Safety and Tolerability of Oral Cannabinoids in People Living with HIV on Long-Term ART: A Randomized, Open-Label, Interventional Pilot Clinical Trial (CTNPT 028) †
Abstract
1. Introduction
2. Methods
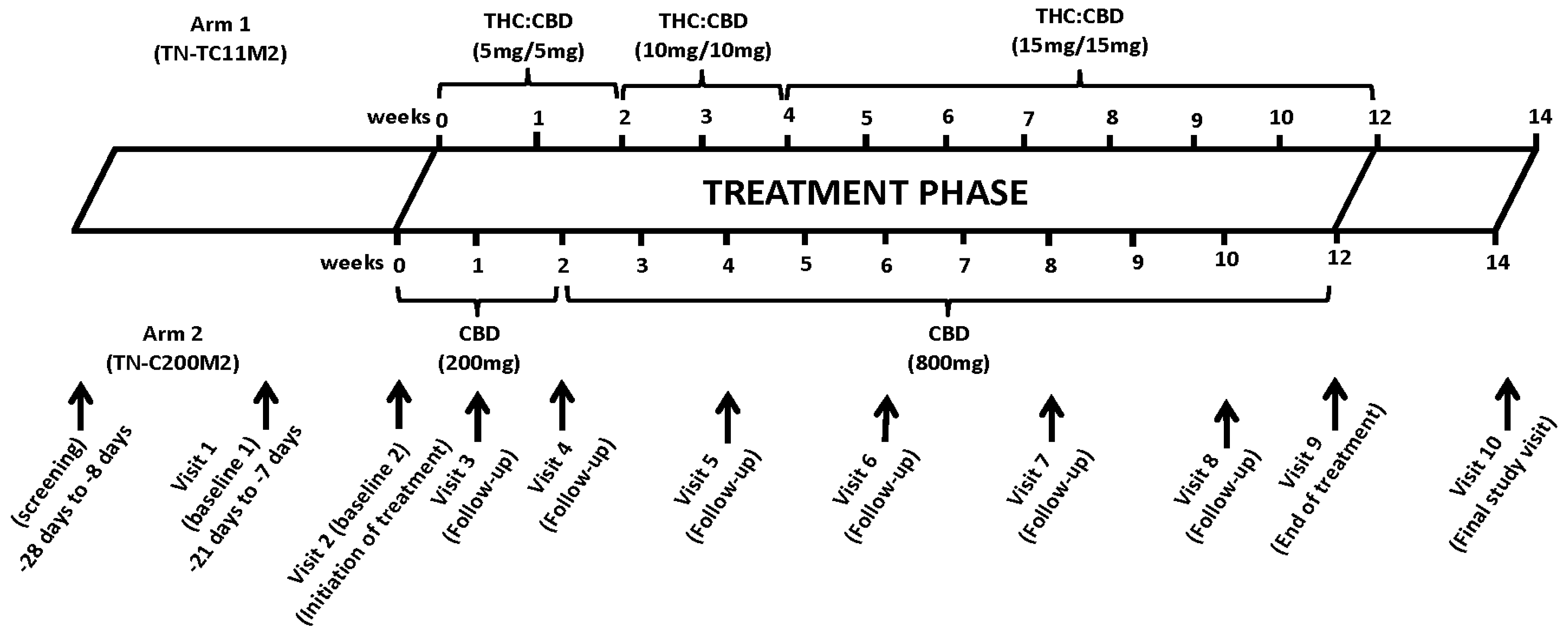
2.1. Study Design
2.2. Enrolment, Selection Criteria and Study Population
2.3. Study Intervention
2.4. Randomization
2.5. Safety and Tolerability Assessments and Specimen Collection
2.6. Quality of Life and Mood Assessment
2.7. Study Outcome Measures
2.8. Ethics
2.9. Statistical Analyses
3. Results
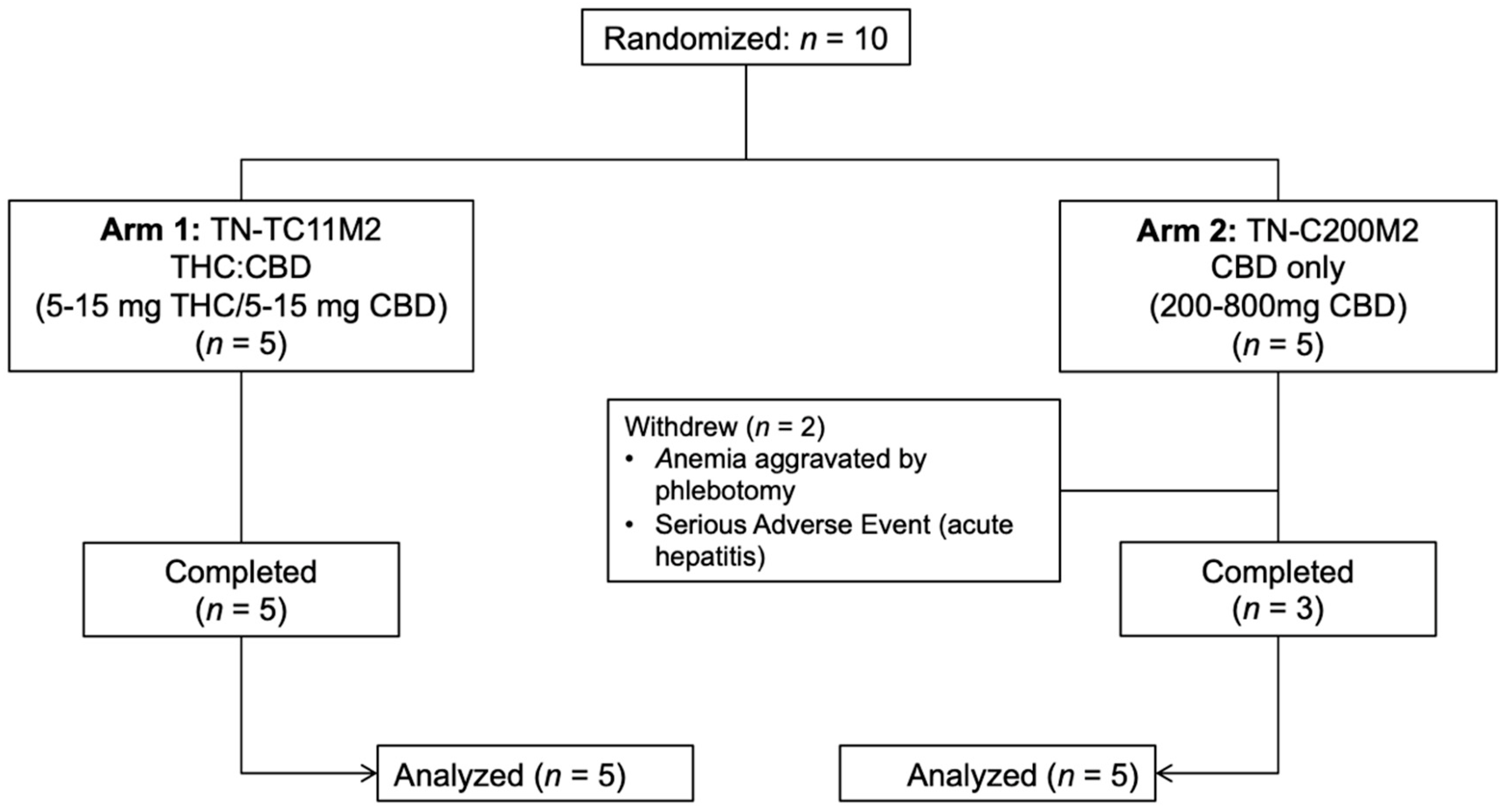
3.1. Study Participants
3.2. Safety and Tolerability
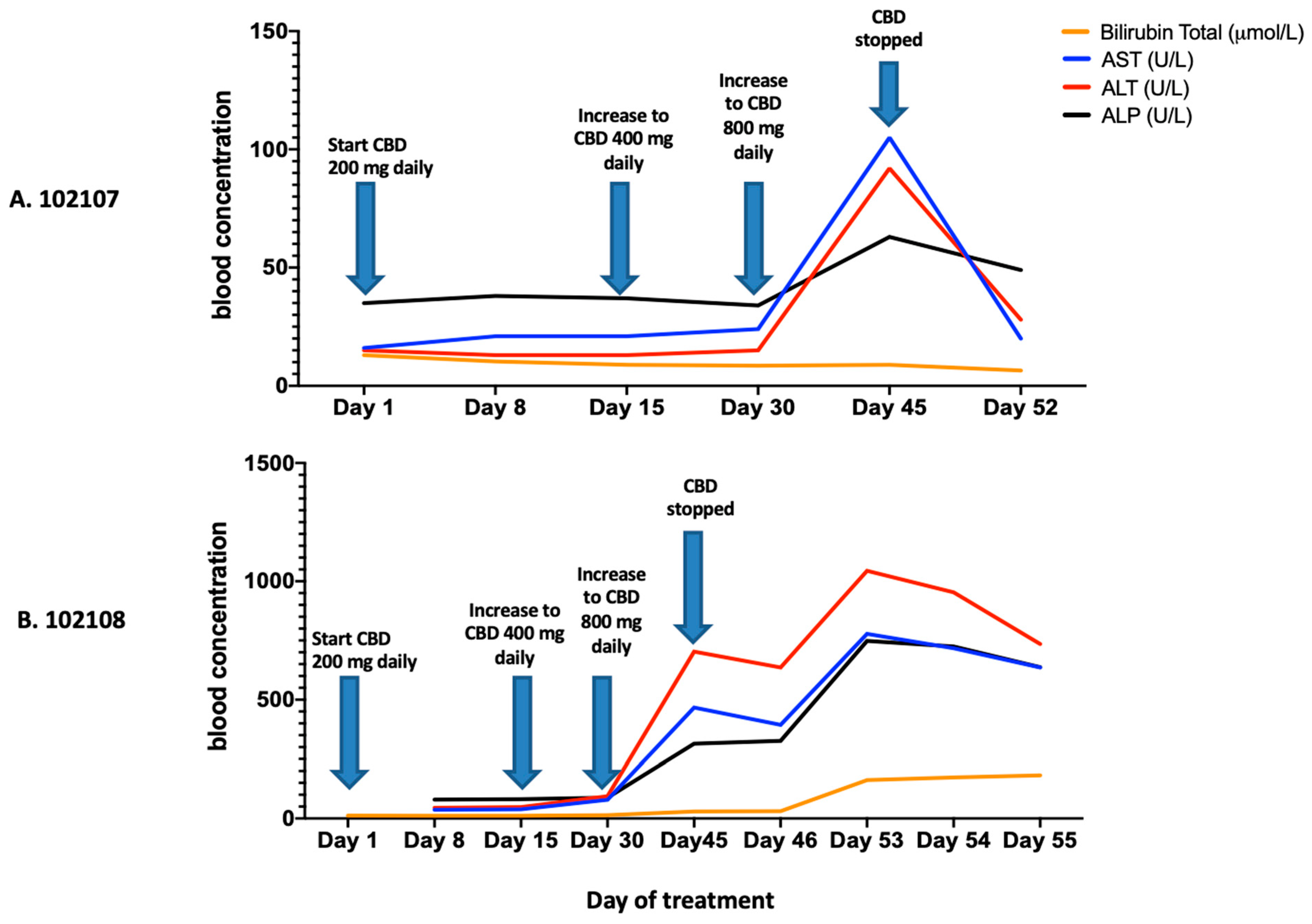
3.3. Hematology, Biochemistry, and HIV Immunology and Virology
3.4. Quality of Life and Mood Assessment
4. Discussion
5. Study Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cassol, E.; Malfeld, S.; Mahasha, P.; van der Merwe, S.; Cassol, S.; Seebregts, C.; Alfano, M.; Poli, G.; Rossouw, T. Persistent microbial translocation and immune activation in HIV-1-infected South Africans receiving combination antiretroviral therapy. J. Infect. Dis. 2010, 202, 723–733. [Google Scholar] [CrossRef] [PubMed]
- Klatt, N.R.; Funderburg, N.T.; Brenchley, J.M. Microbial translocation, immune activation, and HIV disease. Trends Microbiol. 2013, 21, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Marchetti, G.; Tincati, C.; Silvestri, G. Microbial translocation in the pathogenesis of HIV infection and AIDS. Clin. Microbiol. Rev. 2013, 26, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Zicari, S.; Sessa, L.; Cotugno, N.; Ruggiero, A.; Morrocchi, E.; Concato, C.; Rocca, S.; Zangari, P.; Manno, E.C.; Palma, P. Immune Activation, Inflammation, and Non-AIDS Co-Morbidities in HIV-Infected Patients under Long-Term ART. Viruses 2019, 11, 200. [Google Scholar] [CrossRef] [PubMed]
- Baban, B.; Khodadadi, H.; Salles, É.L.; Costigliola, V.; Morgan, J.C.; Hess, D.C.; Vaibhav, K.; Dhandapani, K.M.; Yu, J.C. Inflammaging and Cannabinoids. Ageing Res. Rev. 2021, 72, 101487. [Google Scholar] [CrossRef] [PubMed]
- Costiniuk, C.T.; Jenabian, M.A. Cannabinoids and inflammation: Implications for people living with HIV. Aids 2019, 33, 2273–2288. [Google Scholar] [CrossRef] [PubMed]
- Costiniuk, C.T.; Saneei, Z.; Routy, J.P.; Margolese, S.; Mandarino, E.; Singer, J.; Lebouché, B.; Cox, J.; Szabo, J.; Brouillette, M.J.; et al. Oral cannabinoids in people living with HIV on effective antiretroviral therapy: CTN PT028-study protocol for a pilot randomised trial to assess safety, tolerability and effect on immune activation. BMJ Open 2019, 9, e024793. [Google Scholar] [CrossRef]
- Hsu, D.C.; Sereti, I. Serious Non-AIDS Events: Therapeutic Targets of Immune Activation and Chronic Inflammation in HIV Infection. Drugs 2016, 76, 533–549. [Google Scholar] [CrossRef]
- Furler, M.D.; Einarson, T.R.; Millson, M.; Walmsley, S.; Bendayan, R. Medicinal and recreational marijuana use by patients infected with HIV. AIDS Patient Care STDS 2004, 18, 215–228. [Google Scholar] [CrossRef]
- Abrams, D.I.; Jay, C.A.; Shade, S.B.; Vizoso, H.; Reda, H.; Press, S.; Kelly, M.E.; Rowbotham, M.C.; Petersen, K.L. Cannabis in painful HIV-associated sensory neuropathy: A randomized placebo-controlled trial. Neurology 2007, 68, 515–521. [Google Scholar] [CrossRef]
- Belle-Isle, L.; Hathaway, A. Barriers to access to medical cannabis for Canadians living with HIV/AIDS. AIDS Care 2007, 19, 500–506. [Google Scholar] [CrossRef]
- Ellis, R.J.; Toperoff, W.; Vaida, F.; van den Brande, G.; Gonzales, J.; Gouaux, B.; Bentley, H.; Atkinson, J.H. Smoked medicinal cannabis for neuropathic pain in HIV: A randomized, crossover clinical trial. Neuropsychopharmacology 2009, 34, 672–680. [Google Scholar] [CrossRef]
