UniStArt: A 12-Month Prospective Observational Study of Body Weight, Dietary Intake, and Physical Activity Levels in Australian First-Year University Students
Abstract
:1. Introduction
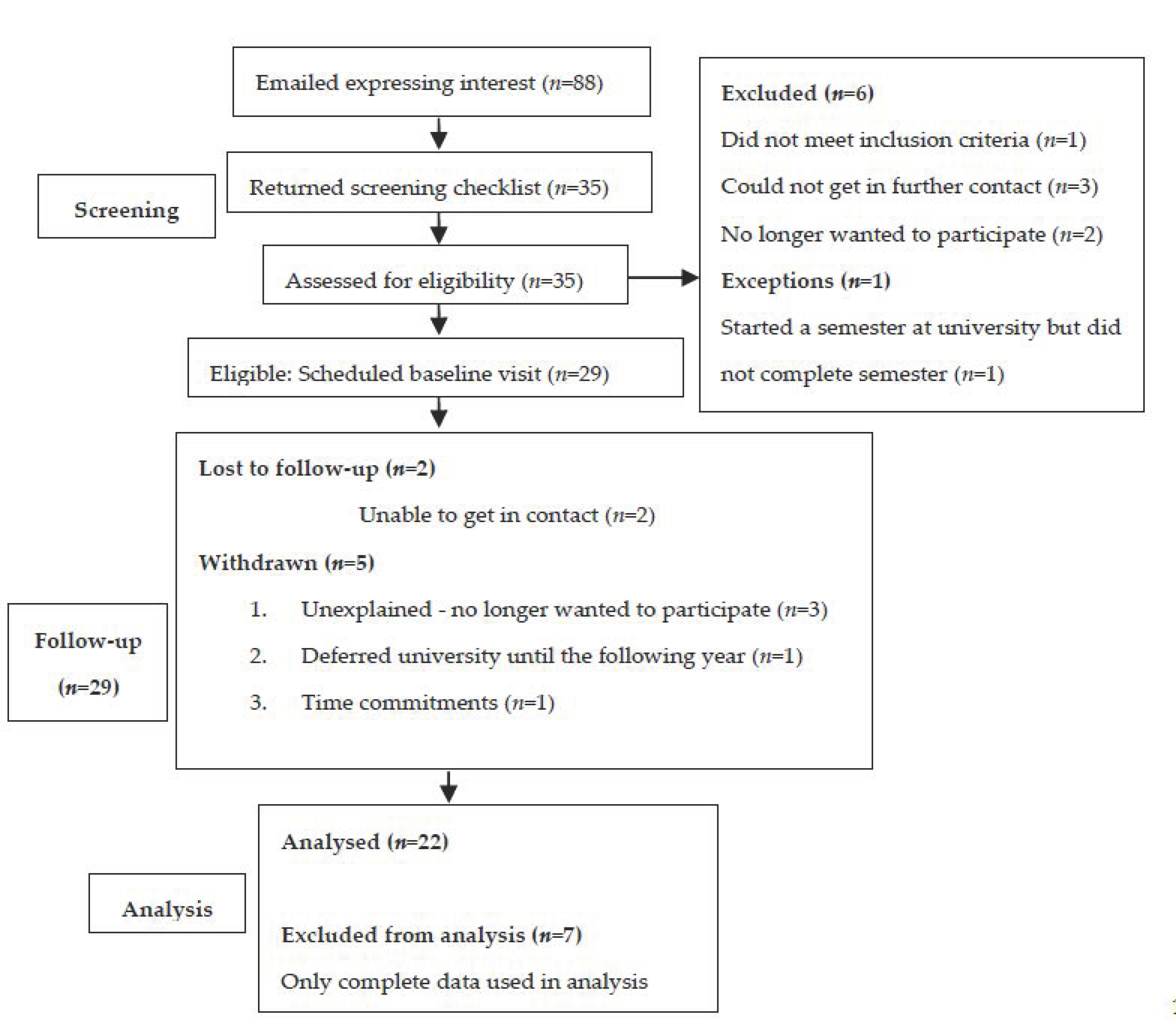
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Australian Bureau of Statistics. National Health Survey: First Results, 2017–2018; Australian Bureau of Statistics: Canberra, Australia, 2018.
- Guh, D.; Zhang, W.; Bansback, N.; Amarsi, Z.; Birmingham, C.L.; Anis, A. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BioMed Cent. Public Health 2009, 9, 88. [Google Scholar] [CrossRef] [PubMed]
- Commonwealth of Australia. The National Obesity Strategy 2022-2032: At a Glance; Health Ministers Meeting: Canberra, Australia, 2022. [Google Scholar]
- Australian Bureau of Statistics. Overweight and Obesity; Australian Bureau of Statistics: Canberra, Australia, 2013.
