Platelet Rich Plasma and Platelet-Related Products in the Treatment of Radiculopathy—A Systematic Review of the Literature
Abstract
1. Introduction
2. Methods
2.1. Literature Search Strategy
2.2. Study Selection
2.3. Data Extraction and Outcomes of Interest
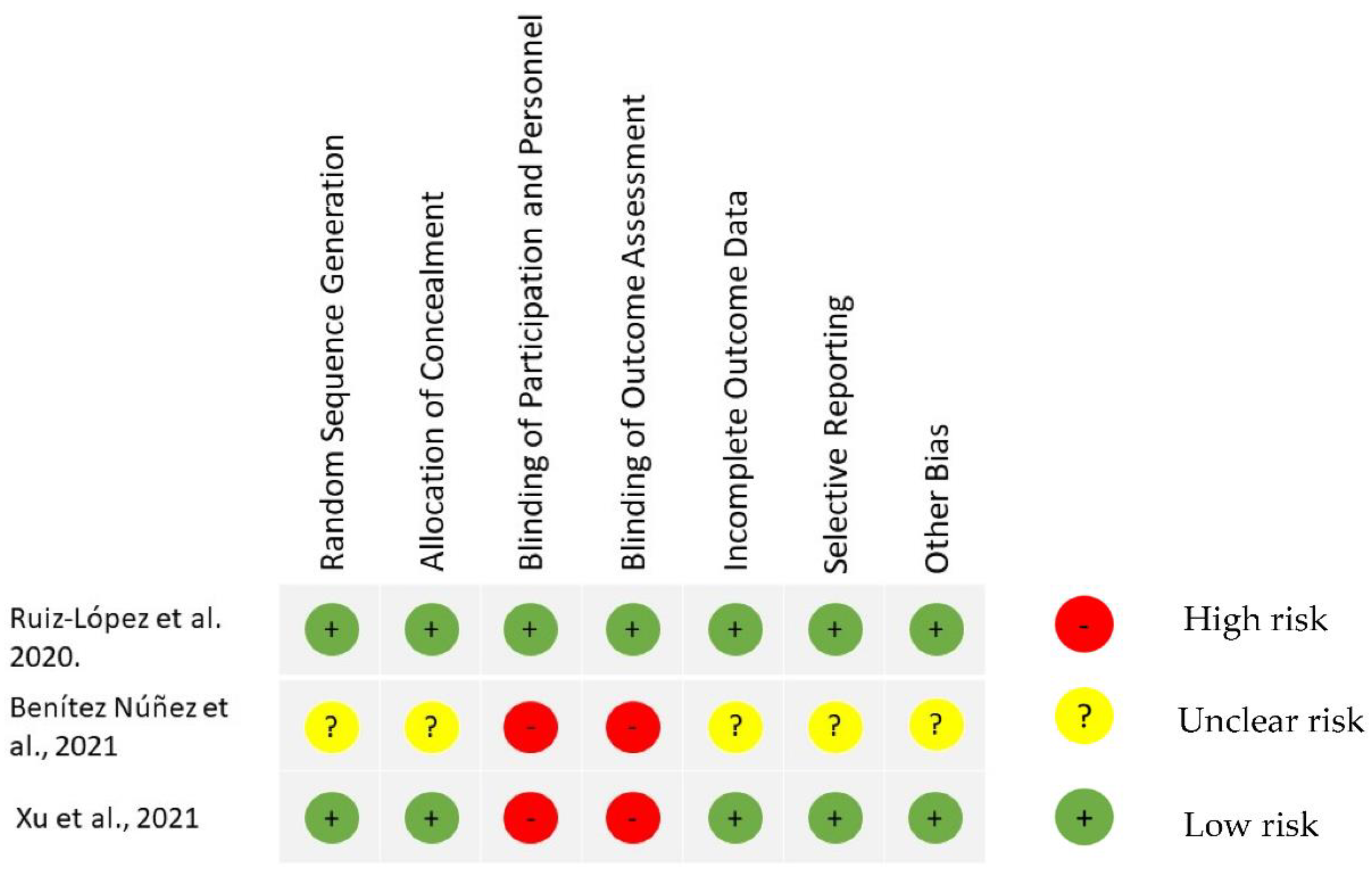
2.4. Assessment of Risk of Bias
2.5. Assessment of Quality of Evidence
3. Results
3.1. Characteristics of Included Studies
3.2. Product Characterization
3.3. Injection Procedure
3.4. Outcome Measure Tools
3.5. Primary Outcome—Change in Pain Intensity
3.6. Secondary Outcome: Functional Outcomes
3.7. Secondary Outcome: Anatomical Changes on Advanced Imaging
3.8. Secondary Outcome—Adverse Events
3.9. Risk of Bias Assessment
3.10. GRADE Quality of Evidence
4. Discussion
5. Limitations
6. Future Considerations
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Actual Search Strategy
- Database and date of the search: 2021-12-6 Cochrane Central
- Time period: Until–<November 2021>
- Search strategy:
| Query # | Query Details | Results |
|---|---|---|
| 1 | (radiculopath$ or radiculitis or radiculitides or (nerve root adj1 (disorder$ or inflammation$ or avulsion$ or compress$ or pain$)) or (radicular adj1 (pain$ or neuralgia))).ti,hw,ab. | 2307 |
| 2 | (platelet$ or thrombocyte$).ti,hw,ab. | 32,982 |
| 3 | ((epidural or extradural or peridural or transforaminal) adj (inject$ or infus$ or administ$)).ti,hw,ab. | 2154 |
| 4 | 1 and 2 and 3 | 2 |
- (radiculopath$ or radiculitis or radiculitides or (nerve root adj1 (disorder$ or inflammation$ or avulsion$ or compress$ or pain$)) or (radicular adj1 (pain$ or neuralgia))).ti,hw,ab.
- (platelet$ or thrombocyte$).ti,hw,ab.
- ((epidural or extradural or peridural or transforaminal) adj (inject$ or infus$ or administ$)).ti,hw,ab.
- and 2 and 3
- Database and date searched: 2021-126, Embase
- Time period: <1974 to 2021 December 03>
- Search strategy:
| Query # | Query Details | Results |
|---|---|---|
| 1 | radiculopathy/or radicular pain/or radiculitis/ | 15,481 |
| 2 | (radiculopath$ or radiculitis or radiculitides or (nerve root adj1 (disorder$ or inflammation$ or avulsion$ or compress$ or pain$)) or (radicular adj1 (pain$ or neuralgia))).ab,kf,ti. | 16,050 |
| 3 | 1 or 2 | 22,414 |
| 4 | thrombocyte rich plasma/or thrombocyte/ | 123,586 |
| 5 | (platelet$ or thrombocyte$).ab,kf,ti. | 340,078 |
| 6 | 4 or 5 | 356,491 |
| 7 | epidural space/ | 6338 |