- Harris, G.E.; Dupuis, L.; Mugford, G.J.; Johnston, L.; Haase, D.; Page, G.; Haldane, H.; Harris, N.; Midodzi, W.K.; Dow, G. Patterns and correlates of cannabis use among individuals with HIV/AIDS in Maritime Canada. Can. J. Infect. Dis. Med. Microbiol. 2014, 25, e1–e7. [Google Scholar] [CrossRef]
- Anil, S.M.; Shalev, N.; Vinayaka, A.C.; Nadarajan, S.; Namdar, D.; Belausov, E.; Shoval, I.; Mani, K.A.; Mechrez, G.; Koltai, H. Cannabis compounds exhibit anti-inflammatory activity in vitro in COVID-19-related inflammation in lung epithelial cells and pro-inflammatory activity in macrophages. Sci. Rep. 2021, 11, 1462. [Google Scholar] [CrossRef]
- DeMarino, C.; Cowen, M.; Khatkar, P.; Cotto, B.; Branscome, H.; Kim, Y.; Sharif, S.A.; Agbottah, E.T.; Zhou, W.; Costiniuk, C.T.; et al. Cannabinoids Reduce Extracellular Vesicle Release from HIV-1 Infected Myeloid Cells and Inhibit Viral Transcription. Cells 2022, 11, 723. [Google Scholar] [CrossRef]
- Henriquez, J.E.; Rizzo, M.D.; Schulz, M.A.; Crawford, R.B.; Gulick, P.; Kaminski, N.E. Δ9-Tetrahydrocannabinol Suppresses Secretion of IFNα by Plasmacytoid Dendritic Cells From Healthy and HIV-Infected Individuals. J. Acquir. Immune Defic. Syndr. 2017, 75, 588–596. [Google Scholar] [CrossRef]
- Janecki, M.; Graczyk, M.; Lewandowska, A.A.; Pawlak, Ł. Anti-Inflammatory and Antiviral Effects of Cannabinoids in Inhibiting and Preventing SARS-CoV-2 Infection. Int. J. Mol. Sci. 2022, 23, 4170. [Google Scholar] [CrossRef]
- Suryavanshi, S.V.; Zaiachuk, M.; Pryimak, N.; Kovalchuk, I.; Kovalchuk, O. Cannabinoids Alleviate the LPS-Induced Cytokine Storm via Attenuating NLRP3 Inflammasome Signaling and TYK2-Mediated STAT3 Signaling Pathways In Vitro. Cells 2022, 11, 1391. [Google Scholar] [CrossRef]
- Carmona-Hidalgo, B.; González-Mariscal, I.; García-Martín, A.; Prados, M.E.; Ruiz-Pino, F.; Appendino, G.; Tena-Sempere, M.; Muñoz, E. Δ9-Tetrahydrocannabinolic Acid markedly alleviates liver fibrosis and inflammation in mice. Phytomedicine 2021, 81, 153426. [Google Scholar] [CrossRef]
- Chandra, L.C.; Kumar, V.; Torben, W.; Stouwe, C.V.; Winsauer, P.; Amedee, A.; Molina, P.E.; Mohan, M. Chronic administration of Δ9-tetrahydrocannabinol induces intestinal anti-inflammatory microRNA expression during acute simian immunodeficiency virus infection of rhesus macaques. J. Virol. 2015, 89, 1168–1181. [Google Scholar] [CrossRef]
- Kumar, V.; Torben, W.; Mansfield, J.; Alvarez, X.; Stouwe, C.V.; Li, J.; Byrareddy, S.N.; Didier, P.J.; Pahar, B.; Molina, P.E.; et al. Cannabinoid Attenuation of Intestinal Inflammation in Chronic SIV-Infected Rhesus Macaques Involves T Cell Modulation and Differential Expression of Micro-RNAs and Pro-inflammatory Genes. Front. Immunol. 2019, 10, 914. [Google Scholar] [CrossRef]
- McDew-White, M.; Lee, E.; Alvarez, X.; Sestak, K.; Ling, B.J.; Byrareddy, S.N.; Okeoma, C.M.; Mohan, M. Cannabinoid control of gingival immune activation in chronically SIV-infected rhesus macaques involves modulation of the indoleamine-2,3-dioxygenase-1 pathway and salivary microbiome. EBioMedicine 2022, 75, 103769. [Google Scholar] [CrossRef] [PubMed]
- Manuzak, J.A.; Gott, T.M.; Kirkwood, J.S.; Coronado, E.; Hensley-McBain, T.; Miller, C.; Cheu, R.K.; Collier, A.C.; Funderburg, N.T.; Martin, J.N.; et al. Heavy Cannabis Use Associated With Reduction in Activated and Inflammatory Immune Cell Frequencies in Antiretroviral Therapy-Treated Human Immunodeficiency Virus-Infected Individuals. Clin. Infect. Dis. 2018, 66, 1872–1882. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, M.D.; Crawford, R.B.; Henriquez, J.E.; Aldhamen, Y.A.; Gulick, P.; Amalfitano, A.; Kaminski, N.E. HIV-infected cannabis users have lower circulating CD16+ monocytes and IFN-γ-inducible protein 10 levels compared with nonusing HIV patients. Aids 2018, 32, 419–429. [Google Scholar] [CrossRef] [PubMed]
