Metformin Is Associated with the Inhibition of Renal Artery AT1R/ET-1/iNOS Axis in a Rat Model of Diabetic Nephropathy with Suppression of Inflammation and Oxidative Stress and Kidney Injury
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals
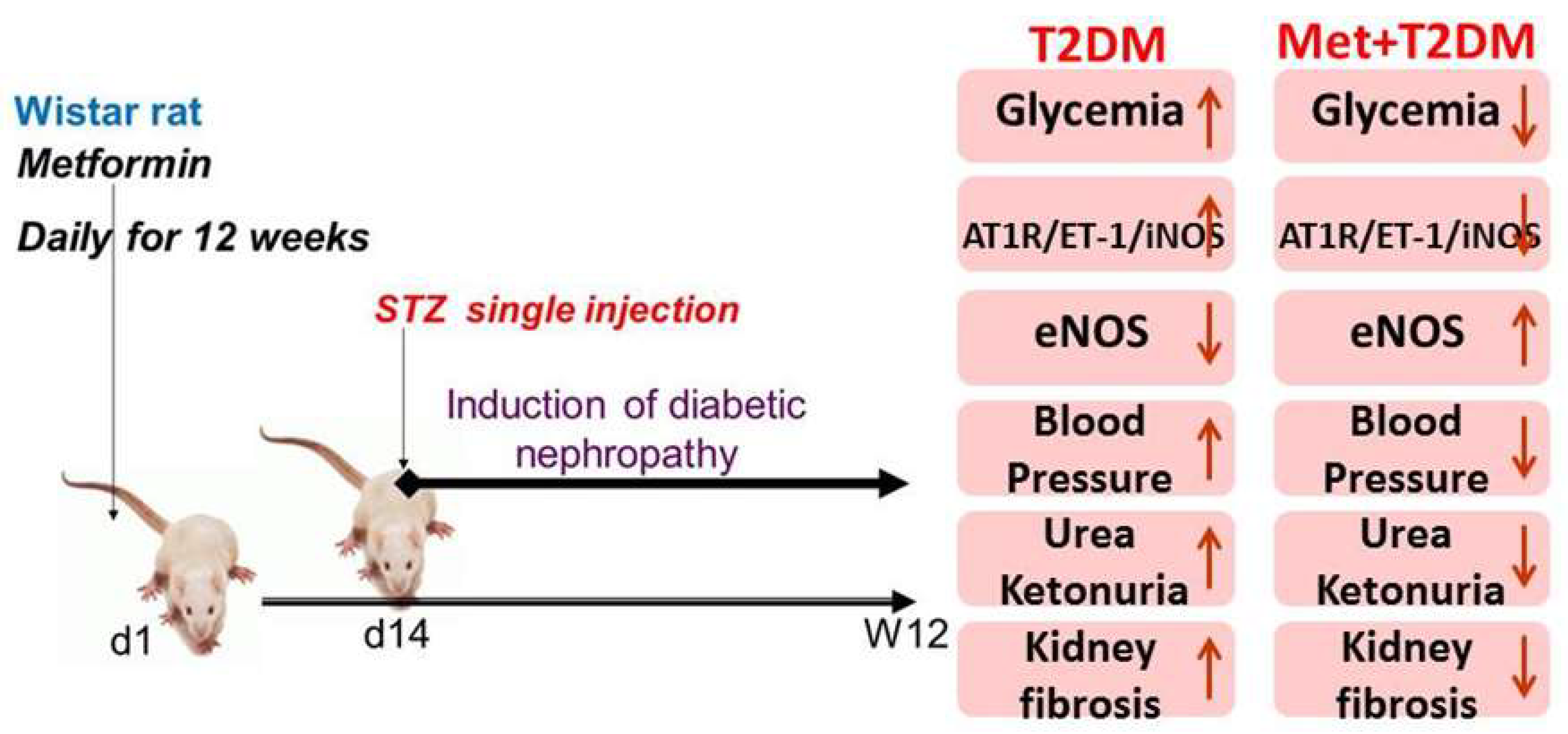
2.2. Experimental Design
2.3. Determination of Glucose, HbA1c, Urea, Creatinine, High Sensitivity C-Reactive Protein (hs-CRP), Tumor Necrosis Factor-Alpha (TNF-α), Interleukin-6 (IL-6), Malondialdehyde (MDA), Superoxide Dismutase (SOD), Glutathione Peroxidase (GPx), Urine Albumin and Ketones
2.4. Quantitative Real-Time Polymerase Chain Reaction (qRT-PCR) of iNOS and eNOS Gene Levels
2.5. Western Blotting Analysis of AT1R
2.6. Immunostaining and Assessment of Kidney Pathology
2.7. Determination of Tissue Levels of ET-1 and Advanced Glycation End Products (AGEs)
2.8. Determination of Mean Arterial Blood Pressure
2.9. Statistical Analysis
3. Results
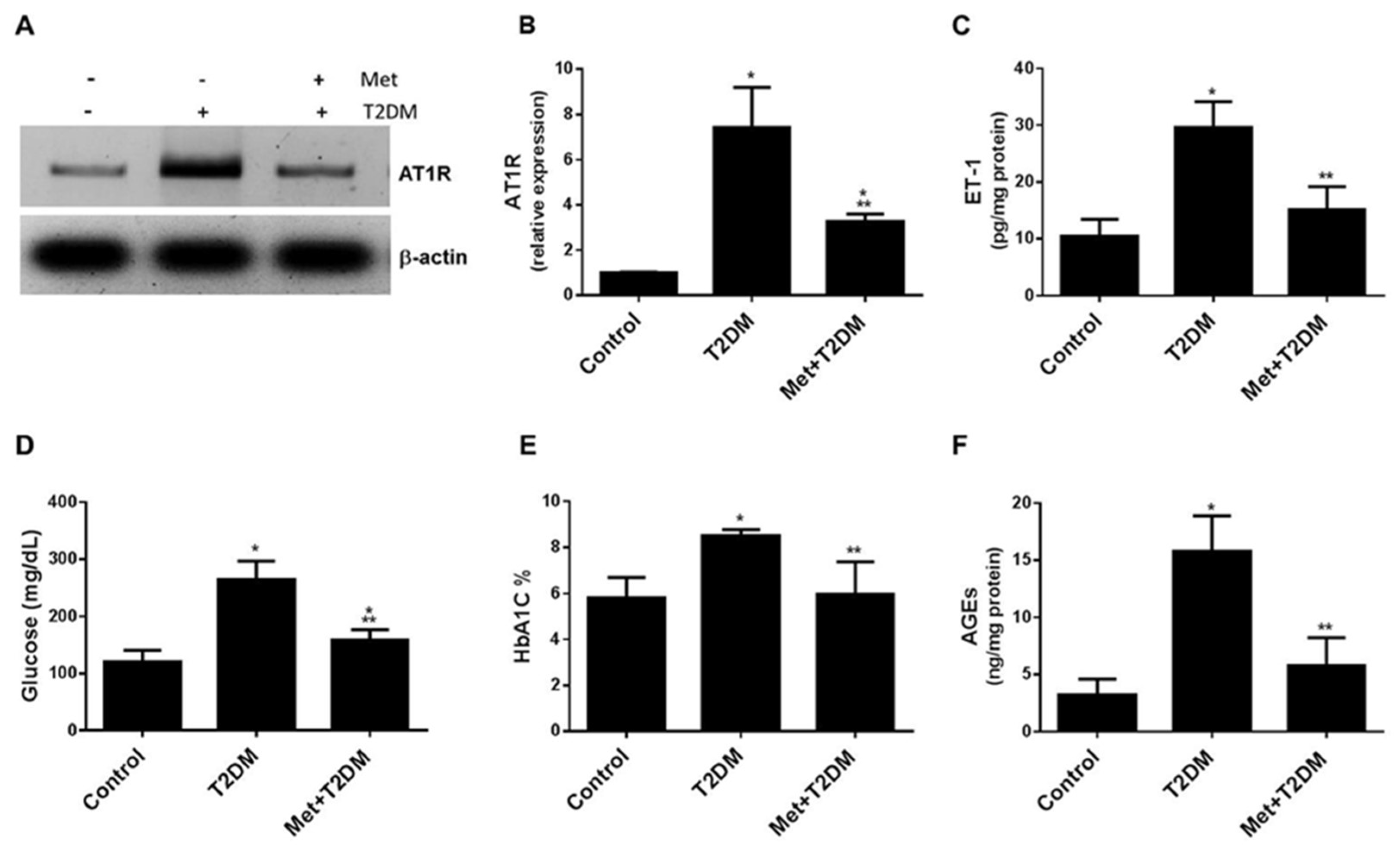
3.1. Metformin Is Associated with the Inhibition of the AT1R/ET-1 Axis and AGEs in the Renal Artery Induced by Diabetes
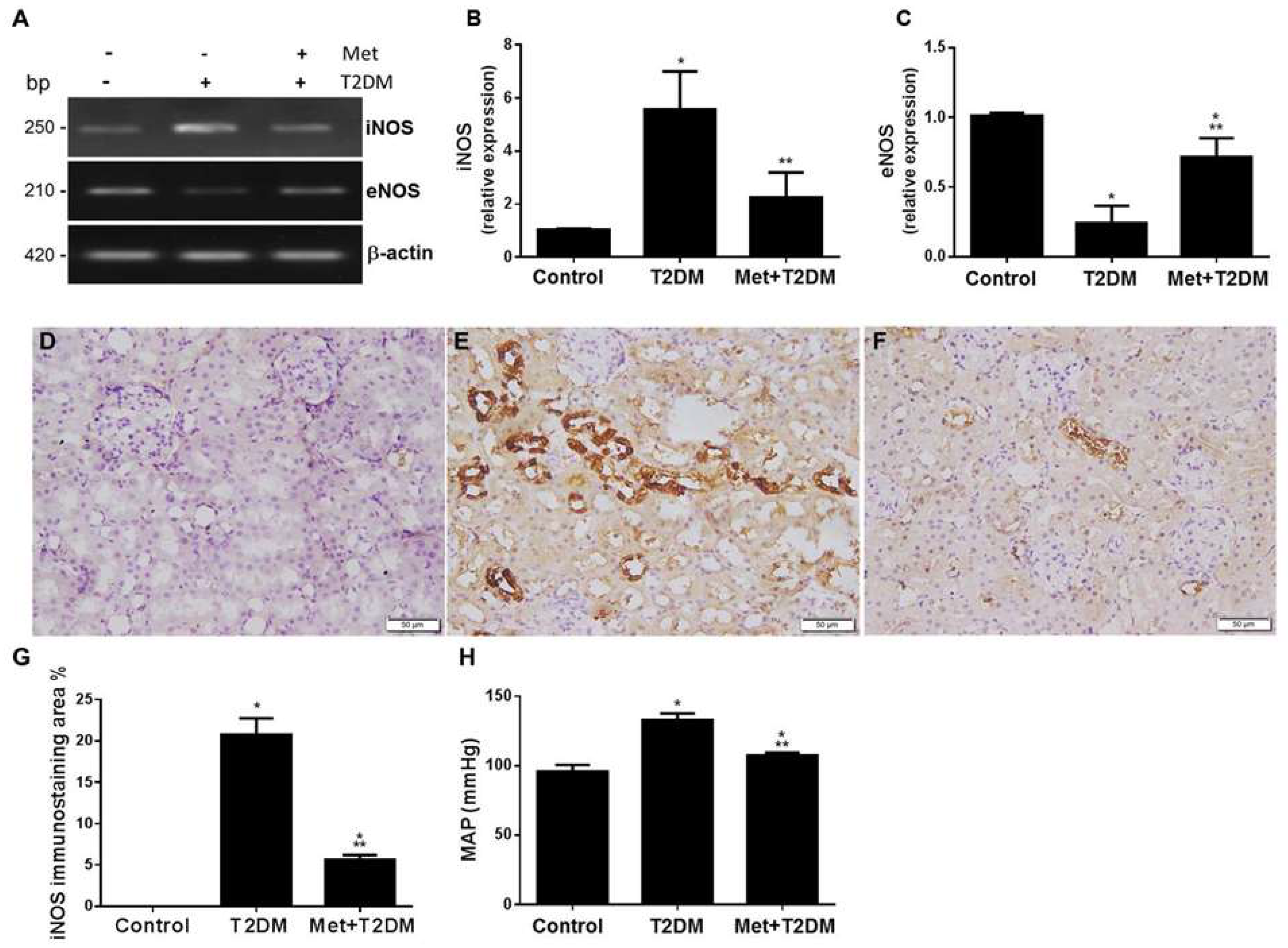
3.2. Metformin Protects against Diabetes-Modulated NOS Enzymes in Renal Artery and Kidney Tissue
3.3. Metformin Inhibits Biomarkers of Inflammation and Oxidative Stress Induced by Diabetes
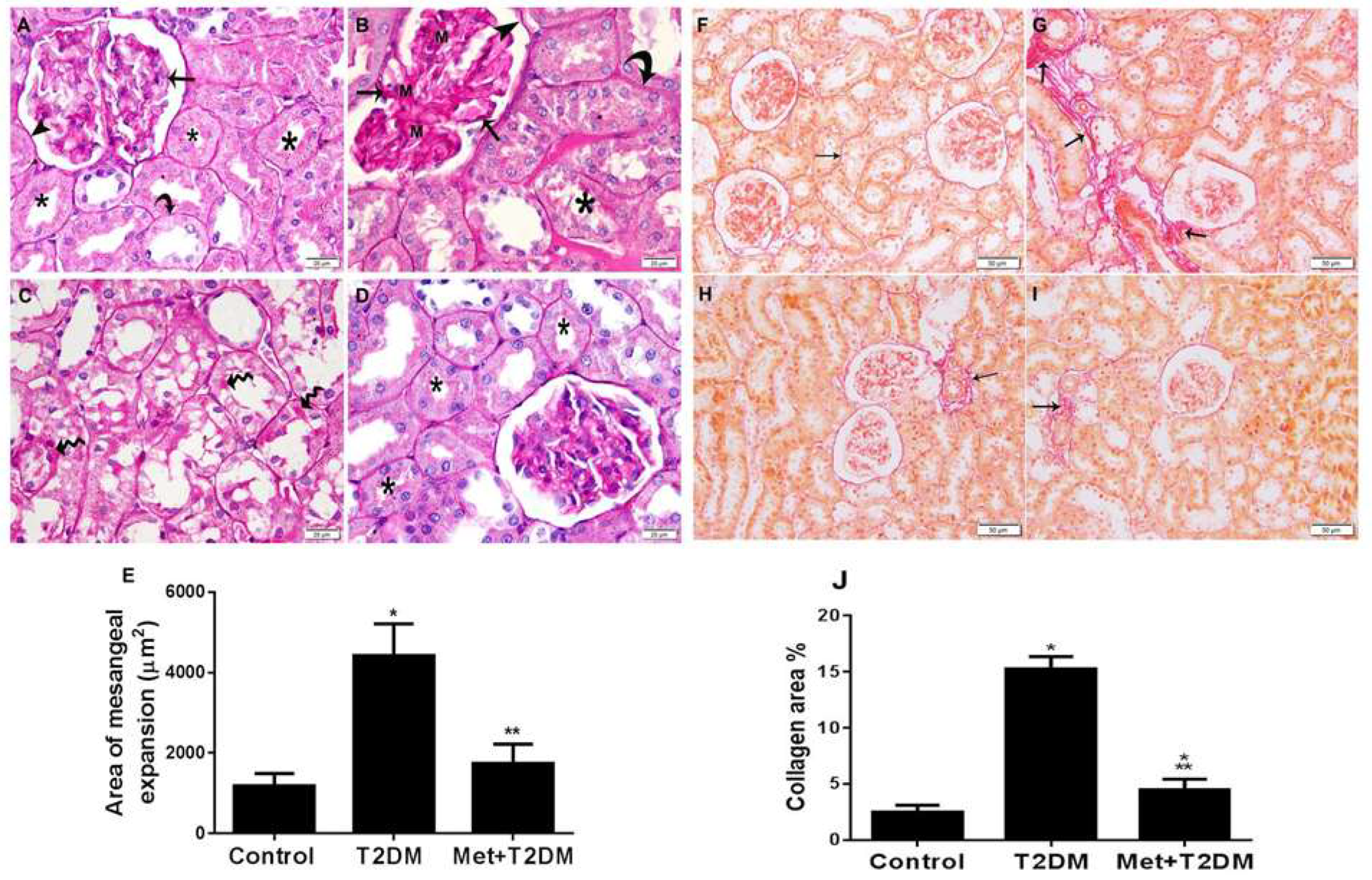
3.4. Metformin Is Associated with Inhibition of Mesangial Matrix Expansion and Kidney Fibrosis Induced by Diabetes
3.5. Metformin Inhibits Biomarkers of Kidney Injury Induced by Diabetes
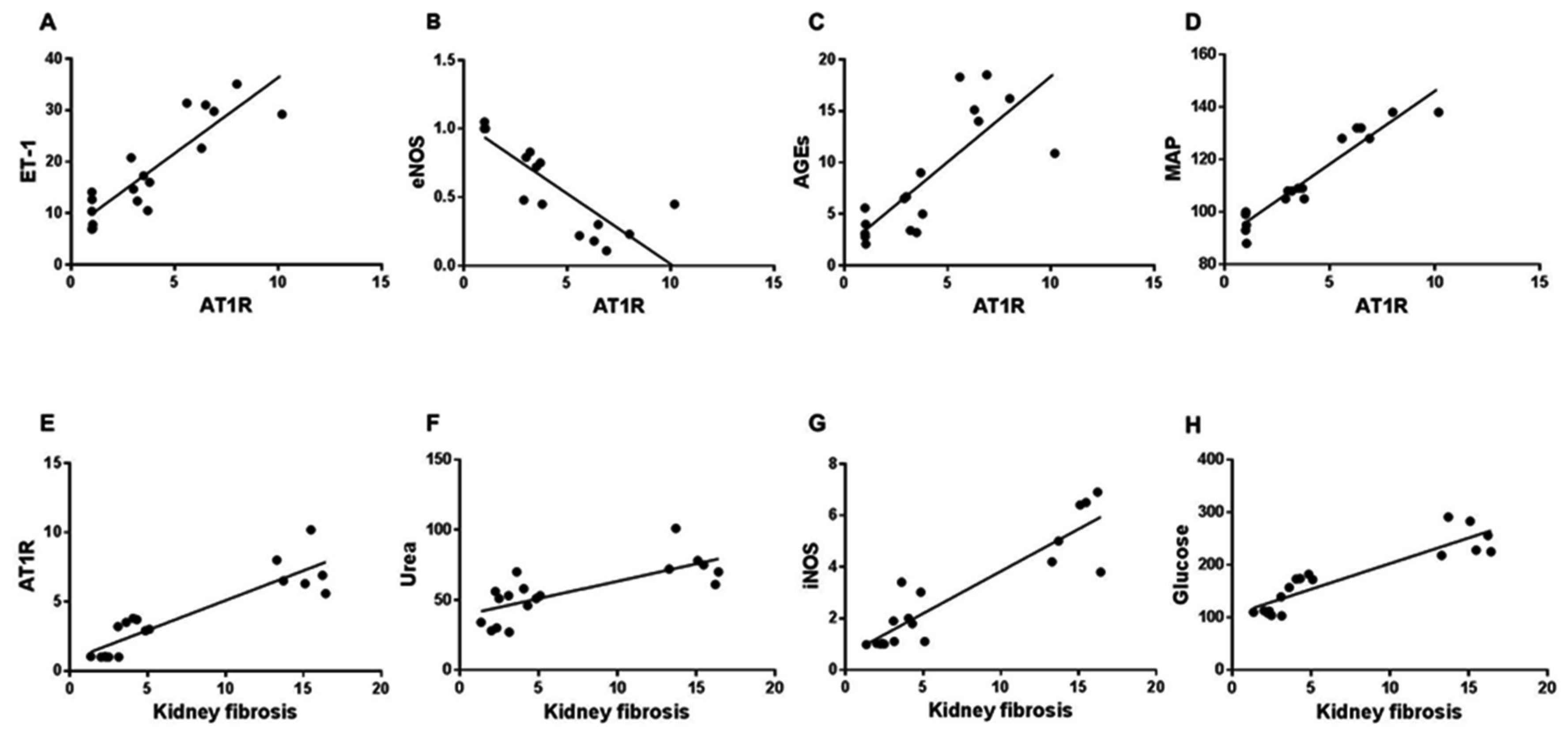
3.6. Correlation between AT1 or Kidney Fibrosis Score and Biomarkers of Vascular and Kidney Injuries
4. Discussion
Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rabkin, R. Diabetic nephropathy. Clin. Cornerstone 2003, 5, 1–11. [Google Scholar] [CrossRef]
- Gheith, O.; Farouk, N.; Nampoory, N.; Halim, M.A.; Al-Otaibi, T. Diabetic kidney disease: World wide difference of prevalence and risk factors. J. Nephropharmacol. 2016, 5, 49–56. [Google Scholar] [CrossRef]
- Kopelman, P.G. Obesity as a medical problem. Nature 2000, 404, 635–643. [Google Scholar] [CrossRef]
- Lustig, R.H.; Schmidt, L.A.; Brindis, C.D. Public health: The toxic truth about sugar. Nature 2012, 482, 27–29. [Google Scholar] [CrossRef]
- Iseki, K.; Ikemiya, Y.; Kinjo, K.; Inoue, T.; Iseki, C.; Takishita, S. Body mass index and the risk of development of end-stage renal disease in a screened cohort. Kidney Int. 2004, 65, 1870–1876. [Google Scholar] [CrossRef] [Green Version]
- Shen, W.-W.; Chen, H.-M.; Chen, H.; Xu, F.; Li, L.-S.; Liu, Z.-H. Obesity-Related Glomerulopathy: Body Mass Index and Proteinuria. Clin. J. Am. Soc. Nephrol. 2010, 5, 1401–1409. [Google Scholar] [CrossRef] [Green Version]
- Bayliss, G.; Weinrauch, L.A.; D’Elia, J.A. Pathophysiology of Obesity-Related Renal Dysfunction Contributes to Diabetic Nephropathy. Curr. Diabetes Rep. 2012, 12, 440–446. [Google Scholar] [CrossRef]
- Jefferson, J.; Shankland, S.; Pichler, R. Proteinuria in diabetic kidney disease: A mechanistic viewpoint. Kidney Int. 2008, 74, 22–36. [Google Scholar] [CrossRef] [Green Version]
- Chawla, T.; Sharma, D.; Singh, A. Role of the renin angiotensin system in diabetic nephropathy. World J. Diabetes 2010, 1, 141–145. [Google Scholar] [CrossRef]
- Erkan, E. Proteinuria and progression of glomerular diseases. Pediatr. Nephrol. 2013, 28, 1049–1058. [Google Scholar] [CrossRef]