| 8 | epidural drug administration/ | 8044 |
| 9 | ((epidural or extradural or peridural or transforaminal) adj (inject$ or infus$ or administ$)).ab,kf,ti. | 5742 |
| 10 | 7 or 8 or 9 | 17,248 |
| 11 | 3 and 6 and 10 | 18 |
| 12 | limit 11 to english language | 18 |
- Radiculopathy/or radicular pain/or radiculitis/
- (radiculopath$ or radiculitis or radiculitides or (nerve root adj1 (disorder$ or inflammation$ or avulsion$ or compress$ or pain$)) or (radicular adj1 (pain$ or neuralgia))).ab,kf,ti.
- or 2
- thrombocyte rich plasma/or thrombocyte/
- (platelet$ or thrombocyte$).ab,kf,ti.
- or 5
- epidural space/
- epidural drug administration/
- ((epidural or extradural or peridural or transforaminal) adj (inject$ or infus$ or administ$)).ab,kf,ti.
- or 8 or 9
- and 6 and 10
- limit 11 to english language
- Database and date searched: 2021-12-6 Scopus
- Search strategy:
- (INDEXTERMS(radiculopathy OR {radicular pain} OR radiculitis) OR TITLE-ABS-KEY (radiculopath* OR radiculitis OR radiculitides OR (“nerve root” W/1(disorder* OR inflammation* OR avulsion* OR compress* OR pain*)) OR (radicular W/1 (pain* OR neuralgia*)))) AND (INDEXTERMS ({blood platelets} OR {thrombocyte rich plasma} OR thrombocyte) OR TITLE-ABS-KEY (platelet* OR thrombocyte*)) AND (INDEXTERMS ({injections, epidural} OR {epidural drug administration}) OR TITLE-ABS-KEY ((epidural OR extradural OR peridural OR transforaminal) W/1 (inject* OR infus* OR administ*))) AND (LIMIT-TO (LANGUAGE, “English”))
- Database and date searched: 2021-12-6 Medline
- Time period: Ovid MEDLINE(R) 1946 to Present and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) Daily
- Search strategy:
| Query # | Query Details | Results |
|---|---|---|
| 1 | Radiculopathy/ | 5516 |
| 2 | (radiculopath$ or radiculitis or radiculitides or (nerve root adj1 (disorder$ or inflammation$ or avulsion$ or compress$)) or radicular-pain).ab,kf,ti. | 11,243 |
| 3 | 1 or 2 | 13,279 |
| 4 | Blood Platelets/ | 79,803 |
| 5 | (platelet$ or thrombocyte$).ab,kf,ti. | 237,487 |
| 6 | 4 or 5 | 248,821 |
| 7 | Injections, Epidural/ | 3091 |
| 8 | ((epidural or extradural or peridural or transforaminal) adj inject$).ab,kf,ti. | 2269 |
| 9 | 7 or 8 | 4394 |
| 10 | 3 and 6 and 9 | 10 |
- Radiculopathy/
- (radiculopath$ or radiculitis or radiculitides or (nerve root adj1 (disorder$ or inflammation$ or avulsion$ or compress$)) or radicular-pain).ab,kf,ti.