- Yin, L.; Dinasarapu, A.R.; Borkar, S.A.; Chang, K.F.; De Paris, K.; Kim-Chang, J.J.; Sleasman, J.W.; Goodenow, M.M. Anti-inflammatory effects of recreational marijuana in virally suppressed youth with HIV-1 are reversed by use of tobacco products in combination with marijuana. Retrovirology 2022, 19, 10. [Google Scholar] [CrossRef] [PubMed]
- Canada, H. Understanding the New Access to Cannabis for Medical Purposes Regulations. 2016. Available online: https://www.canada.ca/en/health-canada/services/publications/drugs-health-products/understanding-new-access-to-cannabis-for-medical-purposes-regulations.html (accessed on 20 August 2022).
- Hawke, L.D.; Henderson, J. Legalization of cannabis use in Canada: Impacts on the cannabis use profiles of youth seeking services for substance use. J. Subst. Abuse Treat 2021, 126, 108340. [Google Scholar] [CrossRef]
- Solowij, N.; Broyd, S.; Greenwood, L.M.; van Hell, H.; Martelozzo, D.; Rueb, K.; Todd, J.; Liu, Z.; Galettis, P.; Martin, J.; et al. A randomised controlled trial of vaporised Δ(9)-tetrahydrocannabinol and cannabidiol alone and in combination in frequent and infrequent cannabis users: Acute intoxication effects. Eur. Arch. Psychiatry Clin. Neurosci. 2019, 269, 17–35. [Google Scholar] [CrossRef]
- Windle, S.B.; Wade, K.; Filion, K.B.; Kimmelman, J.; Thombs, B.D.; Eisenberg, M.J. Potential harms from legalization of recreational cannabis use in Canada. Can. J. Public Health 2019, 110, 222–226. [Google Scholar] [CrossRef]
- Bergamaschi, M.M.; Queiroz, R.H.; Zuardi, A.W.; Crippa, J.A. Safety and side effects of cannabidiol, a Cannabis sativa constituent. Curr. Drug Saf. 2011, 6, 237–249. [Google Scholar] [CrossRef]
- Burstein, S. Cannabidiol (CBD) and its analogs: A review of their effects on inflammation. Bioorg. Med. Chem. 2015, 23, 1377–1385. [Google Scholar] [CrossRef]
- Burstein, S.H.; Zurier, R.B. Cannabinoids, endocannabinoids, and related analogs in inflammation. AAPS J. 2009, 11, 109–119. [Google Scholar] [CrossRef]
- Iuvone, T.; Esposito, G.; De Filippis, D.; Scuderi, C.; Steardo, L. Cannabidiol: A promising drug for neurodegenerative disorders? CNS Neurosci. Ther. 2009, 15, 65–75. [Google Scholar] [CrossRef]
- Ribeiro, A.; Ferraz-de-Paula, V.; Pinheiro, M.L.; Vitoretti, L.B.; Mariano-Souza, D.P.; Quinteiro-Filho, W.M.; Akamine, A.T.; Almeida, V.I.; Quevedo, J.; Dal-Pizzol, F.; et al. Cannabidiol, a non-psychotropic plant-derived cannabinoid, decreases inflammation in a murine model of acute lung injury: Role for the adenosine A(2A) receptor. Eur. J. Pharmacol. 2012, 678, 78–85. [Google Scholar] [CrossRef]
- Zgair, A.; Lee, J.B.; Wong, J.C.M.; Taha, D.A.; Aram, J.; Di Virgilio, D.; McArthur, J.W.; Cheng, Y.K.; Hennig, I.M.; Barrett, D.A.; et al. Oral administration of cannabis with lipids leads to high levels of cannabinoids in the intestinal lymphatic system and prominent immunomodulation. Sci. Rep. 2017, 7, 14542. [Google Scholar] [CrossRef]
- Sachse-Seeboth, C.; Pfeil, J.; Sehrt, D.; Meineke, I.; Tzvetkov, M.; Bruns, E.; Poser, W.; Vormfelde, S.V.; Brockmöller, J. Interindividual variation in the pharmacokinetics of Delta9-tetrahydrocannabinol as related to genetic polymorphisms in CYP2C9. Clin. Pharmacol. Ther. 2009, 85, 273–276. [Google Scholar] [CrossRef]
