Translational Approach to the Protective Effect of Bilirubin in Diabetic Kidney Disease
Abstract
1. Introduction
2. Bilirubin
2.1. Bilirubin Metabolism
2.2. Bilirubin as Janus Bifrons
2.3. Bilirubin Protective Effects
3. Diabetic Kidney Disease
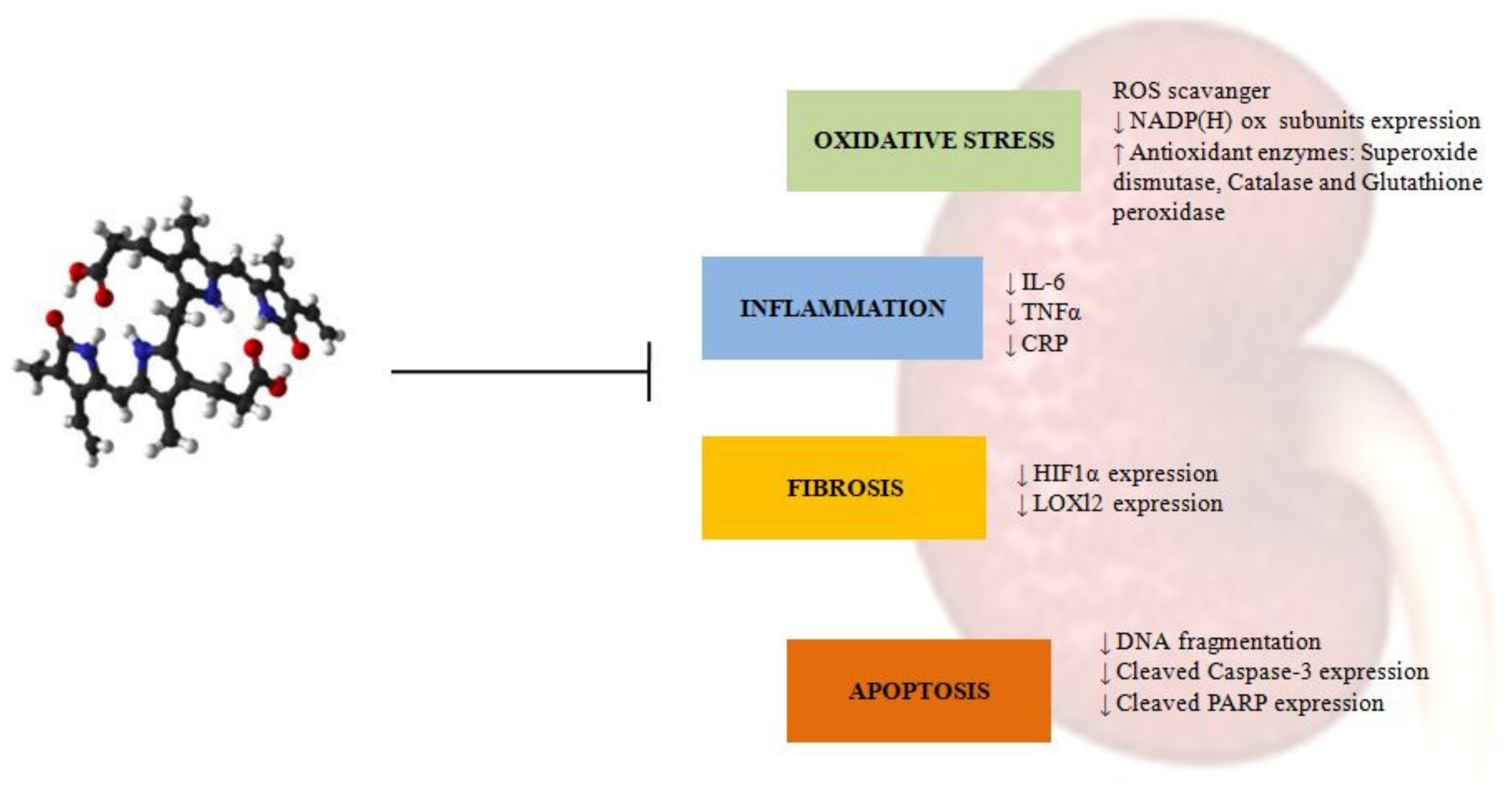
4. Bilirubin Protection against Diabetic Kidney Disease
4.1. Oxidative Stress
4.2. Inflammation
4.3. Fibrosis
4.4. Apoptosis
5. Conclusions and Future Prospective
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ABCC2 | ATP-binding cassette transporters subfamily C2 |
| AGEs | Advanced glycation end products |
| AhR | Aryl-hydrocarbon receptor |
| AMPK | Serine/threonine kinase AMP-activated protein kinase |
| AngII | Angiotensin II |
| ApoA1 | Apolipoprotein A1 |
| ApoB | Apolipoprotein B |
| ApoD | Apolipoprotein D |
| Bax | Bcl-2 Associated X-protein |
| Bcl2 | B-cell lymphoma 2 |
| Bcl-XlB | cell lymphoma-extra large |
| Bf | Free bilirubin |
| BLVRA | Biliverdin reductase A enzyme |
| BRNPs | Bilirubin nanoparticles |
| CAR | Constitutive androstane receptor |
| CB | Conjugated bilirubin |
| CDV | Cardiovascular disease |
| CKD | Chronic kidney diseases |
| CNS | Crigler-Najjar syndromes |
| CO | Carbon monoxide |
| CRP | C-reactive protein |
| CsA | Cyclosporine |
| CXCLs | Soluble C-X-C chemokine ligand |
| CYP-450 | Cytochrome 450 |
| DAG | Diacylglycerol |
| DKD | Diabetic kidney disease |
| DNA | Deoxyribonucleic acid |
| DN | Diabetic nephropathy |
| EMT | Epithelial to mesenchymal transition |
| EPO | Erythropoietin |
| ERK | Extracellular signal-regulated kinase |
| FABP 1 | Fatty acid-binding protein |
| Fe2+ | Ferrous ions |
| GAPDH | Glyceraldehyde-3-phosphate dehydrogenase |
| GLUT1 | Glucose transporter-1 |
| GS | Gilbert syndrome |
| HDL | High-density lipoprotein |
| HIF-1α | Hypoxia-inducible factor 1, alpha subunit |
| HMOX | Hemeoxygenase enzyme |
| IL-10 | Interleukin-10 |
| IL-2 | Interleukin-2 |
| IL-6 | Interleukin-6 |
| iNOS | Inducible nitric oxide synthase |
| LDL | Low density lipoproteins |
| LOXl2 | Lysyl Oxidase Like 2 |
| LPS | Lipopolysaccharid |
| MAPK | Mitogen-activated protein kinase |
| MDA | Malondialdehyde |
| MRGPRX4 | Mas-related G protein-coupled receptor X4 |
| MRP2 | Multidrug resistance-associated protein 2 |
| NADP | Nicotinamide adenine dinucleotide phosphate |
| NADP+ | Nicotinamide adenine dinucleotide phosphate oxidized form |
| NADPH | Nicotinamide adenine dinucleotide phosphate reduced form |
| NADPH oxidase | Nicotinamide adenine dinucleotide phosphate oxidase |
| NF-kβ | Nuclear factor kappa-light-chain-enhancer of activated B cells |
| NO | Nitric oxide |
| NOS | Nitric oxide synthase |
| O2 | Oxygen |
| OATP1B1 | Organic anion transporting polypeptide 1B1 |
| OMIM | Online Mendelian Inheritance in Man |
| P70S6K | p70S6 kinase |
| PARP | Nuclear poly ADP ribose polymerase |
| PGK | Phosphoglycerate kinase-1 |
| PKC | Protein kinase C |
| PPARs | Peroxisome proliferator-activated receptors |
| PXR | Pregnane X receptor |
| RAAS | Renin–angiotensin–aldosterone system |
| Raf | Rapidly accelerated fibrosarcoma |
| ROS | Reactive oxygen species |
| TGF-β | Transforming growth factor-β |
| TIF | Tubulointerstitial fibrosis |
| TIMP-1 | Tissue inhibitor of metalloproteinase-1 |
| TNF-α | Tumor necrosis factor alpha |
| UCB | Unconjugated bilirubin |
| UDP | Uridine diphosphate; |
| UDPGA | uridine 5′-diphosphoglucuronic acid |
| UGT1A1 | uridine diphosphate-glucuronosyl transferase 1A1 |
| VEGF | Vascular endothelial growth factor |
| VLDL | Very low-density lipoprotein |
| α-SMA | α-smooth muscle actin |
References
- Hinds, T.D.; Stec, D.E. Bilirubin Safeguards Cardiorenal and Metabolic Diseases: A Protective Role in Health. Curr. Hypertens. Rep. 2019, 21, 87. [Google Scholar] [CrossRef] [PubMed]