- Andersen, S.; Tarnow, L.; Rossing, P.; Hansen, B.V.; Parving, H.H. Renoprotective effects of angiotensin II receptor blockade in type 1 diabetic patients with diabetic nephropathy. Kidney Int. 2000, 57, 601–606. [Google Scholar] [CrossRef] [PubMed]
- Neuhofer, W.; Pittrow, D. Role of endothelin and endothelin receptor antagonists in renal disease. Eur. J. Clin. Investig. 2006, 36 (Suppl. S3), 78–88. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Harris, R.C. Role of Endothelial Nitric Oxide Synthase in Diabetic Nephropathy: Lessons from Diabetic eNOS Knockout Mice. J. Diabetes Res. 2014, 2014, 1–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawanami, D.; Takashi, Y.; Tanabe, M. Significance of Metformin Use in Diabetic Kidney Disease. Int. J. Mol. Sci. 2020, 21, 4239. [Google Scholar] [CrossRef] [PubMed]
- Amini, F.G.; Rafieian-Kopaei, M.; Nematbakhsh, M.; Baradaran, A.; Nasri, H. Ameliorative effects of metformin on renal histologic and biochemical alterations of gentamicin-induced renal toxicity in Wistar rats. J. Res. Med. Sci. 2012, 17, 621–625. [Google Scholar]
- Reed, M.; Meszaros, K.; Entes, L.; Claypool, M.; Pinkett, J.; Gadbois, T.; Reaven, G. A new rat model of type 2 diabetes: The fat-fed, streptozotocin-treated rat. Metabolism 2000, 49, 1390–1394. [Google Scholar] [CrossRef]
- Al-Ani, B.; ShamsEldeen, A.M. Lipopolysaccharide induces acute lung injury and alveolar haemorrhage in association with the cytokine storm, coagulopathy and AT1R/JAK/STAT augmentation in a rat model that mimics moderate and severe COVID-19 pathology. Clin. Exp. Pharmacol. Physiol. 2022, 49, 483–491. [Google Scholar] [CrossRef]
