New Insights into the Neurodegeneration Mechanisms Underlying Riboflavin Transporter Deficiency (RTD): Involvement of Energy Dysmetabolism and Cytoskeletal Derangement
Abstract
:1. Introduction
2. Riboflavin Transporter Deficiency: From Genetics to Clinical Presentation
| General Information | ||
|---|---|---|
| Name | Riboflavin Transporter Deficiency; Brown-Vialetto-Van Laere Syndrome | |
| Prevalence | <1/1,000,000 | |
| Inheritance | Autosomal recessive, rarely autosomal dominant | |
| Gene Mutations | SLC52A2 on chromosome 8q24; SLC52A3 on chromosome 20p13 | |
| Cases | ~325 genetically confirmed cases (http://curertd.org/what-is-rtd/history/(accessed on 10 April 2022) Underestimated data [22] | |
| Age of Onset | From few months to early teen years; very rarely adulthood | |
| Diagnosis | Mutational analysis of all genes coding riboflavin transporters;Biochemical tests showing abnormalities such as altered plasma acylcarnitine profiles, abnormal urine organic acids and decreased plasma flavin levels(in 50% of RTD patients) | |
| Treatment | RF supplementation from 10 to 80 mg/kilogram bodyweight/day (400 mg to 2700 mg daily for adults) divided into 2, 3 or 4 doses per day | |
| Response to Rf Treatment | Highly variable, ranging from rapid improvement in days to gradual improvement over several years or stabilization of clinical state.No response is also observed. | |
| Clinical Presentation | Common features include peripheral and cranial neuropathy, neuronal loss in anterior horns and atrophy of spinal sensory tracts, causing muscle weakness, sensory loss, diaphragmatic paralysis and respiratory insufficiency, and multiple cranial nerve deficits such as sensorineural hearing loss, bulbar symptoms, and loss of vision due to optic atrophy | |
| Major Manifestations Associated with the Mutated Genes | SLC52A2 (n = 73) | SLC52A3 (n = 45) |
| Auditory Neuropathy | 33% | 75% * |
| Pontobulbar Palsy | 8% | 20% * |
| Sensory Gait Ataxia | 64% | 5% * |
| Optic Atrophy w/o Nnystagmus | 29% | - |
| Muscle Weakness | 26% | 15% * |
| Respiratory Compromise | 8% | 10% * |
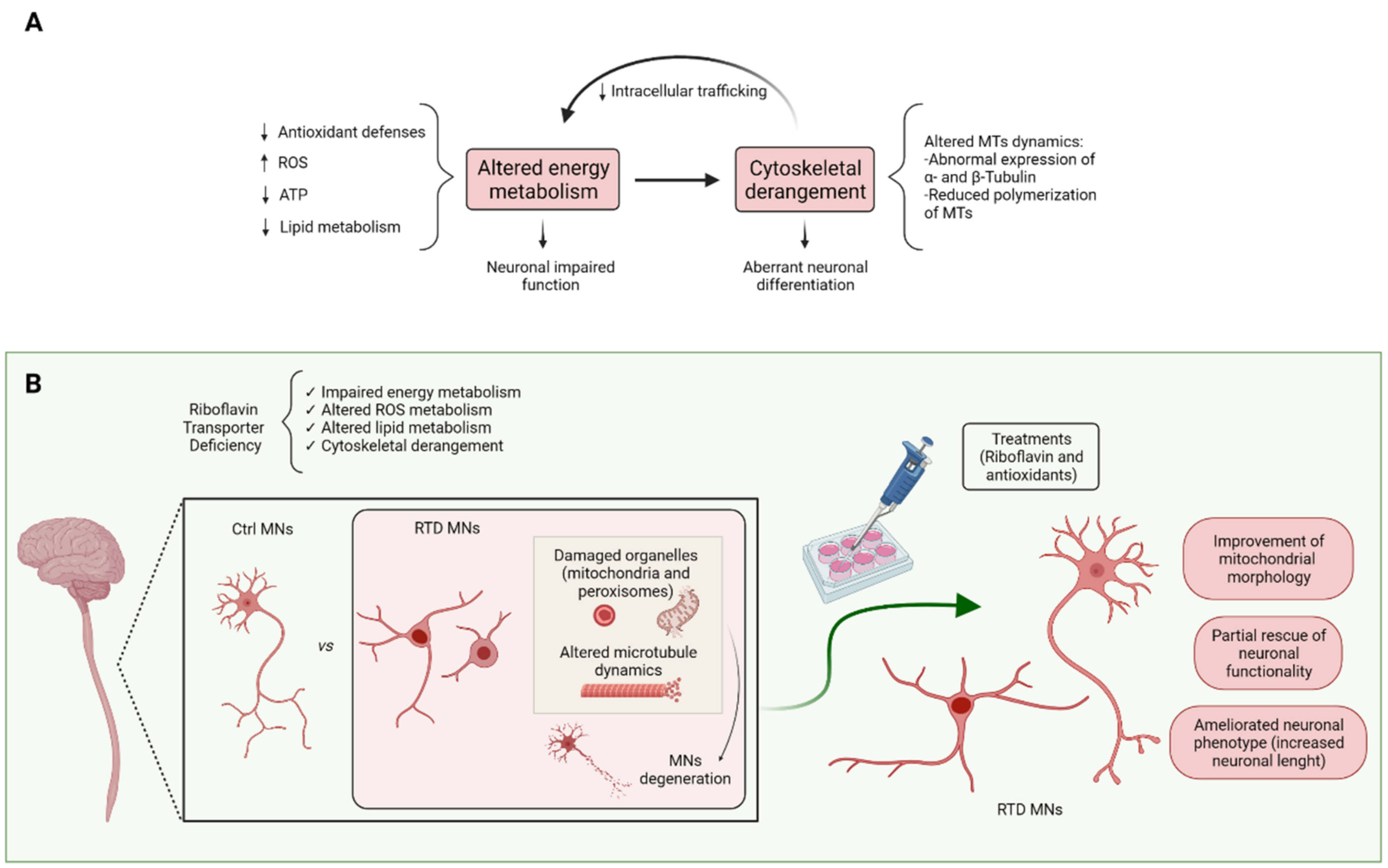
3. Molecular Mechanisms Underlying RTD Pathogenesis
3.1. Dysfunctional Metabolic Pathways Depending on Riboflavin and Its Derivatives
3.1.1. Lipid Metabolism
3.1.2. ROS Metabolism
4. Cytoskeletal Involvement in RTD
5. In Vivo and In Vitro Models of RTD
6. Therapeutic Prospects for RTD
7. Perspective
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tolomeo, M.; Nisco, A.; Leone, P.; Barile, M. Development of Novel Experimental Models to Study Flavoproteome Alterations in Human Neuromuscular Diseases: The Effect of Rf Therapy. Int. J. Mol. Sci. 2020, 21, 5310. [Google Scholar] [CrossRef] [PubMed]
- Ross, N.S.; Hansen, T.P. Riboflavin deficiency is associated with selective preservation of critical flavoenzyme-dependent metabolic pathways. Biofactors 1992, 3, 185–190. [Google Scholar] [PubMed]
