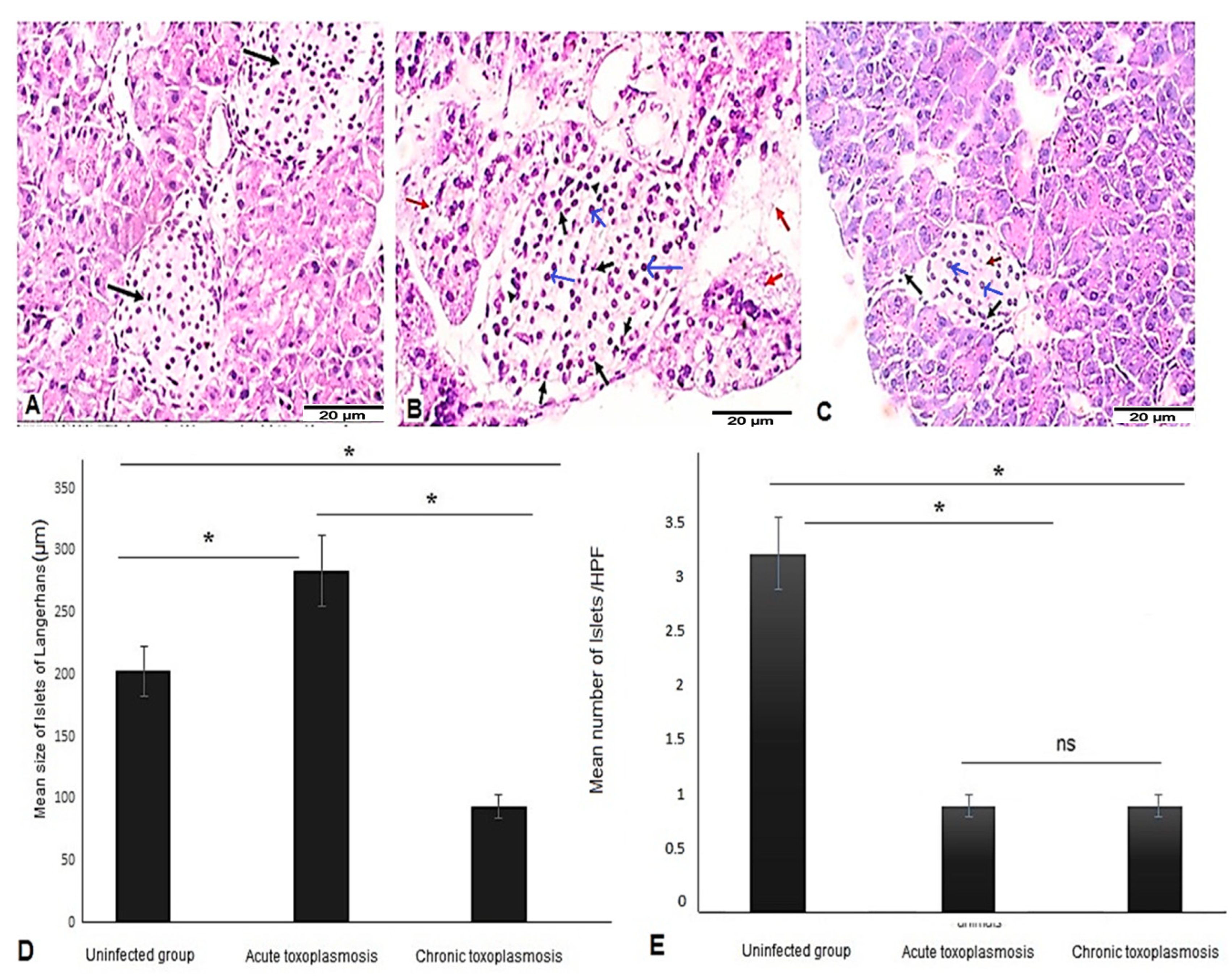
3.1. Pancreatic Tissues of Mice with Acute and Chronic Toxoplasmosis Demonstrated Marked Insulitis Characterized by Reduced Number and Abnormal Size of Islets of Langerhans
3.2. Islets of Langerhans of Mice with Chronic Toxoplasmosis Are Infiltrated with CD8+ T Cells
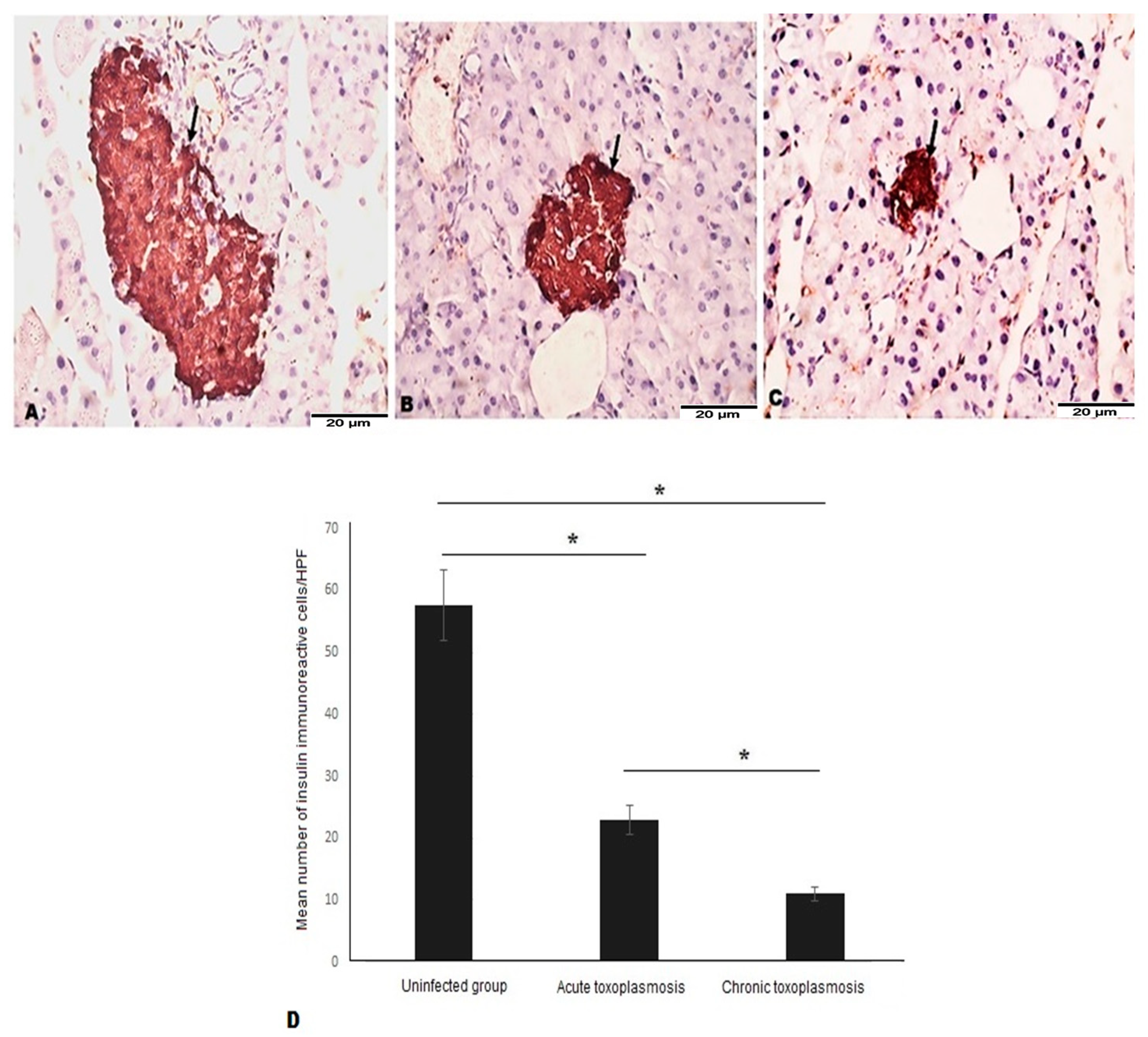
3.3. Acute and Chronic Toxoplasmosis Are Characterized by Lower Number of β Cells in Islets of Langerhans
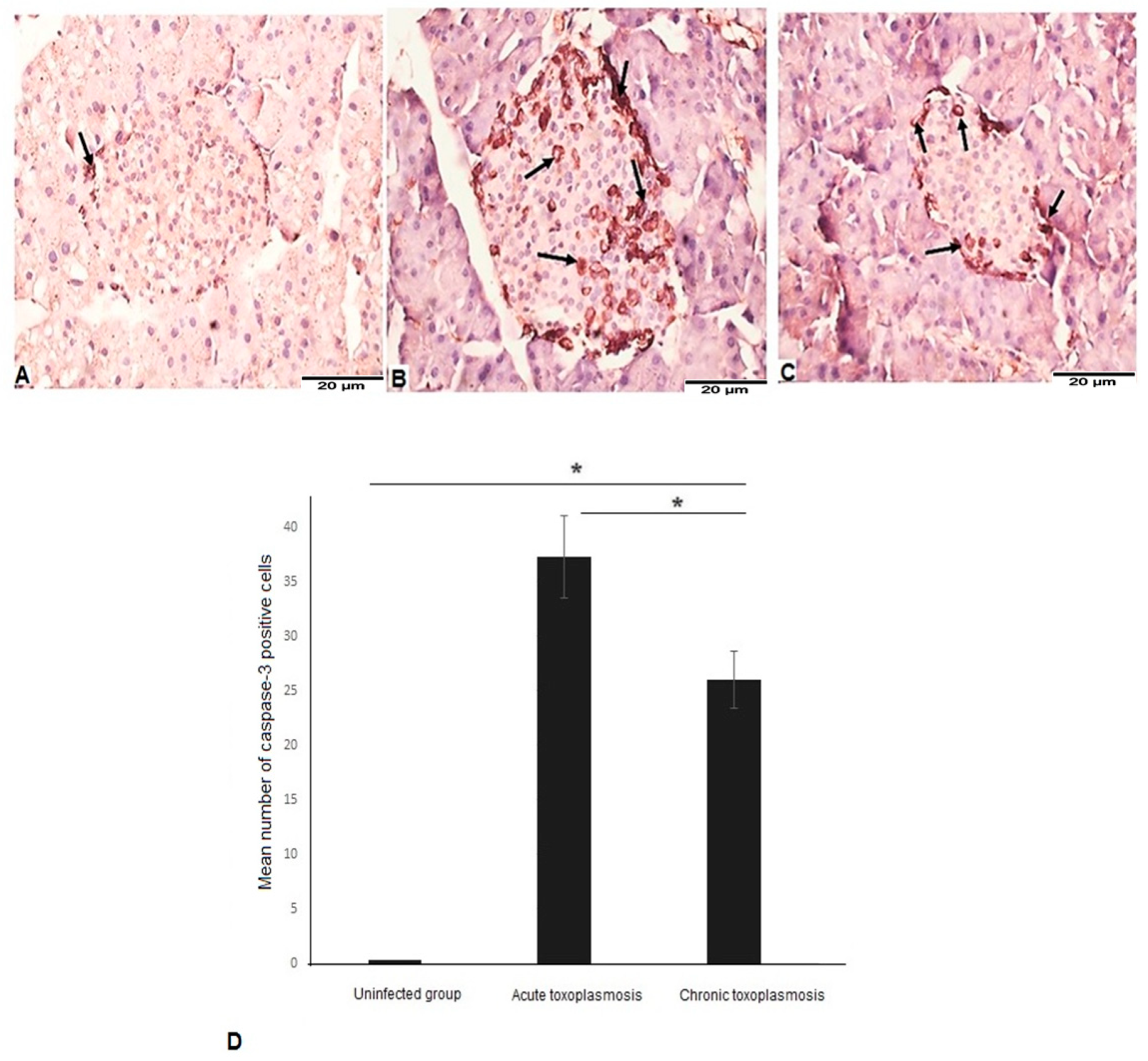
3.4. Acute and Chronic Toxoplasmosis Are Associated with Apoptotic Cell Death of Islets of Langerhans
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Webster, J.P.; Dubey, J.P. Toxoplasmosis of animals and humans. Parasites Vectors 2010, 3, 112. [Google Scholar] [CrossRef]
- Dubey, J.P. Advances in the life cycle of Toxoplasma gondii. Int. J. Parasitol. 1998, 28, 1019–1024. [Google Scholar] [CrossRef] [PubMed]
- Sutterland, A.L.; Fond, G.; Kuin, A.; Koeter, M.W.J.; Lutter, R.; van Gool, T.; Yolken, R.; Szoke, A.; Leboyer, M.; de Haan, L. Beyond the association. Toxoplasma gondii in schizophrenia, bipolar disorder, and addiction: Systematic review and meta-analysis. Acta Psychiatr. Scand. 2015, 132, 161–179. [Google Scholar] [CrossRef] [PubMed]
- Ahmadpour, E.; Daryani, A.; Sharif, M.; Sarvi, S.; Aarabi, M.; Mizani, A.; Rahimi, M.T.; Shokri, A. Toxoplasmosis in immunocompromised patients in Iran: A systematic review and meta-analysis. J. Infect. Dev. Ctries. 2014, 8, 1503–1510. [Google Scholar] [CrossRef] [PubMed]
- Galvan-Ramírez, M.D.L.L.; Troyo-Sanroman, R.; Roman, S.; Bernal-Redondo, R.; Castellanos, J.L.V. Prevalence of Toxoplasma infection in Mexican newborns and children: A systematic review from 1954 to 2009. ISRN Pediatr. 2012, 2012, 501216. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Foroutan-Rad, M.; Khademvatan, S.; Majidiani, H.; Aryamand, S.; Rahim, F.; Malehi, A.S. Seroprevalence of Toxoplasma gondii in the Iranian pregnant women: A systematic review and meta-analysis. Acta Trop. 2016, 158, 160–169. [Google Scholar] [CrossRef]
- Tenter, A.M.; Heckeroth, A.R.; Weiss, L.M. Toxoplasma gondii: From animals to humans. Int. J. Parasitol. 2000, 30, 1217–1258. [Google Scholar] [CrossRef]
