Investigational Treatments in Phase I and II Clinical Trials: A Systematic Review in Asthma
Abstract
1. Introduction
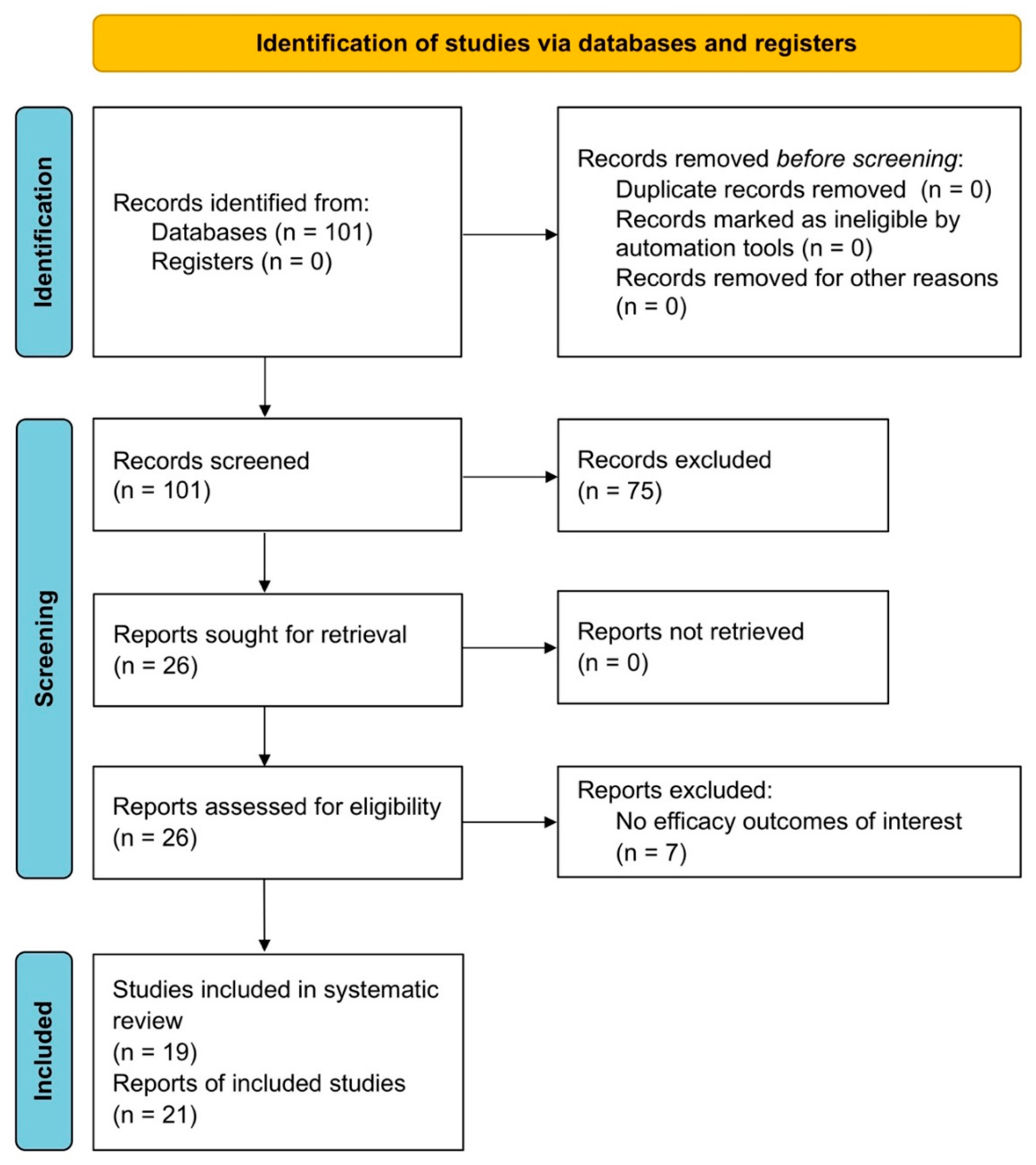
2. Materials and Methods
2.1. Review Question
2.2. Search Strategy
2.3. Study Selection
2.4. Data Extraction
2.5. Endpoints
2.6. Strategy for Data Synthesis
2.7. Quality Score
3. Results
3.1. Study Characteristics
3.2. IL-4Rα Inhibitor
3.3. Anti-IL-5 mAbs
3.4. Anti-IL-17A mAbs
3.5. Anti-IL-33 mAbs
3.6. Anti-TSLP mAbs
3.7. LABAs
3.8. SGRMs
3.9. MABAs
3.10. DP2 Antagonists
3.11. Selective BTK Inhibitors
3.12. ENaC Inhibitors
3.13. Pan-JAK Inhibitors
3.14. Anti-Fel d 1 mAbs
3.15. Synthetic Amino-Benzothiazoles
3.16. Antifungal Triazoles
3.17. Probiotics
3.18. Risk of Bias
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GINA Main Report—Global Initiative for Asthma, 2021 (n.d.). Available online: https://ginasthma.org/wp-content/uploads/2021/05/GINA-Main-Report-2021-V2-WMS.pdf (accessed on 11 June 2021).
- Singh, D.; Garcia, G.; Maneechotesuwan, K.; Daley-Yates, P.; Irusen, E.; Aggarwal, B.; Boucot, I.; Berend, N. New Versus Old: The Impact of Changing Patterns of Inhaled Corticosteroid Prescribing and Dosing Regimens in Asthma Management. Adv. Ther. 2022, 39, 1895–1914. [Google Scholar] [CrossRef] [PubMed]
- Ray, A.; Singh, S.; Dutta, J.; Mabalirajan, U. Targeting molecular and cellular mechanisms in asthma. In Targeting Cellular Signalling Pathways in Lung Diseases; Springer: Singapore, 2021; pp. 27–51. [Google Scholar]
- Hekking, P.P.W.; Wener, R.R.; Amelink, M.; Zwinderman, A.H.; Bouvy, M.L.; Bel, E.H. The prevalence of severe refractory asthma. J. Allergy Clin. Immunol. 2015, 135, 896–902. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.F.; Wenzel, S.E.; Brozek, J.L.; Bush, A.; Castro, M.; Sterk, P.J.; Adcock, I.M.; Bateman, E.D.; Bel, E.H.; Bleecker, E.R.; et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur. Respir. J. 2014, 43, 343–373. [Google Scholar] [CrossRef] [PubMed]
- Kuruvilla, M.E.; Lee, F.E.H.; Lee, G.B. Understanding Asthma Phenotypes, Endotypes, and Mechanisms of Disease. Clin. Rev. Allergy Immunol. 2018, 56, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Sterk, P.J. Chronic diseases like asthma and COPD: Do they truly exist? Eur. Respir. J. 2016, 47, 359–361. [Google Scholar] [CrossRef]
- Wenzel, S.E. Asthma phenotypes: The evolution from clinical to molecular approaches. Nat. Med. 2012, 18, 716–725. [Google Scholar] [CrossRef]
- Pelaia, C.; Calabrese, C.; Terracciano, R.; de Blasio, F.; Vatrella, A.; Pelaia, G. Omalizumab, the first available antibody for biological treatment of severe asthma: More than a decade of real-life effectiveness. Ther. Adv. Respir. Dis. 2018, 12, 1753466618810192. [Google Scholar] [CrossRef]
- Menzies-Gow, A.; Szefler, S.J.; Busse, W.W. The Relationship of Asthma Biologics to Remission for Asthma. J. Allergy Clin. Immunol. Pract. 2020, 9, 1090–1098. [Google Scholar] [CrossRef]
- Moran, A.; Pavord, I.D. Anti-IL-4/IL-13 for the treatment of asthma: The story so far. Expert Opin. Biol. Ther. 2020, 20, 283–294. [Google Scholar] [CrossRef]
- Hoy, S.M. Tezepelumab: First Approval. Drugs. 2022, 82, 461–468. [Google Scholar] [CrossRef]
- Cazzola, M.; Ora, J.; Cavalli, F.; Rogliani, P.; Matera, M.G. Treatable Mechanisms in Asthma. Mol. Diagn. Ther. 2021, 25, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Cazzola, M.; Rogliani, P.; Naviglio, S.; Calzetta, L.; Matera, M.G. An update on the currently available and emerging synthetic pharmacotherapy for uncontrolled asthma. Expert Opin. Pharmacother. 2022, 23, 1205–1216. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Prisma-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021, 372, n71. [Google Scholar] [CrossRef]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inf. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Savović, J.; Page, M.J.; Elbers, R.G.; Sterne, J.A.C. Chapter 8: Assessing Risk of bias in a randomized trial. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2019); John Wiley & Sons: Chichester, UK, 2019; pp. 205–228. Available online: https://training.cochrane.org/handbook (accessed on 1 June 2022).