- Vitek, L.; Hubacek, J.A.; Pajak, A.; Doryńska, A.; Kozela, M.; Eremiasova, L.; Danzig, V.; Stefler, D.; Bobak, M. Association between Plasma Bilirubin and Mortality. Ann. Hepatol. 2019, 18, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Alicic, R.Z.; Rooney, M.T.; Tuttle, K.R. Diabetic Kidney Disease. Clin. J. Am. Soc. Nephrol. CJASN 2017, 12, 2032–2045. [Google Scholar] [CrossRef] [PubMed]
- Keum, H.; Kim, D.; Kim, J.; Kim, T.W.; Whang, C.-H.; Jung, W.; Jon, S. A Bilirubin-Derived Nanomedicine Attenuates the Pathological Cascade of Pulmonary Fibrosis. Biomaterials 2021, 275, 120986. [Google Scholar] [CrossRef] [PubMed]
- Vítek, L. The Role of Bilirubin in Diabetes, Metabolic Syndrome, and Cardiovascular Diseases. Front. Pharmacol. 2012, 3, 55. [Google Scholar] [CrossRef]
- Vítek, L. Bilirubin as a Signaling Molecule. Med. Res. Rev. 2020, 40, 1335–1351. [Google Scholar] [CrossRef]
- Fevery, J. Bilirubin in Clinical Practice: A Review. Liver Int. Off. J. Int. Assoc. Study Liver 2008, 28, 592–605. [Google Scholar] [CrossRef]
- Vitek, L.; Bellarosa, C.; Tiribelli, C. Induction of Mild Hyperbilirubinemia: Hype or Real Therapeutic Opportunity? Clin. Pharmacol. Ther. 2019, 106, 568–575. [Google Scholar] [CrossRef]
- Hahm, J.S.; Ostrow, J.D.; Mukerjee, P.; Celic, L. Ionization and Self-Association of Unconjugated Bilirubin, Determined by Rapid Solvent Partition from Chloroform, with Further Studies of Bilirubin Solubility. J. Lipid Res. 1992, 33, 1123–1137. [Google Scholar] [CrossRef]
- Ahlfors, C.E.; Wennberg, R.P.; Ostrow, J.D.; Tiribelli, C. Unbound (Free) Bilirubin: Improving the Paradigm for Evaluating Neonatal Jaundice. Clin. Chem. 2009, 55, 1288–1299. [Google Scholar] [CrossRef]
- Zelenka, J.; Dvořák, A.; Alán, L.; Zadinová, M.; Haluzík, M.; Vítek, L. Hyperbilirubinemia Protects against Aging-Associated Inflammation and Metabolic Deterioration. Oxid. Med. Cell. Longev. 2016, 2016, 6190609. [Google Scholar] [CrossRef] [PubMed]
- Sundararaghavan, V.L.; Sindhwani, P.; Hinds, T.D. Glucuronidation and UGT Isozymes in Bladder: New Targets for the Treatment of Uroepithelial Carcinomas? Oncotarget 2016, 8, 3640–3648. [Google Scholar] [CrossRef] [PubMed]
- Méndez-Sánchez, N.; Qi, X.; Vitek, L.; Arrese, M. Evaluating an Outpatient with an Elevated Bilirubin. Am. J. Gastroenterol. 2019, 114, 1185–1188. [Google Scholar] [CrossRef]
- Tiribelli, C.; Ostrow, J.D. Intestinal Flora and Bilirubin. J. Hepatol. 2005, 42, 170–172. [Google Scholar] [CrossRef]
- Sticova, E.; Jirsa, M. New Insights in Bilirubin Metabolism and Their Clinical Implications. World J. Gastroenterol. 2013, 19, 6398–6407. [Google Scholar] [CrossRef] [PubMed]
- Vítek, L.; Ostrow, J.D. Bilirubin Chemistry and Metabolism; Harmful and Protective Aspects. Curr. Pharm. Des. 2009, 15, 2869–2883. [Google Scholar] [CrossRef]
- Reddy, D.K.; Pandey, S. Kernicterus. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Watchko, J.F. Kernicterus and the Molecular Mechanisms of Bilirubin-Induced CNS Injury in Newborns. Neuromolecular Med. 2006, 8, 513–529. [Google Scholar] [CrossRef]
- Boon, A.-C.; Bulmer, A.C.; Coombes, J.S.; Fassett, R.G. Circulating Bilirubin and Defense against Kidney Disease and Cardiovascular Mortality: Mechanisms Contributing to Protection in Clinical Investigations. Am. J. Physiol. Renal Physiol. 2014, 307, F123–F136. [Google Scholar] [CrossRef] [PubMed]
- Gunn, C.K. Hereditary Acholuric Jaundice in the Rat. Can. Med. Assoc. J. 1944, 50, 230–237. [Google Scholar]
- Schutta, H.S.; Johnson, L. Bilirubin Encephalopathy in the Gunn Rat: A Fine Structure Study of the Cerebellar Cortex. J. Neuropathol. Exp. Neurol. 1967, 26, 377–396. [Google Scholar] [CrossRef]