- Al-Ani, B.; AlZamil, N.M.; Hewett, P.W.; Al-Hashem, F.; Bin-Jaliah, I.; Shatoor, A.S.; Kamar, S.S.; Latif, N.S.A.; Haidara, M.A.; Dawood, A.F. Metformin ameliorates ROS-p53-collagen axis of fibrosis and dyslipidemia in type 2 diabetes mellitus-induced left ventricular injury. Arch. Physiol. Biochem. 2021, 1–7. [Google Scholar] [CrossRef]
- Wynne, B.M.; Chiao, C.-W.; Webb, R.C. Vascular smooth muscle cell signaling mechanisms for contraction to angiotensin II and endothelin-1. J. Am. Soc. Hypertens. 2009, 3, 84–95. [Google Scholar] [CrossRef] [Green Version]
- Higuchi, S.; Ohtsu, H.; Suzuki, H.; Shirai, H.; Frank, G.D.; Eguchi, S. Angiotensin II signal transduction through the AT1 receptor: Novel insights into mechanisms and pathophysiology. Clin. Sci. 2007, 112, 417–428. [Google Scholar] [CrossRef] [Green Version]
- Cardillo, C.; Campia, U.; Bryant, M.B.; Panza, J.A. Increased activity of endogenous endothelin in patients with type II diabetes mellitus. Circulation 2002, 106, 1783–1787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heemskerk, S.; Pickkers, P.; Bouw, M.P.; Draisma, A.; van der Hoeven, J.G.; Peters, W.H.; Smits, P.; Russel, F.G.; Masereeuw, R. Upregulation of Renal Inducible Nitric Oxide Synthase during Human Endotoxemia and Sepsis Is Associated with Proximal Tubule Injury. Clin. J. Am. Soc. Nephrol. 2006, 1, 853–862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rincón, J.; Correia, D.; Arcaya, J.; Finol, E.; Fernández, A.; Pérez, M.; Yaguas, K.; Talavera, E.; Chávez, M.; Summer, R.; et al. Role of Angiotensin II type 1 receptor on renal NAD(P)H oxidase, oxidative stress and inflammation in nitric oxide inhibition induced-hypertension. Life Sci. 2015, 124, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Sakuma, H.; Hagiwara, S.; Kantharidis, P.; Gohda, T.; Suzuki, Y. Potential Targeting of Renal Fibrosis in Diabetic Kidney Disease Using MicroRNAs. Front. Pharmacol. 2020, 11, 587689. [Google Scholar] [CrossRef] [PubMed]
