Association of Neuropathic Pain Symptoms with Sensitization Related Symptomatology in Women with Fibromyalgia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Neuropathic Pain Assessment: S-LANSS and PainDETECT
2.4. Central Sensitization Inventory
2.5. Pressure Pain Thresholds
2.6. Hospital Anxiety and Depression Scale
2.7. Sample Size Determination
2.8. Statistical Analysis
3. Results
3.1. Bivariate Correlation Analysis
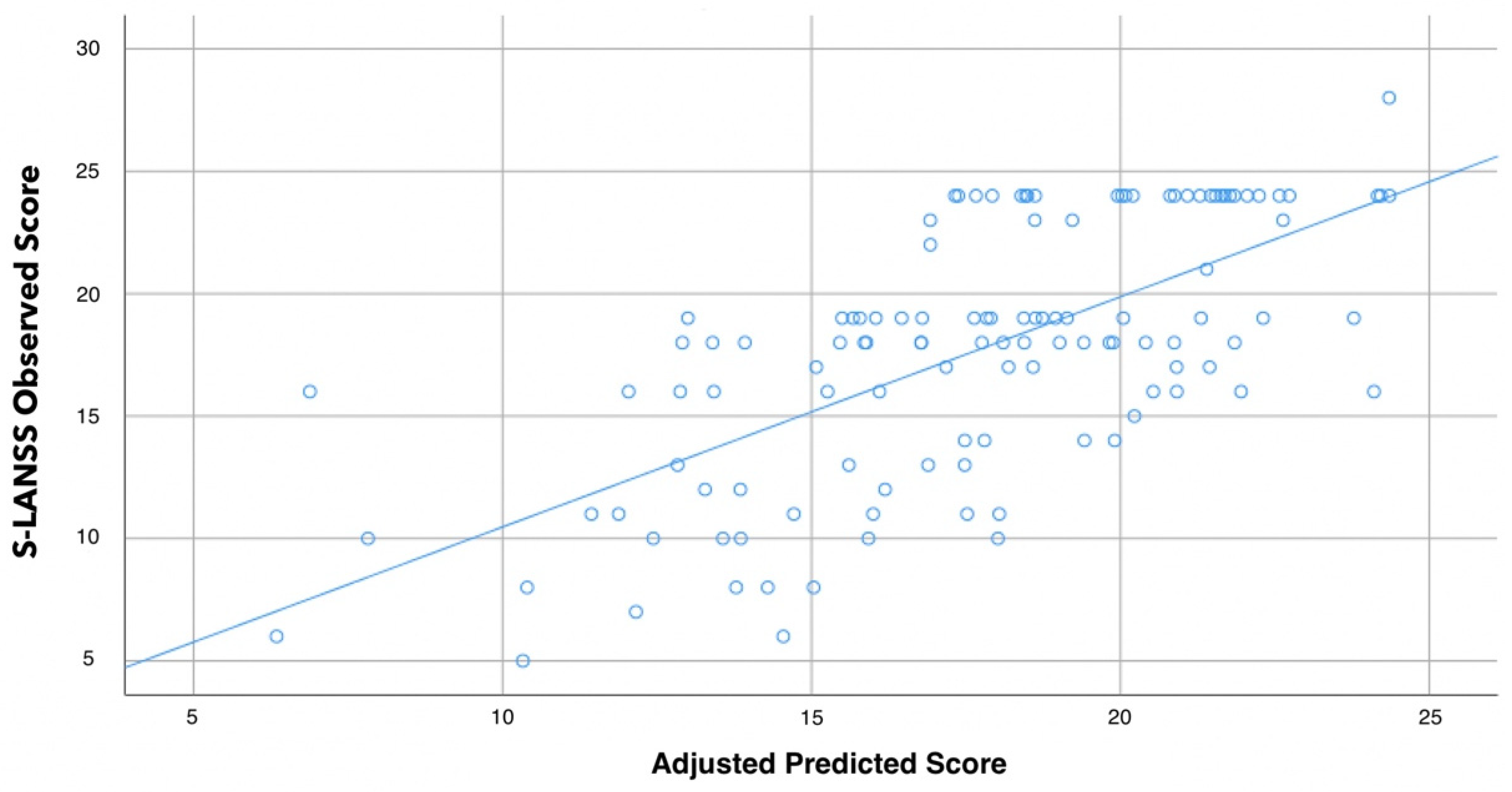
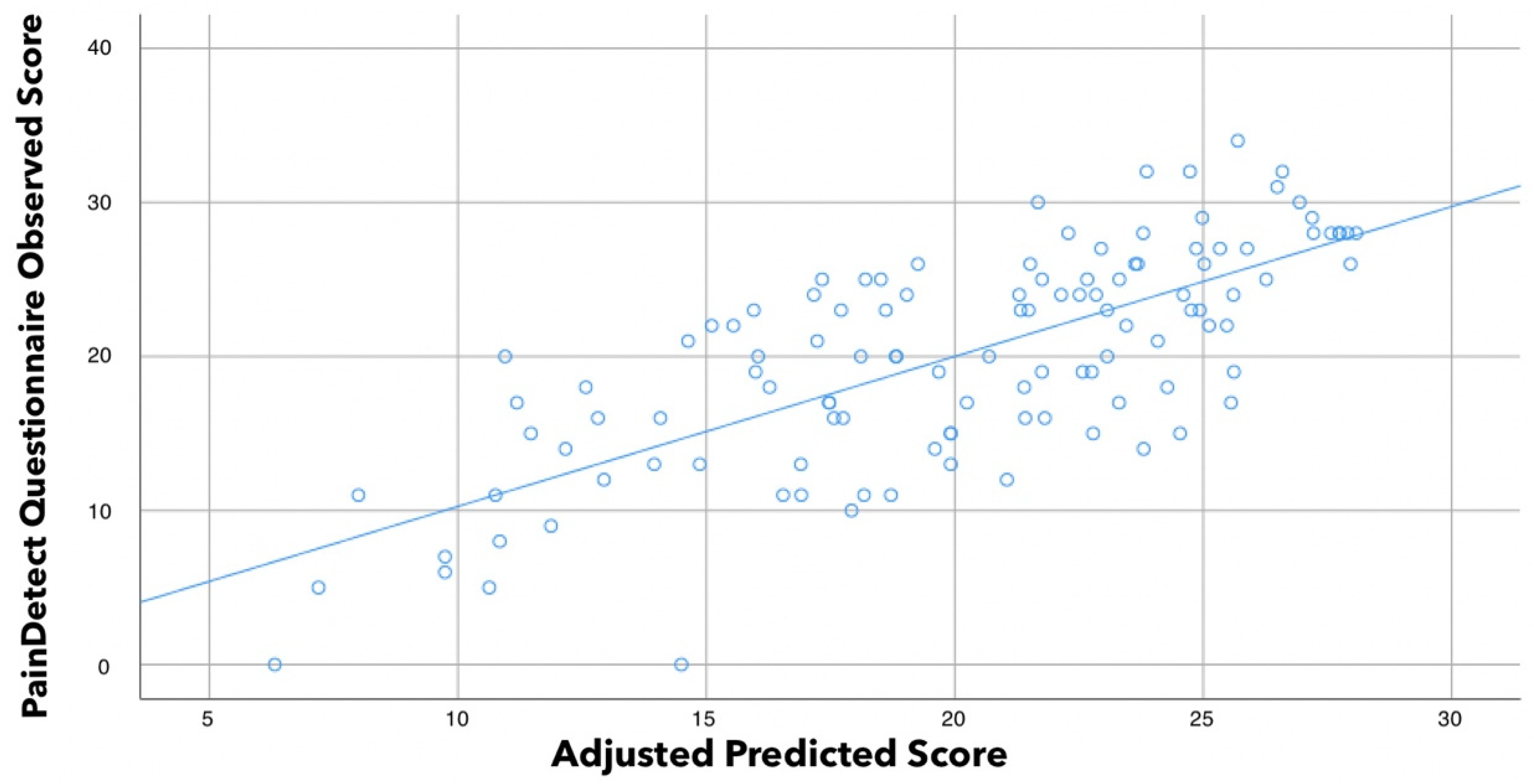
3.2. Multiple Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marques, A.P.; Santo, A.D.S.D.E.; Berssaneti, A.A.; Matsutani, L.A.; Yuan, S.L.K. Prevalence of fibromyalgia: Literature review update. Rev. Bras. Reumatol. Engl. Ed. 2017, 57, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Sumpton, J.E.; Moulin, D.E. Fibromyalgia. Handb. Clin. Neurol. 2014, 119, 513–527. [Google Scholar] [PubMed]
- Boomershine, C.S. Fibromyalgia: The prototypical central sensitivity syndrome. Curr. Rheumatol. Rev. 2015, 11, 131–145. [Google Scholar] [CrossRef] [PubMed]
- Siracusa, R.; Paola, R.; Cuzzocrea, S.; Impellizzeri, D. Fibromyalgia: Pathogenesis, Mechanisms, Diagnosis and Treatment Options Update. Int. J. Mol. Sci. 2021, 22, 3891. [Google Scholar] [CrossRef]
- Cagnie, B.; Coppieters, I.; Denecker, S.; Six, J.; Danneels, L.; Meeus, M. Central sensitization in fibromyalgia? A systematic review on structural and functional brain MRI. Semin. Arthritis Rheum. 2014, 44, 68–75. [Google Scholar] [CrossRef]
- Scholz, J.; Finnerup, N.B.; Attal, N.; Aziz, Q.; Baron, R.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Cruccu, G.; Davis, K.D.; et al. The IASP classification of chronic pain for ICD-11: Chronic neuropathic pain. Pain 2019, 160, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.W.; Wong, C.S.; Hui, G.K.; Chung, E.K.; Wong, S.H. Fibromyalgia: Is it a neuropathic pain? Pain Manag. 2018, 8, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Kosek, E.; Clauw, D.; Nijs, J.; Baron, R.; Gilron, I.; Harris, R.E.; Mico, J.-A.; Rice, A.S.; Sterling, M. Chronic nociplastic pain affecting the musculoskeletal system: Clinical criteria and grading system. Pain 2021, 162, 2629–2634. [Google Scholar] [CrossRef] [PubMed]
- Üçeyler, N.; Zeller, D.; Kahn, A.-K.; Kewenig, S.; Kittel-Schneider, S.; Schmid, A.; Casanova-Molla, J.; Reiners, K.; Sommer, C. Small fibre pathology in patients with fibromyalgia syndrome. Brain 2013, 136, 1857–1867. [Google Scholar] [CrossRef]