- Zhang, L.; Keung, W.; Samokhvalov, V.; Wang, W.; Lopaschuk, G.D. Role of fatty acid uptake and fatty acid beta-oxidation in mediating insulin resistance in heart and skeletal muscle. Biochim. Biophys. Acta 2010, 1801, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Mishra, P. Interfaces between mitochondrial dynamics and disease. Cell Calcium 2016, 60, 190–198. [Google Scholar] [CrossRef]
- Nunnari, J.; Suomalainen, A. Mitochondria: In Sickness and in Health. Cell 2012, 148, 1145–1159. [Google Scholar] [CrossRef] [Green Version]
- Colasuonno, F.; Niceforo, A.; Marioli, C.; Fracassi, A.; Stregapede, F.; Massey, K.; Tartaglia, M.; Bertini, E.; Compagnucci, C.; Moreno, S. Mitochondrial and Peroxisomal Alterations Contribute to Energy Dysmetabolism in Riboflavin Transporter Deficiency. Oxid. Med. Cell. Longev. 2020, 2020, 6821247. [Google Scholar] [CrossRef]
- Valencia, A.; Morán, J. Reactive oxygen species induce different cell death mechanisms in cultured neurons. Free Radic. Biol. Med. 2004, 36, 1112–1125. [Google Scholar] [CrossRef]
- Boldyrev, A.; Song, R.; Dyatlov, V.A.; Lawrence, D.A.; Carpenter, D.O. Neuronal cell death and reactive oxygen species. Cell. Mol. Neurobiol. 2000, 20, 433–450. [Google Scholar] [CrossRef]
- Redza-Dutordoir, M.; Averill-Bates, D.A. Activation of apoptosis signalling pathways by reactive oxygen species. Biochim. Biophys. Acta 2016, 1863, 2977–2992. [Google Scholar] [CrossRef]
- Golpich, M.; Amini, E.; Mohamed, Z.; Azman Ali, R.; Mohamed Ibrahim, N.; Ahmadiani, A. Mitochondrial Dysfunction and Biogenesis in Neurodegenerative diseases: Pathogenesis and Treatment. CNS Neurosci. Ther. 2017, 23, 5–22. [Google Scholar] [CrossRef]
- O’Callaghan, B.; Bosch, A.M.; Houlden, H. An update on the genetics, clinical presentation, and pathomechanisms of human riboflavin transporter deficiency. J. Inherit. Metab. Dis. 2019, 42, 598–607. [Google Scholar] [CrossRef]
- Niceforo, A.; Marioli, C.; Colasuonno, F.; Petrini, S.; Massey, K.; Tartaglia, M.; Bertini, E.; Moreno, S.; Compagnucci, C. Altered cytoskeletal arrangement in induced pluripotent stem cells (iPSCs) and motor neurons from patients with riboflavin transporter deficiency. Dis. Model. Mech. 2021, 14, dmm046391. [Google Scholar] [CrossRef]
- Chang, C.Y.; Ting, H.C.; Liu, C.A.; Su, H.L.; Chiou, T.W.; Harn, H.J.; Lin, S.Z. Induced Pluripotent Stem Cells: A Powerful Neurodegenerative Disease Modeling Tool for Mechanism Study and Drug Discovery. Cell Transpl. 2018, 27, 1588–1602. [Google Scholar] [CrossRef] [Green Version]
- Green, P.; Wiseman, M.; Crow, Y.J.; Houlden, H.; Riphagen, S.; Lin, J.P.; Raymond, F.L.; Childs, A.M.; Sheridan, E.; Edwards, S.; et al. Brown-Vialetto-Van Laere syndrome, a ponto-bulbar palsy with deafness, is caused by mutations in c20orf54. Am. J. Hum. Genet. 2010, 86, 485–489. [Google Scholar] [CrossRef] [Green Version]
- Jin, C.; Yonezawa, A. Recent advances in riboflavin transporter RFVT and its genetic disease. Pharm. Ther. 2022, 233, 108023. [Google Scholar] [CrossRef]
