Abstract
Apixaban can significantly prevent stroke events in patients with non-valvular atrial fibrillation (NVAF), as can be observed from the large, randomized, controlled trial conducted in the present study. However, the real-world evidence of bleeding events related to the apixaban plasma levels in Asian populations is limited. This study aimed to investigate the apixaban plasma levels and clinical outcomes among NVAF patients receiving apixaban, including determining the risk factors associated with bleeding during routine care. Seventy-one patients were included in the study. The median values were 112.79 (5–95th percentiles: 68.69–207.8) μg/L and 185.62 (5–95th percentiles: 124.06–384.34) μg/L for the apixaban trough (Ctrough) and apixaban peak plasma levels (Cpeak), respectively. Stroke and bleeding were found in 8 (11.27%) and 14 patients (19.72%), respectively. There was no statistical significance for Ctrough and Cpeak in the stroke and non-stroke groups, respectively. The median of Ctrough (139.15 μg/L) in patients with bleeding was higher than that in the non-bleeding group (108.14 μg/L), but there was no statistical significance. However, multivariate analyses showed that bleeding history (odds ratio (OR): 17.62; 95% confidence interval (CI): 3.54–176.64; and p-value = 0.002) and Ctrough (OR: 1.01; 95%: CI 1.00–1.03; and p-value = 0.038) were related to bleeding events. Almost all of the patients presented apixaban plasma levels within the expected range. Interestingly, bleeding events were associated with the troughs of the apixaban plasma levels and bleeding history.
1. Introduction
Apixaban is a non-vitamin-K antagonist oral anticoagulant (NOAC) used in stroke prevention for patients with non-valvular atrial fibrillation (NVAF) as a long-term form of treatment [1]. Current clinical practice guidelines strongly recommend the use of apixaban over warfarin, because large, randomized, controlled trials proved the net clinical benefit of these drugs in terms of their efficacy and safety [2,3]. Furthermore, apixaban has presented many advantages compared with warfarin, including rapid onset–offset, convenient dosing, predictable dose–response properties, few drug interactions, no requirement for international normalized ratio monitoring, and less frequent follow-up treatments [4].
Several studies have reported that apixaban is more effective in preventing stroke events or systemic embolism than warfarin in Asian and non-Asian patients with NVAF [5,6]. However, some studies determined that Asians have a higher exposure to apixaban than non-Asians, which could increase the bleeding risk in the former population because of genetic polymorphisms [7,8]. Apixaban is a P-glycoprotein (P-gp) substrate that is encoded by the ATP-binding cassette subfamily B member 1 (ABCB1) gene and presents inter-individual variability [9]. Previous studies have shown that ABCB1 alters the apixaban plasma levels, especially Cpeak [10], whereas apixaban activity can, at present, be measured as the anti-FXa activity and apixaban plasma level. Moreover, the therapeutic range of apixaban plasma levels is defined by the expected drug levels in clinical trials [7,11]. Subsequently, several studies have reported intra- and inter-individual variabilities in apixaban peak and trough concentrations, and that the apixaban concentrations were not associated with the clinical outcomes [12,13]. However, the real-world evidence of the related clinical outcomes of apixaban plasma levels in Caucasian and Asian populations is limited.
Consequently, this study aimed to investigate the clinical outcomes among NVAF patients in real-life clinical practice receiving apixaban, and the risk factors associated with bleeding events, especially the apixaban plasma levels.
2. Materials and Methods
2.1. Study Design and Patients
This study was a single-center, prospective cohort study conducted from January 2021 to January 2022 on patients who received apixaban in the Ambulatory Department of Phramongkutklao Hospital, a tertiary care hospital in Bangkok, Thailand. The study protocol was approved by the Institutional Review Board of the Royal Thai Army Medical Department and Phramongkutklao Hospital (Issued No.: Q021h/63).
Eligible patients were recruited with the following inclusion criteria: age ≥ 18 years with NVAF, receiving the appropriate dose of apixaban, and receiving apixaban continuously for at least seven days. All patients provided written informed consent before joining the study and were assessed for apixaban adherence at least seven days before enrollment via telephone and the pill-count method. The exclusion criteria were moderate-to-severe mitral valve stenosis, mechanical valve replacement, Child–Pugh class C of chronic liver disease, end-stage renal disease, pregnancy, breastfeeding, inability to care for themselves without a caregiver, poor adherence to medication, and receiving an inappropriate dose of apixaban.
2.2. Primary and Secondary Outcomes
The primary outcomes were the apixaban plasma levels and low-molecular-weight heparin (LMWH)-calibrated anti-Factor Xa (anti-FXa) activity at trough and peak concentrations. The expected ranges of the apixaban plasma levels were defined as 69–321 μg/L and 34–230 μg/L for Cpeak and Ctrough, respectively [7,11]. The secondary outcomes were analyzed as follows: (1) stroke and bleeding events: stroke defined as ischemic and hemorrhagic strokes, including a definition of bleeding that was based on the criteria of the International Society on Thrombosis and Haemostasis (ISTH) (major bleeding was defined in nonsurgical patients as fatal bleeding, symptomatic bleeding in a critical area or organ, and/or bleeding causing a decline in the hemoglobin levels of 2 g/dL or more, or leading to the transfusion of two or more units of whole blood or red cells; minor bleeding was defined as “non-major bleeding”) [14]; (2) relationship between the clinical factors and bleeding outcomes; and (3) the correlation between the apixaban plasma levels and LMWH-calibrated anti-FXa activities.