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, L.A. robvis: An R package and web application for visualising risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- NCT03299686; Study to Assess the Efficacy and Safety of CJM112 in Patients with Inadequately Controlled Severe Asthma. 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT03299686 (accessed on 1 June 2022).
- NCT03393806; Repeat Dose Study of GSK3772847 in Participants with Moderate to Severe Asthma with Allergic Fungal Airway Disease (AFAD). 2018. Available online: https://clinicaltrials.gov/ct2/show/NCT03393806 (accessed on 1 June 2022).
- NCT03207243; Efficacy and Safety Study of GSK3772847 in Subjects with Moderately Severe Asthma. 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT03207243 (accessed on 1 June 2022).
- NCT03944707; Study of Efficacy and Safety of LOU064 in Inadequately Controlled Asthma Patients. 2019. Available online: https://www.clinicaltrials.gov/ct2/show/NCT03944707 (accessed on 1 June 2022).
- NCT03135899; BI 443651 Methacholine Challenge. 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT03135899 (accessed on 1 June 2022).
- NCT04150341; Effect of Inhaled TD-8236 on Allergen-induced Asthmatic Response. 2019. Available online: https://clinicaltrials.gov/ct2/show/NCT04150341 (accessed on 1 June 2022).
- Siddiqui, S.; Bozik, M.; Archibald, D.; Dworetzky, S.; Mather, J.; Killingsworth, R.; Ochkur, S.; Jacobsen, E.; Panettieri, R.; Prussin, C. Late Breaking Abstract—Phase 2 trial evaluating the effects of dexpramipexole on blood eosinophils, lung function, and airway biomarkers in eosinophilic asthma. Eur. Respir. J. 2021, 58, RCT2900. [Google Scholar] [CrossRef]
- NCT04046939; Dexpramipexole Dose-Ranging Biomarker Study in Subjects with Eosinophilic Asthma (AS201). 2019. Available online: https://clinicaltrials.gov/ct2/show/NCT04046939 (accessed on 1 June 2022).
- Singh, D.; Fuhr, R.; Bird, N.P.; Mole, S.; Hardes, K.; Man, Y.L.; Cahn, A.; Yancey, S.W.; Pouliquen, I.J. A Phase 1 study of the long-acting anti-IL-5 monoclonal antibody GSK3511294 in patients with asthma. Br. J. Clin. Pharmacol. 2022, 88, 702–712. [Google Scholar] [CrossRef]
- NCT03287310; First Time in Human (FTIH) Study to Evaluate Safety, Tolerability, Immunogenicity, Pharmacokinetics (PK) and Pharmacodynamics (PD) of GSK3511294 Administered Subcutaneously (SC) in Subjects with Mild to Moderate Asthma. 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT03287310 (accessed on 1 June 2022).
- Wechsler, M.E.; Ruddy, M.K.; Pavord, I.D.; Israel, E.; Rabe, K.F.; Ford, L.B.; Maspero, J.F.; Abdulai, R.M.; Hu, C.-C.; Martincova, R.; et al. Efficacy and Safety of Itepekimab in Patients with Moderate-to-Severe Asthma. N. Engl. J. Med. 2021, 385, 1656–1668. [Google Scholar] [CrossRef] [PubMed]
- NCT03387852; Evaluation of SAR440340 and as Combination Therapy with Dupilumab in Moderate-to-Severe Asthma Participants. 2018. Available online: https://clinicaltrials.gov/ct2/show/NCT03387852 (accessed on 1 June 2022).
- Miller, D.; Vaidya, S.; Jauernig, J.; Ethell, B.; Wagner, K.; Radhakrishnan, R.; Tillmann, H.C. Lung function, pharmacokinetics, and tolerability of inhaled indacaterol maleate and acetate in asthma patients. Respir. Res. 2020, 21, 120. [Google Scholar] [CrossRef] [PubMed]
- NCT03257996; Pharmacodynamics, Safety, Tolerability, and Pharmacokinetics of Two Orally Inhaled Indacaterol Salts in Adult Subjects with Asthma. 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT03257995 (accessed on 1 June 2022).
- Moss, M.H.; Lugogo, N.L.; Castro, M.; Hanania, N.A.; Ludwig-Sengpiel, A.; Saralaya, D.; Dobek, R.; Ojanguren, I.; Vyshnyvetskyy, I.; Bruey, J.-M.; et al. Results of a Phase 2b Trial with GB001, a Prostaglandin D2 Receptor 2 Antagonist, in Moderate to Severe Eosinophilic Asthma. Chest 2022, 162, 297–308. [Google Scholar] [CrossRef] [PubMed]
- NCT03683576; GB001 in Adult Subjects with Moderate to Severe Asthma. 2018. Available online: https://clinicaltrials.gov/ct2/show/NCT03683576 (accessed on 1 June 2022).
- Cass, L.; Murray, A.; Davis, A.; Woodward, K.; Albayaty, M.; Ito, K.; Strong, P.; Ayrton, J.; Brindley, C.; Prosser, J.; et al. Safety and nonclinical and clinical pharmacokinetics of PC945, a novel inhaled triazole antifungal agent. Pharmacol. Res. Perspect. 2021, 9, e00690. [Google Scholar] [CrossRef] [PubMed]
- NCT02715570; A Study to Investigate the Safety, Tolerability and Pharmacokinetics of Single and Repeat Doses of PC945. 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT02715570 (accessed on 3 June 2022).