- Ware, M.A.; Wang, T.; Shapiro, S.; Collet, J.P. Cannabis for the Management of Pain: Assessment of Safety Study (COMPASS). J. Pain 2015, 16, 1233–1242. [Google Scholar] [CrossRef]
- Leweke, F.M.; Rohleder, C.; Gerth, C.W.; Hellmich, M.; Pukrop, R.; Koethe, D. Cannabidiol and Amisulpride Improve Cognition in Acute Schizophrenia in an Explorative, Double-Blind, Active-Controlled, Randomized Clinical Trial. Front. Pharmacol. 2021, 12, 614811. [Google Scholar] [CrossRef]
- Leweke, F.M.; Piomelli, D.; Pahlisch, F.; Muhl, D.; Gerth, C.W.; Hoyer, C.; Klosterkötter, J.; Hellmich, M.; Koethe, D. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl. Psychiatry 2012, 2, e94. [Google Scholar] [CrossRef]
- Thiele, E.A.; Marsh, E.D.; French, J.A.; Mazurkiewicz-Beldzinska, M.; Benbadis, S.R.; Joshi, C.; Lyons, P.D.; Taylor, A.; Roberts, C.; Sommerville, K. Cannabidiol in patients with seizures associated with Lennox-Gastaut syndrome (GWPCARE4): A randomised, double-blind, placebo-controlled phase 3 trial. Lancet 2018, 391, 1085–1096. [Google Scholar] [CrossRef]
- Wade, D.T.; Makela, P.; Robson, P.; House, H.; Bateman, C. Do cannabis-based medicinal extracts have general or specific effects on symptoms in multiple sclerosis? A double-blind, randomized, placebo-controlled study on 160 patients. Mult. Scler. 2004, 10, 434–441. [Google Scholar] [CrossRef]
- World Health Organization. WHOQOL-HIV Bref; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed]
- McNair, D.M.; Lorr, M.; Droppleman, L.F. Manual for the Profile of Mood States; Educational and Industrial Testing Services: San Diego, CA, USA, 1971. [Google Scholar]
- Berman, J.S.; Symonds, C.; Birch, R. Efficacy of two cannabis based medicinal extracts for relief of central neuropathic pain from brachial plexus avulsion: Results of a randomised controlled trial. Pain 2004, 112, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Devinsky, O.; Cross, J.H.; Laux, L.; Marsh, E.; Miller, I.; Nabbout, R.; Scheffer, I.E.; Thiele, E.A.; Wright, S. Trial of Cannabidiol for Drug-Resistant Seizures in the Dravet Syndrome. N. Engl. J. Med. 2017, 376, 2011–2020. [Google Scholar] [CrossRef] [PubMed]
- Devinsky, O.; Patel, A.D.; Cross, J.H.; Villanueva, V.; Wirrell, E.C.; Privitera, M.; Greenwood, S.M.; Roberts, C.; Checketts, D.; VanLandingham, K.E.; et al. Effect of Cannabidiol on Drop Seizures in the Lennox-Gastaut Syndrome. N. Engl. J. Med. 2018, 378, 1888–1897. [Google Scholar] [CrossRef] [PubMed]
- Devinsky, O.; Verducci, C.; Thiele, E.A.; Laux, L.C.; Patel, A.D.; Filloux, F.; Szaflarski, J.P.; Wilfong, A.; Clark, G.D.; Park, Y.D.; et al. Open-label use of highly purified CBD (Epidiolex®) in patients with CDKL5 deficiency disorder and Aicardi, Dup15q, and Doose syndromes. Epilepsy Behav. 2018, 86, 131–137. [Google Scholar] [CrossRef]
- Langford, R.M.; Mares, J.; Novotna, A.; Vachova, M.; Novakova, I.; Notcutt, W.; Ratcliffe, S. A double-blind, randomized, placebo-controlled, parallel-group study of THC/CBD oromucosal spray in combination with the existing treatment regimen, in the relief of central neuropathic pain in patients with multiple sclerosis. J. Neurol. 2013, 260, 984–997. [Google Scholar] [CrossRef]
- Miller, I.; Scheffer, I.E.; Gunning, B.; Sanchez-Carpintero, R.; Gil-Nagel, A.; Perry, M.S.; Saneto, R.P.; Checketts, D.; Dunayevich, E.; Knappertz, V. Dose-Ranging Effect of Adjunctive Oral Cannabidiol vs Placebo on Convulsive Seizure Frequency in Dravet Syndrome: A Randomized Clinical Trial. JAMA Neurol. 2020, 77, 613–621. [Google Scholar] [CrossRef]
