Angiogenic T Cells: Potential Biomarkers for the Early Diagnosis of Interstitial Lung Disease in Autoimmune Diseases?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Cell Quantification by Flow Cytometry
2.3. VEGF mRNA Expression
2.4. VEGF Serum Levels Determination
2.5. Statistical Analyses
3. Results
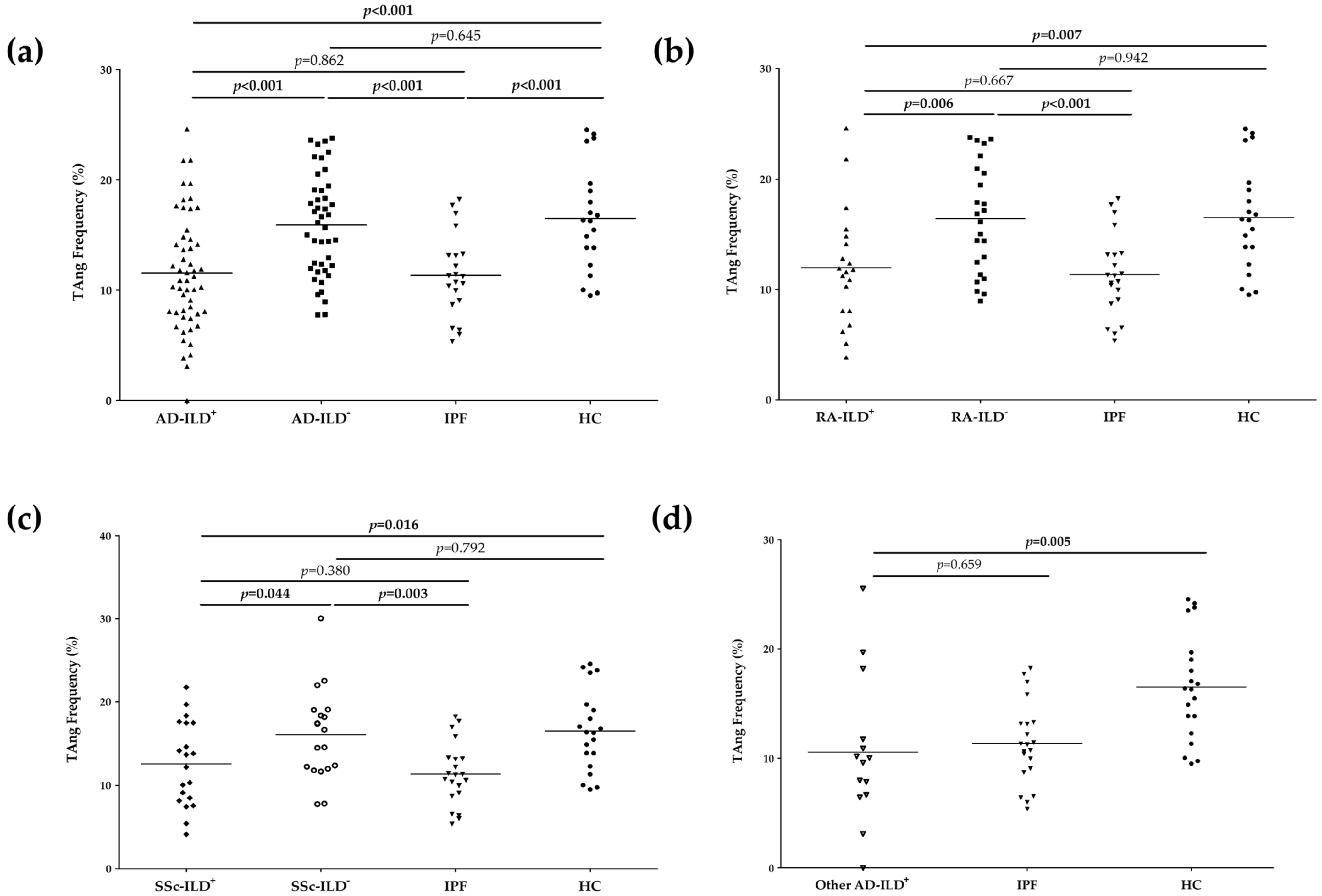
3.1. TAng Play a Role in the Pathogenesis of AD-ILD+
3.2. TAng Are Associated with Demographic and Clinical Features of RA-ILD+, SSc-ILD+ and Other AD-ILD+
3.3. No Relationship of TAng with Biomarkers of Endothelial Dysfunction in the Whole Cohort of AD-ILD+
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Atzeni, F.; Gerardi, M.C.; Barilaro, G.; Masala, I.F.; Benucci, M.; Sarzi-Puttini, P. Interstitial lung disease in systemic autoimmune rheumatic diseases: A comprehensive review. Expert. Rev. Clin. Immunol. 2018, 14, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, K.M.; Margaritopoulos, G.; Economidou, F.; Siafakas, N.M. Pivotal clinical dilemmas in collagen vascular diseases associated with interstitial lung involvement. Eur. Respir. J. 2009, 33, 882–896. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.; Du Bois, R. Interstitial lung disease in connective tissue disorders. Lancet 2012, 380, 689–698. [Google Scholar] [CrossRef]
- Mathai, S.C.; Danoff, S.K. Management of interstitial lung disease associated with connective tissue disease. BMJ 2016, 352, h6819. [Google Scholar] [CrossRef]
- Cottin, V.; Brown, K.K. Interstitial lung disease associated with systemic sclerosis (SSc-ILD). Respir. Res. 2019, 20, 13. [Google Scholar] [CrossRef]
- Orlandi, M.; Landini, N.; Sambataro, G.; Nardi, C.; Tofani, L.; Bruni, C.; Bellando-Randone, S.; Blagojevic, J.; Melchiorre, D.; Hughes, M.; et al. The role of chest ct in deciphering interstitial lung involvement: Systemic sclerosis versus COVID-19. Rheumatology 2021. Preprints. [Google Scholar]
- Ruaro, B.; Baratella, E.; Confalonieri, P.; Wade, B.; Marrocchio, C.; Geri, P.; Busca, A.; Pozzan, R.; Andrisano, A.G.; Cova, M.A.; et al. High-Resolution Computed Tomography: Lights and Shadows in Improving Care for SSc-ILD Patients. Diagnostics 2021, 11, 1960. [Google Scholar] [CrossRef]
- Cottin, V. Idiopathic interstitial pneumonias with connective tissue diseases features: A review. Respirology 2016, 21, 245–258. [Google Scholar] [CrossRef]
- Manetti, M.; Pratesi, S.; Romano, E.; Bellando-Randone, S.; Rosa, I.; Guiducci, S.; Fioretto, B.S.; Ibba-Manneschi, L.; Maggi, E.; Matucci-Cerinic, M. Angiogenic T cell expansion correlates with severity of peripheral vascular damage in systemic sclerosis. PLoS ONE 2017, 12, e0183102. [Google Scholar] [CrossRef]