- Oaklander, A.L.; Herzog, Z.D.; Downs, H.M.; Klein, M.M. Objective evidence that small-fiber polyneuropathy underlies some ill-nesses currently labeled as fibromyalgia. Pain 2013, 154, 2310–2316. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, M.; Martínez-Martínez, L.-A.; Hernández-Quintela, E.; Velazco-Casapía, J.; Vargas, A.; Martínez-Lavín, M. Small fiber neuropathy in women with fibromyalgia. An in vivo assessment using corneal confocal bio-microscopy. Semin. Arthritis Rheum. 2015, 45, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Doppler, K.; Rittner, H.L.; Deckart, M.; Sommer, C. Reduced dermal nerve fiber diameter in skin biopsies of patients with fibrom-yalgia. Pain 2015, 156, 2319–2325. [Google Scholar] [CrossRef] [PubMed]
- Kösehasanoğullari, M.; Erdinç Gündüz, N.; Akalin, E. Is fibromyalgia syndrome a neuropathic pain syndrome? Arch. Rheumatol. 2018, 34, 196–203. [Google Scholar] [CrossRef]
- Bennett, M.I.; Smith, B.H.; Torrance, N.; Potter, J. The S-LANSS score for identifying pain of predominantly neuropathic origin: Validation for use in clinical and postal research. J. Pain 2005, 6, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Freynhagen, R.; Baron, R.; Gockel, U.; Tölle, T.R. painDETECT: A new screening questionnaire to identify neuropathic components in patients with back pain. Curr. Med. Res. Opin. 2006, 22, 1911–1920. [Google Scholar] [CrossRef]
- Martínez-Lavin, M.; López, S.; Medina, M.; Nava, A. Use of the leeds assessment of neuropathic symptoms and signs question-naire in patients with fibromyalgia. Semin. Arthritis Rheum. 2003, 32, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Gauffin, J.; Hankama, T.; Kautiainen, H.; Hannonen, P.; Haanpää, M. Neuropathic pain and use of PainDETECT in patients with fibromyalgia: A cohort study. BMC Neurol. 2013, 13, 21. [Google Scholar] [CrossRef] [PubMed]
- Amris, K.; Jespersen, A.; Bliddal, H. Self-reported somatosensory symptoms of neuropathic pain in fibromyalgia and chronic widespread pain correlate with tender point count and pressure-pain thresholds. Pain 2010, 151, 664–669. [Google Scholar] [CrossRef]