- Naito, T.; Ma, L.-J.; Yang, H.; Zuo, Y.; Tang, Y.; Han, J.Y.; Kon, V.; Fogo, A.B. Angiotensin type 2 receptor actions contribute to angiotensin type 1 receptor blocker effects on kidney fibrosis. Am. J. Physiol. Physiol. 2010, 298, F683–F691. [Google Scholar] [CrossRef] [Green Version]
- Zhang, D.; Yang, H.; Kong, X.; Wang, K.; Mao, X.; Yan, X.; Wang, Y.; Liu, S.; Zhang, X.; Li, J.; et al. Proteomics analysis reveals diabetic kidney as a ketogenic organ in type 2 diabetes. Am. J. Physiol. Metab. 2011, 300, E287–E295. [Google Scholar] [CrossRef]
- Postma, C.; Klappe, E.; Dekker, H.; Thien, T. The prevalence of renal artery stenosis among patients with diabetes mellitus. Eur. J. Intern. Med. 2012, 23, 639–642. [Google Scholar] [CrossRef]
- Dalla Vestra, M.; Saller, A.; Bortoloso, E.; Mauer, M.; Fioretto, P. Structural involvement in type 1 and type 2 diabetic nephropathy. Diabetes Metab. 2000, 26 (Suppl. S4), 8–14. [Google Scholar]
- Cohall, D.; Ojeh, N.; Ferrario, C.M.; Adams, O.P.; Nunez-Smith, M. Is hypertension in African-descent populations contributed to by an imbalance in the activities of the ACE2/Ang-(1–7)/Mas and the ACE/Ang II/AT(1) axes? J. Renin-Angiotensin-Aldosterone Syst. 2020, 21, 1470320320908186. [Google Scholar] [CrossRef] [Green Version]
- Liang, Y.; Deng, H.; Bi, S.; Cui, Z.; Lata, A.; Zheng, D.; Wang, Y. Urinary Angiotensin Converting Enzyme 2 Increases in Patients with Type 2 Diabetic Mellitus. Kidney Blood Press. Res. 2015, 40, 101–110. [Google Scholar] [CrossRef]
