The Effect of Adverse Surgical Margins on the Risk of Biochemical Recurrence after Robotic-Assisted Radical Prostatectomy
Abstract
:1. Introduction
2. Patients and Methods
2.1. Patient Selection
2.2. Surgical Technique
2.3. Pathology Examination
2.4. Study Covariates and Outcomes
2.5. Statistical Analysis
3. Results
3.1. Descriptive Characteristics
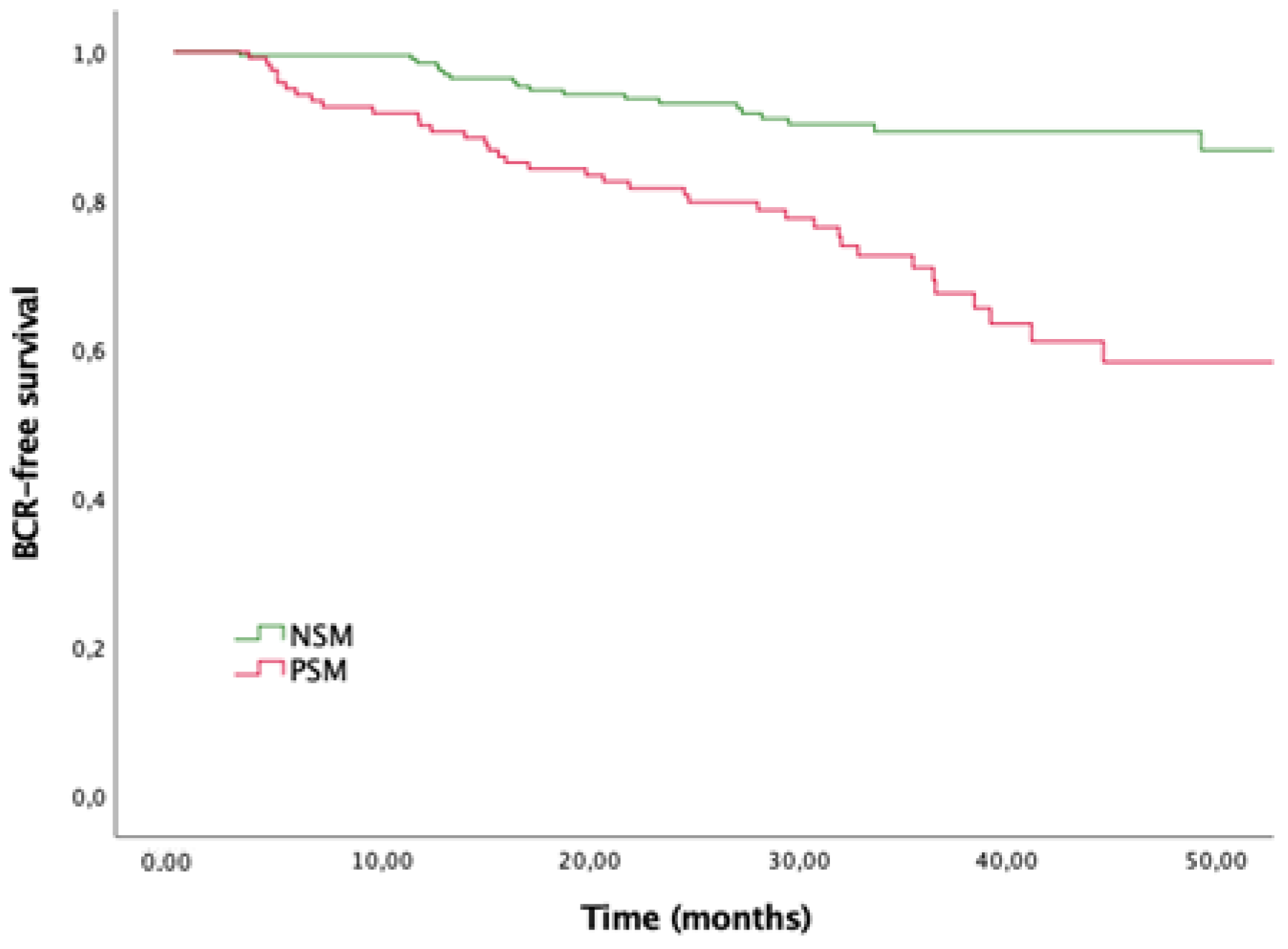
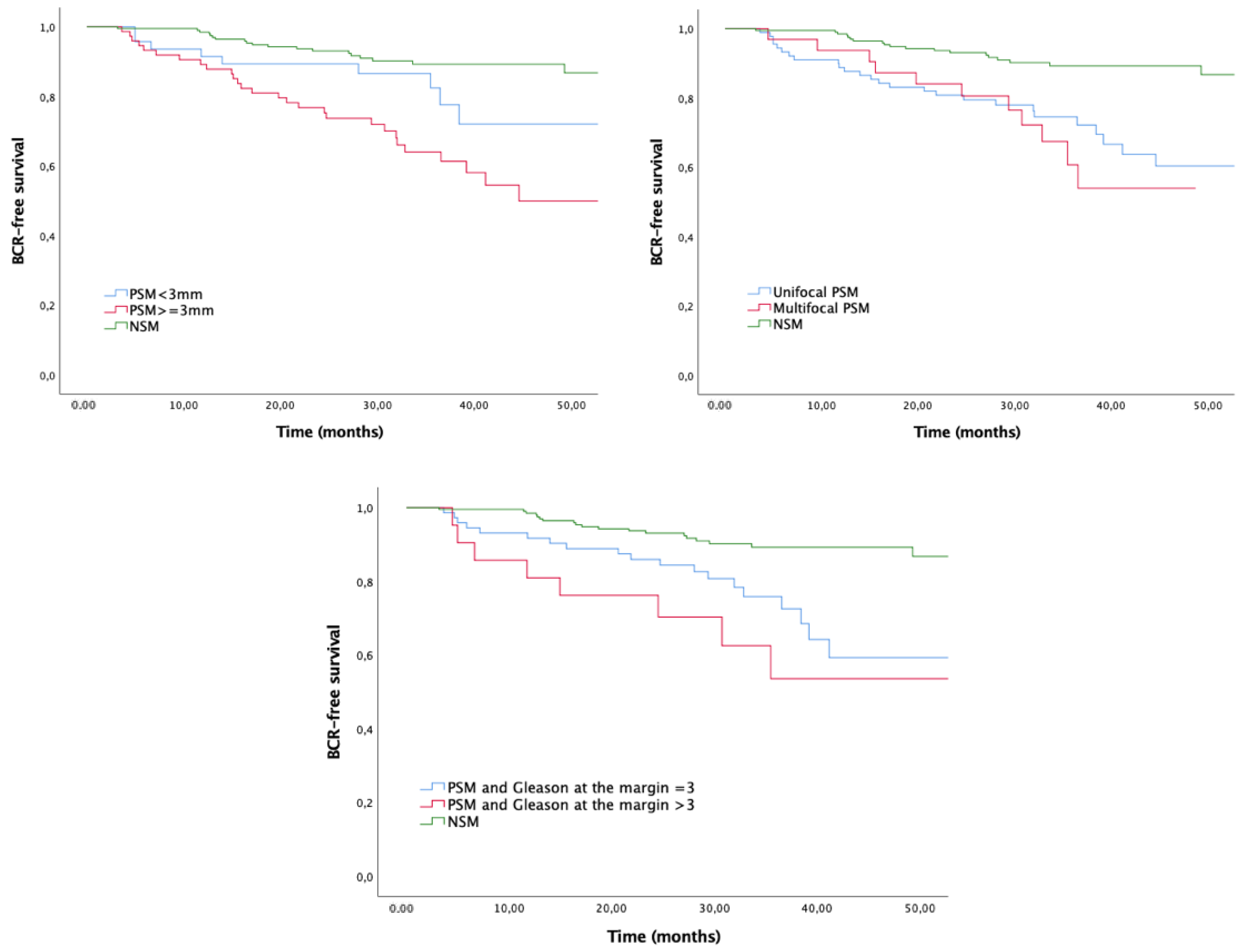
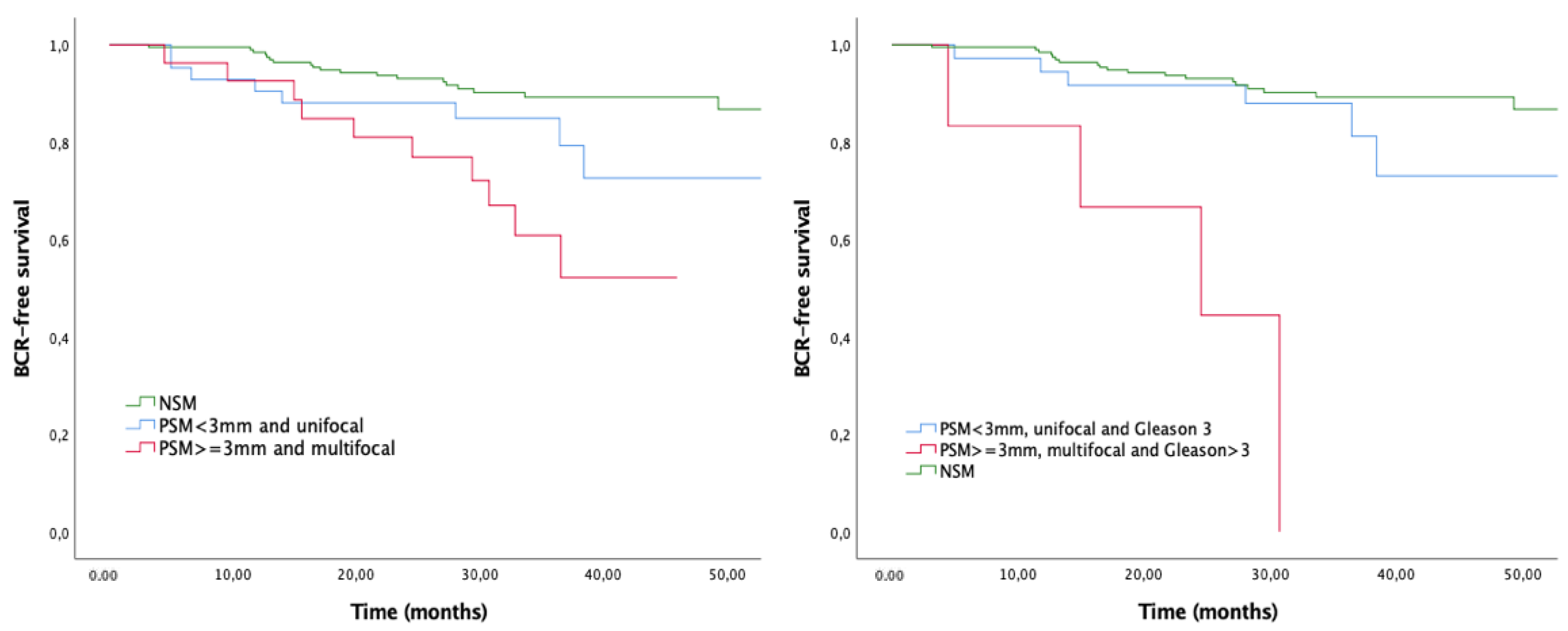
3.2. Impact of PSM and Their Adverse Characteristics on the Risk of BCR
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boorjian, S.A.; Karnes, R.J.; Crispen, P.L.; Carlson, R.E.; Rangel, L.J.; Bergstralh, E.J.; Blute, M.L. The Impact of Positive Surgical Margins on Mortality Following Radical Prostatectomy During the Prostate Specific Antigen Era. J. Urol. 2010, 183, 1003–1009. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.R.; Coelho, R.F.; Rocco, B.; Orvieto, M.; Sivaraman, A.; Palmer, K.J.; Kameh, D.; Santoro, L.; Coughlin, G.D.; Liss, M.; et al. Positive surgical margins after robotic assisted radical prostatectomy: A multi-institutional study. J. Urol. 2011, 186, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.L.; Dalkin, B.L.; True, L.D.; Ellis, W.J.; Stanford, J.L.; Lange, P.H.; Lin, D.W. 127 Positive Surgical Margins At Radical Prostatectomy Predict Prostate Cancer-Specific Mortality: Support for Optimizing Surgical Technique and Pathological Evaluation At Radical Prostatectomy. J. Urol. 2010, 183, 2213–2218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pfitzenmaier, J.; Pahernik, S.; Tremmel, T.; Haferkamp, A.; Buse, S.; Hohenfellner, M. Positive surgical margins after radical prostatectomy: Do they have an impact on biochemical or clinical progression? BJU Int. 2008, 102, 1413–1418. [Google Scholar] [CrossRef] [PubMed]
- Ploussard, G.; Agamy, M.A.; Alenda, O.; Allory, Y.; Mouracade, P.; Vordos, D.; Hoznek, A.; Abbou, C.C.; De La Taille, A.; Salomon, L. Impact of positive surgical margins on prostate-specific antigen failure after radical prostatectomy in adjuvant treatment-naïve patients. BJU Int. 2011, 107, 1748–1754. [Google Scholar] [CrossRef] [PubMed]
- Yossepowitch, O.; Briganti, A.; Eastham, J.A.; Epstein, J.; Graefen, M.; Montironi, R.; Touijer, K. Positive surgical margins after radical prostatectomy: A systematic review and contemporary update. Eur. Urol. 2014, 65, 303–313. [Google Scholar] [CrossRef]