- Pamuk Ömer, N.; Yeþil, Y.; Çakir, N. Factors That Affect the Number of Tender Points in Fibromyalgia and Chronic Widespread Pain Patients Who Did not Meet the ACR 1990 Criteria for Fibromyalgia: Are Tender Points a Reflection of Neuropathic Pain? Semin. Arthritis Rheum. 2006, 36, 130–134. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Segura-Jiménez, V.; Aparicio, V.A.; Álvarez-Gallardo, I.C.; Soriano-Maldonado, A.; Estévez-López, F.; Delgado-Fernández, M.; Carbonell-Baeza, A. Validation of the modified 2010 American College of Rheumatology diagnostic criteria for fibromyalgia in a Spanish population. Rheumatology 2014, 53, 1803–1811. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Häuser, W.; Katz, R.L.; Mease, P.J.; Russell, A.S.; Russell, I.J.; Walitt, B. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin. Arthritis. Rheum. 2016, 46, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Cheatham, S.W.; Kolber, M.J.; Mokha, M.; Hanney, W.J. Concurrent validity of pain scales in individuals with myofascial pain and fibromyalgia. J. Bodyw. Mov. Ther. 2017, 22, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Neblett, R.; Cohen, H.; Choi, Y.; Hartzell, M.M.; Williams, M.; Mayer, T.G.; Gatchel, R.J. The Central Sensitization Inventory (CSI): Establishing Clinically Significant Values for Identifying Central Sensitivity Syndromes in an Outpatient Chronic Pain Sample. J. Pain 2013, 14, 438–445. [Google Scholar] [CrossRef]
- Úbeda-D’Ocasar, E.; Valera-Calero, J.A.; Hervás-Pérez, J.P.; Caballero-Corella, M.; Ojedo-Martín, C.; Gallego-Sendarrubias, G.M. Pain Intensity and Sensory Perception of Tender Points in Female Patients with Fibromyalgia: A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 1461. [Google Scholar] [CrossRef] [PubMed]
- Nie, H.; Arendt-Nielsen, L.; Andersen, H.; Graven-Nielsen, T. Temporal Summation of Pain Evoked by Mechanical Stimulation in Deep and Superficial Tissue. J. Pain 2005, 6, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Cheatham, S.W.; Kolber, M.J.; Mokha, G.M.; Hanney, W.J. Concurrent validation of a pressure pain threshold scale for individuals with myofascial pain syndrome and fibromyalgia. J. Man. Manip. Ther. 2017, 26, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Herrero, M.J.; Blanch, J.; Peri, J.M.; De Pablo, J.; Pintor, L.; Bulbena, A. A validation study of the hospital anxiety and depression scale (HADS) in a Spanish population. Gen Hosp Psychiatry 2003, 25, 277–283. [Google Scholar] [CrossRef]