2.3. Measurement of Apixaban Plasma Levels and Anti-FXa Activities
The steady-state apixaban plasma levels and anti-FXa activities were measured at their peak and trough concentrations by a chromogenic anti-FXa assay. Blood samples were collected at the peak and trough measurements. The current study defined the trough time as the time immediately preceding apixaban intake and the peak time as 2–4 h following the administration of the apixaban dose. Blood samples were collected into two 3.2% citrated tubes to determine both the trough and peak concentrations. The samples were centrifuged immediately for 15 min at 2500–3000× g [15,16]. Subsequently, the anti-FXa activity of the samples was measured using a chromogenic anti-FXa assay. Anti-FXa activity was determined using a BiophenTM heparin LRT kit (Hyphen BioMed, Neuville-sur-Oise, France) and analyzed using a Sysmex CS 2500 System (Siemens Health Care, Milan, Italy). The anti-FXa activity results obtained from the chromogenic assay were converted into commercial apixaban (sensitivity range: 0–600 μg/L) and LMWH units (sensitivity range: 0–1.75 IU/mL) [16].
2.4. Statistical Analysis
Statistical analysis was performed using the Statistical Package of the Social Sciences Statistics version 27.0. (IBM Corp, Armonk, NY, USA). The baseline characteristics, apixaban plasma levels, and anti-FXa activities were analyzed using descriptive statistics. Categorical variables were presented as frequencies with percentages. Conversely, continuous variables were tested for normality following the Kolmogorov–Smirnov test and then reported as the means ± standard deviations (SDs) or medians with the 5th and 95th percentiles or interquartile ranges (IQRs). Student’s t-test or the Mann–Whitney U test were used to measure the continuous variables based on normally distributed continuous variables. More than two groups were analyzed using one-way ANOVA or the Kruskal–Wallis test.
The correlation between the apixaban plasma levels and clinical factors was analyzed using Spearman’s rank (ρ) and point biserial correlation (rbp).
The association between bleeding events and apixaban levels higher than the expected ranges was analyzed using chi-squared or Fisher’s exact tests. Consequently, logistic regression was used to predict any bleeding events.
The relationship between the apixaban plasma levels and LMWH-calibrated anti-FXa activities was analyzed using Spearman’s rank correlation (ρ) and simple linear regression. Statistical significance was considered at a p-value of <0.05.
3. Results
3.1. Baseline Characteristics of Patients
The baseline characteristics of all of the patients are presented in Table 1. Seventy-one patients were enrolled in this study. The mean age was 75.0 ± 10.5 years, and 36.6% of the patients were older than 80 years. Sixty-nine percent were male. More than half of the patients were >60 kg. The mean body weight was 67.3 ± 13.5 kg and the mean body mass index (BMI) was 24.61 ± 3.92 kg/m2. The median serum creatinine (SCr) was 1.1 mg/dL (IQR 0.9–1.4 mg/dL), and the mean creatinine clearance (CrCl) was 54.1 ± 22.0 mL/min. The majority of the patients had a moderate risk of stroke, the median value of the CHA2DS2-VASc score was 4 points (IQR 3–5), and the median value of the HAS-BLED score for bleeding risk was 2 points (IQR1–3). Forty percent had previously documented bleeding events. The most frequently reported sites of bleeding were the gastrointestinal tract (23.9%), cerebrovascular area (5.6%), urinary tract (5.6%), skin (4.3%), and oral cavity (2.8%). Hypertension (83.3%), dyslipidemia (70.4%), and anemia (42.3%) were the three most common comorbidities.

Table 1.
Baseline characteristics for all patients.
3.2. Steady-State Apixaban Plasma Levels and Anti-FXa Activities
The median times for the peak and trough plasma levels were 3.0 and 12.3 h, respectively. The median values (5th–95th percentiles) for the apixaban plasma levels were 112.79 (68.69–207.82) μg/L and 185.62 (124.06–384.34) μg/L at Ctrough and Cpeak, respectively. Additionally, the trough (Xatrough) and peak (Xapeak) anti-FXa activities were 1.23 (0.59–2.21) IU/mL and 2.10 (1.44–3.11) IU/mL, respectively.
A total of 71 patients were divided into standard-dose (n = 46) and reduced-dose groups (n = 25). The apixaban plasma levels of the patients in the standard-dose group were 110.81 (63.08–249.01) μg/L and 205.44 (125.18–412.31) μg/L at Ctrough and Cpeak, respectively. Xatrough and Xapeak were 1.23 (0.73–2.44) IU/mL and 2.21 (1.61–3.16) IU/mL, respectively. In contrast, no significant differences in the apixaban plasma level and anti-FXa activity at the peak and trough concentrations were observed between the standard- and reduced-dose groups. The steady-state apixaban plasma levels and anti-FXa activities are presented in Table 2.

Table 2.
The trough and peak values of the apixaban plasma levels and anti-FXa activities at steady state.
We defined the expected range of the apixaban plasma concentrations as 34–230 μg/L at the trough and 69–321 μg/L at the peak levels, respectively [7,11]. Ninety-six percent of the patients had Ctrough within the expected range, whereas 4% exceeded the expected range. The proportions of patients with Cpeak within and above the expected range were 90% and 10%, respectively.