- Gazzin, S.; Zelenka, J.; Zdrahalova, L.; Konickova, R.; Zabetta, C.C.; Giraudi, P.J.; Berengeno, A.L.; Raseni, A.; Robert, M.C.; Vitek, L.; et al. Bilirubin Accumulation and Cyp MRNA Expression in Selected Brain Regions of Jaundiced Gunn Rat Pups. Pediatr. Res. 2012, 71, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Lanone, S.; Bloc, S.; Foresti, R.; Almolki, A.; Taillé, C.; Callebert, J.; Conti, M.; Goven, D.; Aubier, M.; Dureuil, B.; et al. Bilirubin Decreases Nos2 Expression via Inhibition of NAD(P)H Oxidase: Implications for Protection against Endotoxic Shock in Rats. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2005, 19, 1890–1892. [Google Scholar] [CrossRef] [PubMed]
- Ollinger, R.; Bilban, M.; Erat, A.; Froio, A.; McDaid, J.; Tyagi, S.; Csizmadia, E.; Graça-Souza, A.V.; Liloia, A.; Soares, M.P.; et al. Bilirubin: A Natural Inhibitor of Vascular Smooth Muscle Cell Proliferation. Circulation 2005, 112, 1030–1039. [Google Scholar] [CrossRef] [PubMed]
- Pflueger, A.; Croatt, A.J.; Peterson, T.E.; Smith, L.A.; d’Uscio, L.V.; Katusic, Z.S.; Nath, K.A. The Hyperbilirubinemic Gunn Rat Is Resistant to the Pressor Effects of Angiotensin II. Am. J. Physiol. Renal Physiol. 2005, 288, F552–F558. [Google Scholar] [CrossRef] [PubMed]
- Zelenka, J.; Muchova, L.; Zelenkova, M.; Vanova, K.; Vreman, H.J.; Wong, R.J.; Vitek, L. Intracellular Accumulation of Bilirubin as a Defense Mechanism against Increased Oxidative Stress. Biochimie 2012, 94, 1821–1827. [Google Scholar] [CrossRef]
- Kang, S.J.; Lee, C.; Kruzliak, P. Effects of Serum Bilirubin on Atherosclerotic Processes. Ann. Med. 2014, 46, 138–147. [Google Scholar] [CrossRef]
- Wagner, K.-H.; Wallner, M.; Mölzer, C.; Gazzin, S.; Bulmer, A.C.; Tiribelli, C.; Vitek, L. Looking to the Horizon: The Role of Bilirubin in the Development and Prevention of Age-Related Chronic Diseases. Clin. Sci. Lond. Engl. 1979 2015, 129, 1–25. [Google Scholar] [CrossRef]
- Wagner, K.-H.; Shiels, R.G.; Lang, C.A.; Seyed Khoei, N.; Bulmer, A.C. Diagnostic Criteria and Contributors to Gilbert’s Syndrome. Crit. Rev. Clin. Lab. Sci. 2018, 55, 129–139. [Google Scholar] [CrossRef]
- Erlinger, S.; Arias, I.M.; Dhumeaux, D. Inherited Disorders of Bilirubin Transport and Conjugation: New Insights into Molecular Mechanisms and Consequences. Gastroenterology 2014, 146, 1625–1638. [Google Scholar] [CrossRef]
- Boon, A.-C.; Hawkins, C.L.; Bisht, K.; Coombes, J.S.; Bakrania, B.; Wagner, K.-H.; Bulmer, A.C. Reduced Circulating Oxidized LDL Is Associated with Hypocholesterolemia and Enhanced Thiol Status in Gilbert Syndrome. Free Radic. Biol. Med. 2012, 52, 2120–2127. [Google Scholar] [CrossRef]
- Vianello, E.; Zampieri, S.; Marcuzzo, T.; Tordini, F.; Bottin, C.; Dardis, A.; Zanconati, F.; Tiribelli, C.; Gazzin, S. Histone Acetylation as a New Mechanism for Bilirubin-Induced Encephalopathy in the Gunn Rat. Sci. Rep. 2018, 8, 13690. [Google Scholar] [CrossRef] [PubMed]
- Vítek, L.; Jirsa, M.; Brodanová, M.; Kalab, M.; Marecek, Z.; Danzig, V.; Novotný, L.; Kotal, P. Gilbert Syndrome and Ischemic Heart Disease: A Protective Effect of Elevated Bilirubin Levels. Atherosclerosis 2002, 160, 449–456. [Google Scholar] [CrossRef]
- Bulmer, A.C.; Blanchfield, J.T.; Toth, I.; Fassett, R.G.; Coombes, J.S. Improved Resistance to Serum Oxidation in Gilbert’s Syndrome: A Mechanism for Cardiovascular Protection. Atherosclerosis 2008, 199, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Creeden, J.F.; Gordon, D.M.; Stec, D.E.; Hinds, T.D. Bilirubin as a Metabolic Hormone: The Physiological Relevance of Low Levels. Am. J. Physiol. Endocrinol. Metab. 2021, 320, E191–E207. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Jee, Y.H.; Jung, K.J.; Hong, S.; Shin, E.S.; Jee, S.H. Bilirubin and Stroke Risk Using a Mendelian Randomization Design. Stroke 2017, 48, 1154–1160. [Google Scholar] [CrossRef]
- Stender, S.; Frikke-Schmidt, R.; Nordestgaard, B.G.; Grande, P.; Tybjaerg-Hansen, A. Genetically Elevated Bilirubin and Risk of Ischaemic Heart Disease: Three Mendelian Randomization Studies and a Meta-Analysis. J. Intern. Med. 2013, 273, 59–68. [Google Scholar] [CrossRef]