- Dev, H.S.; Wiklund, P.; Patel, V.; Parashar, D.; Palmer, K.; Nyberg, T.; Skarecky, D.; Neal, D.E.; Ahlering, T.; Sooriakumaran, P. Surgical margin length and location affect recurrence rates after robotic prostatectomy. Urol. Oncol. Semin. Orig. Investig. 2015, 33, 109.e7–109.e13. [Google Scholar] [CrossRef]
- Sooriakumaran, P.; Ploumidis, A.; Nyberg, T.; Olsson, M.; Akre, O.; Haendler, L.; Egevad, L.; Nilsson, A.; Carlsson, S.; Jonsson, M.; et al. The impact of length and location of positive margins in predicting biochemical recurrence after robot-assisted radical prostatectomy with a minimum follow-up of 5 years. BJU Int. 2015, 115, 106–113. [Google Scholar] [CrossRef]
- Sachdeva, A.; Veeratterapillay, R.; Voysey, A.; Kelly, K.; Johnson, M.I.; Aning, J.; Soomro, N.A. Positive surgical margins and biochemical recurrence following minimally-invasive radical prostatectomy-An analysis of outcomes from a UK tertiary referral centre. BMC Urol. 2017, 17, 91. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Wu, B.; Zha, Z.; Zhao, H.; Jiang, Y.; Yuan, J. Positive surgical margin is associated with biochemical recurrence risk following radical prostatectomy: A meta-analysis from high-quality retrospective cohort studies. World J. Surg. Oncol. 2018, 16, 124. [Google Scholar] [CrossRef] [Green Version]
- Mithal, P.; Howard, L.E.; Aronson, W.J.; Terris, M.K.; Cooperberg, M.R.; Kane, C.J.; Amling, C.; Freedland, S.J. Positive surgical margins in radical prostatectomy patients do not predict long-term oncological outcomes: Results from the Shared Equal Access Regional Cancer Hospital (SEARCH) cohort. BJU Int. 2016, 117, 244–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bolla, M.; Van Poppel, H.; Tombal, B.; Vekemans, K.; Da Pozzo, L.; De Reijke, T.M.; Verbaeys, A.; Bosset, J.F.; Van Velthoven, R.; Colombel, M.; et al. Postoperative radiotherapy after radical prostatectomy for high-risk prostate cancer: Long-term results of a randomised controlled trial (EORTC trial 22911). Lancet 2012, 380, 2018–2027. [Google Scholar] [CrossRef]
- Wiegel, T.; Bottke, D.; Steiner, U.; Siegmann, A.; Golz, R.; Störkel, S.; Willich, N.; Semjonow, A.; Souchon, R.; Stöckle, M.; et al. Phase III postoperative adjuvant radiotherapy after radical prostatectomy compared with radical prostatectomy alone in pT3 prostate cancer with postoperative undetectable prostate-specific antigen: ARO 96-02/AUO AP 09/95. J. Clin. Oncol. 2009, 27, 2924–2930. [Google Scholar] [CrossRef]