- Tolomeo, M.; Nisco, A.; Barile, M. Alteration of Flavin Cofactor Homeostasis in Human Neuromuscular Pathologies. Methods Mol. Biol. 2021, 2280, 275–295. [Google Scholar]
- Barile, M.; Giancaspero, T.A.; Leone, P.; Galluccio, M.; Indiveri, C. Riboflavin transport and metabolism in humans. J. Inherit. Metab. Dis. 2016, 39, 545–557. [Google Scholar] [CrossRef]
- Amir, F.; Atzinger, C.; Massey, K.; Greinwald, J.; Hunter, L.L.; Ulm, E.; Kettler, M. The Clinical Journey of Patients with Riboflavin Transporter Deficiency Type 2. J. Child Neurol. 2020, 35, 283–290. [Google Scholar] [CrossRef]
- Hustad, S.; McKinley, M.C.; McNulty, H.; Schneede, J.; Strain, J.J.; Scott, J.M.; Ueland, P.M. Riboflavin, flavin mononucleotide, and flavin adenine dinucleotide in human plasma and erythrocytes at baseline and after low-dose riboflavin supplementation. Clin. Chem. 2002, 48, 1571–1577. [Google Scholar] [CrossRef]
- Buehler, B.A. Vitamin B2: Riboflavin. J. Evid. Based Complement. Altern. Med. 2011, 16, 88–90. [Google Scholar] [CrossRef]
- Manole, A.; Jaunmuktane, Z.; Hargreaves, I.; Ludtmann, M.H.R.; Salpietro, V.; Bello, O.D.; Pope, S.; Pandraud, A.; Horga, A.; Scalco, R.S.; et al. Clinical, pathological and functional characterization of riboflavin-responsive neuropathy. Brain 2017, 140, 2820–2837. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allison, T.; Roncero, I.; Forsyth, R.; Coffman, K.; Pichon, J.L. Brown-Vialetto-Van Laere Syndrome as a Mimic of Neuroimmune Disorders: 3 Cases from the Clinic and Review of the Literature. J. Child Neurol. 2017, 32, 528–532. [Google Scholar] [CrossRef] [PubMed]
- Lienhart, W.D.; Gudipati, V.; Macheroux, P. The human flavoproteome. Arch. Biochem. Biophys. 2013, 535, 150–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mosegaard, S.; Dipace, G.; Bross, P.; Carlsen, J.; Gregersen, N.; Olsen, R. Riboflavin Deficiency-Implications for General Human Health and Inborn Errors of Metabolism. Int. J. Mol. Sci. 2020, 21, 3847. [Google Scholar] [CrossRef]
- Demarquoy, J.; Le Borgne, F. Crosstalk between mitochondria and peroxisomes. World J. Biol. Chem. 2015, 6, 301–309. [Google Scholar] [CrossRef]
- DeBose-Boyd, R.A. Significance and regulation of lipid metabolism. Semin. Cell Dev. Biol. 2018, 81, 97. [Google Scholar] [CrossRef]
- Wanders, R.J.; Waterham, H.R.; Ferdinandusse, S. Metabolic Interplay between Peroxisomes and Other Subcellular Organelles Including Mitochondria and the Endoplasmic Reticulum. Front. Cell Dev. Biol. 2016, 3, 83. [Google Scholar] [CrossRef] [Green Version]
- Braverman, N.E.; D’Agostino, M.D.; Maclean, G.E. Peroxisome biogenesis disorders: Biological, clinical and pathophysiological perspectives. Dev. Disabil. Res. Rev. 2013, 17, 187–196. [Google Scholar] [CrossRef]
- Cipolla, C.M.; Lodhi, I.J. Peroxisomal Dysfunction in Age-Related Diseases. Trends Endocrinol. Metab. 2017, 28, 297–308. [Google Scholar] [CrossRef] [Green Version]
- Islinger, M.; Voelkl, A.; Fahimi, H.D.; Schrader, M. The peroxisome: An update on mysteries 2.0. Histochem. Cell Biol. 2018, 150, 443–471. [Google Scholar] [CrossRef] [Green Version]