- Munoz, M.; Liesenfeld, O.; Heimesaat, M.M. Immunology of Toxoplasma gondii. Immunol. Rev. 2011, 240, 269–285. [Google Scholar] [CrossRef]
- Carter, C.J. Toxoplasmosis and polygenic disease susceptibility genes: Extensive Toxoplasma gondii host/pathogen interactome enrichment in nine psychiatric or neurological disorders. J. Pathog. 2013, 2013, 965046. [Google Scholar] [CrossRef]
- Prandota, J. T. gondii infection acquired during pregnancy and/or after birth may be responsible for development of both type 1 and 2 diabetes mellitus. J. Diabetes Metab. 2013, 4, 55. [Google Scholar] [CrossRef]
- Adams, E.M.; Hafez, G.R.; Carnes, M.; Wiesner, J.K.; Graziano, F.M. The development of polymyositis in a patient with toxoplasmosis: Clinical and pathologic findings and review of literature. Clin. Exp. Rheumatol. 1984, 2, 205–208. [Google Scholar] [PubMed]
- Mousa, M.A.; Soliman, H.E.; el Shafie, M.S.; Abdel-Baky, M.S.; Aly, M.M. Toxoplasma seropositivity in patients with rheumatoid arthritis. J. Egypt. Soc. Parasitol. 1988, 18, 345–351. [Google Scholar] [PubMed]
- Balleari, E.; Cutolo, M.; Accardo, S. Adult-onset still’s disease associated to Toxoplasma gondii infection. Clin. Rheumatol. 1991, 10, 326–327. [Google Scholar] [CrossRef] [PubMed]
- Tomairek, H.A.; Saeid, M.S.; Morsy, T.A.; Michael, S.A. Toxoplasma gondii as a cause of rheumatoid arthritis. J. Egypt. Soc. Parasitol. 1982, 12, 17–23. [Google Scholar] [PubMed]
- Wasserman, E.E.; Nelson, K.; Rose, N.R.; Rhode, C.; Pillion, J.P.; Seaberg, E.; Talor, M.V.; Burek, L.; Eaton, W.; Duggan, A.; et al. Infection and thyroid autoimmunity: A seroepidemiologic study of TPOaAb. Autoimmunity 2009, 42, 439–446. [Google Scholar] [CrossRef]
- Tozzoli, R.; Barzilai, O.; Ram, M.; Villalta, D.; Bizzaro, N.; Sherer, Y.; Shoenfeld, Y. Infections and autoimmune thyroid diseases: Parallel detection of antibodies against pathogens with proteomic technology. Autoimmun. Rev. 2008, 8, 112–115. [Google Scholar] [CrossRef]
- Lidar, M.; Langevitz, P.; Barzilai, O.; Ram, M.; Porat-Katz, B.-S.; Bizzaro, N.; Tonutti, E.; Maieron, R.; Chowers, Y.; Bar-Meir, S.; et al. Infectious serologies and autoantibodies in inflammatory bowel disease: Insinuations at a true pathogenic role. Ann. N. Y. Acad. Sci. 2009, 1173, 640–648. [Google Scholar] [CrossRef]