- Ozaki, N.; Nomura, Y.; Sobajima, H.; Kondo, K.; Oiso, Y. Comparison of the effects of three angiotensin II receptor type 1 blockers on metabolic parameters in hypertensive patients with type 2 diabetes mellitus. Eur. J. Intern. Med. 2010, 21, 236–239. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Wang, X.; Wang, J.; Chen, C.; Wang, N.; Xu, Z.; Zeng, C. Chronic NF-κB blockade improves renal angiotensin II type 1 receptor functions and reduces blood pressure in Zucker diabetic rats. Cardiovasc. Diabetol. 2015, 14, 76. [Google Scholar] [CrossRef] [Green Version]
- Zanchi, A.; Moczulski, D.K.; Hanna, L.S.; Wantman, M.; Warram, J.H.; Krolewski, A.S. Risk of advanced diabetic nephropathy in type 1 diabetes is associated with endothelial nitric oxide synthase gene polymorphism. Kidney Int. 2000, 57, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Dhar, I.; Dhar, A.; Wu, L.; Desai, K.M. Increased Methylglyoxal Formation with Upregulation of Renin Angiotensin System in Fructose Fed Sprague Dawley Rats. PLoS ONE 2013, 8, e74212. [Google Scholar] [CrossRef]
- Kohan, D.E.; Barton, M. Endothelin and endothelin antagonists in chronic kidney disease. Kidney Int. 2014, 86, 896–904. [Google Scholar] [CrossRef] [Green Version]
- Barton, M.; Yanagisawa, M. Endothelin: 20 years from discovery to therapy. Can. J. Physiol. Pharmacol. 2008, 86, 485–498. [Google Scholar] [CrossRef] [PubMed]
- Su, E.; Zhao, L.; Yang, X.; Zhu, B.; Liu, Y.; Zhao, W.; Wang, X.; Qi, D.; Zhu, L.; Gao, C. Aggravated endothelial endocrine dysfunction and intimal thickening of renal artery in high-fat diet-induced obese pigs following renal denervation. BMC Cardiovasc. Disord. 2020, 20, 176. [Google Scholar] [CrossRef] [Green Version]