- Wang, B.; Van Veldhoven, P.P.; Brees, C.; Rubio, N.; Nordgren, M.; Apanasets, O.; Kunze, M.; Baes, M.; Agostinis, P.; Fransen, M. Mitochondria are targets for peroxisome-derived oxidative stress in cultured mammalian cells. Free Radic. Biol. Med. 2013, 65, 882–894. [Google Scholar] [CrossRef] [Green Version]
- Gandhi, S.; Abramov, A.Y. Mechanism of oxidative stress in neurodegeneration. Oxid. Med. Cell Longev. 2012, 2012, 428010. [Google Scholar] [CrossRef] [Green Version]
- Kim, G.H.; Kim, J.E.; Rhie, S.J.; Yoon, S. Role Oxidative Stress Neurodegener. Diseases Exp. Neurobiol. 2015, 24, 325–340. [Google Scholar] [CrossRef]
- Wu, Z.; Du, Y.; Xue, H.; Wu, Y.; Zhou, B. Aluminum induces neurodegeneration and its toxicity arises from increased iron accumulation and reactive oxygen species (ROS) production. Neurobiol. Aging 2012, 33, 199.e1–199.e12. [Google Scholar] [CrossRef]
- Fatokun, A.A.; Stone, T.W.; Smith, R.A. Oxidative stress in neurodegeneration and available means of protection. Front. Biosci. 2008, 13, 3288–3311. [Google Scholar] [CrossRef]
- Uttara, B.; Singh, A.V.; Zamboni, P.; Mahajan, R.T. Oxidative stress and neurodegenerative diseases: A review of upstream and downstream antioxidant therapeutic options. Curr. Neuropharmacol. 2009, 7, 65–74. [Google Scholar] [CrossRef] [Green Version]
- Salim, S. Oxidative Stress and the Central Nervous System. J. Pharmacol. Exp. Ther. 2017, 360, 201–205. [Google Scholar] [CrossRef]
- Fransen, M.; Nordgren, M.; Wang, B.; Apanasets, O. Role of peroxisomes in ROS/RNS-metabolism: Implications for human disease. Biochim. Biophys. Acta 2012, 1822, 1363–1373. [Google Scholar] [CrossRef] [Green Version]
- Plett, A.; Charton, L.; Linka, N. Peroxisomal Cofactor Transport. Biomolecules 2020, 10, 1174. [Google Scholar] [CrossRef]
- Park, J.C.; Jang, S.Y.; Lee, D.; Lee, J.; Kang, U.; Chang, H.; Kim, H.J.; Han, S.H.; Seo, J.; Choi, M.; et al. A logical network-based drug-screening platform for Alzheimer’s disease representing pathological features of human brain organoids. Nat. Commun. 2021, 12, 280. [Google Scholar] [CrossRef]
- Antonenkov, V.D.; Grunau, S.; Ohlmeier, S.; Hiltunen, J.K. Peroxisomes are oxidative organelles. Antioxid. Redox Signal. 2010, 13, 525–537. [Google Scholar] [CrossRef] [PubMed]
- Lismont, C.; Nordgren, M.; Van Veldhoven, P.P.; Fransen, M. Redox interplay between mitochondria and peroxisomes. Front. Cell Dev. Biol. 2015, 3, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colasuonno, F.; Bertini, E.; Tartaglia, M.; Compagnucci, C.; Moreno, S. Mitochondrial Abnormalities in Induced Pluripotent Stem Cells-Derived Motor Neurons from Patients with Riboflavin Transporter Deficiency. Antioxidants 2020, 9, 1252. [Google Scholar] [CrossRef] [PubMed]
- Leone, P.; Tolomeo, M.; Piancone, E.; Puzzovio, P.G.; De Giorgi, C.; Indiveri, C.; Di Schiavi, E.; Barile, M. Mimicking human riboflavin responsive neuromuscular disorders by silencing flad-1 gene in C. elegans: Alteration of vitamin transport and cholinergic transmission. IUBMB Life 2021. [Google Scholar] [CrossRef]