- Nurmikko, T.J.; Serpell, M.G.; Hoggart, B.; Toomey, P.J.; Morlion, B.J.; Haines, D. Sativex successfully treats neuropathic pain characterised by allodynia: A randomised, double-blind, placebo-controlled clinical trial. Pain 2007, 133, 210–220. [Google Scholar] [CrossRef]
- Rog, D.J.; Nurmikko, T.J.; Friede, T.; Young, C.A. Randomized, controlled trial of cannabis-based medicine in central pain in multiple sclerosis. Neurology 2005, 65, 812–819. [Google Scholar] [CrossRef]
- Serpell, M.; Ratcliffe, S.; Hovorka, J.; Schofield, M.; Taylor, L.; Lauder, H.; Ehler, E. A double-blind, randomized, placebo-controlled, parallel group study of THC/CBD spray in peripheral neuropathic pain treatment. Eur. J. Pain 2014, 18, 999–1012. [Google Scholar] [CrossRef]
- Thiele, E.A.; Bebin, E.M.; Filloux, F.; Kwan, P.; Loftus, R.; Sahebkar, F.; Sparagana, S.; Wheless, J. Long-term cannabidiol treatment for seizures in patients with tuberous sclerosis complex: An open-label extension trial. Epilepsia 2022, 63, 426–439. [Google Scholar] [CrossRef]
- Ueberall, M.A.; Essner, U.; Mueller-Schwefe, G.H. Effectiveness and tolerability of THC:CBD oromucosal spray as add-on measure in patients with severe chronic pain: Analysis of 12-week open-label real-world data provided by the German Pain e-Registry. J. Pain Res. 2019, 12, 1577–1604. [Google Scholar] [CrossRef]
- Watkins, P.B.; Church, R.J.; Li, J.; Knappertz, V. Cannabidiol and Abnormal Liver Chemistries in Healthy Adults: Results of a Phase I Clinical Trial. Clin. Pharmacol. Ther. 2021, 109, 1224–1231. [Google Scholar] [CrossRef]
- Chesney, E.; Oliver, D.; Green, A.; Sovi, S.; Wilson, J.; Englund, A.; Freeman, T.P.; McGuire, P. Adverse effects of cannabidiol: A systematic review and meta-analysis of randomized clinical trials. Neuropsychopharmacology 2020, 45, 1799–1806. [Google Scholar] [CrossRef]
- Kaufmann, R.; Aqua, K.; Lombardo, J.; Lee, M. Observed Impact of Long-term Consumption of Oral Cannabidiol on Liver Function in Healthy Adults. Cannabis Cannabinoid Res. 2021; ahead of print. [Google Scholar] [CrossRef]
- Abelev, S.; Warne, L.N.; Benson, M.; Hardy, M.; Nayee, S.; Barlow, J. Medicinal Cannabis for the Treatment of Chronic Refractory Pain: An Investigation of the Adverse Event Profile and Health-Related Quality of Life Impact of an Oral Formulation. Med. Cannabis Cannabinoids 2022, 5, 20–31. [Google Scholar] [CrossRef]
- Jiang, R.; Yamaori, S.; Okamoto, Y.; Yamamoto, I.; Watanabe, K. Cannabidiol is a potent inhibitor of the catalytic activity of cytochrome P450 2C19. Drug Metab. Pharmacokinet. 2013, 28, 332–338. [Google Scholar] [CrossRef]
- Stout, S.M.; Cimino, N.M. Exogenous cannabinoids as substrates, inhibitors, and inducers of human drug metabolizing enzymes: A systematic review. Drug Metab. Rev. 2014, 46, 86–95. [Google Scholar] [CrossRef]
- González-Mariscal, I.; Pozo-Morales, M.; Romero-Zerbo, S.Y.; Espinosa-Jimenez, V.; Escamilla-Sánchez, A.; Sánchez-Salido, L.; Cobo-Vuilleumier, N.; Gauthier, B.R.; Bermúdez-Silva, F.J. Abnormal cannabidiol ameliorates inflammation preserving pancreatic beta cells in mouse models of experimental type 1 diabetes and beta cell damage. Biomed. Pharmacother. 2022, 145, 112361. [Google Scholar] [CrossRef]
- González-Mariscal, I.; Krzysik-Walker, S.M.; Doyle, M.E.; Liu, Q.R.; Cimbro, R.; Santa-Cruz Calvo, S.; Ghosh, S.; Cieśla, Ł.; Moaddel, R.; Carlson, O.D.; et al. Human CB1 Receptor Isoforms, present in Hepatocytes and β-cells, are Involved in Regulating Metabolism. Sci. Rep. 2016, 6, 33302. [Google Scholar] [CrossRef]
- Engeli, S. Dysregulation of the endocannabinoid system in obesity. J. Neuroendocrinol. 2008, 20 (Suppl. 1), 110–115. [Google Scholar] [CrossRef] [PubMed]