- Hinds, T.D.; Stec, D.E. Bilirubin, a Cardiometabolic Signaling Molecule. Hypertens. Dallas Tex 1979 2018, 72, 788–795. [Google Scholar] [CrossRef]
- Stec, D.E.; John, K.; Trabbic, C.J.; Luniwal, A.; Hankins, M.W.; Baum, J.; Hinds, T.D. Bilirubin Binding to PPARα Inhibits Lipid Accumulation. PLoS ONE 2016, 11, e0153427. [Google Scholar] [CrossRef]
- Chan, W.K.; Tsai, S.-S.; Li, Y.-R.; Chou, W.-Y.; Chen, H.-L.; Chen, S.-T. Association between Serum Bilirubin Levels and Progression of Albuminuria in Taiwanese with Type 2 Diabetes Mellitus. Biomed. J. 2021, 44, 201–208. [Google Scholar] [CrossRef]
- Liu, M.; Li, J.; Lv, X.; He, Y. Bilirubin and Its Changes Were Negatively Associated with Diabetic Kidney Disease Incidence and Progression: A Five-Year’s Cohort Study Based on 5323 Chinese Male Diabetic Patients. J. Diabetes Complicat. 2018, 32, 1012–1017. [Google Scholar] [CrossRef]
- Ahn, K.H.; Kim, S.S.; Kim, W.J.; Kim, J.H.; Nam, Y.J.; Park, S.B.; Jeon, Y.K.; Kim, B.H.; Kim, I.J.; Kim, Y.K. Low Serum Bilirubin Level Predicts the Development of Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus. Korean J. Intern. Med. 2017, 32, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Uludag, K.; Oguzhan, N.; Arıkan, T.; Boz, G. Serum Bilirubin Level and Its Impact on the Progression of Chronic Kidney Disease. Int. Urol. Nephrol. 2018, 50, 1695–1701. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhang, L.; Chen, H.; Guo, K.; Yu, H.; Zhou, J.; Li, M.; Li, Q.; Li, L.; Yin, J.; et al. Relationship between Serum Bilirubin Concentrations and Diabetic Nephropathy in Shanghai Han’s Patients with Type 1 Diabetes Mellitus. BMC Nephrol. 2017, 18, 114. [Google Scholar] [CrossRef][Green Version]
- Rigato, I.; Ostrow, J.D.; Tiribelli, C. Bilirubin and the Risk of Common Non-Hepatic Diseases. Trends Mol. Med. 2005, 11, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Bianco, A.; Pinci, S.; Tiribelli, C.; Bellarosa, C. Life-Long Hyperbilirubinemia Exposure and Bilirubin Priming Prevent In Vitro Metabolic Damage. Front. Pharmacol. 2021, 12, 411. [Google Scholar] [CrossRef]
- Brito, M.A.; Lima, S.; Fernandes, A.; Falcão, A.S.; Silva, R.F.M.; Butterfield, D.A.; Brites, D. Bilirubin Injury to Neurons: Contribution of Oxidative Stress and Rescue by Glycoursodeoxycholic Acid. Neurotoxicology 2008, 29, 259–269. [Google Scholar] [CrossRef]
- Kumar, S.; Guha, M.; Choubey, V.; Maity, P.; Srivastava, K.; Puri, S.K.; Bandyopadhyay, U. Bilirubin Inhibits Plasmodium Falciparum Growth through the Generation of Reactive Oxygen Species. Free Radic. Biol. Med. 2008, 44, 602–613. [Google Scholar] [CrossRef]
- Oakes, G.H.; Bend, J.R. Early Steps in Bilirubin-Mediated Apoptosis in Murine Hepatoma (Hepa 1c1c7) Cells Are Characterized by Aryl Hydrocarbon Receptor-Independent Oxidative Stress and Activation of the Mitochondrial Pathway. J. Biochem. Mol. Toxicol. 2005, 19, 244–255. [Google Scholar] [CrossRef]
- Bianco, A.; Dvořák, A.; Capková, N.; Gironde, C.; Tiribelli, C.; Furger, C.; Vitek, L.; Bellarosa, C. The Extent of Intracellular Accumulation of Bilirubin Determines Its Anti- or Pro-Oxidant Effect. Int. J. Mol. Sci. 2020, 21, 8101. [Google Scholar] [CrossRef]
- Jangi, S.; Otterbein, L.; Robson, S. The Molecular Basis for the Immunomodulatory Activities of Unconjugated Bilirubin. Int. J. Biochem. Cell Biol. 2013, 45, 2843–2851. [Google Scholar] [CrossRef]
- Barateiro, A.; Vaz, A.R.; Silva, S.L.; Fernandes, A.; Brites, D. ER Stress, Mitochondrial Dysfunction and Calpain/JNK Activation Are Involved in Oligodendrocyte Precursor Cell Death by Unconjugated Bilirubin. Neuromolecular Med. 2012, 14, 285–302. [Google Scholar] [CrossRef]