- Murdaca, G.; Colombo, B.M.; Cagnati, P.; Gulli, R.; Spanò, F.; Puppo, F. Endothelial dysfunction in rheumatic autoimmune diseases. Atherosclerosis 2020, 224, 309–317. [Google Scholar] [CrossRef]
- Yang, X.; Chang, Y.; Wei, W. Endothelial Dysfunction and Inflammation: Immunity in Rheumatoid Arthritis. Mediat. Inflamm. 2016, 2016, 6813016. [Google Scholar] [CrossRef] [PubMed]
- Asano, Y.; Sato, S. Vasculopathy in scleroderma. Semin. Inmunopathol. 2015, 37, 489–500. [Google Scholar] [CrossRef] [PubMed]
- Arias-Nuñez, M.C.; Llorca, J.; Vazquez-Rodriguez, T.R.; Gomez-Acebo, I.; Miranda-Filloy, J.A.; Martin, J.; Gonzalez-Juanatey, C.; Gonzalez-Gay, M.A. Systemic sclerosis in northwestern Spain: A 19-year epidemiologic study. Medicine 2008, 87, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Pulito-Cueto, V.; Remuzgo-Martínez, S.; Genre, F.; Atienza-Mateo, B.; Mora-Cuesta, V.M.; Iturbe-Fernández, D.; Lera-Gómez, L.; Pérez-Fernández, R.; Prieto-Peña, D.; Portilla, V.; et al. Endothelial Progenitor Cells: Relevant Players in the Vasculopathy and Lung Fibrosis Associated with the Presence of Interstitial Lung Disease in Systemic Sclerosis Patients. Biomedicines 2021, 9, 847. [Google Scholar] [CrossRef]
- Pulito-Cueto, V.; Remuzgo-Martínez, S.; Genre, F.; Mora-Cuesta, V.M.; Iturbe-Fernández, D.; Fernández-Rozas, S.; Atienza-Mateo, B.; Lera-Gómez, L.; Alonso-Lecue, P.; Rodríguez-Carrio, J.; et al. Endothelial Progenitor Cells as a Potential Biomarker in Interstitial Lung Disease Associated with Rheumatoid Arthritis. J. Clin. Med. 2020, 9, 4098. [Google Scholar] [CrossRef]
- Patschan, S.; Tampe, D.; Müller, C.; Seitz, C.; Herink, C.; Müller, G.A.; Zeisberg, E.; Zeisberg, M.; Henze, E.; Patschan, D. Early Endothelial Progenitor Cells (eEPCs) in systemic sclerosis (SSc)—Dynamics of cellular regeneration and mesenchymal transdifferentiation. BMC Musculoskelet Disord. 2016, 17, 339. [Google Scholar] [CrossRef][Green Version]
- Trombetta, A.C.; Soldano, S.; Contini, P.; Tomatis, V.; Ruaro, B.; Paolino, S.; Brizzolara, R.; Montagna, P.; Sulli, A.; Pizzorni, C.; et al. A circulating cell population showing both M1 and M2 monocyte/macrophage surface markers characterizes systemic sclerosis patients with lung involvement. Respir. Res. 2018, 19, 186. [Google Scholar] [CrossRef]
- Hur, J.; Yang, H.M.; Yoon, C.H.; Lee, C.S.; Park, K.W.; Kim, J.H.; Kim, T.Y.; Kim, J.Y.; Kang, H.J.; Chae, I.H.; et al. Identification of a Novel Role of T Cells in Postnatal Vasculogenesis. Characterization of Endothelial Progenitor Cell Colonies. Circulation 2007, 116, 1671–1682. [Google Scholar] [CrossRef]