- NCT03469934; Proof of Concept Study to Investigate ANB020 Activity in Adult Patients with Severe Eosinophilic Asthma. 2018. Available online: https://clinicaltrials.gov/ct2/show/NCT03469934 (accessed on 3 June 2022).
- EudraCT Number 2017-000647-40; Placebo-Controlled Proof of Concept Study to Investigate ANB020 Activity in Adult Patients with Severe Eosinophilic Asthma. 2018. Available online: https://www.clinicaltrialsregister.eu/ctr-search/trial/2017-000647-40/results (accessed on 3 June 2022).
- NCT03378648; A Study to Investigate Safety, Tolerability, Pharmacokinetics and Pharmacodynamics of Single Dose in Healthy Volunteers, Repeat Doses in Asthmatic Patients and of Single Dose in COPD Patients of CHF6366. 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT03378648 (accessed on 6 June 2022).
- EudraCT Number 2015-005551-27; A FIRST in Human Randomised, Double-Blind, Placebo-Controlled Study of Single Ascending Doses in Healthy Male Volunteers and Repeated Ascending Dose in Asthmatic Patients Followed by a 3-Way Cross-Over, Placebo-Controlled, Single-Dose in COPD Patients to Investigate the Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics of CHF6366. 2019. Available online: https://www.clinicaltrialsregister.eu/ctr-search/trial/2015-005551-27/results (accessed on 6 June 2022).
- Moermans, C.; Graff, S.; Medard, L.; Schleich, F.; Paulus, V.; Guissard, F.; Henket, M.; Louis, R. Clinical trial: Impact of Probiotical® on asthma control and inflammation. Eur. Respir. J. 2020, 56, 5281. [Google Scholar] [CrossRef]
- NCT03341403; Effect of a Synbiotic “Probiotical®” in Asthma. 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT03341403 (accessed on 6 June 2022).
- Bruns, I.; Fitzgerald, M.; Mensing, G.; Tsung, M.; Pardali, K.; Gardiner, P.; Keeling, D.; Axelsson, L.; Olsson, M.; Ghobadi, C.; et al. Late Breaking Abstract—Multiple ascending dose study of the inhaled IL-4Ra antagonist, AZD1402/PRS-060, in mild asthmatics demonstrates robust FeNO reduction and a promising clinical profile for the treatment of asthma. Eur. Respir. J. 2019, 54, PA3709. [Google Scholar] [CrossRef]
- NCT03574805; Study of Multiple Doses of PRS-060 Administered by Oral Inhalation in Subjects with Mild Asthma. 2018. Available online: https://clinicaltrials.gov/ct2/show/NCT03574805 (accessed on 6 June 2022).
- Chupp, G.L.; Beeh, K.M.; Jauhiainen, A.; Necander, S.; Brown, M.N.; Hamrén, U.W.; Forsman, H.; Kurdyukova, Y.; Steele, J.; Astbury, C.; et al. Results of a Phase 2b Dose Finding Study of Velsecorat, an Inhaled Non-Steroidal, Selective Glucocorticoid Receptor Modulator in Asthma (GRANIT). Am. Thorac. Soc. Int. Conf. Meet. Abstr. 2021, 203, A1202. [Google Scholar] [CrossRef]
- NCT03622112; A Study to Assess the Efficacy and Safety of Multiple Dose Levels of AZD7594 Administered Once Daily by Inhalation in Asthmatic Subjects. 2018. Available online: https://clinicaltrials.gov/ct2/show/NCT03622112 (accessed on 6 June 2022).
- EudraCT Number 2017-002483-40; A Phase 2b Randomised, Double-Blind, Placebo-Controlled, Parallel Arm, Multi-Centre Study to Assess Efficacy and Safety of Multiple Dose Levels of AZD7594 DPI Given Once Daily for Twelve Weeks, Compared to Placebo, in Asthmatics Symptomatic on Low Dose ICS. 2020. Available online: https://www.clinicaltrialsregister.eu/ctr-search/trial/2017-002483-40/results (accessed on 6 June 2022).
- De Gaix, F.D.B.; Gherasim, A.; Domis, N.; Meier, P.; Shawki, F.; DeVeaux, M.; Ramesh, D.; Perlee, L.; Herman, G.; Weinreich, D.; et al. A Single-Dose of REGN1908-1909 Reduced Bronchoconstriction in Cat-Allergic Subjects with Mild Asthma for up to 3 months following a controlled cat allergen challenge: A Phase 2, Randomized, Double-Blind, Placebo-Controlled Study. J. Allergy Clin. Immunol. 2021, 147, AB158. [Google Scholar] [CrossRef]
- NCT03838731; Study in Cat-Allergic Patients with Asthma to Evaluate the Efficacy of a Single Dose of REGN1908-1909 to Reduce Bronchoconstriction Upon Cat Allergen Challenge. 2019. Available online: https://clinicaltrials.gov/ct2/show/NCT03838731 (accessed on 6 June 2022).
- NCT03138811; A Bronchoprovocation Study to Assess the Safety, Tolerability, Pharmacokinetics and Pharmacodynamics of CSJ117 in Adult Subjects with Mild Atopic Asthma. 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT03138811 (accessed on 6 June 2022).
- Novartis Pharmaceuticals. A randomized, subject and investigator-blinded, placebo-controlled, parallel-design, broncho-provocation study to evaluate the safety, tolerability, pharmacokinetics and pharmacodynamics of multiple doses of inhaled CSJ117 in adult subjects with mild atopic asthma. 2020. Available online: https://www.novctrd.com/ctrdweb/trialresult/trialresults/pdf?trialResultId=17681 (accessed on 6 June 2022).