- Thompson, I.M.; Tangen, C.M.; Paradelo, J.; Lucia, M.S.; Miller, G.; Troyer, D.; Messing, E.; Forman, J.; Chin, J.; Swanson, G.; et al. Adjuvant Radiotherapy for Pathological T3N0M0 Prostate Cancer Significantly Reduces Risk of Metastases and Improves Survival: Long-Term Followup of a Randomized Clinical Trial. J. Urol. 2009, 181, 956–962. [Google Scholar] [CrossRef] [PubMed]
- Hwang, W.L.; Tendulkar, R.D.; Niemierko, A.; Agrawal, S.; Stephans, K.L.; Spratt, D.E.; Hearn, J.W.; Koontz, B.F.; Lee, W.R.; Michalski, J.M.; et al. Comparison between adjuvant and early-salvage postprostatectomy radiotherapy for prostate cancer with adverse pathological features. JAMA Oncol. 2018, 4, e175230. [Google Scholar] [CrossRef] [PubMed]
- Mauermann, J.; Fradet, V.; Lacombe, L.; Dujardin, T.; Tiguert, R.; Tetu, B.; Fradet, Y. The impact of solitary and multiple positive surgical margins on hard clinical end points in 1712 adjuvant treatment-naive pT2-4 N0 radical prostatectomy patients. Eur. Urol. 2013, 64, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Mottet, N.; van den Bergh, R.C.N.; Briers, E.; Van den Broeck, T.; Cumberbatch, M.G.; De Santis, M.; Fanti, S.; Fossati, N.; Gandaglia, G.; Gillessen, S.; et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer—2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur. Urol. 2021, 79, 243–262. [Google Scholar] [CrossRef]
- Parker, C.C.; Clarke, N.W.; Cook, A.D.; Kynaston, H.G.; Petersen, P.M.; Catton, C.; Cross, W.; Logue, J.; Parulekar, W.; Payne, H.; et al. Timing of radiotherapy after radical prostatectomy (RADICALS-RT): A randomised, controlled phase 3 trial. Lancet 2020, 396, 1413–1421. [Google Scholar] [CrossRef]
- Kneebone, A.; Fraser-Browne, C.; Duchesne, G.M.; Fisher, R.; Frydenberg, M.; Herschtal, A.; Williams, S.G.; Brown, C.; Delprado, W.; Haworth, A.; et al. Adjuvant radiotherapy versus early salvage radiotherapy following radical prostatectomy (TROG 08.03/ANZUP RAVES): A randomised, controlled, phase 3, non-inferiority trial. Lancet Oncol. 2020, 21, 1331–1340. [Google Scholar] [CrossRef]
- Sargos, P.; Chabaud, S.; Latorzeff, I.; Magné, N.; Benyoucef, A.; Supiot, S.; Pasquier, D.; Abdiche, M.S.; Gilliot, O.; Graff-Cailleaud, P.; et al. Adjuvant radiotherapy versus early salvage radiotherapy plus short-term androgen deprivation therapy in men with localised prostate cancer after radical prostatectomy (GETUG-AFU 17): A randomised, phase 3 trial. Lancet Oncol. 2020, 21, 1341–1352. [Google Scholar] [CrossRef]