- Zinger, H.; Sherer, Y.; Goddard, G.; Berkun, Y.; Barzilai, O.; Agmon-Levin, N.; Ram, M.; Blank, M.; Tincani, A.; Rozman, B.; et al. Common infectious agents prevalence in antiphospholipid syndrome. Lupus 2009, 18, 1149–1153. [Google Scholar] [CrossRef]
- Lidar, M.; Lipschitz, N.; Langevitz, P.; Barzilai, O.; Ram, M.; Porat-Katz, B.-S.; Pagnoux, C.; Guilpain, P.; Sinico, R.A.; Radice, A.; et al. Infectious serologies and autoantibodies in wegener’s granulomatosis and other vasculitides: Novel associations disclosed using the rad BioPlex 2200. Ann. N. Y. Acad. Sci. 2009, 1173, 649–657. [Google Scholar] [CrossRef]
- Sagi, L.; Baum, S.; Agmon-Levin, N.; Sherer, Y.; Katz, B.S.P.; Barzilai, O.; Ram, M.; Bizzaro, N.; SanMarco, M.; Trau, H.; et al. Autoimmune bullous diseases the spectrum of infectious agent antibodies and review of the literature. Autoimmun. Rev. 2011, 10, 527–535. [Google Scholar] [CrossRef]
- Liesenfeld, O. Oral infection of C57BL/6 mice with Toxoplasma gondii: A new model of inflammatory bowel disease? J. Infect. Dis. 2002, 185 (Suppl. S1), S96–S101. [Google Scholar] [CrossRef] [PubMed]
- Blank, M.; Asherson, R.A.; Cervera, R.; Shoenfeld, Y. Antiphospholipid syndrome infectious origin. J. Clin. Immunol. 2004, 24, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Aosai, F.; Norose, K.; Mun, H.-S.; Ishikura, H.; Hirose, S.; Piao, L.-X.; Fang, H.; Yano, A. Toxoplasma gondii infection inhibits the development of lupus-like syndrome in autoimmune (New Zealand black X New Zealand white) F1 mice. Int. Immunol. 2004, 16, 937–946. [Google Scholar] [CrossRef] [PubMed]
- Rittiphairoj, T.; Owais, M.; Ward, Z.J.; Reddy, C.L.; Yeh, J.M.; Atun, R. Incidence and prevalence of type 1 diabetes and diabetic ketoacidosis in children and adolescents (0–19 Years) in Thailand (2015–2020): A nationwide population-based study. Lancet Reg. Health-West. Pacific 2022, 21, 100392. [Google Scholar] [CrossRef]
- Mobasseri, M.; Shirmohammadi, M.; Amiri, T.; Vahed, N.; Hosseini Fard, H.; Ghojazadeh, M. Prevalence and incidence of type 1 diabetes in the world: A systematic review and meta-analysis. Health Promot. Perspect. 2020, 10, 98–115. [Google Scholar] [CrossRef]