- Jenkins, D.G.; Quintana-Ascencio, P.F. A solution to minimum sample size for regressions. PLoS ONE 2020, 15, e0229345. [Google Scholar] [CrossRef] [PubMed]
- Beneciuk, J.M.; Bishop, M.D.; George, S.Z. Clinical Prediction Rules for Physical Therapy Interventions: A Systematic Review. Phys. Ther. 2009, 89, 114–124. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Giske, L.; Bautz-Holter, E.; Sandvik, L.; Røe, C. Relationship Between Pain and Neuropathic Symptoms in Chronic Musculoskeletal Pain. Pain Med. 2009, 10, 910–917. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wilson, H.D.; Starz, T.W.; Robinson, J.P.; Turk, D.C. Heterogeneity Within the Fibromyalgia Population: Theoretical Implications of Variable Tender Point Severity Ratings. J. Rheumatol. 2009, 36, 2795–2801. [Google Scholar] [CrossRef]
- Moreton, B.J.; Tew, V.; das Nair, R.; Wheeler, M.; Walsh, D.A.; Lincoln, N.B. Pain Phenotype in Patients With Knee Osteoarthritis: Classification and Measurement Properties of painDETECT and Self-Report Leeds Assessment of Neuropathic Symptoms and Signs Scale in a Cross-Sectional Study. Arthritis Care Res. 2014, 67, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Amiri, M.; Alavinia, M.; Singh, M.; Kumbhare, D. Pressure pain threshold in patients with chronic pain: A systematic review and meta-analysis. Am. J. Phys. Med. Rehabil. 2021, 100, 656–674. [Google Scholar] [CrossRef]
- Nijs, J.; George, S.Z.; Clauw, D.J.; Fernández-De-Las-Peñas, C.; Kosek, E.; Ickmans, K.; Fernández-Carnero, J.; Polli, A.; Kapreli, E.; Huysmans, E.; et al. Central sensitisation in chronic pain conditions: Latest discoveries and their potential for precision medicine. Lancet Rheumatol. 2021, 3, e383–e392. [Google Scholar] [CrossRef]
- Vollert, J.; Attal, N.; Baron, R.; Freynhagen, R.; Haanpää, M.; Hansson, P.; Jensen, T.S.; Rice, A.S.C.; Segerdahl, M.; Serra, J.; et al. Quantitative sensory testing using DFNS protocol in Europe: An evaluation of heterogeneity across multiple centers in patients with peripheral neuropathic pain and healthy subjects. Pain 2016, 157, 750–758. [Google Scholar] [CrossRef] [PubMed]
- Moss, P.; Benson, H.A.; Will, R.; Wright, A. Patients With Knee Osteoarthritis Who Score Highly on the PainDETECT Questionnaire Present With Multimodality Hyperalgesia, Increased Pain, and Impaired Physical Function. Clin. J. Pain 2018, 34, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Staud, R. Peripheral pain mechanisms in chronic widespread pain. Best Pract. Re.s Clin. Rheumatol. 2011, 25, 155–164. [Google Scholar] [CrossRef]