For the correlation between the apixaban plasma levels and clinical factors, only CrCl (correlation coefficient, ρ = −0.27; p-value < 0.024) and concomitant drugs with CYP3A4 or P-gp inhibitors (rpb = 0.32; p-value < 0.006) were used as predictors of the apixaban trough plasma levels, whereas there was no correlation between the apixaban peak plasma levels and any other factors.
3.3. Stroke and Bleeding Events
Stroke and bleeding events were observed for one year. The trough and peak values of the apixaban plasma levels classified by stroke are also summarized in Table 3. Stroke events were observed in eight patients (11.27%), five patients were classified as having an ischemic stroke (7.04%), and three patients (4.22%) were classified as having a hemorrhagic stroke. The median value of Ctrough was 146.24 (IQR 92.24, 163.22) μg/L in the stroke group and 111.48 (IQR 89.61, 156.92) μg/L in the non-stroke group, but the difference was not statistically significant (p-value = 0.604). Moreover, the median values of Cpeak in the stroke group were 200.52 (IQR 161.61, 259.50) μg/L and 183.05 (IQR 146.00, 249.74) μg/L (p-value = 0.834). Overall bleeding events were observed in fourteen patients (19.7%) and classified by severity as major bleeding in six patients (8.5%) and minor bleeding in eight patients (11.3%). Most cases of major bleeding involved the gastrointestinal tract. The median values of Ctrough were 139.15 (IQR 109.49, 163.16) μg/L in the bleeding group and 108.14 (IQR 87.23, 160.59) μg/L in the non-bleeding group, with no significant differences (p-value = 0.126). The median values of Cpeak were 209.32 (IQR 145.23, 285.45) μg/L in the bleeding group and 183.05 (IQR 147.08, 247.03) μg/L in the non-bleeding group, with no significant differences (p-value = 0.470). The median values of Ctrough in the minor, major, and non-bleeding groups were 149.46 (IQR 117.42, 172.89) μg/L, 123.95 (IQR 93.81–139.19) μg/L, and 108.14 (IQR 87.23–160.59) μg/L, respectively, with no significant differences (p-value = 0.148). The median values of Cpeak in the minor, major, and non-bleeding groups were 269.30 (IQR 157.83, 317.69) μg/L, 178.66 (IQR 137.49–209.76) μg/L, and 183.05 (IQR 147.08–247.03) μg/L, respectively, with no significant differences (p-value = 0.330). The trough and peak values of the apixaban plasma levels classified by bleeding events are also presented in Table 4.

Table 3.
The trough and peak values of the apixaban plasma levels classified by stroke events.

Table 4.
The trough and peak values of the apixaban plasma levels classified by bleeding events.
3.4. Relationship between Clinical Factors and Clinical Events
Based on the univariate analysis, there were eight factors that exerted potential effects on bleeding events, including hypertension, renal dysfunction, stroke, older age, drugs, alcohol, and the apixaban plasma level. The results of the univariate analysis suggest that the bleeding history is only one factor that is significant for increasing bleeding risk (OR 13.00; 95% CI 2.63–64.24; p-value = 0.002). As shown in Table 5, the multivariate analysis results demonstrated that the bleeding history (OR 17.62; 95% CI 3.54–176.64; p-value = 0.002) and Ctrough (OR 1.01; 95% CI 1.00–1.03; p-value = 0.038) values are significantly related to bleeding events, while Cpeak (OR 1.01; 95% CI 1.00, 1.02; p-value = 0.050) exhibited no significant difference in terms of bleeding events.

Table 5.
Multivariate analysis of the apixaban plasma levels related to bleeding events.
Additionally, in the univariate analysis, there were eight factors that exerted potential effects on stroke events, including hypertension, heart failure, previous stroke events, older age, vascular disease, diabetes mellitus, the CHA2DS2VASC score, and the apixaban plasma level. The results reveal that the CHA2DS2VASC score (OR 1.90; 95% CI 1.15–3.14; p-value = 0.013) is significantly related to stroke events. Unfortunately, the multivariate analysis results do not demonstrate any factors that exhibited significant differences in terms of stroke events.
3.5. Correlation between Apixaban Plasma Level and LMWH-Calibrated Anti-FXa Activity
The scatterplots (Figure 1) show a strong, positive linear relationship between the apixaban plasma levels and LMWH-calibrated anti-FXa activities, as confirmed by Spearman’s correlation coefficient. A statistically significant correlation was observed between Ctrough and Xatrough (correlation coefficient, ρ = 0.95; p-value < 0.001). Similarly, Cpeak was significantly correlated with Xapeak (ρ = 0.96, p-value < 0.001). In this study, a simple linear regression analysis was performed for the studied participants. The significant relationship between Ctrough and Xatrough (R2 = 0.86, p-value < 0.001) presented the following regression equation for the prediction of Ctrough:
Ctrough = 87.21 (Xatrough)
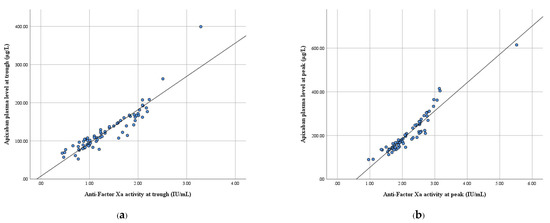
Figure 1.
Scatterplot between the apixaban plasma level and anti-FXa activity. (a) At the trough and (b) at the peak.