- Pollak, D.; Cairns, N.; Lubec, G. Cytoskeleton derangement in brain of patients with Down syndrome, Alzheimer’s disease and Pick’s disease. J. Neural. Transm. Suppl. 2003, 67, 149–158. [Google Scholar]
- Didonna, A.; Opal, P. The role of neurofilament aggregation in neurodegeneration: Lessons from rare inherited neurological disorders. Mol. Neurodegener. 2019, 14, 19. [Google Scholar] [CrossRef]
- Sparaco, M.; Gaeta, L.M.; Tozzi, G.; Bertini, E.; Pastore, A.; Simonati, A.; Santorelli, F.M.; Piemonte, F. Protein glutathionylation in human central nervous system: Potential role in redox regulation of neuronal defense against free radicals. J. Neurosci. Res. 2006, 83, 256–263. [Google Scholar] [CrossRef]
- Munnamalai, V.; Suter, D.M. Reactive oxygen species regulate F-actin dynamics in neuronal growth cones and neurite outgrowth. J. Neurochem. 2009, 108, 644–661. [Google Scholar] [CrossRef] [Green Version]
- Wilson, C.; González-Billault, C. Regulation of cytoskeletal dynamics by redox signaling and oxidative stress: Implications for neuronal development and trafficking. Front. Neurosci. 2015, 9, 381. [Google Scholar] [CrossRef] [Green Version]
- Rizzo, F.; Ramirez, A.; Compagnucci, C.; Salani, S.; Melzi, V.; Bordoni, A.; Fortunato, F.; Niceforo, A.; Bresolin, N.; Comi, G.P.; et al. Genome-wide RNA-seq of iPSC-derived motor neurons indicates selective cytoskeletal perturbation in Brown-Vialetto disease that is partially rescued by riboflavin. Sci. Rep. 2017, 7, 46271. [Google Scholar] [CrossRef]
- Islam, M.S.; Kabir, A.M.; Inoue, D.; Sada, K.; Kakugo, A. Enhanced dynamic instability of microtubules in a ROS free inert environment. Biophys. Chem. 2016, 211, 1–8. [Google Scholar] [CrossRef]
- Marioli, C.; Magliocca, V.; Petrini, S.; Niceforo, A.; Borghi, R.; Petrillo, S.; La Rosa, P.; Colasuonno, F.; Persichini, T.; Piemonte, F.; et al. Antioxidant Amelioration of Riboflavin Transporter Deficiency in Motoneurons Derived from Patient-Specific Induced Pluripotent Stem Cells. Int. J. Mol. Sci. 2020, 21, 7402. [Google Scholar] [CrossRef]
- Ashoori, M.; Saedisomeolia, A. Riboflavin (vitamin B₂) and oxidative stress: A review. Br. J. Nutr. 2014, 111, 1985–1991. [Google Scholar]
- Intoh, A.; Suzuki, N.; Koszka, K.; Eggan, K. SLC52A3, A Brown-Vialetto-van Laere syndrome candidate gene is essential for mouse development, but dispensable for motor neuron differentiation. Hum. Mol. Genet. 2016, 25, 1814–1823. [Google Scholar] [CrossRef] [Green Version]
- Yoshimatsu, H.; Yonezawa, A.; Yao, Y.; Sugano, K.; Nakagawa, S.; Omura, T.; Matsubara, K. Functional involvement of RFVT3/SLC52A3 in intestinal riboflavin absorption. Am. J. Physiol.-Gastrointest. Liver Physiol 2014, 306, G102–G110. [Google Scholar] [CrossRef]
- Spiekerkoetter, U.; Wood, P.A. Mitochondrial fatty acid oxidation disorders: Pathophysiological studies in mouse models. J. Inherit. Metab. Dis. 2010, 33, 539–546. [Google Scholar] [CrossRef] [Green Version]