- Bray, S.R.; Born, H.A. Transition to University and Vigorous Physical Activity: Implications for Health and Psychological Well-Being. J. Am. Coll. Health 2010, 52, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Leslie, E.; Owen, N.; Salmon, J.; Bauman, A.; Sallis, J.F.; Lo, S.K. Insufficiently Active Australian College Students: Perceived Personal, Social, and Environmental Influences. Prev. Med. 1999, 28, 20–27. [Google Scholar] [CrossRef]
- Sinclair, K.M.; Hamlin, M.J.; Steel, G.D. Physical activity levels of first-year New Zealand university students. Youth Stud. Aust. 2005, 24, 38–42. [Google Scholar]
- Levitsky, D.A.; Halbmaier, C.A.; Mrdjenovic, G. The freshman weight gain: A model for the study of the epidemic of obesity. Int. J. Obes. 2004, 28, 1435–1442. [Google Scholar] [CrossRef] [PubMed]
- Racette, S.B.; Deusinger, S.S.; Strube, M.J.; Highstein, G.R.; Deusinger, R.H. Weight Changes, Exercise, and Dietary Patterns During Freshman and Sophomore Years of College. J. Am. Coll. Health 2005, 53, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Niemeier, H.M.; Raynor, H.A.; Lloyd-Richardson, E.E.; Rogers, M.L.; Wing, R.R. Fast Food Consumption and Breakfast Skipping: Predictors of Weight Gain from Adolescence to Adulthood in a Nationally Representative Sample. J. Adolesc. Health 2006, 39, 842–849. [Google Scholar] [CrossRef]
- Adams, T.; Rini, A. Predicting 1-Year Change in Body Mass Index Among College Students. J. Am. Coll. Health 2007, 55, 361–365. [Google Scholar] [CrossRef]
- O’Malley, P.M.; Johnston, L.D. Epidemiology of alcohol and other drug use among American college students. J. Stud. Alcohol Suppl. 2002, 14, 23–39. [Google Scholar] [CrossRef]
- Singh, A.S.; Mulder, C.; Twisk, J.W.R.; Van Mechelen, W.; Chinapaw, M.J.M. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes. Rev. 2008, 9, 474–488. [Google Scholar] [CrossRef]
- Brevard, P.B.; Ricketts, C.D. Residence of College Students Affects Dietary Intake, Physical Activity, and Serum Lipid Levels. J. Am. Diet. Assoc. 1996, 96, 35–38. [Google Scholar] [CrossRef]
- Maillet, M.A.; Grouzet, F.M.E. Understanding changes in eating behavior during the transition to university from a self-determination theory perspective: A systematic review. J. Am. Coll. Health 2021, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Education and Training; Australian Bureau of Statistics: Canberra, Australia, 2012.
- Hodge, C.N.; Jackson, L.A.; Sullivan, L.A. The ‘Freshman 15’. Psychol. Women Q. 1993, 17, 119–126. [Google Scholar] [CrossRef]
- Butler, S.M.; Black, D.R.; Blue, C.L.; Gretebeck, R.J. Change in Diet, Physical Activity, and Body Weight in Female College Freshman. Am. J. Health Behav. 2004, 28, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Baum, C.L. The Effects of College on Weight: Examining the “Freshman 15” Myth and Other Effects of College Over the Life Cycle. Demography 2017, 54, 311–336. [Google Scholar] [CrossRef] [PubMed]
- Vadeboncoeur, C.; Townsend, N.; Foster, C. A meta-analysis of weight gain in first year university students: Is freshman 15 a myth? BMC Obes. 2015, 2, 22. [Google Scholar] [CrossRef]
- Lloyd-Richardson, E.E.; Bailey, S.; Fava, J.L.; Wing, R.; The Tobacco Etiology Research Network (TERN). A prospective study of weight gain during the college freshman and sophomore years. Prev. Med. 2009, 48, 256–261. [Google Scholar] [CrossRef]
- Miller, K.G.; Hartman, J.M. Influence of physical activity on weight status during the first year of college. J. Am. Coll. Health 2020, 68, 258–262. [Google Scholar] [CrossRef] [PubMed]
- International Society for the Advancement of Kinanthropometry. International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry: Lower Hutt, New Zealand, 2011; pp. 52–81. [Google Scholar]
- Gupta, N.; Balasekaran, G.; Govindaswamy, V.V.; Hwa, C.Y.; Shun, L.M. Comparison of body composition with bioelectric impedance (BIA) and dual energy X-ray absorptiometry (DEXA) among Singapore Chinese. J. Sci. Med. Sport 2011, 14, 33–35. [Google Scholar] [CrossRef]