- Lv, T.; Yang, F.; Zhang, K.; Lv, M.; Zhang, Y.; Zhu, P. International Immunopharmacology The risk of circulating angiogenic T cells and subsets in patients with systemic sclerosis. Int. Immunopharmacol. 2020, 81, 106282. [Google Scholar] [CrossRef]
- Zhao, P.; Miao, J.; Zhang, K.; Yu, Z.; Lv, M.; Xu, Y.; Fu, X.; Han, Q.; Zhu, P. CD147 participates in the activation function of circulating angiogenic T cells in patients with rheumatoid arthritis. Clin. Rheumatol. 2019, 38, 2621–2628. [Google Scholar] [CrossRef]
- Kakizaki, M.; Nobori, K.; Watanabe, H.; Iino, K.; Ishida, M.; Ito, H. Increased circulating CD3+/CD31+ T cells in patients with acute coronary syndrome. Heart Vessels 2013, 28, 566–569. [Google Scholar] [CrossRef] [PubMed]
- Alunno, A.; Ibba-Manneschi, L.; Bistoni, O.; Cipriani, S.; Topini, F.; Gerli, R.; Manetti, M. Angiogenic T cells in primary Sjögren ’s syndrome: A double-edged sword? Clin. Exp. Rheumatol. 2019, 37, 36–41. [Google Scholar] [PubMed]
- López, P.; Rodriguez-Carrio, J.; Martínez-Zapico, A.; Caminal-Montero, L.; Suarez, A. Senescent profile of angiogenic T cells from systemic lupus erythematosus patients. J. Leukoc. Biol. 2016, 99, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Carrio, J.; Alperi-lópez, M.; López, P.; Alonso-Castro, S.; Ballina-García, F.J.; Suárez, A. Angiogenic T cells are decreased in rheumatoid arthritis patients. Ann. Rheum. Dis. 2015, 74, 921–927. [Google Scholar] [CrossRef]
- Bortoluzzi, A.; Chighizola, C.B.; Fredi, M.; Raschi, E.; Bodio, C.; Privitera, D.; Gonelli, A.; Silvagni, E.; Govoni, M.; Cavazzana, I.; et al. The IMMENSE Study: The Interplay Between iMMune and ENdothelial Cells in Mediating Cardiovascular Risk in Systemic Lupus Erythematosus. Front. Inmunol. 2020, 11, 572876. [Google Scholar] [CrossRef]
- Miao, J.; Qiu, F.; Li, T.; Zhao, P.; Zhang, K.; Lv, M.; Wan, J.; Qi, X.; Zhu, P. Circulating Angiogenic T Cells and Their Subpopulations in Patients with Systemic Lupus Erythematosus. Mediat. Inflamm. 2016, 2016, 2842143. [Google Scholar] [CrossRef]
- Zhao, P.; Miao, J.; Zhang, K.; Lv, M.; Han, Q.; Zhu, P. Circulating Angiogenic T Cells Are Increased in Lupus Nephritis Patients. Med. Sci. Monit. 2018, 24, 5384–5390. [Google Scholar] [CrossRef]
- Weil, B.R.; Kushner, E.J.; Diehl, K.J.; Greiner, J.J.; Stauffer, B.L.; Desouza, C.A. CD31+ T Cells, Endothelial Function and Cardiovascular Risk. Heart Lung Circ. 2011, 20, 659–662. [Google Scholar] [CrossRef]
- Bella, S.D.; Mavilio, D. Editorial: Senescent angiogenic T cells: The use of CD28 makes the difference in endothelial homeostasis. J. Leukoc. Biol. 2016, 99, 399–401. [Google Scholar] [CrossRef]