- Vale, C.L.; Fisher, D.; Kneebone, A.; Parker, C.; Pearse, M.; Richaud, P.; Sargos, P.; Sydes, M.R.; Brawley, C.; Brihoum, M.; et al. Adjuvant or early salvage radiotherapy for the treatment of localised and locally advanced prostate cancer: A prospectively planned systematic review and meta-analysis of aggregate data. Lancet 2020, 396, 1422–1431. [Google Scholar] [CrossRef]
- Martini, A.; Gandaglia, G.; Fossati, N.; Scuderi, S.; Bravi, C.A.; Mazzone, E.; Stabile, A.; Scarcella, S.; Robesti, D.; Barletta, F.; et al. Defining Clinically Meaningful Positive Surgical Margins in Patients Undergoing Radical Prostatectomy for Localised Prostate Cancer. Eur. Urol. Oncol. 2021, 4, 42–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shikanov, S.; Song, J.; Royce, C.; Al-Ahmadie, H.; Zorn, K.; Steinberg, G.; Zagaja, G.; Shalhav, A.; Eggener, S. Length of Positive Surgical Margin After Radical Prostatectomy as a Predictor of Biochemical Recurrence. J. Urol. 2009, 182, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Udo, K.; Cronin, A.M.; Carlino, L.J.; Savage, C.J.; Maschino, A.C.; Al-Ahmadie, H.A.; Gopalan, A.; Tickoo, S.K.; Scardino, P.T.; Eastham, J.A.; et al. Prognostic impact of subclassification of radical prostatectomy positive margins by linear extent and Gleason grade. J. Urol. 2013, 189, 1302–1307. [Google Scholar] [CrossRef]
- Ploussard, G.; Drouin, S.J.; Rode, J.; Allory, Y.; Vordos, D.; Hoznek, A.; Abbou, C.C.; de la Taille, A.; Salomon, L. Location, extent, and multifocality of positive surgical margins for biochemical recurrence prediction after radical prostatectomy. World J. Urol. 2014, 32, 1393–1400. [Google Scholar] [CrossRef]
- Chapin, B.F.; Nguyen, J.N.; Achim, M.F.; Navai, N.; Williams, S.B.; Prokhorova, I.N.; Wang, X.; Tapia, E.M.L.N.; Davis, J.W.; Troncoso, P. Positive margin length and highest Gleason grade of tumor at the margin predict for biochemical recurrence after radical prostatectomy in patients with organ-confined prostate cancer. Prostate Cancer Prostatic Dis. 2018, 21, 221–227. [Google Scholar] [CrossRef]
- Preisser, F.; Coxilha, G.; Heinze, A.; Oh, S.; Chun, F.K.H.; Sauter, G.; Pompe, R.S.; Huland, H.; Graefen, M.; Tilki, D. Impact of positive surgical margin length and Gleason grade at the margin on biochemical recurrence in patients with organ-confined prostate cancer. Prostate 2019, 79, 1832–1836. [Google Scholar] [CrossRef]
- Hollemans, E.; Verhoef, E.I.; Bangma, C.H.; Rietbergen, J.; Helleman, J.; Roobol, M.J.; Van Leenders, G.J.L.H. Prostate Carcinoma Grade and Length but Not Cribriform Architecture at Positive Surgical Margins Are Predictive for Biochemical Recurrence after Radical Prostatectomy. Am. J. Surg. Pathol. 2020, 44, 191–197. [Google Scholar] [CrossRef]