- Tosur, M.; Geyer, S.M.; Rodriguez, H.; Libman, I.; Baidal, D.A.; Redondo, M.J. Ethnic Differences in Progression of Islet Autoimmunity and type 1 diabetes in relatives at risk. Diabetologia 2018, 61, 2043–2053. [Google Scholar] [CrossRef]
- Rodriguez-Calvo, T.; Ekwall, O.; Amirian, N.; Zapardiel-Gonzalo, J.; von Herrath, M.G. Increased immune cell infiltration of the exocrine pancreas: A possible contribution to the pathogenesis of type 1 diabetes. Diabetes 2014, 63, 3880–3890. [Google Scholar] [CrossRef]
- Steck, A.K.; Rewers, M.J. Genetics of type 1 diabetes. Clin. Chem. 2011, 57, 176–185. [Google Scholar] [CrossRef]
- Butalia, S.; Kaplan, G.G.; Khokhar, B.; Rabi, D.M. Environmental risk factors and type 1 diabetes: Past, present, and future. Can. J. Diabetes 2016, 40, 586–593. [Google Scholar] [CrossRef]
- Ismail, M.H.; Molan, A.-L. Study the possible association between toxoplasmosis and diabetes mellitus in Iraq. World J. Pharm. Pharm. Sci. 2017, 6, 85–96. [Google Scholar] [CrossRef]
- Shirbazou, S.; Delpisheh, A.; Mokhetari, R.; Tavakoli, G. Serologic detection of anti Toxoplasma gondii infection in diabetic patients. Iran. Red Crescent Med. J. 2013, 15, 701–703. [Google Scholar] [CrossRef] [PubMed]
- Shapira, Y.; Agmon-Levin, N.; Selmi, C.; Petríková, J.; Barzilai, O.; Ram, M.; Bizzaro, N.; Valentini, G.; Matucci-Cerinic, M.; Anaya, J.-M.; et al. Prevalence of anti-toxoplasma antibodies in patients with autoimmune diseases. J. Autoimmun. 2012, 39, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Saki, J.; Shafieenia, S.; Foroutan-Rad, M. Seroprevalence of toxoplasmosis in diabetic pregnant women in southwestern of Iran. J. Parasit. Dis. Off. Organ Indian Soc. Parasitol. 2016, 40, 1586–1589. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.-X.; Xin, H.; Zhang, X.-Y.; Wei, C.-Y.; Duan, Y.-H.; Wang, H.-F.; Niu, H.-T. Toxoplasma gondii infection in diabetes mellitus patients in China: Seroprevalence, risk factors, and case-control studies. Biomed. Res. Int. 2018, 2018, 4723739. [Google Scholar] [CrossRef]
- Kaňková, Š.; Flegr, J.; Calda, P. An elevated blood glucose level and increased incidence of gestational diabetes mellitus in pregnant women with latent toxoplasmosis. Folia Parasitol. 2015, 62, 1. [Google Scholar] [CrossRef]