- Batterham, M.; Tapsell, L.; Jenkins, A. A comparison of bioelectrical impedance and near infra-red interactance with dual energy x-ray absorptiometry for the determination of body fat. Nutr. Diet. 2002, 59, 120–126. [Google Scholar]
- Xyris Software Australia Pty Ltd. FoodWorks 8 Professional, 8; Xyris Software Australia Pty Ltd.: Brisbane, Australia, 2015. [Google Scholar]
- National Health and Medical Research Council. Eat for Health: Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2013; pp. 1–226. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Leon, A.S.; Jacobs, D.R., Jr.; Montoye, H.J.; Sallis, J.F.; Paffenbarger, R.S., Jr. Compendium of Physical Activities: Classification of energy costs of human physical activities. Med. Sci. Sports Exerc. 1993, 25, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Crouter, S.E.; Antczak, A.; Hudak, J.R.; DellaValle, D.M.; Haas, J.D. Accuracy and reliability of the ParvoMedics TrueOne 2400 and MedGraphics VO2000 metabolic systems. Eur. J. Appl. Physiol. 2006, 98, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Weir, J.B.D.B. New methods for calculating metabolic rate with special reference to protein metabolism. J. Physiol. 1949, 109, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Stunkard, A.J.; Messick, S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J. Psychosom. Res. 1985, 29, 71–83. [Google Scholar] [CrossRef]
- IBM. Statistical Product and Service Solution (SPSS) Statistics, 21; IBM: Chicago, IL, USA, 2012. [Google Scholar]
- Hajhosseini, L.; Holmes, T.; Mohamadi, P.; Goudarzi, V.; McProud, L.; Hollenbeck, C.B. Changes in Body Weight, Body Composition and Resting Metabolic Rate (RMR) in First-Year University Freshmen Students. J. Am. Coll. Nutr. 2006, 25, 123–127. [Google Scholar] [CrossRef]
- Finlayson, G.; Cecil, J.; Higgs, S.; Hill, A.; Hetherington, M. Susceptibility to weight gain. Eating behaviour traits and physical activity as predictors of weight gain during the first year of university. Appetite 2012, 58, 1091–1098. [Google Scholar] [CrossRef]
- Deliens, T.; Clarys, P.; Van Hecke, L.; De Bourdeaudhuij, I.; Deforche, B. Changes in weight and body composition during the first semester at university. A prospective explanatory study. Appetite 2013, 65, 111–116. [Google Scholar] [CrossRef]
- Mifsud, G.; Duval, K.; Doucet, E. Low body fat and high cardiorespiratory fitness at the onset of the freshmen year may not protect against weight gain. Br. J. Nutr. 2009, 101, 1406–1412. [Google Scholar] [CrossRef]
- Anderson, D.A.; Shapiro, J.R.; Lundgren, J.D. The freshman year of college as a critical period for weight gain: An initial evaluation. Eat. Behav. 2003, 4, 363–367. [Google Scholar] [CrossRef]
- Levitsky, D.A.; Garay, J.; Nausbaum, M.; Neighbors, L.; Dellavalle, D.M. Monitoring weight daily blocks the freshman weight gain: A model for combating the epidemic of obesity. Int. J. Obes. 2006, 30, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Kȩska, A.; Lutosławska, G.; Mazurek, K.; Czajkowska, A.; Tkaczyk, J.; Iwanska, D. Changes in Anthropometry and Selected Metabolic Parameters in Young Men During Their First Year of Study at a University of Physical Education. Am. J. Men’s Health 2017, 12, 463–471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, M.E.; Bray, S.R.; Martin Ginis, K.A. Behavior Change and the Freshman 15: Tracking Physical Activity and Dietary Patterns in 1st-Year University Women. J. Am. Coll. Health 2008, 56, 523–530. [Google Scholar] [CrossRef]
- Olansky, S.; Beaudry, K.M.; Woods, S.; Barbour-Tuck, E.; Gammage, K.L.; Klentrou, P.; Josse, A.R. Changes in Body Composition, Energy Expenditure, and Energy Intake during Four Years of University—A Follow-Up Study. Int. J. Environ. Res. Public Health 2021, 18, 3990. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.; Moreira, P.; Teixeira, V. Holiday weight gain in university students. Aliment. Hum. 2007, 13, 17–19. [Google Scholar]
- Tayyem, R.F.; Bayadoo, F.; Kassab, M.; Khriesat, W.M.; Al-Haifi, A.R.; Banks, A.D.; Bawadi, H.A. Association of college entrance exam with changes in some lifestyle factors among adolescents. Nutr. Food Sci. 2013, 43, 573–581. [Google Scholar] [CrossRef]