- Preisser, F.; Heinze, A.; Abrams-Pompe, R.S.; Budäus, L.; Chun, F.K.-H.; Graefen, M.; Huland, H.; Tilki, D. Impact of positive surgical margin length and Gleason grade at the margin on oncologic outcomes in patients with nonorgan-confined prostate cancer. Prostate 2022, 1, 1832–1836. [Google Scholar] [CrossRef]
- Remmers, S.; Hollemans, E.; Nieboer, D.; Luiting, H.B.; van Leenders, G.J.L.H.; Helleman, J.; Roobol, M.J. Improving the prediction of biochemical recurrence after radical prostatectomy with the addition of detailed pathology of the positive surgical margin and cribriform growth. Ann. Diagn. Pathol. 2022, 56, 151842. [Google Scholar] [CrossRef]
- Dason, S.; Vertosick, E.A.; Udo, K.; Sjoberg, D.D.; Vickers, A.J.; Al-Ahmadie, H.; Chen, Y.B.; Gopalan, A.; Joseph Sirintrapun, S.; Tickoo, S.K.; et al. Clinical utility of subclassifying positive surgical margins at radical prostatectomy. BJU Int. 2022, 129, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Morizane, S.; Yumioka, T.; Makishima, K.; Tsounapi, P.; Iwamoto, H.; Hikita, K.; Honda, M.; Umekita, Y.; Takenaka, A. Impact of positive surgical margin status in predicting early biochemical recurrence after robot-assisted radical prostatectomy. Int. J. Clin. Oncol. 2021, 26, 1961–1967. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, A.E.; Carlsson, S.; Laven, B.A.; Wiklund, N.P. Karolinska prostatectomy: A robot-assisted laparoscopic radical prostatectomy technique. Scand. J. Urol. Nephrol. 2006, 40, 453–458. [Google Scholar] [CrossRef]
- Gandaglia, G.; De Lorenzis, E.; Novara, G.; Fossati, N.; De Groote, R.; Dovey, Z.; Suardi, N.; Montorsi, F.; Briganti, A.; Rocco, B.; et al. Robot-assisted Radical Prostatectomy and Extended Pelvic Lymph Node Dissection in Patients with Locally-advanced Prostate Cancer. Eur. Urol. 2017, 71, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Brimo, F.; Partin, A.W.; Epstein, J.I. Tumor grade at margins of resection in radical prostatectomy specimens is an independent predictor of prognosis. Urology 2010, 76, 1206–1209. [Google Scholar] [CrossRef] [PubMed]
- Lysenko, I.; Mori, K.; Mostafaei, H.; Enikeev, D.V.; Karakiewicz, P.I.; Briganti, A.; Quhal, F.; Janisch, F.; Shariat, S.F. Prognostic Value of Gleason Score at Positive Surgical Margin in Prostate Cancer: A Systematic Review and Meta-analysis. Clin. Genitourin. Cancer 2020, 18, e517–e522. [Google Scholar] [CrossRef]