- Beshay, E.V.N.; El-Refai, S.A.; Helwa, M.A.; Atia, A.F.; Dawoud, M.M. Toxoplasma gondii as a possible causative pathogen of type-1 diabetes mellitus: Evidence from case-control and experimental studies. Exp. Parasitol. 2018, 188, 93–101. [Google Scholar] [CrossRef]
- Majidiani, H.; Dalvand, S.; Daryani, A.; Galvan-Ramirez, M.D.L.L.; Foroutan-Rad, M. Is chronic toxoplasmosis a risk factor for diabetes mellitus? A systematic review and meta-analysis of case—Control studies. Braz. J. Infect. Dis. 2016, 20, 605–609. [Google Scholar] [CrossRef]
- Ridley, D.S.; Hawgood, B.C. The value of formol-ether concentration of faecal cysts and ova. J. Clin. Pathol. 1956, 9, 74. [Google Scholar] [CrossRef]
- Henriksen, S.A.; Pohlenz, J.F. Staining of cryptosporidia by a modified ziehl-neelsen technique. Acta Vet. Scand. 1981, 22, 594–596. [Google Scholar] [CrossRef]
- El-Sayed, N.M.; Aly, E.M. Toxoplasma gondii infection can induce retinal DNA damage: An experimental study. Int. J. Ophthalmol. 2014, 7, 431–436. [Google Scholar] [CrossRef]
- Djurković-Djaković, O.; Milenković, V.; Nikolić, A.; Bobić, B.; Grujić, J. Efficacy of atovaquone combined with clindamycin against murine infection with a cystogenic (Me49) strain of Toxoplasma gondii. J. Antimicrob. Chemother. 2002, 50, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Jafari, M.; Lorigooini, Z.; Kheiri, S.; Naeini, K.M. Anti-Toxoplasma effect of hydroalchohlic extract of terminalia chebula retz in cell culture and murine model. Iran. J. Parasitol. 2021, 16, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-da-Silva, M.D.F.; Rodrigues, R.M.; Andrade, E.F.D.; Carvalho, L.D.; Gross, U.; Lüder, C.G.K.; Barbosa, H.S. Spontaneous stage differentiation of mouse-virulent Toxoplasma gondii RH parasites in skeletal muscle cells: An ultrastructural evaluation. Mem. Inst. Oswaldo Cruz 2009, 104, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Asgari, Q.; Keshavarz, H.; Shojaee, S.; Motazedian, M.H.; Mohebali, M.; Miri, R.; Mehrabani, D.; Rezaeian, M. In vitro and in vivo potential of RH strain of Toxoplasma gondii (type I) in tissue cyst forming. Iran. J. Parasitol. 2013, 8, 367–375. [Google Scholar] [PubMed]