- Maguire, J.J.; Kuc, R.E.; O’Reilly, G.; Davenport, A.P. Vasoconstrictor endothelin receptors characterized in human renal artery and vein in vitro. Br. J. Pharmacol. 1994, 113, 49–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diamanti-Kandarakis, E.; Spina, G.; Kouli, C.; Migdalis, I. Increased endothelin-1 levels in women with polycystic ovary syndrome and the beneficial effect of metformin therapy. J. Clin. Endocrinol. Metab. 2001, 86, 4666–4673. [Google Scholar] [CrossRef]
- Yoshida, T.; Matsuura, K.; Goya, S.; Ma, D.; Shimada, K.; Kitpipatkun, P.; Namiki, R.; Uemura, A.; Suzuki, K.; Tanaka, R. Metformin prevents the development of monocrotaline-induced pulmonary hypertension by decreasing serum levels of big endothelin-1. Exp. Ther. Med. 2020, 20, 149. [Google Scholar] [CrossRef]
| Animal Groups | hs-CRP (μg/mL) | TNF-α (pg/mL) | IL-6 (pg/mL) | MDA (nmol/L) | SOD (U/L) | GPx (nmol/min/mL) |
|---|---|---|---|---|---|---|
| Control | 1.22 ± 0.28 | 33.32 ± 2.26 | 16.60 ± 4.91 | 13.44 ± 2.97 | 2.41 ± 0.40 | 161.3 ± 9.07 |
| T2DM | 8.24 ± 2.10 a | 113.00 ± 7.93 a | 118.70 ± 6.85 a | 80.44 ± 6.42 a | 0.74 ± 0.160 a | 80.57 ± 5.62 a |
| Met + T2DM | 4.29 ± 1.31 ab | 55.29 ± 13.57 ab | 37.29 ± 10.25 ab | 28.09 ± 11.46 ab | 2.07 ± 0.52 b | 114.6 ± 5.29 ab |
| Animal Groups | Urine Albumin (mg/24 h) | Ketonuria (mmol/L) | Urine Specific Gravity (pg/mL) | Urea | Creatinine (mg/dL) | Body Weight (gram) |
|---|---|---|---|---|---|---|
| Control | 13.71 ± 3.69 | 0.00 ± 0.00 | 1005.83 ± 2.04 | 37.67 ± 12.60 | 0.17 ± 0.06 | 270.0 ± 5.25 |
| T2DM | 42.86 ± 4.67 a | 5.54 ± 2.25 a | 1030.0 ± 0.00 a | 78.75 ± 15.49 a | 1.05 ± 0.32 a | 163.3 ± 7.52 a |