- Eggener, S.E.; Scardino, P.T.; Walsh, P.C.; Han, M.; Partin, A.W.; Trock, B.J.; Feng, Z.; Wood, D.P.; Eastham, J.A.; Yossepowitch, O.; et al. Predicting 15-year prostate cancer specific mortality after radical prostatectomy. J. Urol. 2011, 185, 869–875. [Google Scholar] [CrossRef] [Green Version]
- Meeks, J.J.; Eastham, J.A. Radical prostatectomy: Positive surgical margins matter. Urol. Oncol. Semin. Orig. Investig. 2013, 31, 974–979. [Google Scholar] [CrossRef]
- Novara, G.; Ficarra, V.; Mocellin, S.; Ahlering, T.E.; Carroll, P.R.; Graefen, M.; Guazzoni, G.; Menon, M.; Patel, V.R.; Shariat, S.F.; et al. Systematic review and meta-analysis of studies reporting oncologic outcome after robot-assisted radical prostatectomy. Eur. Urol. 2012, 62, 382–404. [Google Scholar] [CrossRef]
- Cao, D.; Humphrey, P.A.; Gao, F.; Tao, Y.; Kibel, A.S. Ability of linear length of positive margin in radical prostatectomy specimens to predict biochemical recurrence. Urology 2011, 77, 1409–1414. [Google Scholar] [CrossRef]
- Stephenson, A.J.; Wood, D.P.; Kattan, M.W.; Klein, E.A.; Scardino, P.T.; Eastham, J.A.; Carver, B.S. Location, Extent and Number of Positive Surgical Margins Do Not Improve Accuracy of Predicting Prostate Cancer Recurrence After Radical Prostatectomy. J. Urol. 2009, 182, 1357–1363. [Google Scholar] [CrossRef] [PubMed]
- Tan, P.H.; Cheng, L.; Srigley, J.R.; Griffiths, D.; Humphrey, P.A.; Van Der Kwast, T.H.; Montironi, R.; Wheeler, T.M.; Delahunt, B.; Egevad, L.; et al. International society of urological pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens. Working group 5: Surgical margins. Mod. Pathol. 2011, 24, 48–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yossepowitch, O.; Bjartell, A.; Eastham, J.A.; Graefen, M.; Guillonneau, B.D.; Karakiewicz, P.I.; Montironi, R.; Montorsi, F. Positive Surgical Margins in Radical Prostatectomy: Outlining the Problem and Its Long-Term Consequences. Eur. Urol. 2009, 55, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Wadhwa, H.; Terris, M.K.; Aronson, W.J.; Kane, C.J.; Amling, C.L.; Cooperberg, M.R.; Freedland, S.J.; Abern, M.R. Long-term oncological outcomes of apical positive surgical margins at radical prostatectomy in the Shared Equal Access Regional Cancer Hospital cohort. Prostate Cancer Prostatic Dis. 2016, 19, 423–428. [Google Scholar] [CrossRef]