- González-Mariscal, I.; Krzysik-Walker, S.M.; Kim, W.; Rouse, M.; Egan, J.M. Blockade of cannabinoid 1 receptor improves GLP-1R mediated insulin secretion in mice. Mol. Cell Endocrinol. 2016, 423, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Jourdan, T.; Godlewski, G.; Cinar, R.; Bertola, A.; Szanda, G.; Liu, J.; Tam, J.; Han, T.; Mukhopadhyay, B.; Skarulis, M.C.; et al. Activation of the Nlrp3 inflammasome in infiltrating macrophages by endocannabinoids mediates beta cell loss in type 2 diabetes. Nat. Med. 2013, 19, 1132–1140. [Google Scholar] [CrossRef]
- González-Mariscal, I.; Montoro, R.A.; Doyle, M.E.; Liu, Q.R.; Rouse, M.; O’Connell, J.F.; Calvo, S.S.-C.; Krzysik-Walker, S.M.; Ghosh, S.; Carlson, O.D.; et al. Absence of cannabinoid 1 receptor in beta cells protects against high-fat/high-sugar diet-induced beta cell dysfunction and inflammation in murine islets. Diabetologia 2018, 61, 1470–1483. [Google Scholar] [CrossRef] [PubMed]
- Cinar, R.; Godlewski, G.; Liu, J.; Tam, J.; Jourdan, T.; Mukhopadhyay, B.; Harvey-White, J.; Kunos, G. Hepatic cannabinoid-1 receptors mediate diet-induced insulin resistance by increasing de novo synthesis of long-chain ceramides. Hepatology 2014, 59, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Bouassa, R.-S.M.; Sebastiani, G.; Di Marzo, V.; Jenabian, M.-A.; Costiniuk, C.T. Cannabinoids and Chronic Liver Diseases. Int. J. Mol. Sci. 2022, 23, 9423. [Google Scholar] [CrossRef]
- Penner, E.A.; Buettner, H.; Mittleman, M.A. The impact of marijuana use on glucose, insulin, and insulin resistance among US adults. Am. J. Med. 2013, 126, 583–589. [Google Scholar] [CrossRef]
- Rajavashisth, T.B.; Shaheen, M.; Norris, K.C.; Pan, D.; Sinha, S.K.; Ortega, J.; Friedman, T.C. Decreased prevalence of diabetes in marijuana users: Cross-sectional data from the National Health and Nutrition Examination Survey (NHANES) III. BMJ Open 2012, 2, e000494. [Google Scholar] [CrossRef]
- Vidot, D.C.; Prado, G.; Hlaing, W.M.; Florez, H.J.; Arheart, K.L.; Messiah, S.E. Metabolic Syndrome Among Marijuana Users in the United States: An Analysis of National Health and Nutrition Examination Survey Data. Am. J. Med. 2016, 129, 173–179. [Google Scholar] [CrossRef]
- Jadoon, K.A.; Ratcliffe, S.H.; Barrett, D.A.; Thomas, E.L.; Stott, C.; Bell, J.D.; O’Sullivan, S.E.; Tan, G.D. Efficacy and Safety of Cannabidiol and Tetrahydrocannabivarin on Glycemic and Lipid Parameters in Patients with Type 2 Diabetes: A Randomized, Double-Blind, Placebo-Controlled, Parallel Group Pilot Study. Diabetes Care 2016, 39, 1777–1786. [Google Scholar] [CrossRef]
- Costiniuk, C.T.; Saneei, Z.; Salahuddin, S.; Cox, J.; Routy, J.P.; Rueda, S.; Abdallah, S.J.; Jensen, D.; Lebouché, B.; Brouillette, M.J.; et al. Cannabis Consumption in People Living with HIV: Reasons for Use, Secondary Effects, and Opportunities for Health Education. Cannabis Cannabinoid Res. 2019, 4, 204–213. [Google Scholar] [CrossRef]

| Arm 1 (TN-TC11M2: (THC: 2.5 mg/CBD: 2.5 mg)) | Arm 2 (TN-C200M2: CBD; 200 mg) Original Titration Schedule * | Arm 2 (TN-C200M2: CBD; 200 mg) Revised Titration Schedule # | ||||||
|---|---|---|---|---|---|---|---|---|
| Weeks | Daily Dose | Number of Capsules (Taken Orally and Spaced Out Every 12 h) | Weeks | Daily Dose | Number of Capsules (Taken Orally and Spaced Out Every 12 h) | Weeks | Daily Dose | Number of Capsules (Taken Orally and Spaced Out Every 12 h) |
| Week 0 and 1 (Day 1–14) | 5 mg THC/5 mg CBD | 1 capsule twice daily (2 capsules per day) | Week 0 and 1 (Day 1–14) | 200 mg CBD | 1 capsule once daily | Week 0 and 1 (Day 1–14) | 200 mg CBD | 1 capsule once daily |