- Zhu, H.; Wang, J.; Jiang, H.; Ma, Y.; Pan, S.; Reddy, S.; Sun, X. Bilirubin Protects Grafts against Nonspecific Inflammation-Induced Injury in Syngeneic Intraportal Islet Transplantation. Exp. Mol. Med. 2010, 42, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Tran, D.T.; Jeong, Y.Y.; Kim, J.M.; Bae, H.B.; Son, S.K.; Kwak, S.H. The Anti-Inflammatory Role of Bilirubin on “Two-Hit” Sepsis Animal Model. Int. J. Mol. Sci. 2020, 21, 8650. [Google Scholar] [CrossRef]
- Li, Y.; Huang, B.; Ye, T.; Wang, Y.; Xia, D.; Qian, J. Physiological Concentrations of Bilirubin Control Inflammatory Response by Inhibiting NF-ΚB and Inflammasome Activation. Int. Immunopharmacol. 2020, 84, 106520. [Google Scholar] [CrossRef] [PubMed]
- Mazzone, G.L.; Rigato, I.; Ostrow, J.D.; Tiribelli, C. Bilirubin Effect on Endothelial Adhesion Molecules Expression Is Mediated by the NF-KappaB Signaling Pathway. Biosci. Trends 2009, 3, 151–157. [Google Scholar] [PubMed]
- Gundamaraju, R.; Vemuri, R.; Chong, W.C.; Bulmer, A.C.; Eri, R. Bilirubin Attenuates ER Stress-Mediated Inflammation, Escalates Apoptosis and Reduces Proliferation in the LS174T Colonic Epithelial Cell Line. Int. J. Med. Sci. 2019, 16, 135–144. [Google Scholar] [CrossRef]
- Hinds, T.D.; Gordon, D.M.; Combs, S.D.; Stec, D.E. Bilirubin, a Novel Endocrine Hormone with Fat Burning Properties. FASEB J. 2018, 32, 605.6. [Google Scholar] [CrossRef]
- Vítek, L.; Tiribelli, C. Bilirubin: The Yellow Hormone? J. Hepatol. 2021. [Google Scholar] [CrossRef]
- Žiberna, L.; Jenko-Pražnikar, Z.; Petelin, A. Serum Bilirubin Levels in Overweight and Obese Individuals: The Importance of Anti-Inflammatory and Antioxidant Responses. Antioxid. Basel Switz. 2021, 10, 1352. [Google Scholar] [CrossRef]
- Persson, F.; Rossing, P. Diagnosis of Diabetic Kidney Disease: State of the Art and Future Perspective. Kidney Int. Suppl. 2018, 8, 2–7. [Google Scholar] [CrossRef]
- Slyne, J.; Slattery, C.; McMorrow, T.; Ryan, M.P. New Developments Concerning the Proximal Tubule in Diabetic Nephropathy: In Vitro Models and Mechanisms. Nephrol. Dial. Transplant. 2015, 30, iv60–iv67. [Google Scholar] [CrossRef] [PubMed]
- Amatruda, M.; Gembillo, G.; Giuffrida, A.E.; Santoro, D.; Conti, G. The Aggressive Diabetic Kidney Disease in Youth-Onset Type 2 Diabetes: Pathogenetic Mechanisms and Potential Therapies. Medicina 2021, 57, 868. [Google Scholar] [CrossRef] [PubMed]
- Giandalia, A.; Giuffrida, A.E.; Gembillo, G.; Cucinotta, D.; Squadrito, G.; Santoro, D.; Russo, G.T. Gender Differences in Diabetic Kidney Disease: Focus on Hormonal, Genetic and Clinical Factors. Int. J. Mol. Sci. 2021, 22, 5808. [Google Scholar] [CrossRef] [PubMed]
- Santoro, D.; Torreggiani, M.; Pellicanò, V.; Cernaro, V.; Messina, R.M.; Longhitano, E.; Siligato, R.; Gembillo, G.; Esposito, C.; Piccoli, G.B. Kidney Biopsy in Type 2 Diabetic Patients: Critical Reflections on Present Indications and Diagnostic Alternatives. Int. J. Mol. Sci. 2021, 22, 5425. [Google Scholar] [CrossRef]
- Bose, M.; Almas, S.; Prabhakar, S. Wnt Signaling and Podocyte Dysfunction in Diabetic Nephropathy. J. Investig. Med. Off. Publ. Am. Fed. Clin. Res. 2017, 65, 1093–1101. [Google Scholar] [CrossRef]
- Maezawa, Y.; Takemoto, M.; Yokote, K. Cell Biology of Diabetic Nephropathy: Roles of Endothelial Cells, Tubulointerstitial Cells and Podocytes. J. Diabetes Investig. 2015, 6, 3–15. [Google Scholar] [CrossRef]
- Xiong, Y.; Zhou, L. The Signaling of Cellular Senescence in Diabetic Nephropathy. Oxid. Med. Cell. Longev. 2019, 2019, 7495629. [Google Scholar] [CrossRef]
- Duran-Salgado, M.B.; Rubio-Guerra, A.F. Diabetic Nephropathy and Inflammation. World J. Diabetes 2014, 5, 393–398. [Google Scholar] [CrossRef]
- Talsma, D.T.; Katta, K.; Ettema, M.A.B.; Kel, B.; Kusche-Gullberg, M.; Daha, M.R.; Stegeman, C.A.; van den Born, J.; Wang, L. Endothelial Heparan Sulfate Deficiency Reduces Inflammation and Fibrosis in Murine Diabetic Nephropathy. Lab. Invest. 2018, 98, 427–438. [Google Scholar] [CrossRef]