- Vatrella, A.; Fabozzi, I.; Calabrese, C.; Maselli, R.; Pelaia, G. Dupilumab: A novel treatment for asthma. J. Asthma Allergy 2014, 7, 123–130. [Google Scholar] [CrossRef]
- Gour, N.; Wills-Karp, M. IL-4 and IL-13 signaling in allergic airway disease. Cytokine 2015, 75, 68–78. [Google Scholar] [CrossRef]
- Legrand, F.; Klion, A.D. Biologic Therapies Targeting Eosinophils: Current Status and Future Prospects. J. Allergy Clin. Immunol. Pract. 2015, 3, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Molet, S.; Hamid, Q.; Davoine, F.; Nutku, E.; Taha, R.; Pagé, N.; Olivenstein, R.; Elias, J.; Chakir, J. IL-17 is increased in asthmatic airways and induces human bronchial fibroblasts to produce cytokines. J. Allergy Clin. Immunol. 2001, 108, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Chakir, J.; Shannon, J.; Molet, S.; Fukakusa, M.; Elias, J.; Laviolette, M.; Boulet, L.P.; Hamid, Q. Airway remodeling-associated mediators in moderate to severe asthma: Effect of steroids on TGF-β, IL-11, IL-17, and type I and type III collagen expression. J. Allergy Clin. Immunol. 2003, 111, 1293–1298. [Google Scholar] [CrossRef] [PubMed]
- Bullens, D.M.A.; Truyen, E.; Coteur, L.; Dilissen, E.; Hellings, P.W.; Dupont, L.J.; Ceuppens, J.L. IL-17 mRNA in sputum of asthmatic patients: Linking T cell driven inflammation and granulocytic influx? Respir. Res. 2006, 7, 135. [Google Scholar] [CrossRef]
- Zheng, R.; Wang, F.; Huang, Y.; Xiang, Q.; Dai, H.; Zhang, W. Elevated Th17 cell frequencies and Th17/Treg ratio are associated with airway hyperresponsiveness in asthmatic children. J. Asthma 2020, 58, 707–716. [Google Scholar] [CrossRef]
- Doe, C.; Bafadhel, M.; Siddiqui, S.; Desai, D.; Mistry, V.; Rugman, P.; McCormick, M.; Woods, J.; May, R.; Sleeman, M.A.; et al. Expression of the T helper 17-associated cytokines IL-17A and IL-17F in asthma and COPD. Chest 2010, 138, 1140–1147. [Google Scholar] [CrossRef]
- Agache, I.; Ciobanu, C.; Agache, C.; Anghel, M. Increased serum IL-17 is an independent risk factor for severe asthma. Respir. Med. 2010, 104, 1131–1137. [Google Scholar] [CrossRef]
- Al-Ramli, W.; Préfontaine, D.; Chouiali, F.; Martin, J.G.; Olivenstein, R.; Lemière, C.; Hamid, Q. TH17-associated cytokines (IL-17A and IL-17F) in severe asthma. J. Allergy Clin. Immunol. 2009, 123, 1185–1187. [Google Scholar] [CrossRef]
- Chesné, J.; Braza, F.; Mahay, G.; Brouard, S.; Aronica, M.; Magnan, A. IL-17 in severe asthma: Where do we stand? Am. J. Respir. Crit. Care Med. 2014, 190, 1094–1101. [Google Scholar] [CrossRef]
- Chambers, E.S.; Nanzer, A.M.; Pfeffer, P.E.; Richards, D.F.; Timms, P.M.; Martineau, A.R.; Griffiths, C.J.; Corrigan, C.J.; Hawrylowicz, C.M. Distinct endotypes of steroid-resistant asthma characterized by IL-17Ahigh and IFN-γhigh immunophenotypes: Potential benefits of calcitriol. J. Allergy Clin. Immunol. 2015, 136, 628–637.e4. [Google Scholar] [CrossRef]
- Rahmawati, S.F.; Velde, M.t.; Kerstjens, H.A.M.; Dömling, A.S.S.; Groves, M.R.; Gosens, R. Pharmacological Rationale for Targeting IL-17 in Asthma. Front. Allergy 2021, 2, 694514. [Google Scholar] [CrossRef]
- Mitchell, P.D.; O’Byrne, P.M. Epithelial-Derived Cytokines in Asthma. Chest 2017, 151, 1338–1344. [Google Scholar] [CrossRef]
- Smith, S.G.; Chen, R.; Kjarsgaard, M.; Huang, C.; Oliveria, J.P.; O’Byrne, P.M.; Gauvreau, G.M.; Boulet, L.P.; Lemiere, C.; Martin, J.; et al. Increased numbers of activated group 2 innate lymphoid cells in the airways of patients with severe asthma and persistent airway eosinophilia. J. Allergy Clin. Immunol. 2016, 137, 75–86.e8. [Google Scholar] [CrossRef]
- Bartemes, K.R.; Iijima, K.; Kobayashi, T.; Kephart, G.M.; McKenzie, A.N.; Kita, H. IL-33-responsive lineage-CD25+ CD44(hi) lymphoid cells mediate innate type 2 immunity and allergic inflammation in the lungs. J. Immunol. 2012, 188, 1503–1513. [Google Scholar] [CrossRef] [PubMed]
- Kabata, H.; Flamar, A.L.; Mahlakõiv, T.; Moriyama, S.; Rodewald, H.R.; Ziegler, S.F.; Artis, D. Targeted deletion of the TSLP receptor reveals cellular mechanisms that promote type 2 airway inflammation. Mucosal Immunol. 2020, 13, 626–636. [Google Scholar] [CrossRef] [PubMed]
- Ying, S.; O’Connor, B.; Ratoff, J.; Meng, Q.; Mallett, K.; Cousins, D.; Robinson, D.; Zhang, G.; Zhao, J.; Lee, T.H.; et al. Thymic Stromal Lymphopoietin Expression Is Increased in Asthmatic Airways and Correlates with Expression of Th2-Attracting Chemokines and Disease Severity. J. Immunol. 2005, 174, 8183–8190. [Google Scholar] [CrossRef] [PubMed]
- Shikotra, A.; Choy, D.F.; Ohri, C.M.; Doran, E.; Butler, C.; Hargadon, B.; Shelley, M.; Abbas, A.R.; Austin, C.D.; Jackman, J.; et al. Increased expression of immunoreactive thymic stromal lymphopoietin in patients with severe asthma. J. Allergy Clin. Immunol. 2012, 129, 104–111.e9. [Google Scholar] [CrossRef]
- Park, S.; Park, Y.; Son, S.H.; Lee, K.; Jung, Y.W.; Lee, K.Y.; Jeon, Y.H.; Byun, Y. Synthesis and biological evaluation of peptide-derived TSLP inhibitors. Bioorg. Med. Chem. Lett. 2017, 27, 4710–4713. [Google Scholar] [CrossRef]
- Chuchalin, A.G.; Tsoi, A.N.; Richter, K.; Krug, N.; Dahl, R.; Luursema, P.B.; Cameron, R.; Bao, W.; Higgins, M.; Woessner, R.; et al. Safety and tolerability of indacaterol in asthma: A randomized, placebo-controlled 28-day study. Respir. Med. 2007, 101, 2065–2075. [Google Scholar] [CrossRef]
- Beasley, R.W.; Donohue, J.F.; Mehta, R.; Nelson, H.S.; Clay, M.; Moton, A.; Kim, H.J.; Hederer, B.M. Effect of once-daily indacaterol maleate/mometasone furoate on exacerbation risk in adolescent and adult asthma: A double-blind randomised controlled trial. BMJ Open 2015, 5, e006131. [Google Scholar] [CrossRef]