- Kushner, E.J.; MacEneaney, O.J.; Morgan, R.G.; Van Engelenburg, A.M.; Van Guilder, G.P.; Desouza, C.A. CD31+ T cells represent a functionally distinct vascular T cell phenotype. Blood Cells Mol. Dis. 2010, 44, 74–78. [Google Scholar] [CrossRef]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O., 3rd; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010, 62, 2569–2581. [Google Scholar] [CrossRef] [PubMed]
- Van Den Hoogen, F.; Khanna, D.; Fransen, J.; Johnson, S.R.; Baron, M.; Tyndall, A.; Matucci-Cerinic, M.; Naden, R.P.; Medsger, T.A., Jr.; Carreira, P.E.; et al. 2013 classification criteria for systemic sclerosis: An American college of rheumatology/European league against rheumatism collaborative initiative. Arthritis Rheum. 2013, 65, 2737–2747. [Google Scholar] [CrossRef] [PubMed]
- Travis, W.D.; Costabel, U.; Hansell, D.M.; King, T.E., Jr.; Lynch, D.A.; Nicholson, A.G.; Ryerson, C.J.; Ryu, J.H.; Selman, M.; Wells, A.U.; et al. An Official American Thoracic Society/European Respiratory Society Statement: Update of the International Multidisciplinary Classification of the Idiopathic Interstitial Pneumonias. Am. J. Respir. Crit. Care Med. 2013, 188, 733–748. [Google Scholar] [CrossRef] [PubMed]
- Lynch, D.A.; Sverzellati, N.; Travis, W.D.; Brown, K.K.; Colby, T.V.; Galvin, J.R.; Goldin, J.G.; Hansell, D.M.; Inoue, Y.; Johkoh, T.; et al. Diagnostic criteria for idiopathic pulmonary fibrosis: A Fleischner Society White Paper. Lancet Respir. Med. 2018, 6, 138–153. [Google Scholar] [CrossRef]
- Remuzgo-Martínez, S.; Genre, F.; Pulito-Cueto, V.; Atienza-Mateo, B.; Mora-Cuesta, V.M.; Iturbe-Fernández, D.; Fernández-Rozas, S.M.; Lera-Gómez, L.; Alonso-Lecue, P.; Piedad-Ussetti, M.; et al. Role of VEGF Polymorphisms in the Susceptibility and Severity of Interstitial Lung Disease. Biomedicines 2021, 9, 458. [Google Scholar] [CrossRef]
- Rouhl, R.P.W.; Mertens, A.E.C.S.; Van Oostenbrugge, R.J.; Damoiseaux, J.G.; Debrus-Palmans, L.L.; Henskens, L.H.; Kroon, A.A.; De Leeuw, P.W.; Lodder, J.; Tervaert, J.W. Angiogenic T-Cells and Putative Endothelial Progenitor Cells in Hypertension-Related Cerebral Small Vessel Disease. Stroke 2012, 43, 256–258. [Google Scholar] [CrossRef]
- De Boer, S.A.; Reijrink, M.; Abdulahad, W.H.; Hoekstra, E.S.; Slart, R.H.J.A.; Heerspink, H.J.L.; Westra, J.; Mulder, D.J. Angiogenic T cells are decreased in people with type 2 diabetes mellitus and recruited by the dipeptidyl peptidase-4 inhibitor Linagliptin: A subanalysis from a randomized, placebo-controlled trial (RELEASE study). Diabetes Obes. Metab. 2020, 22, 1220–1225. [Google Scholar] [CrossRef]