- Reddy, S.; Chai, R.C.C.; Rodrigues, J.A.; Hsu, T.-H.; Robinson, E. Presence of residual beta cells and co-existing islet autoimmunity in the NOD Mouse during longstanding diabetes: A combined histochemical and immunohistochemical study. J. Mol. Histol. 2008, 39, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Ilić, I.R.; Stojanović, N.M.; Radulović, N.S.; Živković, V.V.; Randjelović, P.J.; Petrović, A.S.; Božić, M.; Ilić, R.S. The quantitative ER immunohistochemical analysis in breast cancer: Detecting the 3 + 0, 4 + 0, and 5 + 0 allred score cases. Medicina 2019, 55, 461. [Google Scholar] [CrossRef] [PubMed]
- Saad, E.A.; Hassanien, M.M.; El-Hagrasy, M.A.; Radwan, K.H. Antidiabetic, hypolipidemic and antioxidant activities and protective effects of Punica Granatum peels powder against pancreatic and hepatic tissues injuries in streptozotocin induced Iddm in rats. Int. J. Pharm. Pharm. Sci. 2015, 7, 397–402. [Google Scholar]
- Molan, A.; Nosaka, K.; Hunter, M.; Wang, W. The role of Toxoplasma gondii as a possible inflammatory agent in the pathogenesis of type 2 diabetes mellitus in humans. Fam. Med. Community Health 2016, 4, 44–62. [Google Scholar] [CrossRef]
- Waree, P. Toxoplasmosis: Pathogenesis and immune response. Thammasat Med. J. 2008, 8, 487–496. [Google Scholar]
- Pugliese, A. Insulitis in the pathogenesis of type 1 diabetes. Pediatr. Diabetes 2016, 17 (Suppl. S2), 31–36. [Google Scholar] [CrossRef]
- In’t Veld, P. Insulitis in human type 1 diabetes: The quest for an elusive lesion. Islets 2011, 3, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Eizirik, D.L.; Colli, M.L.; Ortis, F. The role of inflammation in insulitis and β-cell loss in type 1 diabetes. Nat. Rev. Endocrinol. 2009, 5, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Campbell-Thompson, M.L.; Atkinson, M.A.; Butler, A.E.; Chapman, N.M.; Frisk, G.; Gianani, R.; Giepmans, B.N.; von Herrath, M.G.; Hyöty, H.; Kay, T.W.; et al. The diagnosis of insulitis in human type 1 diabetes. Diabetologia 2013, 56, 2541–2543. [Google Scholar] [CrossRef] [PubMed]