| Week 2 and 3 (Day 15–28) | 10 mg THC/10 mg CBD | 2 capsules twice daily, (4 capsules per day) | Week 2 and 3 (Day 15–28) | 400 mg CBD | 1 capsule twice daily (2 capsules per day) | Week 2–11 (Day 15–84) | 400 mg CBD | 1 capsule twice daily (2 capsules per day) |
| Week 4–11(Day 29–84) | 15 mg THC/15 mg CBD | 2 capsules three times daily,(6 capsules per day) | Week 4–11(Day 29–84) | 800 mg # CBD | 2 capsules twice daily(4 capsules per day) | |||
| Total Population | THC:CBD Arm (n = 5) | CBD Arm (n = 5) | |
|---|---|---|---|
| Age (Years), median (±IQR) | 57.5 (54.75–61.75) | 57.0 (46.5–57.5) | 62 (47.0–65.0) |
| Sex assigned at birth (n (%)) | |||
| Male | 8 (80%) | 5 (100%) | 3 (60%) |
| Female | 2 (20%) | 0 (0%) | 2 (40%) |
| Ethnicity (n (%)) | |||
| White-North American | 6 (60%) | 3 (60%) | 3 (60%) |
| Black-African | 1 (10%) | 0 (0%) | 1 (20%) |
| Asian | 1 (10%) | 1 (20%) | 0 (0%) |
| Mixed ethnicity | 2 (20%) | 2 (40%) | 0 (0%) |
| Marital status (n (%)) | |||
| Single | 5 (50%) | 2 (40%) | 3 (60%) |
| Living as married | 3 (30%) | 2 (40%) | 1 (20%) |
| Married | 0 (0%) | 0 (0%) | 0 (0%) |
| Divorced | 2 (20%) | 2 (40%) | 0 (0%) |
| Widowed | 0 (0%) | 0 (0%) | 0 (0%) |
| Highest education level (n (%)) | |||
| Elementary (grade) school | 0 (0%) | 0 (0%) | 0 (0%) |
| Secondary (High) school diploma | 3 (30%) | 1 (20%) | 2 (40%) |
| College diploma | 2 (20%) | 1 (20%) | 1 (20%) |
| Apprenticeship or trades certificate or diploma | 1 (10%) | 1 (20%) | 0 (0%) |
| Bachelor’s degree | 2 (20%) | 1 (20%) | 1 (20%) |
| Professional degree (e.g., MD, PharmD) | 0 (0%) | 0 (0%) | 0 (0%) |
| Graduate degree (Master or Doctorate) | 2 (20%) | 2 (40%) | 0 (0%) |
| Cannabis use in the past 6 months (n (%)) | |||
| No | 3 (30%) | 2 (40%) | 1 (20%) |
| Yes | 7 (70%) | 3 (60%) | 4 (80%) |
| Monthly | 5 (72.43%) | 2 (40%) | 3 (60%) |
| Weekly | 2 (28.57%) | 1 (20%) | 1 (20%) |
| Daily | 0 (0%) | 0 (0%) | 0 (0%) |
| Alcohol use in the past 6 months (n (%)) | |||
| No | 5 (50%) | 2 (40%) | 3 (60%) |
| Yes | 5 (50%) | 3 (60%) | 2 (40%) |
| Drug use in the past 6 months (n (%)) | |||
| No | 3 (30%) | 2 (40%) | 1 (20%) |
| Yes | 7 (70%) | 3 (60%) | 4 (80%) |
| History of infectious diseases (n (%)) | |||
| Syphilis (treated) | 2 (20%) | 2 (40%) | 0 (0%) |
| Hepatitis B (Anti-Hepatitis B core antibodies) | 4 (40%) | 2 (40%) | 2 (40%) |
| Hepatitis C (Anti-Hepatitis C Antibodies) | 0 (0%) | 0 (0%) | 0 (0%) |
| Adverse Events | Total Population (n = 10) (n (%)) | THC:CBD Arm (n = 5) (n (%)) | CBD Arm (n = 5) (n (%)) |
|---|---|---|---|
| Somnolence | 5 (50%) | 2 (40%) | 3 (60) |
| Diarrhea | 2 (20%) | 1 (20%) | 1 (20%) |
| Difficulty concentrating | 2 (20%) | 1 (20%) | 1 (20%) |
| Transaminitis | 2 (20%) | 0 (0%) | 2 (40%) |
| Worsened diabetes type 2 | 2 (20%) | 1 (20%) | 1 (20%) |
| Abdominal cramps | 1 (10%) | 1 (20%) | 0 (0%) |
| Acute hepatitis * | 1 (10%) | 0 (0%) | 1 (20%) |
| Altered perception of peripheral neuropathy of feet bilaterally | 1 (10%) | 1 (20%) | 0 (0%) |
| Bilateral leg weakness | 1 (10%) | 0 (0%) | 1 (20%) |
| Cognitive impairment | 1 (10%) | 1 (20%) | 0 (0%) |
| Constipation | 1 (10%) | 0 (0%) | 1 (20%) |
| Dental abscess | 1 (10%) | 1 (20%) | 0 (0%) |
| Dizziness | 1 (10%) | 0 (0%) | 1 (20%) |
| Dry mouth | 1 (10%) | 1 (20%) | 0 (0%) |
| Fatigue | 1 (10%) | 1 (20%) | 0 (0%) |
| Gastroenteritis | 1 (10%) | 0 (0%) | 1 (20%) |
| Hypocalcemia | 1 (10%) | 0 (0%) | 1 (20%) |
| Increase appetite | 1 (10%) | 1 (20%) | 0 (0%) |
| Nausea | 1 (10%) | 1 (20%) | 0 (0%) |
| Nightmares | 1 (10%) | 1 (20%) | 0 (0%) |
| Palpitations | 1 (10%) | 0 (0%) | 1 (20%) |
| Paranoid thoughts | 1 (10%) | 1 (20%) | 0 (0%) |
| Right sided cramps | 1 (10%) | 0 (0%) | 1 (20%) |