- Taslipinar, A.; Yaman, H.; Yilmaz, M.I.; Demirbas, S.; Saglam, M.; Taslipinar, M.Y.; Agilli, M.; Kurt, Y.G.; Sonmez, A.; Azal, O.; et al. The Relationship between Inflammation, Endothelial Dysfunction and Proteinuria in Patients with Diabetic Nephropathy. Scand. J. Clin. Lab. Invest. 2011, 71, 606–612. [Google Scholar] [CrossRef]
- Feigerlová, E.; Battaglia-Hsu, S.-F. IL-6 Signaling in Diabetic Nephropathy: From Pathophysiology to Therapeutic Perspectives. Cytokine Growth Factor Rev. 2017, 37, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Haase, V.H. Hypoxia-Inducible Factor Signaling in the Development of Kidney Fibrosis. Fibrogenesis Tissue Repair 2012, 5, S16. [Google Scholar] [CrossRef] [PubMed]
- Higgins, D.F.; Kimura, K.; Bernhardt, W.M.; Shrimanker, N.; Akai, Y.; Hohenstein, B.; Saito, Y.; Johnson, R.S.; Kretzler, M.; Cohen, C.D.; et al. Hypoxia Promotes Fibrogenesis in Vivo via HIF-1 Stimulation of Epithelial-to-Mesenchymal Transition. J. Clin. Investig. 2007, 117, 3810–3820. [Google Scholar] [CrossRef] [PubMed]
- Kimura, K.; Iwano, M.; Higgins, D.F.; Yamaguchi, Y.; Nakatani, K.; Harada, K.; Kubo, A.; Akai, Y.; Rankin, E.B.; Neilson, E.G.; et al. Stable Expression of HIF-1alpha in Tubular Epithelial Cells Promotes Interstitial Fibrosis. Am. J. Physiol. Renal Physiol. 2008, 295, F1023–F1029. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Fan, Y.; Gao, Z.; Wang, W.; Shao, N.; Zhang, L.; Yang, Y.; Zhu, W.; Chen, Z.; Hu, J.; et al. HIF-1α Contributes to Ang II-Induced Inflammatory Cytokine Production in Podocytes. BMC Pharmacol. Toxicol. 2019, 20, 59. [Google Scholar] [CrossRef]
- Schietke, R.; Warnecke, C.; Wacker, I.; Schödel, J.; Mole, D.R.; Campean, V.; Amann, K.; Goppelt-Struebe, M.; Behrens, J.; Eckardt, K.-U.; et al. The Lysyl Oxidases LOX and LOXL2 Are Necessary and Sufficient to Repress E-Cadherin in Hypoxia: Insights into Cellular Transformation Processes Mediated by HIF-1. J. Biol. Chem. 2010, 285, 6658–6669. [Google Scholar] [CrossRef]
- Habib, S.L. Diabetes and Renal Tubular Cell Apoptosis. World J. Diabetes 2013, 4, 27–30. [Google Scholar] [CrossRef]
- Jagtap, P.; Szabó, C. Poly(ADP-Ribose) Polymerase and the Therapeutic Effects of Its Inhibitors. Nat. Rev. Drug Discov. 2005, 4, 421–440. [Google Scholar] [CrossRef]
- Lee, S.H.; Yoo, T.-H.; Nam, B.-Y.; Kim, D.K.; Li, J.J.; Jung, D.-S.; Kwak, S.-J.; Ryu, D.-R.; Han, S.H.; Lee, J.E.; et al. Activation of Local Aldosterone System within Podocytes Is Involved in Apoptosis under Diabetic Conditions. Am. J. Physiol. Renal Physiol. 2009, 297, F1381–F1390. [Google Scholar] [CrossRef]
- Liu, F.; Brezniceanu, M.-L.; Wei, C.-C.; Chénier, I.; Sachetelli, S.; Zhang, S.-L.; Filep, J.G.; Ingelfinger, J.R.; Chan, J.S.D. Overexpression of Angiotensinogen Increases Tubular Apoptosis in Diabetes. J. Am. Soc. Nephrol. JASN 2008, 19, 269–280. [Google Scholar] [CrossRef]
- Sanchez-Niño, M.-D.; Benito-Martin, A.; Ortiz, A. New Paradigms in Cell Death in Human Diabetic Nephropathy. Kidney Int. 2010, 78, 737–744. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, V.G.; Gonçalves, G.L.; Costa-Pessoa, J.M.; Thieme, K.; Lins, B.B.; Casare, F.A.M.; de Ponte, M.C.; Camara, N.O.S.; Oliveira-Souza, M. Angiotensin II-Induced Podocyte Apoptosis Is Mediated by Endoplasmic Reticulum Stress/PKC-δ/P38 MAPK Pathway Activation and Trough Increased Na+/H+ Exchanger Isoform 1 Activity. BMC Nephrol. 2018, 19, 179. [Google Scholar] [CrossRef] [PubMed]
- Wallner, M.; Marculescu, R.; Doberer, D.; Wolzt, M.; Wagner, O.; Vitek, L.; Bulmer, A.C.; Wagner, K.-H. Protection from Age-Related Increase in Lipid Biomarkers and Inflammation Contributes to Cardiovascular Protection in Gilbert’s Syndrome. Clin. Sci. Lond. Engl. 1979 2013, 125, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Bahreini, E.; Rezaei-Chianeh, Y.; Nabi-Afjadi, M. Molecular Mechanisms Involved in Intrarenal Renin-Angiotensin and Alternative Pathways in Diabetic Nephropathy—A Review. Rev. Diabet. Stud. RDS 2021, 17, 1–10. [Google Scholar] [CrossRef]