- Atienza-Mateo, B.; Remuzgo-Martínez, S.; Mora-Cuesta, V.M.; Iturbe-Fernández, D.; Fernández-Rozas, S.; Prieto-Peña, D.; Calderón-Goercke, M.; Corrales, A.; Blanco-Rodriguez, G.; Gómez-Román, J.J.; et al. The Spectrum of Interstitial Lung Disease Associated with Autoimmune Diseases: Data of a 3.6-Year Prospective Study from a Referral Center of Interstitial Lung Disease and Lung Transplantation. J. Clin. Med. 2020, 9, 1606. [Google Scholar] [CrossRef]
| Study Objective Groups | Comparative Groups | |||||
|---|---|---|---|---|---|---|
| RA-ILD+ n = 21 | SSc-ILD+ n = 21 | Other AD-ILD+ n = 15 | RA-ILD− n = 25 | SSc-ILD− n = 20 | IPF n = 21 | |
| Sex (women), n (%) | 9 (45.9) | 13 (61.9) | 5 (33.3) | 15 (60.0) | 18 (90.0) | 7 (33.3) |
| Age at study, mean ± SD, years | 66.5 ± 10.1 | 60.3 ± 7.0 | 62.0 ± 10.1 | 60.1 ± 11.8 | 56.6 ± 15.4 | 69.2 ± 10.0 |
| Smoking ever, n (%) | 13 (65.0) | 11 (52.4) | 11 (73.3) | 13 (52.0) | 11 (55.0) | 16 (76.2) |
| Pulmonary function tests | ||||||
| FVC (% predicted), mean ± SD | 95.2 ± 24.1 | 88.4 ± 27.1 | 88.3 ± 28.8 | 99.2 ± 16.0 | 106.6 ± 15.9 | 84.9 ± 14.7 |
| FEV1 (% predicted), mean ± SD | 92.2 ± 21.0 | 87.3 ± 25.6 | 88.7 ± 27.6 | 94.9 ± 22.0 | 101.9 ± 17.8 | 87.3 ± 19.6 |
| FEV1/FVC (% predicted), mean ± SD | 77.8 ± 9.1 | 79.7 ± 5.5 | 79.7 ± 4.6 | 93.6 ± 12.3 | 79.2 ± 9.9 | 79.7 ± 7.8 |
| DLCO (% predicted), mean ± SD | 43.3 ± 15.9 | 47.5 ± 19.5 | 44.6 ± 14.6 | 79.9 ± 20.0 | 71.5 ± 15.3 | 43.6 ± 18.4 |
| HRCT | ||||||
| Pulmonary involvement on HRCT | 21 (100.0) | 21 (100.0) | 15 (100.0) | 0 (0.0) | 0 (0.0) | 21 (100.0) |
| UIP pattern, n (%) | 11 (52.4) | 3 (14.3) | 4 (26.7) | - | - | 21 (100.0) |
| Probable UIP pattern, n (%) | 2 (9.5) | 3 (14.3) | 5 (33.3) | - | - | 0 (0.0) |
| NSIP pattern, n (%) | 7 (33.3) | 14 (66.7) | 6 (40.0) | - | - | 0 (0.0) |
| Non-NSIP pattern, n (%) | 1 (4.8) | 1 (4.7) | 0 (0.0) | - | - | 0 (0.0) |
| Received therapies | ||||||
| csDMARDs n (%) | 17 (81.0) | 16 (76.2) | 2 (13.3) | 13 (52) | 12 (60.0) | 0 (0.0) |
| bDMARDs, n (%) | 15 (71.4) | 7 (33.3) | 3 (20.0) | 2 (8) | 2 (10.0) | 0 (0.0) |
| Antifibrotic drugs, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 9 (42.9) |
| Variable | r | p |
|---|---|---|
| Duration of RA (years) | −0.16 | 0.50 |
| CRP (mg/dL) | 0.02 | 0.94 |
| ESR (mm/1st hour) | −0.18 | 0.44 |
| FVC (% predicted) | 0.13 | 0.58 |
| FEV1 (% predicted) | 0.18 | 0.43 |
| FEV1/FVC (% predicted) | 0.18 | 0.44 |
| DLCO (% predicted) | 0.15 | 0.62 |
| Category | Mean ± SD | p |
| Men | 9.75 ± 4.12 | <0.01 |
| Women | 16.44 ± 5.97 | |
| Non-Smoker | 15.50 ± 5.63 | 0.24 |
| Smoker | 12.02 ± 5.86 | |
| RF− | 13.59 ± 3.29 | 0.79 |
| RF+ | 12.52 ± 6.50 | |
| UIP HRCT Pattern | 12.40 ± 6.34 | 0.76 |
| NSIP HRCT Pattern | 13.36 ± 6.55 |
| Variable | r | p |
|---|---|---|
| Duration of SSc disease (years) | 0.04 | 0.86 |
| CRP (mg/dL) | 0.31 | 0.22 |
| ESR (mm/1st hour) | −0.17 | 0.51 |