- Sprake, E.; Lavin, J.; Grabowski, P.; Russell, J.; Featherstone, M.; Barker, M. Eating habits associated with body weight gain in female university students. Br. Food J. 2017, 119, 2571–2582. [Google Scholar] [CrossRef]
- Economos, C.D.; Hildebrandt, M.L.; Hyatt, R.R. College freshman stress and weight change: Differences by gender. Am. J. Health Behav. 2008, 32, 16–25. [Google Scholar] [CrossRef]
- Du, C.; Luo, N.; Wu, L.; Gadd, S.; Zhang, X.; Tucker, R.M. Health behavior changes associated with weight gain among first-year international students studying at an American university. J. Am. Coll. Health 2021, 1–10. [Google Scholar] [CrossRef]
- Pullman, A.W.; Masters, R.C.; Zalot, L.C.; Carde, L.E.; Saraiva, M.M.; Dam, Y.Y.; Randall Simpson, J.A.; Duncan, A.M. Effect of the transition from high school to university on anthropometric and lifestyle variables in males Presented in part at the Canadian Society for Nutritional Sciences, Canadian Nutrition Congress, held in Winnipeg, Manitoba, from 18–21 June 2007. Appl. Physiol. Nutr. Metab. 2009, 34, 162–171. [Google Scholar] [CrossRef]
- Jebb, S.A.; Moore, M.S. Contribution of a sedentary lifestyle and inactivity to the etiology of overweight and obesity: Current evidence and research issues. Med. Sci. Sports Exerc. 1999, 31, S534–S541. [Google Scholar] [CrossRef] [PubMed]
- De Cocker, K.A.; van Uffelen, J.G.; Brown, W.J. Associations between sitting time and weight in young adult Australian women. Prev. Med. 2010, 51, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Van Der Ploeg, H.P.; Chey, T.; Korda, R.J.; Banks, E.; Bauman, A. Sitting Time and All-Cause Mortality Risk in 222 497 Australian Adults. Arch. Intern. Med. 2012, 172, 494–500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilmot, E.G.; Edwardson, C.L.; Achana, F.A.; Davies, M.J.; Gorely, T.; Gray, L.J.; Khunti, K.; Yates, T.; Biddle, S.J.H. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia 2012, 55, 2895–2905. [Google Scholar] [CrossRef]
- Diehl, K.; Fuchs, A.K.; Rathmann, K.; Hilger-Kolb, J. Students’ Motivation for Sport Activity and Participation in University Sports: A Mixed-Methods Study. BioMed Res. Int. 2018, 2018, 9524861. [Google Scholar] [CrossRef]
- Leslie, E.; Sparling, P.B.; Owen, N. University campus settings and the promotion of physical activity in young adults: Lessons from research in Australia and the USA. Health Educ. 2001, 101, 116–125. [Google Scholar] [CrossRef]
- Cluskey, M.; Grobe, D. College Weight Gain and Behavior Transitions: Male and Female Differences. J. Am. Diet. Assoc. 2009, 109, 325–329. [Google Scholar] [CrossRef]
- Papadaki, A.; Hondros, G.; Scott, J.A.; Kapsokefalou, M. Eating habits of University students living at, or away from home in Greece. Appetite 2007, 49, 169–176. [Google Scholar] [CrossRef]
- Vella-Zarb, R.A.; Elgar, F.J. Predicting the ‘freshman 15’: Environmental and psychological predictors of weight gain in first-year university students. Health Educ. J. 2010, 69, 321–332. [Google Scholar] [CrossRef]
- Nikolaou, C.K.; Hankey, C.R.; Lean, M.E. Weight changes in young adults: A mixed-methods study. Int. J. Obes. 2014, 39, 508–513. [Google Scholar] [CrossRef]
- Yakusheva, O.; Kapinos, K.; Weiss, M. Peer effects and the Freshman 15: Evidence from a natural experiment. Econ. Hum. Biol. 2011, 9, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Rocks, T.; Pelly, F.; Slater, G.; Martin, L.A. Eating attitudes and behaviours of students enrolled in undergraduate nutrition and dietetics degrees. Nutr. Diet. 2016, 74, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Hootman, K.C.; Guertin, K.A.; Cassano, P.A. Stress and psychological constructs related to eating behavior are associated with anthropometry and body composition in young adults. Appetite 2018, 125, 287–294. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity and Overweight. Published 2017. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 12 June 2015).