- Bouhassira, D.; Attal, N.; Alchaar, H.; Boureau, F.; Brochet, B.; Bruxelle, J.; Cunin, G.; Fermanian, J.; Ginies, P.; Grun-Overdyking, A.; et al. Comparison of pain syndromes associated with nervous orsomatic lesions and development of a new Neuropathic pain Diagnostic Questionnaire (DN4). Pain 2005, 114, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Bouhassira, D.; Branders, S.; Attal, N.; Fernandes, A.M.; Demolle, D.; Barbour, J.; de Andrade, D.C.; Pereira, A. Stratification of patients based on the Neuropathic Pain Symptom Inventory: Development and validation of a new algorithm. Pain 2020, 162, 1038–1046. [Google Scholar] [CrossRef] [PubMed]
| Baseline Variable | Female Patients with FMS (n = 126) |
|---|---|
| Sociodemographic characteristics | |
| Age (years) | 52.0 ± 10.7 |
| Height (m) | 1.61 ± 0.06 |
| Weight (kg) | 71.4 ± 16.6 |
| Body Mass Index (kg/cm2) | 27.5 ± 6.2 |
| Clinical characteristics | |
| Years with pain (years) | 20.1 ± 15.3 |
| Years with FMS (years) | 10.2 ± 8.9 |
| Pain intensity (NPRS, 0–10) | |
| Mean at rest | 6.4 ± 1.7 |
| Worst at rest | 7.3 ± 2.2 |
| During daily activities | 8.1 ± 1.9 |
| CSI (0–100) | 70.7 ± 11.6 |
| S-LANSS (0–24) | 17.5 ± 5.5 |
| PainDETECT (0–38) | 19.9 ± 7.1 |
| Psychological characteristics | |
| HADS-A (0–21) | 11.4 ± 3.7 |
| HADS-D (0–21) | 10.0 ± 4.0 |
| Pressure Pain Thresholds | |
| PPT Mastoid (kPa) | 151.2 ± 90.7 |
| PPT Upper Trapezius (kPa) | 125.6 ± 60.4 |
| PPT Elbow (kPa) | 149.0 ± 87.1 |
| PPT Hand (kPa) | 120.2 ± 59.0 |
| PPT Posterosuperior Iliac Spine (kPa) | 233.9 ± 130.7 |
| PPT Greater Trochanter (kPa) | 257.7 ± 123.9 |
| PPT Knee (kPa) | 148.1 ± 107.1 |
| PPT Tibialis Anterior (kPa) | 187.0 ± 108.7 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | |||||||||||||||||||
| 2. BMI | n.s. | ||||||||||||||||||
| 3. Years with pain | 0.566 ** | n.s. | |||||||||||||||||
| 4. Years with FMS | 0.598 ** | n.s. | 0.615 ** | ||||||||||||||||
| 5. Mean pain at rest | n.s. | n.s. | n.s. | n.s. | |||||||||||||||
| 6. Worst pain at rest | n.s. | n.s. | n.s. | n.s. | 0.427 ** | ||||||||||||||
| 7. PDDA | n.s. | n.s. | n.s. | n.s. | 0.302 ** | n.s. | |||||||||||||