- Dinneen, E.P.; Van Der Slot, M.; Adasonla, K.; Tan, J.; Grierson, J.; Haider, A.; Freeman, A.; Oakley, N.; Shaw, G. Intraoperative Frozen Section for Margin Evaluation During Radical Prostatectomy: A Systematic Review. Eur. Urol. Focus 2020, 6, 664–673. [Google Scholar] [CrossRef] [Green Version]
| Variable | All Patients n = 333 | Negative Surgical Margins n (%) = 209 (62.8) | Positive Surgical Margins n (%) = 124 (37.2) | p Value |
|---|---|---|---|---|
| Age (years), median (IQR) | 65 (59–68.5) | 65 (60–69) | 65 (59–68) | 0.328 |
| BMI (kg/m2), median (IQR) | 27 (25–29.75) | 26 (25–29) | 27.50 (25–30) | 0.021 |
| Preop PSA (ng/mL), median (IQR) | 6 (4.8–8.5) | 5.98 (4.74–8.0) | 6.17 (5.02–9.22) | 0.088 |
| Surgery time (min), median (IQR) | 170 (140–210) | 170 (140–210) | 175 (140–205) | 0.611 |
| Prostate volume (gr), median (IQR) | 50 (39–65) | 55 (40–65) | 42.5 (34.25–60.00) | <0.001 |
| pT, n (%) | 0.020 | |||
| pT2 | 250 (75.1) | 167 (79.9) | 83 (67.0) | |
| pT3a | 70 (21) | 34 (16.3) | 36 (29.0) | |
| pT3b-T4 | 13 (3.9) | 8 (3.8) | 5 (4.0) | |
| pN, n (%) | 0.735 | |||
| Nx | 244 (73.3) | 156 (74.6) | 88 (71.0) | |
| N0 | 87 (26.1) | 52 (24.9) | 35 (28.2) | |
| N1 | 2 (0.6) | 1 (0.5) | 1 (0.8) | |
| Pathological ISUP, n (%) | 0.149 | |||
| 1 | 76 (22.8) | 54 (25.8) | 22 (17.7) | |
| 2–3 | 223 (67.0) | 137 (65.6) | 86 (69.4) | |
| 4–5 | 34 (10.2) | 18 (8.6) | 16 (12.9) | |
| Positive surgical margins, n (%) | 124 (37.2) | |||
| ECE, n (%) | 83 (24.9) | 42 (20.1) | 41 (33.1) | 0.008 |
| SVI, n (%) | 13 (3.9) | 8 (3.8) | 5 (4.0) | 0.926 |
| Follow-up (months), median (IQR) | 34.5 (26.3–47.0) | 33.7 (25.0–46.6) | 36.62 (28.06–48.04) | 0.275 |
| BCR, n (%) | 60 (18.0) | 20 (9.6) | 40 (32.3) | <0.001 |
| Variable | Positive Surgical Margins |
|---|---|
| Length of PSM (mm), median (IQR) | 3.5 (2–6) |
| Length of PSM (mm), n (%) | |
| <3 mm | 49 (39.5) |
| ≥3 mm | 75 (60.5) |
| Focality, n (%) | |
| Unifocal | 91 (73.4) |
| Multifocal | 33 (26.6) |
| Location, n (%) | |
| Apex | 32 (25.8) |
| Posterior | 39 (31.5) |
| Lateral | 8 (6.5) |
| Anterior | 8 (6.5) |
| Vesical | 4 (3.2) |
| Multiple | 33 (26.6) |
| Gleason Grade at PSM, n (%) | |
| 3 | 74 (59.7) |
| 4 | 20 (16.1) |
| 5 | 2 (1.6) |
| Unknown | 28 (22.6) |
| Variable | Univariable Analysis | Multivariable Analysis* | |||
|---|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | c-Index | |
| PSM (vs. neg) | 3.74 (2.18–6.41) | <0.001 | 3.71 (2.13–6.47) | <0.001 | 0.738 (0.66–0.80) |
| PSM ≥ 3 mm (vs. neg) | 4.66 (2.63–8.27) | <0.001 | 4.51 (2.49–8.17) | <0.001 | 0.751 (0.69–0.82) |
| (vs. favourable margins) | 3.68 (2.21–6.13) | <0.001 | 3.50 (2.05–5.95) | <0.001 | |