- Kanniess, F.; Boulet, L.P.; Pierzchala, W.; Cameron, R.; Owen, R.; Higgins, M. Efficacy and safety of indacaterol, a new 24-hour β2-agonist, in patients with asthma: A dose-ranging study. J. Asthma 2008, 45, 887–892. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.H.; Martinot, J.B.; Pohunek, P.; Beier, J.; Magula, D.; Cameron, R.; Owen, R.; Higgins, M. Tolerability of indacaterol, a novel once-daily beta2-agonist, in patients with asthma: A randomized, placebo-controlled, 28-day safety study. Ann. Allergy Asthma Immunol. 2007, 99, 555–561. [Google Scholar] [CrossRef]
- Sedwick, C. Wanted: A New Model for Glucocorticoid Receptor Transactivation and Transrepression. PLoS Biol. 2014, 12, e1001814. [Google Scholar] [CrossRef] [PubMed]
- Van Moortel, L.; Gevaert, K.; de Bosscher, K. Improved Glucocorticoid Receptor Ligands: Fantastic Beasts, but How to Find Them? Front. Endocrinol. 2020, 11, 712. [Google Scholar] [CrossRef]
- Cazzola, M.; Lopez-Campos, J.L.; Puente-Maestu, L. The MABA approach: A new option to improve bronchodilator therapy. Eur. Respir. J. 2013, 42, 885–887. [Google Scholar] [CrossRef]
- de Miguel-Díez, J.; Jiménez-García, R. Considerations for new dual-acting bronchodilator treatments for chronic obstructive pulmonary disease. Expert Opin. Investig. Drugs 2014, 23, 453–456. [Google Scholar] [CrossRef]
- Domingo, C.; Palomares, O.; Sandham, D.A.; Erpenbeck, V.J.; Altman, P. The prostaglandin D2 receptor 2 pathway in asthma: A key player in airway inflammation 11 Medical and Health Sciences 1107 Immunology 11 Medical and Health Sciences 1102 Cardiorespiratory Medicine and Haematology. Respir. Res. 2018, 19, 189. [Google Scholar] [CrossRef]
- Hata, D.; Kawakami, Y.; Inagaki, N.; Lantz, C.S.; Kitamura, T.; Khan, W.N.; Maeda-Yamamoto, M.; Miura, T.; Han, W.; Hartman, S.E.; et al. Involvement of Bruton’s tyrosine kinase in FcepsilonRI-dependent mast cell degranulation and cytokine production. J. Exp. Med. 1998, 187, 1235–1247. [Google Scholar] [CrossRef]
- Iyer, A.S.; Morales, J.L.; Huang, W.; Ojo, F.; Ning, G.; Wills, E.; Baines, J.D.; August, A. Absence of Tec family kinases interleukin-2 inducible T cell kinase (Itk) and Bruton’s tyrosine kinase (Btk) severely impairs Fc epsilonRI-dependent mast cell responses. J. Biol. Chem. 2011, 286, 9503–9513. [Google Scholar] [CrossRef]
- MacGlashan, D.; Honigberg, L.A.; Smith, A.; Buggy, J.; Schroeder, J.T. Inhibition of IgE-mediated secretion from human basophils with a highly selective Bruton’s tyrosine kinase, Btk, inhibitor. Int. Immunopharmacol. 2011, 11, 475–479. [Google Scholar] [CrossRef]
- Phillips, J.E.; Renteria, L.; Burns, L.; Harris, P.; Peng, R.; Bauer, C.M.T.; Laine, D.; Stevenson, C.S. Btk Inhibitor RN983 Delivered by Dry Powder Nose-only Aerosol Inhalation Inhibits Bronchoconstriction and Pulmonary Inflammation in the Ovalbumin Allergic Mouse Model of Asthma. J. Aerosol. Med. Pulm. Drug Deliv. 2016, 29, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Ji, H.L. Epithelial sodium and chloride channels and asthma. Chin. Med. J. 2015, 128, 2242–2249. [Google Scholar] [CrossRef] [PubMed]
- Southworth, T.; Plumb, J.; Gupta, V.; Pearson, J.; Ramis, I.; Lehner, M.D.; Miralpeix, M.; Singh, D. Anti-inflammatory potential of PI3Kδ and JAK inhibitors in asthma patients. Respir. Res. 2016, 17, 124. [Google Scholar] [CrossRef] [PubMed]
- Ashino, S.; Takeda, K.; Li, H.; Taylor, V.; Joetham, A.; Pine, P.R.; Gelfand, E.W. Janus kinase 1/3 signaling pathways are key initiators of TH2 differentiation and lung allergic responses. J. Allergy Clin. Immunol. 2013, 133, 1162–1174.e4. [Google Scholar] [CrossRef]
- Calama, E.; Ramis, I.; Domènech, A.; Carreño, C.; de Alba, J.; Prats, N.; Miralpeix, M. Tofacitinib ameliorates inflammation in a rat model of airway neutrophilia induced by inhaled LPS. Pulm. Pharmacol. Ther. 2017, 43, 60–67. [Google Scholar] [CrossRef]
- Calbet, M.; Ramis, I.; Calama, E.; Carreño, C.; Paris, S.; Maldonado, M.; Orellana, A.; Calaf, E.; Pauta, M.; de Alba, J.; et al. Novel inhaled pan-JAK inhibitor, LAS194046, reduces allergen-induced airway inflammation, late asthmatic response, and PSTAT activation in brown Norway rats. J. Pharmacol. Exp. Ther. 2019, 370, 137–147. [Google Scholar] [CrossRef]
- van Ree, R.; van Leeuwen, W.A.; Bulder, I.; Bond, J.; Aalberse, R.C. Purified natural and recombinant Fel d 1 and cat albumin in in vitro diagnostics for cat allergy. J. Allergy Clin. Immunol. 1999, 104, 1223–1230. [Google Scholar] [CrossRef]
- Grönlund, H.; Saarne, T.; Gafvelin, G.; van Hage, M. The major cat allergen, fel d 1, in diagnosis and therapy. Int. Arch. Allergy Immunol. 2010, 151, 265–274. [Google Scholar] [CrossRef]
- Kamal, M.A.; Dingman, R.; Wang, C.Q.; Lai, C.H.; Rajadhyaksha, M.; DeVeaux, M.; Orengo, J.M.; Radin, A.; Davis, J.D. REGN1908-1909 monoclonal antibodies block Fel d 1 in cat allergic subjects: Translational pharmacokinetics and pharmacodynamics. Clin. Transl. Sci. 2021, 14, 2440–2449. [Google Scholar] [CrossRef]
- Orengo, J.M.; Radin, A.R.; Kamat, V.; Badithe, A.; Ben, L.H.; Bennett, B.L.; Zhong, S.; Birchard, D.; Limnander, A.; Rafique, A.; et al. Treating cat allergy with monoclonal IgG antibodies that bind allergen and prevent IgE engagement. Nat. Commun. 2018, 14, 2440–2449. [Google Scholar] [CrossRef]
- Shamji, M.H.; Singh, I.; Layhadi, J.A.; Ito, C.; Karamani, A.; Kouser, L.; Sharif, H.; Tang, J.; Handijiev, S.; Parkin, R.V.; et al. Passive prophylactic administration with a single dose of Anti–Fel d 1 monoclonal antibodies REGN1908–1909 in cat allergen–induced allergic rhinitis: A randomized, double-blind, placebo-controlled clinical trial. Am. J. Respir. Crit. Care Med. 2021, 204, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Knopp Biosciences. Dexpramipexole Targets Eosinophilic Inflammation, (n.d.). Available online: https://www.nature.com/articles/d43747-020-01157-2 (accessed on 6 June 2022).