| 8. Mastoid PPT | 0.201 * | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | ||||||||||||
| 9. Trapezius PPT | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | 0.399 ** | |||||||||||
| 10. Elbow PPT | 0.244 ** | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | 0.535 ** | 0.580 ** | ||||||||||
| 11. Hand PPT | 0.192 * | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | 0.519 ** | 0.564 ** | 0.726 ** | |||||||||
| 12. Posterior Iliac PPT | 0.195 * | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | 0.502 ** | 0.565 ** | 0.756 ** | 0.563 ** | ||||||||
| 13. Trochanter PPT | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | −0.265 ** | 0.439 ** | 0.625 ** | 0.711 ** | 0.609 ** | 0.658 ** | |||||||
| 14. Knee PPT | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | 0.303 ** | 0.516 ** | 0.470 ** | 0.461 ** | 0.458 ** | 0.523 ** | ||||||
| 15. Tibialis PPT | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | −0.195 * | 0.492 ** | 0.660 ** | 0.804 ** | 0.714 ** | 0.712 ** | 0.812 ** | 0.601 ** | |||||
| 16. CSI | −0.262 ** | n.s. | n.s. | n.s. | 0.305 ** | 0.249 ** | 0.398 ** | −0.371 ** | −0.263 ** | −0.341 ** | −0.221 * | −0.372 ** | −0.418 ** | −0.228 * | −0.332 ** | ||||
| 17. HADS-A | −0.179 * | n.s. | n.s. | −0.187 * | 0.198 * | 0.254 ** | n.s. | −0.223 * | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | 0.541 ** | |||
| 18. HADS-D | −0.181 * | n.s. | −0.299 ** | −0.197 * | n.s. | n.s. | 0.186 * | −0.230 * | −0.250 ** | −0.245 ** | −0.177 * | −0.189 * | −0.212 * | n.s. | −0.247 ** | 0.415 ** | 0.566 ** | ||
| 19. S-LANSS | n.s. | 0.206 * | n.s. | n.s. | 0.237 ** | 0.206 * | 0.298 ** | n.s. | −0.187 * | −0.305 ** | −0.180 * | −0.333 ** | −0.234 ** | −0.208 * | −0.239 ** | 0.336 ** | n.s. | n.s. | |
| 20. PainDetect | −0.272 ** | n.s. | n.s. | n.s. | 0.258 ** | n.s. | 0.439 ** | −0.279 ** | −0.271 ** | −0.331 ** | −0.280 ** | −0.378 ** | −0.352 ** | −0.226 * | −0.343 ** | 0.538 ** | 0.246 ** | 0.258 ** | 0.672 ** |
| Predictor Outcome | Β | SE B | 95% CI | β | t | p | |
|---|---|---|---|---|---|---|---|
| S-LANSS | Step 1 | ||||||
| PainDETECT | 0.519 | 0.051 | 0.418; 0.621 | 0.677 | 10.147 | <0.001 | |
| Step 2 | |||||||
| PainDETECT | 0.493 | 0.055 | 0.384; 0.603 | 0.643 | 8.928 | 0 | |
| Posterior Iliac PPT | −0.004 | 0.003 | −0.010; 0.002 | −0.088 | −1.227 | 0.222 | |
| Step 3 | |||||||