| PSM multifocal (vs. neg) | 4.23 (2.01–8.92) | <0.001 | 4.16 (1.90–9.09) | <0.001 | 0.740 (0.68–0.81) |
| (vs. favourable margins) | 2.40 (1.24–4.66) | 0.009 | 2.18 (1.09–4.37) | 0.028 | |
| PSM with GG > 3 (vs. neg) | 6.06 (2.83–12.99) | <0.001 | 3.02(1.33–6.86) | 0.008 | 0.739 (0.66–0.82) |
| (vs. favourable margins) | 3.98 (1.98–7.98) | <0.001 | 2.00 (0.94–4.27) | 0.072 | |
| PSM ≥ 3 mm and multifocal (vs. neg) | 4.75 (2.20–10.26) | <0.001 | 4.66 (2.08–10.42) | <0.001 | 0.740 (0.68–0.81) |
| (vs. favourable margins) | 2.69 (1.35–5.34) | 0.005 | 2.43 (1.18–4.99) | 0.016 | |
| PSM ≥ 3 mm, multifocal and GG> 3 (vs. neg) | 15.17 (4.42–39.27) | <0.001 | 5.98 (1.86–19.24) | 0.003 | 0.740 (0.68–0.80) |
| (vs. favourable margins) | 6.99 (2.49–19.61) | <0.001 | 2.99 (0.99–9.02) | 0.052 | |
| Variable | HR (95% CI) | p Value |
|---|---|---|
| PSM (vs. neg) | 5.05 (2.55–11.90) | <0.001 |
| PSM ≥ 3 mm (vs. neg) | 6.82 (2.95–15.79) | <0.001 |
| PSM multifocal (vs. neg) | 7.06 (2.34–21.29) | 0.001 |
| PSM with Gleason at margin > 3 (vs. neg) | 8.20 (2.50–26.92) | 0.001 |
| PSM ≥3 mm and multifocal (vs. neg) | 7.12 (2.17–23.33) | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carbonell, E.; Matheu, R.; Muní, M.; Sureda, J.; García-Sorroche, M.; Ribal, M.J.; Alcaraz, A.; Vilaseca, A. The Effect of Adverse Surgical Margins on the Risk of Biochemical Recurrence after Robotic-Assisted Radical Prostatectomy. Biomedicines 2022, 10, 1911. https://doi.org/10.3390/biomedicines10081911
Carbonell E, Matheu R, Muní M, Sureda J, García-Sorroche M, Ribal MJ, Alcaraz A, Vilaseca A. The Effect of Adverse Surgical Margins on the Risk of Biochemical Recurrence after Robotic-Assisted Radical Prostatectomy. Biomedicines. 2022; 10(8):1911. https://doi.org/10.3390/biomedicines10081911
Chicago/Turabian StyleCarbonell, Enric, Roger Matheu, Maria Muní, Joan Sureda, Mónica García-Sorroche, María José Ribal, Antonio Alcaraz, and Antoni Vilaseca. 2022. "The Effect of Adverse Surgical Margins on the Risk of Biochemical Recurrence after Robotic-Assisted Radical Prostatectomy" Biomedicines 10, no. 8: 1911. https://doi.org/10.3390/biomedicines10081911
APA StyleCarbonell, E., Matheu, R., Muní, M., Sureda, J., García-Sorroche, M., Ribal, M. J., Alcaraz, A., & Vilaseca, A. (2022). The Effect of Adverse Surgical Margins on the Risk of Biochemical Recurrence after Robotic-Assisted Radical Prostatectomy. Biomedicines, 10(8), 1911. https://doi.org/10.3390/biomedicines10081911