Likewise, Cpeak and Xapeak were significantly related (R2 = 0.90, p-value < 0.001), and the regression equation for Cpeak’s prediction of Cpeak is as follows:
Cpeak = 129.48 (Xapeak) − 75.47
From the analysis, it can be observed that the slopes of the equation were different for Ctrough and Cpeak. The scatterplots between the overall apixaban plasma levels (Call) and anti-FXa activities (Xaall) presented a curvilinear pattern. Therefore, the apixaban plasma levels were adjusted using a logarithmic scale. The simple linear regression was re-analyzed, and the equation was as follows:
ln (Call) = (0.58) Xaall + 3.99 (R2 = 0.91, p-value < 0.001)
4. Discussion
Our study aimed to investigate the apixaban plasma levels and clinical outcomes among Thai patients with NVAF who received apixaban as a form of medication. Approximately 90% of patients presented Ctrough and Cpeak within the expected range at the 5th–95th percentiles based on clinical practice guidelines [11]. The median values of the apixaban plasma levels were similar for Ctrough and Cpeak, but slightly higher and lower when compared with the results obtained from Korean and Taiwanese patients [17,18]. In addition, the median values of Ctrough and Cpeak in the standard- and reduced-dose groups in the present study were lower and higher than the data obtained from the ARISTOTLE-J study, respectively [19]. Similarly, previous pharmacokinetic studies reported that apixaban exposure was 17.7% and 4.5% higher in Japanese and other Asian people, respectively [7]. However, the exposure to apixaban decreased by 3.2% in the Korean population [7].
The reduced-dose group showed a 10% higher median Ctrough value and an 18% lower median Cpeak value than the standard-dose group. However, the differences in the median values of Cpeak and Ctrough were not statistically significant in the standard- and reduced-dose groups. A previous study reported that the median values of Ctrough and Cpeak were approximately 25–30% lower in the reduced-dose group than in the standard-dose group [7]. Similar to the previous real-life studies, the results showed a 25–35% difference in Ctrough and Cpeak between the standard- and reduced-dose groups [9,12,20]. The results for the reduced-dose group presented a pharmacokinetic alteration, but the clinical outcomes were consistent in terms of efficacy and safety [21]. Interestingly, apixaban dose adjustment based on clinical practice guidelines among Thai patients with NVAF was maintainable within the expected range [11]. In this study, anti-FXa activity was slightly higher than that recorded in the data in a previous study conducted in Japan [22], since our study perhaps included some patients who concomitantly received CYP3A4 or P-gp inhibitors.
In addition, a previous study reported that apixaban concomitant with CYP3A or P-gp inhibitor drugs was not related to higher plasma levels in patients with AF [23]. However, our study presented a positive correlation between the concomitant CYP3A or P-gp inhibitor drugs and Ctrough. Amiodarone and dronedarone are moderate CYP3A4 and P-gp inhibitors that may increase the apixaban plasma levels [24,25]. These results conform to the results obtained from a previous pharmacokinetic study that suggested that strong to moderate CYP3A and P-gp inhibitors affect the AUC and apixaban plasma levels [26]. Furthermore, approximately 27% of apixaban was excreted unchanged by the kidneys. This pharmacokinetic finding illustrates that the impact of renal impairment on apixaban exposure is modest [27]. A regression analysis showed that AUC0–∞ was inversely related to apixaban clearance in renal impairment compared with healthy volunteers with normal renal functions [7,28]. Testa et al. provided data from a real-world study that determined that CrCl was poorly correlated with the apixaban plasma levels [9]. Similar to the present study, they observed a weak inverse correlation between CrCl and the trough apixaban plasma levels.
As the results of our study show, almost every patient had peak and trough apixaban plasma levels in the expected therapeutic range. It is noteworthy that the apixaban plasma levels in the stroke group had a higher trend than the non-stroke group, but no apixaban plasma levels were below the expected therapeutic range. Unlike in previous studies, the results revealed that the apixaban plasma levels were below the expected trough concentrations in 25–27% of patients affected by stroke events [29,30]. One potential explanation for why the apixaban plasma levels in the stroke group were higher than those in the non-stroke group may be related to low CrCl concomitant with amiodarone. Interestingly, all stroke cases in our study had previously suffered from stroke events in six to eight octogenarian patients. A history of stroke events and age ≥ 75 years were major risk factors for stroke events in AF patients [31]. As mentioned above, it may be that the apixaban plasma levels cannot be used to predict stroke outcomes, as suggested by the previous report [12]. In addition, a cohort study previously reported that thrombotic complications occurred in AF patients who had depleted apixaban plasma levels (22–145 µ/L) and high CHA2DS2VASc scores [32]. Therefore, the apixaban plasma level is the not only factor that predicts stroke outcomes in patients who receive apixaban—other factors, such as a history of stroke, age, hypertension, and diabetes mellitus, should be considered [33].
In the ARISTOTLE trial, a population pharmacokinetic model provided information for predicted apixaban levels in patients with or without bleeding events [34]. The analysis revealed a substantial overlap in the apixaban plasma levels between bleeding severity. The median plasma levels in each group only differed by approximately 15%, which caused difficulty in identifying a therapeutic range [34]. Subsequently, the results of our study are similar to those obtained in a previous study [35]. Explicitly, the bleeding group showed no difference from the non-bleeding group in terms of the median values of Ctrough and Cpeak. Furthermore, the bleeding events were not associated with the expected therapeutic range listed above. However, the real-world pilot prospective study reported significantly higher Ctrough and Cpeak values in the bleeding group compared with the non-bleeding group [36], which is similar to our study. Concomitant with CYP3A4 and P-gp inhibitors, older age was a factor causing high apixaban plasma levels in the bleeding group [37,38]. Many reports demonstrated drug interactions and the effect of age on the apixaban levels [7,26,39].