| FVC (% predicted) | −0.06 | 0.79 |
| FEV1 (% predicted) | −0.02 | 0.94 |
| FEV1/FVC (% predicted) | 0.48 | 0.03 |
| DLCO (% predicted) | −0.06 | 0.77 |
| Category | Mean ± SD | p |
| Men | 10.30 ± 5.67 | 0.07 |
| Women | 15.02 ± 5.25 | |
| Non-Smoker | 14.97 ± 5.20 | 0.19 |
| Smoker | 11.64 ± 6.04 | |
| ATA (Scl70)− | 10.30 ± 5.09 | 0.03 |
| ATA (Scl70)+ | 15.73 ± 5.44 | |
| Non-Pulmonary hypertension | 12.38 ± 6.08 | 0.37 |
| Pulmonary hypertension | 15.86 ± 5.15 | |
| NSIP HRCT Pattern | 13.52 ± 6.61 | 0.70 |
| UIP HRCT Pattern | 12.38 ± 4.28 |
| Variable | r | p |
|---|---|---|
| FVC (% predicted) | −0.27 | 0.32 |
| FEV1 (% predicted) | −0.27 | 0.32 |
| FEV1/FVC (% predicted) | 0.15 | 0.59 |
| DLCO (% predicted) | −0.36 | 0.27 |
| Category | Mean ± SD | p |
| Men | 11.92 ± 8.97 | 0.84 |
| Women | 11.05 ± 4.92 | |
| Non-Smoker | 17.83 ± 7.30 | 0.06 |
| Smoker | 9.38 ± 6.74 | |
| NSIP HRCT Pattern | 6.43 ± 3.99 | 0.03 |
| UIP HRCT Pattern | 15.11 ± 7.69 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pulito-Cueto, V.; Remuzgo-Martínez, S.; Genre, F.; Atienza-Mateo, B.; Mora-Cuesta, V.M.; Iturbe-Fernández, D.; Lera-Gómez, L.; Rodriguez-Carrio, J.; Prieto-Peña, D.; Portilla, V.; et al. Angiogenic T Cells: Potential Biomarkers for the Early Diagnosis of Interstitial Lung Disease in Autoimmune Diseases? Biomedicines 2022, 10, 851. https://doi.org/10.3390/biomedicines10040851
Pulito-Cueto V, Remuzgo-Martínez S, Genre F, Atienza-Mateo B, Mora-Cuesta VM, Iturbe-Fernández D, Lera-Gómez L, Rodriguez-Carrio J, Prieto-Peña D, Portilla V, et al. Angiogenic T Cells: Potential Biomarkers for the Early Diagnosis of Interstitial Lung Disease in Autoimmune Diseases? Biomedicines. 2022; 10(4):851. https://doi.org/10.3390/biomedicines10040851
Chicago/Turabian StylePulito-Cueto, Verónica, Sara Remuzgo-Martínez, Fernanda Genre, Belén Atienza-Mateo, Víctor M. Mora-Cuesta, David Iturbe-Fernández, Leticia Lera-Gómez, Javier Rodriguez-Carrio, Diana Prieto-Peña, Virginia Portilla, and et al. 2022. "Angiogenic T Cells: Potential Biomarkers for the Early Diagnosis of Interstitial Lung Disease in Autoimmune Diseases?" Biomedicines 10, no. 4: 851. https://doi.org/10.3390/biomedicines10040851
APA StylePulito-Cueto, V., Remuzgo-Martínez, S., Genre, F., Atienza-Mateo, B., Mora-Cuesta, V. M., Iturbe-Fernández, D., Lera-Gómez, L., Rodriguez-Carrio, J., Prieto-Peña, D., Portilla, V., Blanco, R., Corrales, A., Gualillo, O., Cifrián, J. M., López-Mejías, R., & González-Gay, M. A. (2022). Angiogenic T Cells: Potential Biomarkers for the Early Diagnosis of Interstitial Lung Disease in Autoimmune Diseases? Biomedicines, 10(4), 851. https://doi.org/10.3390/biomedicines10040851