- Denning, D.W.; O’Driscoll, B.R.; Hogaboam, C.M.; Bowyer, P.; Niven, R.M. The link between fungi and severe asthma: A summary of the evidence. Eur. Respir. J. 2006, 27, 615–626. [Google Scholar] [CrossRef] [PubMed]
- Denning, D.W.; Pashley, C.; Hartl, D.; Wardlaw, A.; Godet, C.; del Giacco, S.; Delhaes, L.; Sergejeva, S. Fungal allergy in asthma-state of the art and research needs. Clin. Transl. Allergy. 2014, 4, 14. [Google Scholar] [CrossRef]
- Van Norman, G.A. Drugs and Devices: Comparison of European and U.S. Approval Processes. JACC Basic Transl. Sci. 2016, 1, 399–412. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Guideline for Good Clinical Practice E6(R2); European Medicines Agency: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Rogliani, P.; Calzetta, L. Clinical Interpretation of Efficacy Outcomes in Pharmacological Studies on Triple Fixed-Dose Combination Therapy for Uncontrolled Asthma: Assessment of IRIDIUM and ARGON Studies. J. Exp. Pharmacol. 2022, 14, 1–5. [Google Scholar] [CrossRef]
- FDA. Dietary Supplements: Questions and Answers; FDA: Silver Spring, MD, USA, 2015. [Google Scholar]
- European Food Safety Authority (EFSA). Food Supplements, (n.d.); EFSA: Parma, Italy, 2006. [Google Scholar]
- Jang, S.O.; Kim, H.J.; Kim, Y.J.; Kang, M.J.; Kwon, J.W.; Seo, J.H.; Kim, H.Y.; Kim, B.J.; Yu, J.; Hong, S.J. Asthma prevention by Lactobacillus rhamnosus in a mouse model is associated with CD4 +CD25 +Foxp3 +T cells, Allergy. Asthma Immunol. Res. 2012, 4, 150–156. [Google Scholar] [CrossRef]
- Feleszko, W.; Jaworska, J.; Rha, R.D.; Steinhausen, S.; Avagyan, A.; Jaudszus, A.; Ahrens, B.; Groneberg, D.A.; Wahn, U.; Hamelmann, E. Probiotic-induced suppression of allergic sensitization and airway inflammation is associated with an increase of T regulatory-dependent mechanisms in a murine model of asthma. Clin. Exp. Allergy 2006, 37, 498–505. [Google Scholar] [CrossRef]
- Drago, L.; de Vecchi, E.; Gabrieli, A.; de Grandi, R.; Toscano, M. Immunomodulatory effects of Lactobacillus salivarius LS01 and Bifidobacterium breve BR03, alone and in combination, on peripheral blood mononuclear cells of allergic asthmatics, Allergy. Asthma Immunol. Res. 2015, 7, 409–413. [Google Scholar] [CrossRef]
- Liu, A.; Ma, T.; Xu, N.; Jin, H.; Zhao, F.; Kwok, L.-Y.; Zhang, H.; Zhang, S.; Sun, Z. Adjunctive Probiotics Alleviates Asthmatic Symptoms via Modulating the Gut Microbiome and Serum Metabolome. Microbiol. Spectr. 2021, 9, e0085921. [Google Scholar] [CrossRef]
- Food and Drug Administration (FDA). Investigational New Drug Applications (INDs)—Determining Whether Human Research Studies Can Be Conducted without an IND|FDA; FDA: Silver Spring, MD, USA, 2013.
- Salminen, S.; Collado, M.C.; Endo, A.; Hill, C.; Lebeer, S.; Quigley, E.M.M.; Sanders, M.E.; Shamir, R.; Swann, J.R.; Szajewska, H.; et al. The International Scientific Association of Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 649–667. [Google Scholar] [CrossRef]
- Chiu, C.J.; Huang, M.T. Asthma in the precision medicine era: Biologics and probiotics. Int. J. Mol. Sci. 2021, 22, 4528. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Zhang, Y.; He, C.; Dai, J. Probiotics supplementation in children with asthma: A systematic review and meta-analysis. J. Paediatr. Child Health 2018, 54, 953–961. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Wang, L.; Wu, S.; Yuan, L.; Tang, S.; Xiang, Y.; Qu, X.; Liu, H.; Qin, X.; Liu, C. Efficacy of probiotic supplementary therapy for asthma, allergic rhinitis, and wheeze: A meta-analysis of randomized controlled trials. Allergy Asthma Proc. 2019, 40, 250–260. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.; Jiang, P.; Liu, J.; Sun, R.; Zhu, L. Association between probiotic supplementation and asthma incidence in infants: A meta-analysis of randomized controlled trials. J. Asthma. 2020, 57, 167–178. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Collins, A.M.; Coughlin, D.; Kirk, S. The role of google scholar in evidence reviews and its applicability to grey literature searching. PLoS ONE 2015, 10, e0138237. [Google Scholar] [CrossRef]
- Lommatzsch, M.; Brusselle, G.G.; Canonica, G.W.; Jackson, D.J.; Nair, P.; Buhl, R.; Virchow, J.C. Disease-Modifying Anti-Asthmatic Drugs. Lancet 2022, 399, 1664–1668. [Google Scholar] [CrossRef]
- Calzetta, L.; Rogliani, P. Letter to the Editor Regarding “Clinical Remission in Severe Asthma: A Pooled Post Hoc Analysis of the Patient Journey with Benralizumab”. Adv. Ther. 2022, 39, 3857–3861. [Google Scholar] [CrossRef]

| Study and Year | Class of Drug | ClinicalTrials.gov Identifier and/or Company ID | Study Characteristics | Treatment Duration (wks) | Number of Analysed Patients | Drugs, Doses, and Regimen of Administration | Comparator | Route of Administration | Inhaler Device (Brand) | Patients’ Characteristics | Age (Years) | Male (%) | Current Smokers (%) | Post Bronchodilator FEV1 (% Predicted) | Investigated Outcome | Jadad Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moss et al., 2022, LEDA [36,37] | DP2 antagonist | NCT03683576 | Phase IIb, multicentre, randomised, PCB-controlled, double-blind parallel-group study | 24 | 481 | Standard of care treatment + GB001 20 mg, 40 mg, 60 mg QD | Standard of care treatment + PCB | GB001 and PCB: PO | NA | Moderate to severe eosinophilic asthma (pre-bronchodilator FEV1 ≤ 85% predicted and airway reversibility or AHR; peripheral blood eosinophil count ≥ 250 cells/μL) | 51.8 | 35.8 | 0.0 | NA | FEV1, PEF, ACQ, symptoms control, and exacerbations | 3 |