- Akinola, O.B.; Caxton-Martins, E.A.; Dini, L. Chronic treatment with ethanolic extract of the leavesof azadirachta indica ameliorates lesions of pancreatic islets in streptozotocin diabetes. Int. J. Morphol. 2010, 28, 291–302. [Google Scholar] [CrossRef]
- Seiron, P.; Wiberg, A.; Kuric, E.; Krogvold, L.; Jahnsen, F.L.; Dahl-Jørgensen, K.; Skog, O.; Korsgren, O. Characterisation of the endocrine pancreas in type 1 diabetes: Islet size is maintained but islet number is markedly reduced. J. Pathol. Clin. Res. 2019, 5, 248–255. [Google Scholar] [CrossRef]
- Kou, K.; Saisho, Y.; Sato, S.; Yamada, T.; Itoh, H. Islet number rather than islet size is a major determinant of β- and α-cell mass in humans. J. Clin. Endocrinol. Metab. 2014, 99, 1733–1740. [Google Scholar] [CrossRef]
- Saha, D.; Ghosh, S.K.; Das, T.; Mishra, S.B. Hypoglycemic and antihyperlipidemic effects of Adiantum Caudatum in alloxan induced diabetes in rats. Asian J. Pharm. Clin. Res. 2016, 9, 339–341. [Google Scholar]
- Balamash, K.S.; Alkreathy, H.M.; Al Gahdali, E.H.; Khoja, S.O.; Ahmad, A. Comparative biochemical and histopathological studies on the efficacy of metformin and virgin olive oil against streptozotocin-induced diabetes in sprague-dawley rats. J. Diabetes Res. 2018, 2018, 4692197. [Google Scholar] [CrossRef]
- Abdul-Hamid, M.; Moustafa, N. Protective effect of curcumin on histopathology and ultrastructure of pancreas in the alloxan treated rats for induction of diabetes. J. Basic Appl. Zool. 2013, 66, 169–179. [Google Scholar] [CrossRef]
- El-Desouki, N.I.; Tabl, G.A.; Abdel-Aziz, K.K.; Salim, E.I.; Nazeeh, N. Improvement in beta-islets of langerhans in alloxan-induced diabetic rats by erythropoietin and spirulina. J. Basic Appl. Zool. 2015, 71, 20–31. [Google Scholar] [CrossRef]
- Liadis, N.; Murakami, K.; Eweida, M.; Elford, A.R.; Sheu, L.; Gaisano, H.Y.; Hakem, R.; Ohashi, P.S.; Woo, M. Caspase-3-dependent beta-cell apoptosis in the initiation of autoimmune diabetes mellitus. Mol. Cell. Biol. 2005, 25, 3620–3629. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, S.; Karimian, S.M.; Sotoudeh, M.; Bahadori, M.; Dehghani, G.A. Pancreatic islet beta cell protective effect of oral vanadyl sulphate in streptozotocin-induced diabetic rats, an ultrastructure study. Pakistan J. Biol. Sci. PJBS 2010, 13, 1135–1140. [Google Scholar] [CrossRef] [PubMed]