- Subramanian, V.S.; Lambrecht, N.; Lytle, C.; Said, H.M. Conditional (intestinal-specific) knockout of the riboflavin transporter-3 (RFVT-3) impairs riboflavin absorption. Am. J. Physiol.-Gastrointest. Liver Physiol. 2016, 310, G285–G293. [Google Scholar] [CrossRef] [Green Version]
- Jin, C.; Yonezawa, A.; Yoshimatsu, H.; Imai, S.; Koyanagi, M.; Yamanishi, K.; Nakagawa, S.; Itohara, K.; Omura, T.; Nakagawa, T.; et al. Effect of riboflavin deficiency on development of the cerebral cortex in Slc52a3 knockout mice. Sci. Rep. 2020, 10, 18443. [Google Scholar] [CrossRef]
- Cornelius, N.; Frerman, F.E.; Corydon, T.J.; Palmfeldt, J.; Bross, P.; Gregersen, N.; Olsen, R.K. Molecular mechanisms of riboflavin responsiveness in patients with ETF-QO variations and multiple acyl-CoA dehydrogenation deficiency. Hum. Mol. Genet. 2012, 21, 3435–3448. [Google Scholar] [CrossRef] [Green Version]
- Faustino Martins, J.M.; Fischer, C.; Urzi, A.; Vidal, R.; Kunz, S.; Ruffault, P.L.; Kabuss, L.; Hube, I.; Gazzerro, E.; Birchmeier, C.; et al. Self-Organizing 3D Human Trunk Neuromuscular Organoids. Cell Stem Cell 2020, 26, 172–186.e6. [Google Scholar] [CrossRef]
- Lancaster, M.A.; Renner, M.; Martin, C.A.; Wenzel, D.; Bicknell, L.S.; Hurles, M.E.; Homfray, T.; Penninger, J.M.; Jackson, A.P.; Knoblich, J.A. Cerebral organoids model human brain development and microcephaly. Nature 2013, 501, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Tian, A.; Muffat, J.; Li, Y. Studying Human Neurodevelopment and Diseases Using 3D Brain Organoids. J. Neurosci. 2020, 40, 1186–1193. [Google Scholar] [CrossRef]
- Ciccolella, M.; Corti, S.; Catteruccia, M.; Petrini, S.; Tozzi, G.; Rizza, T.; Carrozzo, R.; Nizzardo, M.; Bordoni, A.; Ronchi, D.; et al. Riboflavin transporter 3 involvement in infantile Brown-Vialetto-Van Laere disease: Two novel mutations. J. Med. Genet. 2013, 50, 104–107. [Google Scholar] [CrossRef] [PubMed]
- Bosch, A.M.; Stroek, K.; Abeling, N.G.; Waterham, H.R.; Ijlst, L.; Wanders, R.J. The Brown-Vialetto-Van Laere and Fazio Londe syndrome revisited: Natural history, genetics, treatment and future perspectives. Orphanet J. Rare Dis. 2012, 7, 83. [Google Scholar] [CrossRef] [Green Version]
- Anand, G.; Hasan, N.; Jayapal, S.; Huma, Z.; Ali, T.; Hull, J.; Blair, E.; McShane, T.; Jayawant, S. Early use of high-dose riboflavin in a case of Brown-Vialetto-Van Laere syndrome. Dev. Med. Child Neurol. 2012, 54, 187–189. [Google Scholar] [CrossRef] [PubMed]
- Carreau, C.; Benoit, C.; Ahle, G.; Cauquil, C.; Roubertie, A.; Lenglet, T.; Cosgrove, J.; Meunier, I.; Veauville-Merllié, A.; Acquaviva-Bourdain, C.; et al. Late-onset riboflavin transporter deficiency: A treatable mimic of various motor neuropathy aetiologies. J. Neurol. Neurosurg. Psychiatry 2021, 92, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Rebec, G.V.; Pierce, R.C. A vitamin as neuromodulator: Ascorbate release into the extracellular fluid of the brain regulates dopaminergic and glutamatergic transmission. Prog. Neurobiol. 1994, 43, 537–565. [Google Scholar] [CrossRef]