| Singh et al., 2022 [30,31] | Anti-IL-5 mAb | NCT03287310 | Phase I, multicentre, randomised, PCB-controlled, double-blind parallel-group study | 1 day | 48 | As-needed SABA and stable low to moderate dose of ICS or ICS/LABA + single dose of depemokimab (GSK3511294) 2 mg, 10 mg, 30 mg, 100, 300 mg | As-needed SABA and stable low-to-moderate dose of ICS or stable low-to-moderate dose of ICS/LABA + PCB | SABA, ICS/LABA, ICS: oral inhalation; depemokimab: SC | NA | Mild to moderate asthma (pre-bronchodilator FEV1≥ 60% predicted, ACT score >19, and blood eosinophil count of ≥200 cells/μL) | 44.0 | 95.8 | 0.0 | 81.0 | FEV1 and eosinophil count | 5 |
| Cass et al., 2021 [38,39] | Antifungal triazole | NCT02715570 | Phase I, single centre, two-part randomised, PCB-controlled, single-blind crossover study | 1 day | 9 | Single dose of PC945 5 mg | PCB | Oral inhalation | NA | Mild asthma | 37.7 | 66.7 | NA | NA | FEV1 | 2 |
| Chupp et al., 2021, GRANIT [48,49,50] | SGRM | NCT03622112 | Phase IIb, multicentre, randomised, PCB-controlled, double-blind parallel-group study | 12 | 805 | Velsecorat (AZD7594) 50μg, 90 µg, 180 µg, 360 µg, 720 µg QD | FF (100 µg QD); PCB | Oral inhalation | DPI (NA) | Asthma (patients who remain symptomatic on low dose BUD [200 μg BID in Europe and 180 μg BID in US] | 53.2 | 42.0 | NA | NA | FEV1, PEF, ACQ, symptoms control, FENO, rescue medication use, and exacerbations | 3 |
| De Gaix et al., 2021 [51,52] | Anti-Fel d 1 mAb cocktail | NCT03838731 | Phase II, single-centre, randomised, PCB-controlled, double-blind parallel-group study | 1 day | 56 | Single dose of REGN1908-1909 600 mg | PCB | SC | NA | Mild asthma with cat allergy | 29.3 | 37.5 | NA | NA | FEV1 | 3 |
| Siddiqui et al., 2021, EXHALE [28,29] | Synthetic aminobenzothiazole | NCT04046939 | Phase II, multicentre, randomised, PCB-controlled, double-blind parallel-group study | 12 | 103 | Dexpramipexole (KNS-760704) 37.5 mg, 75 mg, 150 mg BID | PCB | PO | NA | Moderate to severe eosinophilic asthma (FEV1 < 80% predicted and bronchodilator FEV1 reversibility ≥ 12% and ≥200 mL) | 45.3 | 47.6 | 0.0 | NA | FEV1, ACQ, eosinophil count, FENO, and AQLQ | 3 |
| Wechsler et al., 2021 [32,33] | Anti-IL-33 mAb | NCT03387852 | Phase II, multicentre, randomised, PCB-controlled, double-blind parallel-group study | 12 | 296 | Progressive withdrawal of background medication with medium-to-high-dose FP/LABA + itepekimab (SAR440340/REGN3500) 300 mg Q2W with or without dupilumab 300 mg Q2W | Progressive withdrawal of background medication with medium-to-high-dose FP/LABA + PCB or dupilumab | FP/LABA: oral inhalation; itepekimab and dupilumab: SC | NA | Moderate to severe asthma (pre-bronchodilator FEV1 ≥ 50% and ≤85% predicted and bronchodilator FEV1 reversibility ≥ 12% and ≥200 mL; ≥1 severe exacerbation within 12 months prior to screening; FEV1 ≥ 20% reduction in response to a provocative concentration of inhaled methacholine of <8 mg/mL within 12 months prior to screening) | 49.1 | 36.0 | 0.0 | NA | FEV1, ACQ, symptoms control, eosinophil count, and FENO | 3 |
| Miller et al., 2020 [34,35] | LABA | NCT03257995 | Phase II, multicentre, three-period complete block, randomised, PCB-controlled, double-blind crossover study | 2 | 54 | Background ICS medication and SABA + indacaterol maleate 150 μg QD | Background ICS medication and SABA + indacaterol acetate 150 μg QD; PCB | Oral inhalation | DPI (Breezhaler) | Asthma (pre-bronchodilator FEV1 ≥ 50% and ≤90% predicted normal, increase in FEV1 ≥ 12% and ≥ 200 mL within 30 min after administration of salbutamol 400 μg/albuterol 360 μg or equivalent dose) | 48.0 | 33.3 | 0.0 | 86.0 | FEV1, PEF, and rescue medication use | 3 |
| Moermans et al., 2020 [44,45] | Probiotic | NCT03341403 | Phase II/III, single-centre, randomised, PCB-controlled, double-blind parallel-group study | 12 | 46 | Stable asthma treatment + Probiotical® TID (containing Lactobacillus, Bifidobacterium, and Streptococcus thermophilus, 18 billion bacteria per pill) | Stable asthma treatment + PCB | PO | NA | Severe uncontrolled asthma (ACQ score > 1.5) | 18.0–75.0 | NA | NA | NA | ACQ and eosinophil count | 3 |
| NA, 2019 [25] | Selective BTK inhibitor | NCT03944707 | Phase II, multicentre, randomised, PCB-controlled, subject- and investigator-blinded parallel-group study | 12 | 76 | BUD/FOR 160/9 μg BID + remibrutinib (LOU064) 100 mg QD | BUD/FOR 160/9 μg BID + PCB | BUD/FOR: oral inhalation; LOU064 and PCB: PO | BUD/FOR: DPI (NA) | Inadequately controlled asthma | 50.7 | 34.2 | NA | NA | FEV1, PEF, ACQ, rescue medication use, and symptoms control | 3 |
| NA, 2019 [27] | Pan-JAK inhibitor | NCT04150341 | Phase II, multicentre, randomised, PCB-controlled, double-blind crossover study | 2 | 24 | TD-8236 150 µg, 1500 µg QD | PCB | Oral inhalation | DPI (NA) | Mild asthma with a known response to an allergen challenge (pre-bronchodilator FEV1 ≥ 70% predicted) | 42.0 | 70.8 | NA | NA | FEV1 | 3 |
| Bruns et al., 2019 [46,47] | IL-4Rα inhibitor | NCT03574805 | Phase I, multicentre, randomised, PCB-controlled, single-blind parallel-group study | ≅1.4 | 42 | AZD1402 (PRS-060) 2 mg, 6 mg, 20 mg, 60 mg BID | PCB | Oral inhalation | Nebuliser (InnoSpire Go) | Mild asthma (pre-bronchodilator FEV1 ≥ 70% predicted and FEV1/FVC ≥ 0.7) | 28.4 | 88.1 | 0.0 | NA | FENO | 2 |
| NA, 2018 [23] | Anti-IL-33R mAb | NCT03393806 | Phase II, single-centre, randomised, PCB-controlled, double-blind parallel-group study | 12 | 17 | Standard of care treatment + melrilimab (GSK3772847/CNTO7160) 10 mg/kg Q4W | Standard of care treatment + PCB | Melrilimab and PCB: IV | NA | Moderate to severe asthma with allergic fungal airway disease | 56.9 | 70.6 | 0.0 | NA | FEV1, ACQ, eosinophil count, FENO, and AQLQ | 3 |