- Elmadfa, I.; Kornsteiner, M. Fats and Fatty Acid Requirements for Adults. Ann. Nutr. Metab. 2009, 55, 56–75. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. Sodium: Nutrient Reference Values for Australia and New Zealand Including Recommended Dietary Intakes; National Health and Medical Research Council: Canberra, Australia, 2017; pp. 209–216. [Google Scholar]
- Strazzullo, P.; D’Elia, L.; Kandala, N.-B.; Cappuccio, F.P. Salt intake, stroke, and cardiovascular disease: Meta-analysis of prospective studies. BMJ 2009, 339, 1296. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Sugars Intake for Adults and Children; WHO Press: Geneva, Switzerland, 2015; pp. 16–17. [Google Scholar]
- World Health Organization. Diet, Nutrition and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation; World Health Organization: Geneva, Switzerland, 2003; pp. 1–149. [Google Scholar]
- Hilger, J.; Loerbroks, A.; Diehl, K. Eating behaviour of university students in Germany: Dietary intake, barriers to healthy eating and changes in eating behaviour since the time of matriculation. Appetite 2017, 109, 100–107. [Google Scholar] [CrossRef]
- Pinto Guedes, D.; dos Santos Silva, A.L.; Guedes, D.P.; Silva, A.L.D.S. Ejercicio físico y consumo de frutas/verduras, y sus asociaciones con el estado del peso corporal en estudiantes universitarios. Nutr. Hosp. 2021, 38, 545–554. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Manuel Gómez, J.; Lilienthal Heitmann, B.; Kent-Smith, L.; Melchior, J.-C.; Pirlich, M.; et al. Bioelectrical impedance analysis—part II: Utilization in clinical practice. Clin. Nutr. 2004, 23, 1430–1453. [Google Scholar] [CrossRef]

| Characteristics (n = 22) | Mean ± SD |
|---|---|
| Clinical characteristics | |
| Sex (M/F) | 5 males & 17 females |
| Age (years) | 21.1 ± 6.8 |
| Height (cm) | 167.6 ± 9.3 |
| Weight (kg) | 65.0 ± 19.2 |
| Body fat (%) | 24.0 ± 9.2 |
| Body mass index (kg/m2) | 22.9 ± 5.4 |
| Waist circumference (cm) | 75.2 ± 13.2 |
| Hip circumference (cm) | 97.9 ± 11.9 |
| Basal metabolic rate (kcal/day) | 1392 ± 376 |
| Demographic characteristics | n(%) |
| Marital status | |
| Single | 20 (90.9%) |
| Married | 1 (4.5%) |
| Divorced | 0 (0%) |
| De facto | 1 (4.5%) |
| Smoking status | |
| Current smoker | 1 (4.5%) |
| Non-smoker | 20 (90.9%) |
| Smoked previously | 1 (4.5%) |
| Employment status | |
| Employed | 8 (36.4%) |
| Living situation prior to university | |
| Alone | 1 (4.5%) |
| With parents | 18 (81.8%) |
| With partner | 2 (9.1%) |
| With friends (rent a room) | 1 (4.5%) |
| Residential college | 0 (0%) |
| Current living situation | |
| Alone | 2 (9.1%) |
| With parents | 13 (59.1%) |
| With partner | 4 (18.2%) |
| With friends (rent a room) | 2 (9.1%) |
| Residential college | 1 (4.5%) |
| Pre-university vs. current living situation 1, p = 0.515 | |