| Met + T2DM | 24.57 ± 6.02 ab | 1.18 ± 1.64 b | 1020.83 ± 5.85 ab | 49.89 ± 11.21b | 0.533 ± 0.23 ab | 305.83 ± 31.05 ab |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dawood, A.F.; Maarouf, A.; Alzamil, N.M.; Momenah, M.A.; Shati, A.A.; Bayoumy, N.M.; Kamar, S.S.; Haidara, M.A.; ShamsEldeen, A.M.; Yassin, H.Z.; et al. Metformin Is Associated with the Inhibition of Renal Artery AT1R/ET-1/iNOS Axis in a Rat Model of Diabetic Nephropathy with Suppression of Inflammation and Oxidative Stress and Kidney Injury. Biomedicines 2022, 10, 1644. https://doi.org/10.3390/biomedicines10071644
Dawood AF, Maarouf A, Alzamil NM, Momenah MA, Shati AA, Bayoumy NM, Kamar SS, Haidara MA, ShamsEldeen AM, Yassin HZ, et al. Metformin Is Associated with the Inhibition of Renal Artery AT1R/ET-1/iNOS Axis in a Rat Model of Diabetic Nephropathy with Suppression of Inflammation and Oxidative Stress and Kidney Injury. Biomedicines. 2022; 10(7):1644. https://doi.org/10.3390/biomedicines10071644
Chicago/Turabian StyleDawood, Amal F., Amro Maarouf, Norah M. Alzamil, Maha A. Momenah, Ayed A. Shati, Nervana M. Bayoumy, Samaa S. Kamar, Mohamed A. Haidara, Asmaa M. ShamsEldeen, Hanaa Z. Yassin, and et al. 2022. "Metformin Is Associated with the Inhibition of Renal Artery AT1R/ET-1/iNOS Axis in a Rat Model of Diabetic Nephropathy with Suppression of Inflammation and Oxidative Stress and Kidney Injury" Biomedicines 10, no. 7: 1644. https://doi.org/10.3390/biomedicines10071644
APA StyleDawood, A. F., Maarouf, A., Alzamil, N. M., Momenah, M. A., Shati, A. A., Bayoumy, N. M., Kamar, S. S., Haidara, M. A., ShamsEldeen, A. M., Yassin, H. Z., Hewett, P. W., & Al-Ani, B. (2022). Metformin Is Associated with the Inhibition of Renal Artery AT1R/ET-1/iNOS Axis in a Rat Model of Diabetic Nephropathy with Suppression of Inflammation and Oxidative Stress and Kidney Injury. Biomedicines, 10(7), 1644. https://doi.org/10.3390/biomedicines10071644