In addition, we analyzed the model to predict the effects of bleeding history and Ctrough on bleeding events. Similarly, the AVERROES study reported that Ctrough was related to minor bleeding [40]; however, other previous clinical trials showed that the trough NOAC plasma level could predict the risk of bleeding [41,42]. Our study shared some differences from a previous observational study, which was the relationship between the bleeding events and Cpeak [43]. Meanwhile, the present study observed no relationship between Cpeak and bleeding events. At present, studies conducted on the correlation between the apixaban plasma levels and clinical outcomes are limited, since a real-world multicenter study confirmed high NOAC inter-individual variability.
In this study, we used chromogenic anti-FXa assays, and the BiophenTM heparin LRT can be utilized as a surrogate reference standard [16,44]. In addition, the chromogenic anti-FXa assay is the most appropriate method to measure the pharmacodynamics of apixaban because of the strong linear correlation with the apixaban plasma levels [45,46]. Our study consistently observed a significant correlation between the apixaban plasma level and LMWH-calibrated anti-FXa activity. The real-life model in this study predicted that the linear relationships between the apixaban plasma levels and anti-FXa activities were R2 = 0.86 and R2 = 0.90 at the trough and peak, respectively. However, this relationship presented a curvilinear scatter plot between the Call and Xaall, which was similar to the previous studies conducted using chromogenic assays and mass spectrometry [47,48]. All the patients presented anti-FXa activity within the range presented previously [27,49]. However, some patients in this study had apixaban plasma levels above the expected ranges. Thus, the LMWH-calibrated anti-FXa activity interpreted as the action of apixaban may be underestimated for the apixaban level.
It is important to note the limitations of this study. First, the sample size was insufficient to detect the relationship between the apixaban plasma levels and clinical outcomes. Second, minor bleeding events may not have been documented in the medical records, which can cause underreporting, and some cases were analyzed through interviews. Therefore, recall bias was possibly present. Third, we obtained samples at the estimated times at which the apixaban plasma levels were at their peak; at 2–4 h, there were no data available for peak levels for each patient. Finally, our study compared the apixaban plasma levels with the expected range presented in clinical practice guidelines [11]. The exact therapeutic range of the apixaban plasma levels was not defined, while intra-individual variability in the apixaban plasma levels was already reported in another study [9,13].
5. Conclusions
In summary, almost every Thai patient with NVAF was in the unexpected range of peak and trough apixaban plasma levels during all dosage regimens. Our study is the first to investigate the apixaban plasma levels in a developing Asian country and observe that bleeding events are associated with the trough of apixaban plasma level and bleeding history. While stroke events could occur, the apixaban plasma levels were unexpected in the previously described ranges, and it was noticeable that all patients in the stroke group had a history of stroke.
Author Contributions
Conceptualization: S.L. (Sutee Limcharoen), M.P., P.P., S.L. (Sarawuth Limprasert), J.S., and P.B.; methodology: S.L. (Sutee Limcharoen), M.P., P.P., S.L. (Sarawuth Limprasert), J.S., and P.B.; formal analysis: S.L. (Sutee Limcharoen), M.P., P.P., S.L. (Sarawuth Limprasert), J.S., and P.B.; investigation: S.L. (Sutee Limcharoen), J.S., W.S. (Weerayuth Saelim), and P.B.; writing—original draft preparation: S.L. (Sutee Limcharoen) and P.B.; writing—review and editing: S.L. (Sutee Limcharoen), S.L. (Sarawuth Limprasert), J.S., W.S. (Wichai Santimaleeworagun), and P.B.; funding acquisition: S.L. (Sutee Limcharoen) and P.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Doctor Kasem Pangsrivongse Foundation, Thailand, grant no. 02-001-64.
Institutional Review Board Statement
The study protocol was approved by the institutional review board of the Royal Thai Army Medical Department and Phramongkutklao Hospital (approval no. Q021h/63 on 23 December 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
The authors acknowledge the Division of Cardiology, and laboratory support from the Division of Hematology, Department of Internal Medicine, Phramongkutklao Hospital. The authors would also like to thank Nattakrit Tongpoonsakdi (QLS Certificate No. 1603177) for conducting a comprehensive language review of this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Eliquis (Apixaban) Oral Tablets Prescribing Information. Available online: https://packageinserts.bms.com/pi/pi_eliquis.pdf (accessed on 17 November 2021).