- Ajzenberg, D. Type I strains in human toxoplasmosis: Myth or reality? Future Microbiol. 2010, 5, 841–843. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Su, C.; German, M.; Storch, G.A.; Clifford, D.B.; Sibley, L.D. Genotyping of Toxoplasma gondii strains from immunocompromised patients reveals high prevalence of type I strains. J. Clin. Microbiol. 2005, 43, 5881–5887. [Google Scholar] [CrossRef] [PubMed]
- Negrato, C.A.; Lauris, J.R.P.; Saggioro, I.B.; Corradini, M.C.M.; Borges, P.R.; Crês, M.C.; Junior, A.L.; Guedes, M.F.S.; Gomes, M.B. Increasing incidence of type 1 diabetes between 1986 and 2015 in Bauru, Brazil. Diabetes Res. Clin. Pract. 2017, 127, 198–204. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-kady, A.M.; Alzahrani, A.M.; Elshazly, H.; Alshehri, E.A.; Wakid, M.H.; Gattan, H.S.; Al-Megrin, W.A.I.; Alfaifi, M.S.; Mohamed, K.; Alharbi, W.; et al. Pancreatic Pathological Changes in Murine Toxoplasmosis and Possible Association with Diabetes Mellitus. Biomedicines 2023, 11, 18. https://doi.org/10.3390/biomedicines11010018
El-kady AM, Alzahrani AM, Elshazly H, Alshehri EA, Wakid MH, Gattan HS, Al-Megrin WAI, Alfaifi MS, Mohamed K, Alharbi W, et al. Pancreatic Pathological Changes in Murine Toxoplasmosis and Possible Association with Diabetes Mellitus. Biomedicines. 2023; 11(1):18. https://doi.org/10.3390/biomedicines11010018
Chicago/Turabian StyleEl-kady, Asmaa M., Amal M. Alzahrani, Hayam Elshazly, Eman Abdullah Alshehri, Majed H. Wakid, Hattan S. Gattan, Wafa Abdullah I. Al-Megrin, Mashael S. Alfaifi, Khalil Mohamed, Waheeb Alharbi, and et al. 2023. "Pancreatic Pathological Changes in Murine Toxoplasmosis and Possible Association with Diabetes Mellitus" Biomedicines 11, no. 1: 18. https://doi.org/10.3390/biomedicines11010018
APA StyleEl-kady, A. M., Alzahrani, A. M., Elshazly, H., Alshehri, E. A., Wakid, M. H., Gattan, H. S., Al-Megrin, W. A. I., Alfaifi, M. S., Mohamed, K., Alharbi, W., Elshabrawy, H. A., & Younis, S. S. (2023). Pancreatic Pathological Changes in Murine Toxoplasmosis and Possible Association with Diabetes Mellitus. Biomedicines, 11(1), 18. https://doi.org/10.3390/biomedicines11010018