| Enrolment type | |
| Full-time (n = 20) | 90.9 |
| Part-time (n = 2) | 9.1 |
| Grocery shopping | |
| Myself (n = 5) | 22.7 |
| Parents/partner/housemate (n = 16) | 72.7 |
| Homestay/residential college (n = 1) | 4.5 |
| Baseline | 3-Months | 6-Months | 9-Months | 12-Months | Time, | Sex, | Time X sex, p | |
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | p | p | ||
| Anthropometry | ||||||||
| Weight, kg | 65.0 ± 19.2 | 66.0 ± 19.8 a | 65.8 ± 19.7 | 65.4 ± 19.9 | 65.1 ± 20.1 | 0.723 | 0.115 | 0.467 |
| M (n = 5) | 78.3 ± 30.1 | 77.6 ± 30.8 | 77.7 ± 29.5 | 76.7 ± 28.0 | 78.2 ± 28.4 | |||
| F (n = 17) | 61.1 ± 13.6 | 62.6 ± 15.0 a | 62.4 ± 15.3 | 62.1 ± 16.5 | 61.2 ± 16.1 | |||
| Body fat, % | 24.0 ± 9.2 | 25.3 ± 10.4 | 24.3 ± 9.6 | 24.0 ± 9.2 | 24.2 ± 9.2 | 0.199 | 0.033 * | 0.381 |
| M (n = 5) | 16.9 ± 9.1 | 19.3 ± 15.5 | 16.4 ± 9.1 | 16.2 ± 9.1 a | 17.5 ± 8.7 | |||
| F (n = 17) | 26.1 ± 8.4 | 27.0 ± 8.3 a | 26.6 ± 8.7 | 26.2 ± 8.1 | 26.2 ± 8.6 | |||
| Waist, cm | 75.2 ± 13.2 | 76.8 ± 12.2 | 76.4 ± 12.8 | 75.9 ± 12.9 | 76.0 ± 13.2 | 0.855 | 0.167 | 0.235 |
| M (n = 5) | 83.9 ± 17.8 | 82.2 ± 19.0 | 82.7 ± 18.4 | 82.3 ± 17.5 | 83.9 ± 17.1 | |||
| F (n = 17) | 72.7 ± 10.9 | 75.2 ± 9.6 a | 74.6 ± 10.7 | 74.0 ± 11.1 | 73.7 ± 11.4 | |||
| Hip, cm | 97.9 ± 11.9 | 99.1 ± 12.2 | 99.3 ± 12.8 | 98.2 ± 13.3 | 97.3 ± 13.3 | 0.591 | 0.698 | 0.31 |
| M (n = 5) | 100.7 ± 12.8 | 12.2 ± 12.6 | 100.1 ± 13.2 | 100.0 ± 11.7 | 100.5 ± 11.4 | |||
| F (n = 17) | 97.1 ± 11.9 | 98.7 ± 12.5 | 99.1 ± 13.1 | 97.6 ± 14.0 | 96.3 ± 14.0 | |||
| Dietary intake | ||||||||
| Energy intake, kJ | 8915 ± 2437 | 9245 ± 2978 | 8532 ± 2862 | 7679 ± 2393 a | 7606 ±2060 a | 0.073 | 0.001 *** | 0.83 |
| M (n = 5) | 10339 ± 3687 | 11969 ± 2575 | 10825 ± 1822 | 9305 ± 3513 | 9584 ± 2465 | |||
| F (n = 17) | 8496 ± 1892 | 8444 ± 2643 | 7857 ± 2791 | 7201 ± 1834 a | 7024 ± 1572 a | |||
| Protein intake, g | 85.3 ± 31.5 | 94.9 ± 32.7 | 90.3 ± 32.5 | 79.0 ± 29.9 | 83.0 ± 30.7 | 0.095 | 0.126 | 0.568 |
| M (n = 5) | 91.5 ± 34.7 | 115.9 ± 31.1 a | 113.9 ± 18.2 | 85.2 ± 35.0 | 96.3 ± 31.9 | |||
| F (n = 17) | 83.5 ± 31.3 | 88.7 ± 31.3 | 83.5 ± 32.9 | 77.1 ± 29.2 | 79.1 ± 30.1 | |||
| Fat intake, g | 85.3 ± 29.2 | 82.3 ± 27.7 | 74.4 ± 25.8 | 65.9 ± 23.0 a | 64.5 ± 20.1 a | 0.031 * | 0.184 | 0.99 |
| M (n = 5) | 96.6 ± 46.1 | 89.1 ± 33.2 | 84.0 ± 13.1 | 71.0 ± 32.7 | 71.1 ± 16.2 | |||
| F (n = 17) | 81.9 ± 23.1 | 80.3 ± 26.8 | 71.6 ± 28.2 | 64.4 ± 20.5 a | 62.5 ± 21.1 a | |||
| Saturated fat intake, g | 30.7 ± 10.4 | 30.7 ± 11.9 | 26.9 ± 12.6 | 23.3 ± 8.5 a | 23.1 ± 9.4 a | 0.083 | 0.128 | 0.983 |
| M (n = 5) | 34.3 ± 13.1 | 33.9 ± 13.4 | 31.4 ± 11.2 | 25.1 ± 10.5 | 28.0 ± 5.3 | |||
| F (n = 17) | 29.7 ± 9.6 | 29.7 ± 11.6 | 25.6 ± 12.9 | 22.8 ± 8.2 a | 21.7 ± 10.0 a | |||
| CHO intake, g | 242.2 ± 77.4 | 260.6 ± 111.4 | 240.0 ± 91.6 | 218.5 ± 81.8 | 211.5 ± 80.9 | 0.122 | <0.001 *** | 0.445 |