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European As-sociation for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar]
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fi-brillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration with the Society of Thoracic Surgeons. Circulation 2019, 140, e125–e151. [Google Scholar]
- Rose, D.K.; Bar, B. Direct Oral Anticoagulant Agents: Pharmacologic Profile, Indications, Coagulation Monitoring, and Reversal Agents. J. Stroke Cerebrovasc. Dis. 2018, 27, 2049–2058. [Google Scholar] [CrossRef]
- Granger, C.B.; Alexander, J.H.; McMurray, J.J.V.; Lopes, R.D.; Hylek, E.M.; Hanna, M.; Al-Khalidi, H.R.; Ansell, J.; Atar, D.; Ave-zum, A.; et al. Apixaban versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2011, 365, 981–992. [Google Scholar] [CrossRef]
- Bang, O.Y.; Hong, K.-S.; Heo, J.H. Asian Patients with Stroke plus Atrial Fibrillation and the Dose of Non-Vitamin K Oral Anticoagulants. J. Stroke 2016, 18, 169–178. [Google Scholar] [CrossRef][Green Version]
- Cirincione, B.; Kowalski, K.; Nielsen, J.; Roy, A.; Thanneer, N.; Byon, W.; Boyd, R.; Wang, X.; Leil, T.; LaCreta, F.; et al. Population Phar-macokinetics of Apixaban in Subjects with Nonvalvular Atrial Fibrillation. CPT Pharmacomet. Syst. Pharmacol. 2018, 7, 728–738. [Google Scholar] [CrossRef]
- Dorji, P.W.; Tshering, G.; Na-Bangchang, K. CYP2C9, CYP2C19, CYP2D6 and CYP3A5 polymorphisms in South-East and East Asian populations: A systematic review. J. Clin. Phar. Ther. 2019, 44, 508–524. [Google Scholar] [CrossRef] [PubMed]
- Testa, S.; Tripodi, A.; Legnani, C.; Pengo, V.; Abbate, R.; Dellanoce, C.; Carraro, P.; Salomone, L.; Paniccia, R.; Paoletti, O.; et al. Plasma levels of direct oral anticoagulants in real life patients with atrial fibrillation: Results observed in four anticoagulation clinics. Thromb. Res. 2015, 137, 178–183. [Google Scholar] [CrossRef]
- Dimatteo, C.; D’Andrea, G.; Vecchione, G.; Paoletti, O.; Tiscia, G.L.; Santacroce, R.; Correale, M.; Brunetti, N.; Grandone, E.; Testa, S.; et al. ABCB1 SNP rs4148738 modulation of apixaban interindividual variability. Thromb. Res. 2016, 145, 24–26. [Google Scholar] [CrossRef] [PubMed]
- Steffel, J.; Collins, R.; Antz, M.; Cornu, P.; Desteghe, L.; Haeusler, K.G.; Oldgren, J.; Reinecke, H.; Roldan-Schilling, V.; Rowell, N.; et al. 2021 European Heart Rhythm Association Practical Guide on the Use of Non-Vitamin K Antagonist Oral Anticoagulants in Patients with Atrial Fibrillation. EP Eur. 2021, 23, 1612–1676. [Google Scholar] [CrossRef] [PubMed]
- Mavri, A.; Vene, N.; Božič-Mijovski, M.; Miklič, M.; Söderblom, L.; Pohanka, A.; Malmström, R.E.; Antovic, J. Apixaban con-centration variability and relation to clinical outcomes in real-life patients with atrial fibrillation. Sci. Rep. 2021, 11, 13908. [Google Scholar] [CrossRef]
- Gulilat, M.; Tang, A.; Gryn, S.E.; Leong-Sit, P.; Skanes, A.C.; Alfonsi, J.E.; Dresser, G.K.; Henderson, S.L.; Rose, R.V.; Lizotte, D.J.; et al. In-terpatient Variation in Rivaroxaban and Apixaban Plasma Concentrations in Routine Care. Can. J. Cardiol. 2017, 33, 1036–1043. [Google Scholar] [CrossRef]
- Schulman, S.; Kearon, C.; The Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J. Thromb. Haemost. 2005, 3, 692–694. [Google Scholar] [CrossRef]
- McGrail, R.; Revsholm, J.; Nissen, P.H.; Grove, E.L.; Hvas, A.-M. Stability of direct oral anticoagulants in whole blood and plasma from patients in steady state treatment. Thromb. Res. 2016, 148, 107–110. [Google Scholar] [CrossRef]
- Gosselin, R.C.; Adcock, D.M.; Bates, S.M.; Douxfils, J.; Favaloro, E.J.; Gouin-Thibault, I.; Guillermo, C.; Kawai, Y.; Lindhoff-Last, E.; Kitchen, S. International Council for Standardization in Haematology (ICSH) Recommendations for Laboratory Measurement of Direct Oral Anticoagulants. Thromb. Haemost. 2018, 118, 437–450. [Google Scholar] [CrossRef]
- Shin, H.; Cho, M.-C.; Kim, R.B.; Kim, C.-H.; Choi, N.-C.; Kim, S.-K.; Koh, E.-H. Laboratory measurement of apixaban using anti-factor Xa assays in acute ischemic stroke patients with non-valvular atrial fibrillation. J. Thromb. Thrombolysis 2017, 45, 250–256. [Google Scholar] [CrossRef]
- Lin, S.; Kuo, C.; Yeh, S.-J.; Tsai, L.; Liu, Y.; Huang, C.; Tang, S.; Jeng, J.-S. Real-World Rivaroxaban and Apixaban Levels in Asian Patients with Atrial Fibrillation. Clin. Pharmacol. Ther. 2019, 107, 278–286. [Google Scholar] [CrossRef]