- Yuan, T.; Yang, T.; Chen, H.; Fu, D.; Hu, Y.; Wang, J.; Yuan, Q.; Yu, H.; Xu, W.; Xie, X. New Insights into Oxidative Stress and Inflammation during Diabetes Mellitus-Accelerated Atherosclerosis. Redox Biol. 2018, 20, 247–260. [Google Scholar] [CrossRef]
- Kumar, A.; Pant, P.; Basu, S.; Rao, G.R.K.; Khanna, H.D. Oxidative Stress in Neonatal Hyperbilirubinemia. J. Trop. Pediatr. 2007, 53, 69–71. [Google Scholar] [CrossRef]
- Yan, P.; Zhang, Z.; Miao, Y.; Xu, Y.; Zhu, J.; Wan, Q. Physiological Serum Total Bilirubin Concentrations Were Inversely Associated with Diabetic Peripheral Neuropathy in Chinese Patients with Type 2 Diabetes: A Cross-Sectional Study. Diabetol. Metab. Syndr. 2019, 11, 100. [Google Scholar] [CrossRef]
- Jha, J.C.; Banal, C.; Chow, B.S.M.; Cooper, M.E.; Jandeleit-Dahm, K. Diabetes and Kidney Disease: Role of Oxidative Stress. Antioxid. Redox Signal. 2016, 25, 657–684. [Google Scholar] [CrossRef]
- Boon, A.-C.; Lam, A.K.; Gopalan, V.; Benzie, I.F.; Briskey, D.; Coombes, J.S.; Fassett, R.G.; Bulmer, A.C. Endogenously Elevated Bilirubin Modulates Kidney Function and Protects from Circulating Oxidative Stress in a Rat Model of Adenine-Induced Kidney Failure. Sci. Rep. 2015, 5, 15482. [Google Scholar] [CrossRef]
- Oh, S.W.; Lee, E.S.; Kim, S.; Na, K.Y.; Chae, D.W.; Kim, S.; Chin, H.J. Bilirubin Attenuates the Renal Tubular Injury by Inhibition of Oxidative Stress and Apoptosis. BMC Nephrol. 2013, 14, 105. [Google Scholar] [CrossRef]
- Adin, C.A.; Croker, B.P.; Agarwal, A. Protective Effects of Exogenous Bilirubin on Ischemia-Reperfusion Injury in the Isolated, Perfused Rat Kidney. Am. J. Physiol. Renal Physiol. 2005, 288, F778–F784. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.Y.; Kang, K.J.; Ahn, J.M.; Kim, H.-R.; Na, K.Y.; Chae, D.-W.; Kim, S.; Chin, H.J. Hyperbilirubinemia Reduces the Streptozotocin-Induced Pancreatic Damage through Attenuating the Oxidative Stress in the Gunn Rat. Tohoku J. Exp. Med. 2010, 222, 265–273. [Google Scholar] [CrossRef][Green Version]
- Fujii, M.; Inoguchi, T.; Sasaki, S.; Maeda, Y.; Zheng, J.; Kobayashi, K.; Takayanagi, R. Bilirubin and Biliverdin Protect Rodents against Diabetic Nephropathy by Downregulating NAD(P)H Oxidase. Kidney Int. 2010, 78, 905–919. [Google Scholar] [CrossRef] [PubMed]
- Vera, T.; Stec, D.E. Moderate Hyperbilirubinemia Improves Renal Hemodynamics in ANG II-Dependent Hypertension. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 299, R1044–R1049. [Google Scholar] [CrossRef] [PubMed]
- Stec, D.E.; Hosick, P.A.; Granger, J.P. Bilirubin, Renal Hemodynamics, and Blood Pressure. Front. Pharmacol. 2012, 3, 18. [Google Scholar] [CrossRef]
- Stec, D.E.; Storm, M.V.; Pruett, B.E.; Gousset, M.U. Antihypertensive Actions of Moderate Hyperbilirubinemia: Role of Superoxide Inhibition. Am. J. Hypertens. 2013, 26, 918–923. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Herder, C.; Kannenberg, J.M.; Huth, C.; Carstensen-Kirberg, M.; Rathmann, W.; Koenig, W.; Heier, M.; Püttgen, S.; Thorand, B.; Peters, A.; et al. Proinflammatory Cytokines Predict the Incidence and Progression of Distal Sensorimotor Polyneuropathy: KORA F4/FF4 Study. Diabetes Care 2017, 40, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.; Lee, S.W.; Mo, E.Y.; Moon, S.D.; Han, J.H. Inverse Association between Serum Total Bilirubin Levels and Diabetic Peripheral Neuropathy in Patients with Type 2 Diabetes. Endocrine 2015, 50, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wang, J.; Zhang, X.; Zhu, H. Inverse Relationship Between Serum Bilirubin Levels and Diabetic Foot in Chinese Patients with Type 2 Diabetes Mellitus. Med. Sci. Monit. 2017, 23, 5916–5923. [Google Scholar] [CrossRef]