| Upper tract respiratory infection | 1 (10%) | 0 (0%) | 1 (20%) |
| Worsened anemia | 1 (10%) | 0 (0%) | 1 (20%) |
| Worsened renal function | 1 (10%) | 0 (0%) | 1 (20%) |
| (Median (IQR)) | Screening Visit | Visit 3 | Visit 4 | Visit 5 | Visit 6 | Visit 7 | Visit 8 | Visit 9 | p-Value Friedman Test | p-Value Wilcoxon Matched-Pairs Signed Rank Test (Visit 3 vs. Visit 9) |
|---|---|---|---|---|---|---|---|---|---|---|
| Creatinine (mol/L) $ | 86.0 (70.5–100.0) | 87.0 (68.75–105.3) | 88.50 (66.50–103.5) | 89.00 (71.75–104.5) | 92.00 (69.75–104.5) | 90.0 (77.0–104.8) | 102.0 (76.5–109.5) | 80.0 (66.5–103.0) | 0.49 | 0.55 |
| Alanine Aminotransferase (ALT) (U/L) € | 19.5 (13.75–37.0) | 21.5 (11.5–36.75) | 19.5 (12.0–41.25) | 19.0 (13.25–34.0) | 21.0 (14.25–50.75) | 20.5 (9.5–31.25) | 20.5 (11.0–25.5) | 23.0 (14.0–35.5) | 0.31 | 0.87 |
| Aspartate Aminotransferase (AST) (U/L) | 19.0 (13.5–28.0) | 18.5 (15.75–26.5) | 20.5 (14.75–30.0) | 17.0 (14.5–23.5) | 19.5 (15.5–48.75) | 18.0 (12.0–22.75) | 18.0 (10.0–21.0) | 20.0 (15.0–28.5) | 0.76 | >0.99 |
| Alkaline Phosphatase (ALP) (U/L) | 68.0 (56.25–83.5) | 65.0 (55.5–73.25) | 61.0 (52.5–70.5) | 58.5 (53.25–78.5) | 63.5 (54.75–77.5) | 60.0 (51.5–72.5) | 60.0 (55.0–62.0) | 61.0 (54.0–73.5) | 0.0107 * | 0.29 |
| Urea (mmol/L) £ | 6.1 (4.4–7.43) | 5.9 (3.87–7.45) | 6.3 (4.55–6.83) | 6.25 (4.33–7.13) | 6.15 (4.95–7.85) | 5.95 (4.45–7.67) | 6.1 (4.5–8.63) | 6.0 (4.4–7.05) | 0.38 | 0.71 |
| Blood Glucose (mmol/L) | 5.2 (4.87–6.97) | 5.5 (4.57–7.3) | 5.3 (4.9–9.4) | 5.6 (4.93–9.77) | 5.7 (5.1–9.1) | 5.0 (4.6–6.13) | 5.2 (4.95–5.37) | 5.1 (5.0–6.15) | 0.38 | 0.46 |
| Total Bilirubin mol/L) | 10.15 (7.65–12.25) | 9.4 (7.87–11.33) | 10.0 (7.65–11.53) | 8.8 (6.8–15.05) | 9.0 (7.67–11.40) | 8.05 (7.1–9.57) | 9.3 (7.65–10.0) | 8.5 (7.05–12.20) | 0.98 | 0.64 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mboumba Bouassa, R.-S.; Needham, J.; Nohynek, D.; Singer, J.; Lee, T.; Bobeuf, F.; Samarani, S.; Del Balso, L.; Paisible, N.; Vertzagias, C.; et al. Safety and Tolerability of Oral Cannabinoids in People Living with HIV on Long-Term ART: A Randomized, Open-Label, Interventional Pilot Clinical Trial (CTNPT 028). Biomedicines 2022, 10, 3168. https://doi.org/10.3390/biomedicines10123168
Mboumba Bouassa R-S, Needham J, Nohynek D, Singer J, Lee T, Bobeuf F, Samarani S, Del Balso L, Paisible N, Vertzagias C, et al. Safety and Tolerability of Oral Cannabinoids in People Living with HIV on Long-Term ART: A Randomized, Open-Label, Interventional Pilot Clinical Trial (CTNPT 028). Biomedicines. 2022; 10(12):3168. https://doi.org/10.3390/biomedicines10123168
Chicago/Turabian StyleMboumba Bouassa, Ralph-Sydney, Judy Needham, Dana Nohynek, Joel Singer, Terry Lee, Florian Bobeuf, Suzanne Samarani, Lina Del Balso, Natalie Paisible, Claude Vertzagias, and et al. 2022. "Safety and Tolerability of Oral Cannabinoids in People Living with HIV on Long-Term ART: A Randomized, Open-Label, Interventional Pilot Clinical Trial (CTNPT 028)" Biomedicines 10, no. 12: 3168. https://doi.org/10.3390/biomedicines10123168
APA StyleMboumba Bouassa, R.-S., Needham, J., Nohynek, D., Singer, J., Lee, T., Bobeuf, F., Samarani, S., Del Balso, L., Paisible, N., Vertzagias, C., Sebastiani, G., Margolese, S., Mandarino, E., Klein, M., Lebouché, B., Cox, J., Brouillette, M.-J., Routy, J.-P., Szabo, J., ... Costiniuk, C. T. (2022). Safety and Tolerability of Oral Cannabinoids in People Living with HIV on Long-Term ART: A Randomized, Open-Label, Interventional Pilot Clinical Trial (CTNPT 028). Biomedicines, 10(12), 3168. https://doi.org/10.3390/biomedicines10123168