- Ogawa, S.; Shinohara, Y.; Kanmuri, K. Safety and Efficacy of the Oral Direct Factor Xa Inhibitor Apixaban in Japanese Patients with Non-Valvular Atrial Fibrillation. Circ. J. 2011, 75, 1852–1859. [Google Scholar] [CrossRef]
- Skeppholm, M.; Al-Aieshy, F.; Berndtsson, M.; Al-Khalili, F.; Rönquist-Nii, Y.; Söderblom, L.; Östlund, A.Y.; Pohanka, A.; Antovic, J.; Malmström, R.E. Clinical evaluation of laboratory methods to monitor apixaban treatment in patients with atrial fibrillation. Thromb. Res. 2015, 136, 148–153. [Google Scholar] [CrossRef]
- Zeitouni, M.; Giczewska, A.; Lopes, R.D.; Wojdyla, D.M.; Christersson, C.; Siegbahn, A.; De Caterina, R.; Steg, P.G.; Granger, C.B.; Wallentin, L.; et al. Clinical and Pharmacological Effects of Apixaban Dose Adjustment in the ARISTOTLE Trial. J. Am. Coll. Cardiol. 2020, 75, 1145–1155. [Google Scholar] [CrossRef]
- Osanai, H.; Ajioka, M.; Masutomi, T.; Kuwayama, T.; Ishihama, S.; Sakamato, Y.; Otaka, N.; Sakaguchi, T.; Inoue, Y.; Kanbara, T.; et al. Measurement of Anti-Factor Xa Activity in Patients on Apixaban for Non-Valvular Atrial Fibrillation. Circ. J. 2015, 79, 2584–2590. [Google Scholar] [CrossRef]
- Raccah, B.H.; Rottenstreich, A.; Zacks, N.; Muszkat, M.; Matok, I.; Perlman, A.; Kalish, Y. Drug interaction as a predictor of direct oral anticoagulant drug levels in atrial fibrillation patients. J. Thromb. Thrombolysis 2018, 46, 521–527. [Google Scholar] [CrossRef]
- Iram, F.; Ali, S.; Ahmad, A.; Alam Khan, S.; Husain, A. A review on dronedarone: Pharmacological, pharmacodynamic and pharmacokinetic profile. J. Acute Dis. 2016, 5, 102–108. [Google Scholar] [CrossRef]
- McDonald, M.G.; Au, N.T.; Rettie, A.E. P450-Based Drug-Drug Interactions of Amiodarone and its Metabolites: Diversity of Inhibitory Mechanisms. Drug Metab. Dispos. 2015, 43, 1661–1669. [Google Scholar] [CrossRef]
- Frost, C.E.; Byon, W.; Song, Y.; Wang, J.; Schuster, A.E.; Boyd, R.A.; Zhang, D.; Yu, Z.; Dias, C.; Shenker, A.; et al. Effect of ketoconazole and diltiazem on the pharmacokinetics of apixaban, an oral direct factor Xa inhibitor. Br. J. Clin. Pharmacol. 2014, 79, 838–846. [Google Scholar] [CrossRef]
- Byon, W.; Garonzik, S.; Boyd, R.A.; Frost, C.E. Apixaban: A Clinical Pharmacokinetic and Pharmacodynamic Review. Clin. Pharmacokinet. 2019, 58, 1265–1279. [Google Scholar] [CrossRef]
- Chang, M.; Yu, Z.; Shenker, A.; Wang, J.; Bs, J.P.; Byon, W.; Boyd, R.A.; LaCreta, F.; Frost, C.E. Effect of renal impairment on the pharmacokinetics, pharmacodynamics, and safety of apixaban. J. Clin. Pharmacol. 2015, 56, 637–645. [Google Scholar] [CrossRef]
- Macha, K.; Marsch, A.; Siedler, G.; Breuer, L.; Strasser, E.F.; Engelhorn, T.; Schwab, S.; Kallmünzer, B. Cerebral Ischemia in Patients on Direct Oral Anticoagulants. Stroke 2019, 50, 873–879. [Google Scholar] [CrossRef]
- Rizos, T.; Meid, A.D.; Huppertz, A.; Dumschat, C.; Purrucker, J.; Foerster, K.I.; Burhenne, J.; Czock, D.; Jenetzky, E.; Ringleb, P.A.; et al. Low Exposure to Direct Oral Anticoagulants Is Associated with Ischemic Stroke and Its Severity. J. Stroke 2022, 24, 88–97. [Google Scholar] [CrossRef]
- You, R.X.; McNeil, J.; Farish, S.J.; O’Malley, H.M.; Donnan, G. The influence of age on atrial fibrillation as a risk factor for stroke. Clin. Exp. Neurol. 1991, 28, 37–42. [Google Scholar]
- Testa, S.; Paoletti, O.; Legnani, C.; Dellanoce, C.; Antonucci, E.; Cosmi, B.; Pengo, V.; Poli, D.; Morandini, R.; Testa, R.; et al. Low drug levels and thrombotic complications in high-risk atrial fibrillation patients treated with direct oral anticoagulants. J. Thromb. Haemost. 2018, 16, 842–848. [Google Scholar] [CrossRef]
- Lip, G.Y.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest 2010, 137, 263–272. [Google Scholar] [CrossRef]
- Eikelboom, J.W.; Quinlan, D.J.; Hirsh, J.; Connolly, S.J.; Weitz, J.I. Laboratory Monitoring of Non-Vitamin K Antagonist Oral Anticoagulant Use in Patients with Atrial Fibrillation: A Review. JAMA Cardiol. 2017, 2, 566–574. [Google Scholar] [CrossRef]
- Jakowenko, N.; Nguyen, S.; Ruegger, M.; Dinh, A.; Salazar, E.; Donahue, K.R. Apixaban and rivaroxaban anti-Xa level utili-zation and associated bleeding events within an academic health system. Thromb. Res. 2020, 196, 276–282. [Google Scholar] [CrossRef]