| PainDETECT | 0.514 | 0.053 | 0.408; 0.619 | 0.669 | 9.656 | <0.001 | |
| Posterior Iliac PPT | −0.009 | 0.003 | −0.015; −0.002 | −0.208 | −2.701 | 0.007 | |
| Mastoid PPT | 0.016 | 0.004 | 0.007; 0.024 | 0.258 | 3.485 | 0.001 |
| Predictor Outcome | Β | SE B | 95% CI | β | t | p | |
|---|---|---|---|---|---|---|---|
| PainDETECT | Step 1 | ||||||
| S-LANSS | 0.891 | 0.094 | 0.704; 1.078 | 0.663 | 9.444 | <0.001 | |
| Step 2 | |||||||
| S-LANSS | 0.717 | 0.093 | 0.533; 0.901 | 0.533 | 7.723 | <0.001 | |
| CSI | 0.203 | 0.041 | 0.121; 0.284 | 0.341 | 4.936 | <0.001 | |
| Step 3 | |||||||
| S-LANSS | 0.677 | 0.092 | 0.494; 0.859 | 0.503 | 7.348 | <0.001 | |
| CSI | 0.168 | 0.042 | 0.084; 0.252 | 0.282 | 3.959 | <0.001 | |
| PDDA | 0.662 | 0.258 | 0.150; 1.174 | 0.177 | 2.561 | 0.012 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Úbeda-D’Ocasar, E.; Valera-Calero, J.A.; Gallego-Sendarrubias, G.M.; Fernández-de-las-Peñas, C.; Arias-Buría, J.L.; Morales-Cabezas, M.; Arendt-Nielsen, L.; Cigarán-Méndez, M. Association of Neuropathic Pain Symptoms with Sensitization Related Symptomatology in Women with Fibromyalgia. Biomedicines 2022, 10, 612. https://doi.org/10.3390/biomedicines10030612
Úbeda-D’Ocasar E, Valera-Calero JA, Gallego-Sendarrubias GM, Fernández-de-las-Peñas C, Arias-Buría JL, Morales-Cabezas M, Arendt-Nielsen L, Cigarán-Méndez M. Association of Neuropathic Pain Symptoms with Sensitization Related Symptomatology in Women with Fibromyalgia. Biomedicines. 2022; 10(3):612. https://doi.org/10.3390/biomedicines10030612
Chicago/Turabian StyleÚbeda-D’Ocasar, Edurne, Juan Antonio Valera-Calero, Gracia María Gallego-Sendarrubias, César Fernández-de-las-Peñas, José Luis Arias-Buría, Matilde Morales-Cabezas, Lars Arendt-Nielsen, and Margarita Cigarán-Méndez. 2022. "Association of Neuropathic Pain Symptoms with Sensitization Related Symptomatology in Women with Fibromyalgia" Biomedicines 10, no. 3: 612. https://doi.org/10.3390/biomedicines10030612
APA StyleÚbeda-D’Ocasar, E., Valera-Calero, J. A., Gallego-Sendarrubias, G. M., Fernández-de-las-Peñas, C., Arias-Buría, J. L., Morales-Cabezas, M., Arendt-Nielsen, L., & Cigarán-Méndez, M. (2022). Association of Neuropathic Pain Symptoms with Sensitization Related Symptomatology in Women with Fibromyalgia. Biomedicines, 10(3), 612. https://doi.org/10.3390/biomedicines10030612