- Jin, J.; Wang, W.; Gu, T.; Chen, C.; Sun, J.; Chen, W.; Bi, Y.; Zhu, D. Low Serum Bilirubin Levels Contribute to the Presence and Progression of Distal Symmetrical Polyneuropathy in Chinese Patients with Type 2 Diabetes. Diabetes Metab. 2019, 45, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Valaskova, P.; Dvorak, A.; Lenicek, M.; Zizalova, K.; Kutinova-Canova, N.; Zelenka, J.; Cahova, M.; Vitek, L.; Muchova, L. Hyperbilirubinemia in Gunn Rats Is Associated with Decreased Inflammatory Response in LPS-Mediated Systemic Inflammation. Int. J. Mol. Sci. 2019, 20, 2306. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.G.; Ahn, S.-Y.; Lee, E.S.; Kim, S.; Na, K.Y.; Chae, D.-W.; Chin, H.J. Bilirubin Activates Transcription of HIF-1α in Human Proximal Tubular Cells Cultured in the Physiologic Oxygen Content. J. Korean Med. Sci. 2014, 29, S146. [Google Scholar] [CrossRef] [PubMed]
- Bulmer, A.C.; Bakrania, B.; Du Toit, E.F.; Boon, A.-C.; Clark, P.J.; Powell, L.W.; Wagner, K.-H.; Headrick, J.P. Bilirubin Acts as a Multipotent Guardian of Cardiovascular Integrity: More than Just a Radical Idea. Am. J. Physiol. Heart Circ. Physiol. 2018, 315, H429–H447. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Kim, D.H.; Hwang, J.H.; Kim, Y.-C.; Kim, J.H.; Lim, C.S.; Kim, Y.S.; Yang, S.H.; Lee, J.P. Elevated Bilirubin Levels Are Associated with a Better Renal Prognosis and Ameliorate Kidney Fibrosis. PLoS ONE 2017, 12, e0172434. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Tang, L.; Zhu, Q.; Yi, F.; Zhang, F.; Li, P.-L.; Li, N. Hypoxia-Inducible Factor-1α Contributes to the Profibrotic Action of Angiotensin II in Renal Medullary Interstitial Cells. Kidney Int. 2011, 79, 300–310. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.W.; Ahn, J.M.; Lee, Y.-M.; Kim, S.; Chin, H.J.; Chae, D.-W.; Na, K.Y. Activation of Hypoxia-Inducible Factor by Cobalt Is Associated with the Attenuation of Tissue Injury and Apoptosis in Cyclosporine-Induced Nephropathy. Tohoku J. Exp. Med. 2012, 226, 197–206. [Google Scholar] [CrossRef]
- Li, X.; Zhu, Q.; Zheng, R.; Yan, J.; Wei, M.; Fan, Y.; Deng, Y.; Zhong, Y. Puerarin Attenuates Diabetic Nephropathy by Promoting Autophagy in Podocytes. Front. Physiol. 2020, 11, 73. [Google Scholar] [CrossRef]
- Huang, S.-S.; Ding, D.-F.; Chen, S.; Dong, C.-L.; Ye, X.-L.; Yuan, Y.-G.; Feng, Y.-M.; You, N.; Xu, J.-R.; Miao, H.; et al. Resveratrol Protects Podocytes against Apoptosis via Stimulation of Autophagy in a Mouse Model of Diabetic Nephropathy. Sci. Rep. 2017, 7, 45692. [Google Scholar] [CrossRef]
- Qaisiya, M.; Mardešić, P.; Pastore, B.; Tiribelli, C.; Bellarosa, C. The Activation of Autophagy Protects Neurons and Astrocytes against Bilirubin-Induced Cytotoxicity. Neurosci. Lett. 2017, 661, 96–103. [Google Scholar] [CrossRef]
- Dong, C.; Zheng, H.; Huang, S.; You, N.; Xu, J.; Ye, X.; Zhu, Q.; Feng, Y.; You, Q.; Miao, H.; et al. Heme Oxygenase-1 Enhances Autophagy in Podocytes as a Protective Mechanism against High Glucose-Induced Apoptosis. Exp. Cell Res. 2015, 337, 146–159. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bianco, A.; Tiribelli, C.; Bellarosa, C. Translational Approach to the Protective Effect of Bilirubin in Diabetic Kidney Disease. Biomedicines 2022, 10, 696. https://doi.org/10.3390/biomedicines10030696
Bianco A, Tiribelli C, Bellarosa C. Translational Approach to the Protective Effect of Bilirubin in Diabetic Kidney Disease. Biomedicines. 2022; 10(3):696. https://doi.org/10.3390/biomedicines10030696
Chicago/Turabian StyleBianco, Annalisa, Claudio Tiribelli, and Cristina Bellarosa. 2022. "Translational Approach to the Protective Effect of Bilirubin in Diabetic Kidney Disease" Biomedicines 10, no. 3: 696. https://doi.org/10.3390/biomedicines10030696
APA StyleBianco, A., Tiribelli, C., & Bellarosa, C. (2022). Translational Approach to the Protective Effect of Bilirubin in Diabetic Kidney Disease. Biomedicines, 10(3), 696. https://doi.org/10.3390/biomedicines10030696