- Škorňová, I.; Samoš, M.; Bolek, T.; Kamenišťáková, A.; Stančiaková, L.; Galajda, P.; Staško, J.; Kubisz, P.; Mokáň, M. Direct Oral Anticoagulants Plasma Levels in Patients with Atrial Fibrillation at the Time of Bleeding: A Pilot Prospective Study. J. Cardiovasc. Pharmacol. 2021, 78, e122–e127. [Google Scholar] [CrossRef]
- Suzuki, S.; Yamashita, T.; Akao, M.; Okumura, K. Clinical implications of assessment of apixaban levels in elderly atrial fibrillation patients: J-ELD AF registry sub-cohort analysis. Eur. J. Clin. Pharmacol. 2020, 76, 1111–1124. [Google Scholar] [CrossRef]
- Milner, E.; Ainsworth, M.; Gleaton, M.; Bookstaver, D. Assessment of Anti-Xa activity in patients receiving concomitant apixaban with strong p-glycoprotein inhibitors and statins. J. Clin. Pharm. Ther. 2022, 47, 668–675. [Google Scholar] [CrossRef]
- Frost, C.E.; Song, Y.; Shenker, A.; Wang, J.; Barrett, Y.C.; Schuster, A.; Harris, S.I.; LaCreta, F. Effects of Age and Sex on the Single-Dose Pharmacokinetics and Pharmacodynamics of Apixaban. Clin. Pharmacokinet. 2015, 54, 651–662. [Google Scholar] [CrossRef]
- Bhagirath, V.C.; Eikelboom, J.W.; Hirsh, J.; Coppens, M.; Ginsberg, J.; Vanassche, T.; Yuan, F.; Chan, N.; Yusuf, S.; Connolly, S.J. Apix-aban-Calibrated Anti-FXa Activity in Relation to Outcome Events and Clinical Characteristics in Patients with Atrial Fibril-lation: Results from the AVERROES Trial. TH Open 2017, 1, e139–e145. [Google Scholar]
- Reilly, P.A.; Lehr, T.; Haertter, S.; Connolly, S.J.; Yusuf, S.; Eikelboom, J.W.; Ezekowitz, M.D.; Nehmiz, G.; Wang, S.; Wallentin, L.; et al. The effect of dabigatran plasma concentrations and patient characteristics on the frequency of ischemic stroke and major bleeding in atrial fibrillation patients: The RE-LY Trial (Randomized Evaluation of Long-Term Anticoagulation Therapy). J. Am. Coll. Cardiol. 2014, 63, 321–328. [Google Scholar] [CrossRef]
- Ruff, C.T.; Giugliano, R.P.; Braunwald, E.; Morrow, D.A.; Murphy, S.A.; Kuder, J.F.; Deenadayalu, N.; Jarolim, P.; Betcher, J.; Shi, M.; et al. Association between edoxaban dose, concentration, anti-Factor Xa activity, and outcomes: An analysis of data from the ran-domised, double-blind ENGAGE AF-TIMI 48 trial. Lancet 2015, 385, 2288–2295. [Google Scholar] [CrossRef]
- Testa, S.; Legnani, C.; Antonucci, E.; Paoletti, O.; Dellanoce, C.; Cosmi, B.; Pengo, V.; Poli, D.; Morandini, R.; Testa, R.; et al. Drug levels and bleeding complications in atrial fibrillation patients treated with direct oral anticoagulants. J. Thromb. Haemost. 2019, 17, 1064–1072. [Google Scholar] [CrossRef] [PubMed]
- Gosselin, R.C.; Adcock, D.M.; Douxfils, J. An update on laboratory assessment for direct oral anticoagulants (DOACs). Int. J. Lab. Hematol. 2019, 41, 33–39. [Google Scholar] [CrossRef]
- Becker, R.C.; Yang, H.; Barrett, Y.; Mohan, P.; Wang, J.; Wallentin, L.; Alexander, J.H. Chromogenic laboratory assays to measure the factor Xa-inhibiting properties of apixaban--an oral, direct and selective factor Xa inhibitor. J. Thromb. Thrombolysis 2011, 32, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Flaujac, C.; Delavenne, X.; Quenet, S.; Horellou, M.-H.; Laporte, S.; Siguret, V.; Lecompte, T.; Gouin-Thibault, I. Assessment of apixaban plasma levels by laboratory tests: Suitability of three anti-Xa assays. Thromb. Haemost. 2014, 111, 240–248. [Google Scholar] [CrossRef]
- Willekens, G.; Studt, J.; Mendez, A.; Alberio, L.; Fontana, P.; Wuillemin, W.A.; Schmidt, A.; Graf, L.; Gerber, B.; Bovet, C.; et al. A universal anti-Xa assay for rivaroxaban, apixaban, and edoxaban measurements: Method validation, diagnostic accuracy and external validation. Br. J. Haematol. 2021, 193, 1203–1212. [Google Scholar] [CrossRef]
- von Horn, H.; Rasmusson, A.; Söderblom, L.; Malmström, R.E.; Antovic, J. Using a low–molecular weight heparin–calibrated anti–factor Xa assay to assess the concentration of apixaban and rivaroxaban. Int. J. Lab. Hematol. 2022, 44, 163–167. [Google Scholar] [CrossRef]
- Heidbuchel, H.; Verhamme, P.; Alings, M.; Antz, M.; Diener, H.-C.; Hacke, W.; Oldgren, J.; Sinnaeve, P.; Camm, A.J.; Kirchhof, P.; et al. Updated European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace 2015, 17, 1467–1507. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).