| M (n = 5) | 290.8 ± 103.0 | 385.6 ± 108.1 | 329.4 ± 80.7 | 292.5 ± 109.3 | 299.1 ± 120.8 | |||
| F (n = 17) | 227.9 ± 65.3 | 223.8 ± 84.0 | 213.8 ± 78.4 | 196.7 ± 59.8 | 185.8 ± 42.9 a | |||
| Sugar intake, g | 96.1 ± 34.0 | 90.1 ± 35.9 | 87.9 ± 30.6 | 84.4 ± 35.2 | 71.0 ± 27.7 a | 0.028 * | 0.081 | 0.397 |
| M (n = 5) | 113.8 ± 51.1 | 122.1 ± 18.9 | 92.5 ± 31.4 | 98.6 ± 43.4 | 78.0 ± 32.2 | |||
| F (n = 17) | 90.9 ± 27.1 | 80.7 ± 34.5 | 86.6 ± 31.2 | 80.2 ± 32.7 | 69.0 ± 26.9 a | |||
| Sodium, mg | 2440 ± 767 | 3029 ± 1558 | 2827 ± 1449 | 2673 ± 2140 | 2542 ± 953 | 0.115 | −0.042 * | 0.241 |
| M (n = 5) | 2775 ± 959 | 4717 ± 1344 a | 3673 ± 1134 | 3063 ± 1994 | 3219 ± 406 | |||
| F (n = 17) | 2341 ± 704 | 2532 ± 1258 | 2579 ± 1465 | 2558 ± 2226 | 2342 ± 983 | |||
| Physical activity | ||||||||
| PA, MET mins | 3704 ± 3260 | 2896 ± 2301 | 4824 ± 3479 | 5897 ± 9910 | 3770 ± 1840 | 0.265 | 0.258 | 0.645 |
| M (n = 5) | 5985 ± 2197 | 3688 ± 1782 | 7481 ± 3531 | 7282 ± 8787 | 3989 ± 1270 | |||
| F (n = 17) | 3033 ± 3263 | 2662 ± 2430 | 4042 ± 3149 | 5490 ± 10432 | 3705 ± 2005 | |||
| Sitting time, min/wk | 2360 ± 912 | 2527 ± 1095 | 2729 ± 1007 | 2340 ± 1066 | 2663 ± 1070 | 0.09 | 0.827 | 0.037 * |
| M (n = 5) | 1944 ± 757 | 2172 ± 1170 | 2712 ± 1187 | 2676 ± 1383 | 3444 ± 1209 a | |||
| F (n = 17) | 2483 ± 937 | 2631 ± 1086 | 2734 ± 989 | 2241 ± 983 | 2434 ± 944 | |||
| Basal metabolic rate | ||||||||
| BMR, kcal/d | 1392 ± 376 | Not measured | Not measured | Not measured | 1293 ± 338 | 0.001 *** | 0.003 ** | 0.062 |
| M (n = 5) | 1817 ± 458 | 1613 ± 503 | ||||||
| F (n = 16) | 1259 ± 230 | 1193 ± 201 | ||||||
| Eating behaviours | ||||||||
| Restraint | 8.2 ± 5.1 | 8.0 ± 5.7 | 7.2 ± 5.4 | 7.7 ± 5.3 | 7.4 ± 5.0 | 0.347 | 0.159 | 0.722 |
| M (n = 5) | 6.2 ± 3.6 | 5.0 ± 2.1 | 4.6 ± 2.7 | 4.2 ± 1.6 | 4.4 ± 1.5 | |||
| F (n = 16) | 8.8 ± 5.4 | 8.9 ± 6.1 | 7.9 ± 5.9 | 8.7 ± 5.6 | 8.3 ± 5.4 | |||
| Hunger | 5.5 ± 3.1 | 5.8 ± 3.5 | 6.0 ± 3.6 | 5.8 ± 3.1 | 5.5 ± 3.6 | 0.671 | 0.013 * | 0.548 |
| M (n = 5) | 8.0 ± 2.9 | 8.8 ± 3.6 | 9.4 ± 3.8 | 8.2 ± 3.1 | 9.0 ± 4.3 | |||
| F (n = 16) | 4.8 ± 2.8 | 4.9 ± 3.0 | 5.0 ± 3.0 | 5.1 ± 2.9 | 4.5 ± 2.8 | |||
| Disinhibition | 5.6 ± 2.4 | 6.0 ± 2.6 | 6.0 ± 3.1 | 5.4 ± 2.6 | 5.3 ± 2.8 | 0.264 | 0.879 | 0.19 |
| M (n = 5) | 5.6 ± 2.4 | 5.2 ± 3.3 | 7.0 ± 4.4 | 4.6 ± 3.4 | 5.2 ± 3.8 | |||
| F (n = 16) | 5.6 ± 2.5 | 6.3 ± 2.5 | 5.6 ± 2.6 | 5.7 ± 3.4 | 5.3 ± 2.6 |
| Food Group | AGHE Serving Size | Baseline | 6-Months | 12-Months | Time p | Interaction p | |||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||||
| Bread and cereals | 30–125 g | 3.9 | 2.4 | 3.5 | 1.8 | 3.5 | 1.8 | 0.844 | 0.268 |
| Fruit | 150 g | 0.9 | 1.1 | 0.8 | 0.7 | 0.5 | 0.6 | 0.205 | 0.428 |