| NA, 2018 [40,41] | Anti-IL-33 mAb | NCT03469934 | Phase II, multicentre, randomised, PCB-controlled, double-blind parallel-group study | ≅18 | 25 | Background medication with high dose ICS/LABA + single dose of etokimab (ANB-020) 300 mg/100 mL | Background medication with high dose ICS/LABA + PCB | ICS/LABA: oral inhalation; etokimab and PCB: IV | NA | Severe eosinophilic asthma | 38.5 | 72.0 | NA | NA | FEV1, eosinophil count, FENO, and exacerbations | 3 |
| NA, 2017 [22] | anti-IL-17A mAb | NCT03299686 | Phase II, multicentre, randomised, PCB-controlled, subject- and investigator-blinded parallel-group study | 12 | 118 | Standard care of treatment + CJM112 300 mg QW for 4 wks, then Q2W up to 12 wks | Standard care of treatment + PCB | CJM112 and PCB: SC | NA | Inadequately controlled moderate to severe asthma (FEV1 ≥ 40% and ≤90% predicted; ACQ score ≥ 1.5; total serum IgE <1 50 IU/mL; peripheral blood eosinophils < 300/μL) | 56.6 | 39.8 | NA | NA | FEV1 and ACQ | 3 |
| NA, 2017, [24] | Anti-IL-33R mAb | NCT03207243 | Phase IIa, multicentre, randomised, PCB-controlled, double-blind parallel-group study | 16 | 165 | FP/SAL 500/50 μg BID for 2 wks, then switch to FP 500 μg BID for 2 wks, then FP dose reduction by 50% Q2W until discontinuation + melrilimab (GSK3772847/CNTO7160) 10 mg/kg Q4W | FP/SAL (500/50 μg BID) for 2 wks, then switch to FP (500 μg BID) for 2 wks, then FP dose reduction by 50% Q2W until discontinuation + PCB | FP/SAL, FP: oral inhalation; melrilimab and PCB: IV | FP/SAL, FP: DPI (Diskus) | Moderately severe asthma (bronchodilator FEV1 reversibility ≥ 12% and ≥200 mL; ACQ score ≥ 1.0 and <4.0) | 52.9 | 28.5 | 0.0 | NA | FEV1, PEF, ACQ, symptoms control, rescue eosinophil count, FENO, exacerbations and hospitalisations, and SGRQ | 3 |
| NA, 2017 [53,54] | Anti-TSLP mAb fragment | NCT03138811 | Phase I, multicentre, randomised, PCB-controlled, double-blind parallel-group study | 12 | 28 | Ecleralimab (CSJ117) 4 mg QD | PCB | Oral inhalation | DPI (PulmoSol) | Mild atopic asthma with an early and late response to a common inhaled allergen challenge | 34.1 | 39.3 | NA | NA | FEV1 | 3 |
| NA, 2017 [26] | ENaC inhibitor | NCT03135899 | Phase I, single-centre, randomised, PCB-controlled, double-blind, double-dummy crossover study | 2 days | 37 | BI 443651 100 μg, 400 μg, 1200 μg, thrice 12 h apart | PCB | Oral inhalation | SMI (Respimat) | Mild asthma upon methacholine challenge (pre-bronchodilator FEV1 ≥ 70% predicted; FEV1 ≥ 20% reduction in response to a provocative concentration of inhaled methacholine of ≤1 mg; ACQ score < 1.5) | 37.4 | 91.9 | 0.0 | NA | FEV1 | 3 |
| NA, 2017 [42,43] | MABA | NCT03378648 | Phase I/II, single-centre, randomised, PCB-controlled, double-blind parallel-group study | 1 | 48 | CHF6366 40 μg, 80 μg, 160 μg, 240 μg QD | PCB | Oral inhalation | NA | Asthma (bronchodilator FEV1 reversibility ≥ 12% and ≥200 mL) | 38.1 | 64.6 | NA | NA | FEV1 | 3 |
| Outcome | Treatment | Drug Class | Delta Effect | Suggested MCID [103] | Beneficial Clinically Relevant Effect |
|---|---|---|---|---|---|
| Trough FEV1 | Itepekimab 300 mg Q2W | Anti-IL-33 mAb | 140 mL (10–270) | >100 mL | Yes |
| Indacaterol maleate 150 μg QD | LABA | 186 mL (129–243) | >100 mL | Yes | |
| Peak FEV1 | Itepekimab 300 mg Q2W + dupilumab 300 Q2W | Anti-IL-33 mAb + anti IL-4/IL-13 mAb | 130 mL (10–250) | ≥12% and ≥200 mL | No |
| PEF | Indacaterol maleate 150 μg QD | LABA | 33.00 L/min (25.60–40.30) | >5.39% | ? |
| Morning PEF | Velsecorat 720 μg QD | SGRM | 16.60 L/min (8.03–25.17) | >5.39% | ? |
| Evening PEF | Velsecorat 720 μg QD | SGRM | 11.99 L/min (3.57–20.42) | >5.39% | ? |
| ACQ | Itepekimab 300 mg Q2W | Anti-IL-33 mAb | −0.42 points (−0.73–−0.12) | >0.5 points | Borderline |
| Itepekimab 300 mg Q2W + dupilumab 300 mg Q2W | Anti-IL-33 mAb + anti IL-4/IL-13 mAb | −0.32 points (−0.63–−0.01) | >0.5 points | No | |
| Velsecorat 720 μg QD | SGRM | −0.27 points (−0.43–−0.10) | >0.5 points | No | |
| CJM112 300 mg QW | IL-17A mAb | −0.23 points (−0.40–−0.06) * | >0.5 points | No | |
| Exacerbations | Velsecorat 720 μg QD | SGRM | 0.11 rate (0.04–0.25) | >−20% rate | Yes |
| AQLQ | Itepekimab 300 mg Q2W | Anti-IL-33 mAb | 0.45 points (0.14–0.77) | >0.5 points | Borderline |
| Itepekimab 300 mg Q2W + dupilumab 300 mg Q2W | Anti-IL-33 mAb + anti IL-4/IL-13 mAb | 0.43 points (0.11–0.75) | >0.5 points | Borderline |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calzetta, L.; Aiello, M.; Frizzelli, A.; Pistocchini, E.; Ritondo, B.L.; Rogliani, P.; Chetta, A. Investigational Treatments in Phase I and II Clinical Trials: A Systematic Review in Asthma. Biomedicines 2022, 10, 2330. https://doi.org/10.3390/biomedicines10092330
Calzetta L, Aiello M, Frizzelli A, Pistocchini E, Ritondo BL, Rogliani P, Chetta A. Investigational Treatments in Phase I and II Clinical Trials: A Systematic Review in Asthma. Biomedicines. 2022; 10(9):2330. https://doi.org/10.3390/biomedicines10092330
Chicago/Turabian StyleCalzetta, Luigino, Marina Aiello, Annalisa Frizzelli, Elena Pistocchini, Beatrice Ludovica Ritondo, Paola Rogliani, and Alfredo Chetta. 2022. "Investigational Treatments in Phase I and II Clinical Trials: A Systematic Review in Asthma" Biomedicines 10, no. 9: 2330. https://doi.org/10.3390/biomedicines10092330
APA StyleCalzetta, L., Aiello, M., Frizzelli, A., Pistocchini, E., Ritondo, B. L., Rogliani, P., & Chetta, A. (2022). Investigational Treatments in Phase I and II Clinical Trials: A Systematic Review in Asthma. Biomedicines, 10(9), 2330. https://doi.org/10.3390/biomedicines10092330