- Shults, C.W. Coenzyme Q10 in neurodegenerative diseases. Curr. Med. Chem. 2003, 10, 1917–1921. [Google Scholar] [CrossRef]
- Carelli, V.; La Morgia, C.; Valentino, M.L.; Rizzo, G.; Carbonelli, M.; De Negri, A.M.; Sadun, F.; Carta, A.; Guerriero, S.; Simonelli, F.; et al. Idebenone treatment in Leber’s hereditary optic neuropathy. Brain 2011, 134, e188. [Google Scholar] [CrossRef]
- Enns, G.M.; Kinsman, S.L.; Perlman, S.L.; Spicer, K.M.; Abdenur, J.E.; Cohen, B.H.; Amagata, A.; Barnes, A.; Kheifets, V.; Shrader, W.D.; et al. Initial experience in the treatment of inherited mitochondrial disease with EPI-743. Mol. Genet. Metab. 2012, 105, 91–102. [Google Scholar] [CrossRef]
- Pastore, A.; Petrillo, S.; Tozzi, G.; Carrozzo, R.; Martinelli, D.; Dionisi-Vici, C.; Di Giovamberardino, G.; Ceravolo, F.; Klein, M.B.; Miller, G.; et al. Glutathione: A redox signature in monitoring EPI-743 therapy in children with mitochondrial encephalomyopathies. Mol. Genet. Metab. 2013, 109, 208–214. [Google Scholar] [CrossRef]
- Martinelli, D.; Catteruccia, M.; Piemonte, F.; Pastore, A.; Tozzi, G.; Dionisi-Vici, C.; Pontrelli, G.; Corsetti, T.; Livadiotti, S.; Kheifets, V.; et al. EPI-743 reverses the progression of the pediatric mitochondrial disease--genetically defined Leigh Syndrome. Mol. Genet. Metab. 2012, 107, 383–388. [Google Scholar] [CrossRef]
- La Rosa, P.; Russo, M.; D’Amico, J.; Petrillo, S.; Aquilano, K.; Lettieri-Barbato, D.; Turchi, R.; Bertini, E.S.; Piemonte, F. Nrf2 Induction Re-establishes a Proper Neuronal Differentiation Program in Friedreich’s Ataxia Neural Stem Cells. Front. Cell. Neurosci. 2019, 13, 356. [Google Scholar] [CrossRef] [Green Version]
- Kerr, D.S. Review of clinical trials for mitochondrial disorders: 1997-2012. Neurotherapeutics 2013, 10, 307–319. [Google Scholar] [CrossRef] [Green Version]
- Farioli-Vecchioli, S.; Moreno, S.; Cerù, M.P. Immunocytochemical localization of acyl-CoA oxidase in the rat central nervous system. J. Neurobiol. 2001, 30, 21–33. [Google Scholar]
- Scaricamazza, S.; Salvatori, I.; Ferri, A.; Valle, C. Skeletal Muscle in ALS: An Unappreciated Therapeutic Opportunity? Cells 2021, 10, 525. [Google Scholar] [CrossRef]
- Klionsky, D.J.; Abdel-Aziz, A.K.; Abdelfatah, S.; Abdellatif, M.; Abdoli, A.; Abel, S.; Abeliovich, H.; Abildgaard, M.H.; Abudu, Y.P.; Acevedo-Arozena, A.; et al. Guidelines for the use and interpretation of assays for monitoring autophagy (4th edition)1. Autophagy 2021, 17, 1–382. [Google Scholar] [CrossRef]
- Li, H.; Yang, Y.; Hong, W.; Huang, M.; Wu, M.; Zhao, X. Applications of genome editing technology in the targeted therapy of human diseases: Mechanisms, advances and prospects. Signal Transduct. Targe. 2020, 5, 1. [Google Scholar] [CrossRef]
- Paolini Sguazzi, G.; Muto, V.; Tartaglia, M.; Bertini, E.; Compagnucci, C. Induced Pluripotent Stem Cells (iPSCs) and Gene Therapy: A New Era for the Treatment of Neurological Diseases. Int. J. Mol. Sci. 2021, 22, 13674. [Google Scholar] [CrossRef]