| Processed fruit | 30 g/125 mL | 0.5 | 0.8 | 0.4 | 0.6 | 0.2 | 0.5 | 0.351 | 0.173 |
| Fresh/frozen veg | 75 g | 2.8 | 2.3 | 3 | 2.2 | 2.6 | 2 | 0.864 | 0.571 |
| Canned veg | 75 g | 0.2 | 0.4 | 0.2 | 0.4 | 0.3 | 0.5 | 0.847 | 0.468 |
| Legumes | 150 g | 0.1 | 0.2 | 0.1 | 0.2 | 0 | 0.1 | 0.407 | 0.07 |
| Milk and alternatives | 40–250 g/mL | 1.1 | 0.9 | 1 | 0.7 | 1 | 0.8 | 0.894 | 0.734 |
| Low-fat milk | 40–250 g/mL | 0.3 | 0.6 | 0.2 | 0.3 | 0.2 | 0.3 | 0.129 | 0.743 |
| Meat and alternatives | 65–80 g | 0.4 | 0.7 | 0.6 | 0.7 | 0.6 | 0.4 | 0.49 | 0.609 |
| Fatty meat | 60 g (processed)-65 g | 0.2 | 0.3 | 0.3 | 0.6 | 0.1 | 0.2 | 0.389 | 0.464 |
| Lean meat/poultry | 65 g lean/80 g poultry | 1 | 1.2 | 0.9 | 0.8 | 1.1 | 1.6 | 0.978 | 0.152 |
| Fish and seafood | 100 g | 0.3 | 0.4 | 0.4 | 0.5 | 0.2 | 0.3 | 0.108 | 0.134 |
| Eggs | 2 large eggs (120 g) | 0.2 | 0.3 | 0.1 | 0.2 | 0.1 | 0.2 | 0.14 | 0.566 |
| Nuts and seeds | 30 g | 0.2 | 0.4 | 0.2 | 0.4 | 0.2 | 0.4 | 0.792 | 0.596 |
| Unsaturated oils | 5 g | 2.5 | 3.2 | 1.8 | 1.9 | 1.7 | 1.8 | 0.293 | 0.255 |
| Alcohol | 100 mL wine 285 mL full strength beer 60 mL port or sherry 30 mL spirits | 0.2 | 0.6 | 0.1 | 0.3 | 0.2 | 0.4 | 0.309 | 0.079 |
| Discretionary sweet | 600 kJ | 2.1 | 1.4 | 1.7 | 1.9 | 1 | 1 | 0.026 * | 0.972 |
| Discretional savoury | 600 kJ | 2.4 | 2.1 | 2.2 | 2.3 | 1.9 | 2.2 | 0.587 | 0.582 |
| Soft drink | 375 mL | 0.2 | 0.5 | 0.3 | 0.5 | 0.4 | 0.6 | 0.345 | 0.947 |
| Water | 2600 mL | 1360 | 627 | 1101 | 811 | 1228 | 903 | 0.069 | 0.96 |
| Tea/Coffee | Not stated | 99 | 210 | 71 | 280 | 109 | 249 | 0.298 | 0.903 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilson, N.A.; Villani, A.; Tan, S.-Y.; Mantzioris, E. UniStArt: A 12-Month Prospective Observational Study of Body Weight, Dietary Intake, and Physical Activity Levels in Australian First-Year University Students. Biomedicines 2022, 10, 2241. https://doi.org/10.3390/biomedicines10092241
Wilson NA, Villani A, Tan S-Y, Mantzioris E. UniStArt: A 12-Month Prospective Observational Study of Body Weight, Dietary Intake, and Physical Activity Levels in Australian First-Year University Students. Biomedicines. 2022; 10(9):2241. https://doi.org/10.3390/biomedicines10092241
Chicago/Turabian StyleWilson, Nina A., Anthony Villani, Sze-Yen Tan, and Evangeline Mantzioris. 2022. "UniStArt: A 12-Month Prospective Observational Study of Body Weight, Dietary Intake, and Physical Activity Levels in Australian First-Year University Students" Biomedicines 10, no. 9: 2241. https://doi.org/10.3390/biomedicines10092241
APA StyleWilson, N. A., Villani, A., Tan, S.-Y., & Mantzioris, E. (2022). UniStArt: A 12-Month Prospective Observational Study of Body Weight, Dietary Intake, and Physical Activity Levels in Australian First-Year University Students. Biomedicines, 10(9), 2241. https://doi.org/10.3390/biomedicines10092241