- Cali, E.; Dominik, N.; Manole, A.; Houlden, H. Riboflavin Transporter Deficiency. In GeneReviews®; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Mierzaa, G.M., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 2015. [Google Scholar]

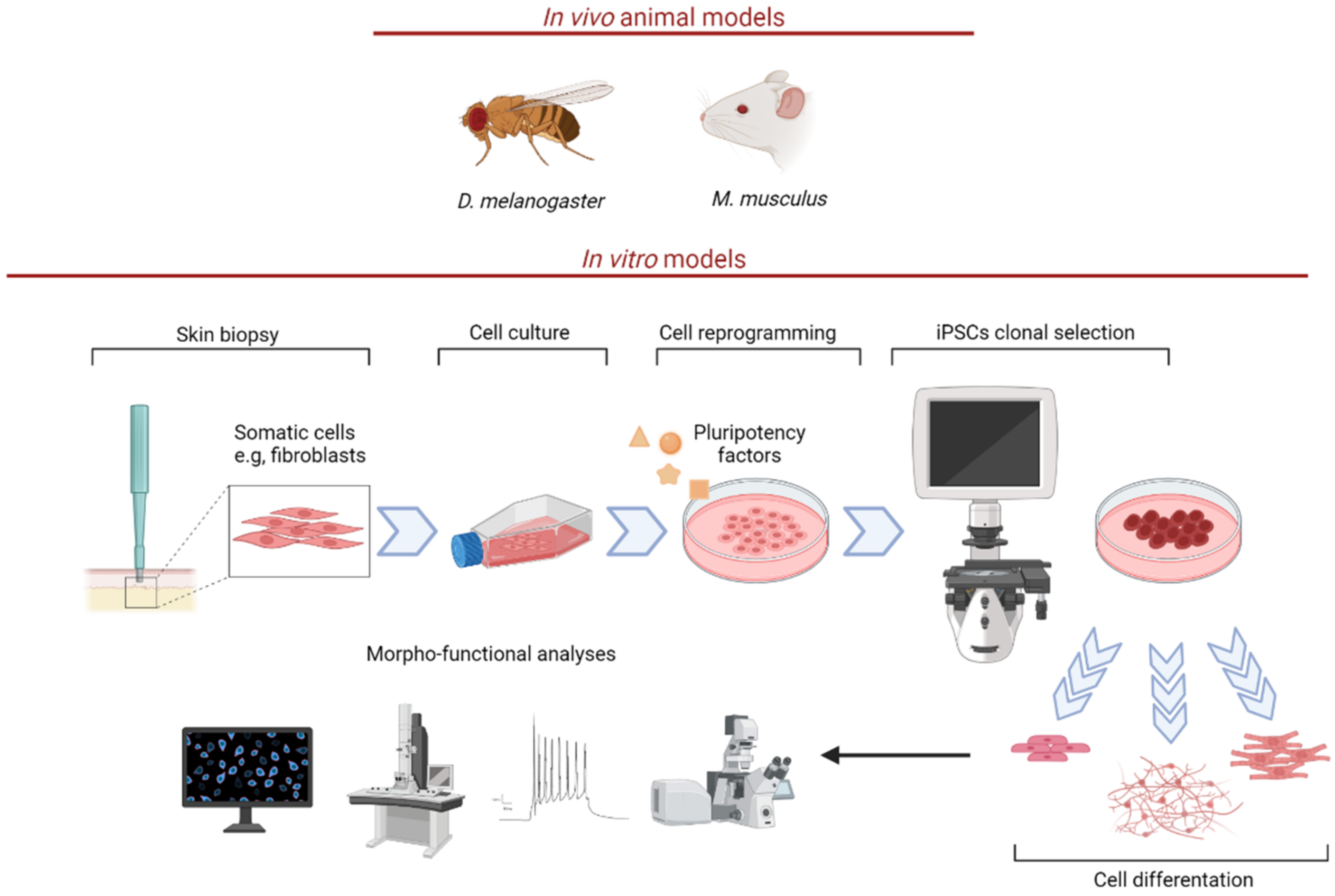
| RTD Models | |
|---|---|
| D. melanogaster | Drift knockdown results in abnormal mitochondrial morphology, reduced ETC activity, and lower MMP [21]. |
| M. musculus | Slc52a3+/− mice display same body weight and plasma RF concentration as in WT. Intercrossing between Slc52a2+/− mice fail to generate Slc52a2−/− mice, due to early embryonic lethality, for a failure in placental development [54]. Slc52a3−/− mice die from hyperlipidemia and hypoglycemia within 48 h after birth [55]. They show abnormal development of the cerebral cortex and altered brain morphology [55]. Slc52a3 conditional KO in the intestine also leads to early postnatal death (6–12 weeks) [57]. |
| Fibroblasts | Skin fibroblasts from two RTD patients carrying either SLC52A2 or SLC52A3 mutations show significant reduction in RF transport [63]. Skin fibroblasts from patients with SLC52A2 mutations reveal significant reduction in ETC complex I and II activity [21]. |
| iPSCs and MNs | iPSCs-derived MNs from RTD patients carrying SLC52A3 gene mutations show cytoskeletal perturbation [50]. iPSCs and iPSCs-derived MNs from RTD patients carrying SLC52A2 gene mutations show altered redox balance together with cytoskeletal derangement [6,12,43]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colasuonno, F.; Marioli, C.; Tartaglia, M.; Bertini, E.; Compagnucci, C.; Moreno, S. New Insights into the Neurodegeneration Mechanisms Underlying Riboflavin Transporter Deficiency (RTD): Involvement of Energy Dysmetabolism and Cytoskeletal Derangement. Biomedicines 2022, 10, 1329. https://doi.org/10.3390/biomedicines10061329
Colasuonno F, Marioli C, Tartaglia M, Bertini E, Compagnucci C, Moreno S. New Insights into the Neurodegeneration Mechanisms Underlying Riboflavin Transporter Deficiency (RTD): Involvement of Energy Dysmetabolism and Cytoskeletal Derangement. Biomedicines. 2022; 10(6):1329. https://doi.org/10.3390/biomedicines10061329
Chicago/Turabian StyleColasuonno, Fiorella, Chiara Marioli, Marco Tartaglia, Enrico Bertini, Claudia Compagnucci, and Sandra Moreno. 2022. "New Insights into the Neurodegeneration Mechanisms Underlying Riboflavin Transporter Deficiency (RTD): Involvement of Energy Dysmetabolism and Cytoskeletal Derangement" Biomedicines 10, no. 6: 1329. https://doi.org/10.3390/biomedicines10061329
APA StyleColasuonno, F., Marioli, C., Tartaglia, M., Bertini, E., Compagnucci, C., & Moreno, S. (2022). New Insights into the Neurodegeneration Mechanisms Underlying Riboflavin Transporter Deficiency (RTD): Involvement of Energy Dysmetabolism and Cytoskeletal Derangement. Biomedicines, 10(6), 1329. https://doi.org/10.3390/biomedicines10061329