- or 2
- Blood Platelets/
- (platelet$ or thrombocyte$).ab,kf,ti.
- or 5
- Injections, Epidural/
- ((epidural or extradural or peridural or transforaminal) adj inject$).ab,kf,ti.
- or 8
- and 6 and 9
References
- Freburger, J.K.; Holmes, G.M.; Agans, R.P.; Jackman, A.M.; Darter, J.D.; Wallace, A.S.; Castel, L.D.; Kalsbeek, W.D.; Carey, T.S. The rising prevalence of chronic low back pain. Arch. Intern. Med. 2009, 169, 251–258. [Google Scholar] [CrossRef]
- Manchikanti, L.; Knezevic, N.N.; Boswell, M.V.; Kaye, A.D.; Hirsch, J.A. Epidural Injections for Lumbar Radiculopathy and Spinal Stenosis: A Comparative Systematic Review and Meta-Analysis. Pain Physician 2016, 19, E365–E410. [Google Scholar] [CrossRef]
- D’Souza, R.S.; Langford, B.; Wilson, R.E.; Her, Y.F.; Schappell, J.; Eller, J.S.; Evans, T.C.; Hagedorn, J.M. The state-of-the-art pharmacotherapeutic options for the treatment of chronic non-cancer pain. Expert Opin. Pharm. 2022, 23, 775–789. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, R.; Chopra, G. Efficacy of Platelet Rich Plasma via Lumbar Epidural Route in Chronic Prolapsed Intervertebral Disc Patients-A Pilot Study. J. Clin. Diagn. Res. JCDR 2016, 10, UC05–UC07. [Google Scholar] [CrossRef]
- Hagedorn, J.M.; Yadav, A.; D’Souza, R.S.; DeTemple, N.; Wolff, J.S.; Parmele, J.B.; Deer, T.R. The incidence of lumbar spine surgery following Minimally Invasive Lumbar Decompression and Superion Indirect Decompression System for treatment of lumbar spinal stenosis: A retrospective review. Pain Pract. 2022, 22, 516–521. [Google Scholar] [CrossRef]
- Centeno, C.; Markle, J.; Dodson, E.; Stemper, I.; Hyzy, M.; Williams, C.; Freeman, M. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J. Exp. Orthop. 2017, 4, 38. [Google Scholar] [CrossRef]
- Younes, M.; Neffati, F.; Touzi, M.; Hassen-Zrour, S.; Fendri, Y.; Béjia, I.; Ben Amor, A.; Bergaoui, N.; Najjar, M.F. Systemic effects of epidural and intra-articular glucocorticoid injections in diabetic and non-diabetic patients. Jt. Bone Spine 2007, 74, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Cohen, K.R. Management of Chronic Low Back Pain. JAMA Intern. Med. 2022, 182, 222–223. [Google Scholar] [CrossRef] [PubMed]
- Kubrova, E.; D’Souza, R.S.; Hunt, C.L.; Wang, Q.; Van Wijnen, A.J.; Qu, W. Injectable Biologics: What Is the Evidence? Am. J. Phys. Med. Rehabil. 2020, 99, 950–960. [Google Scholar] [CrossRef]
- Mautner, K.; Kneer, L. Treatment of Tendinopathies with Platelet-rich Plasma. Phys. Med. Rehabil. Clin. 2014, 25, 865–880. [Google Scholar] [CrossRef]
- Visser, L.C.; Arnoczky, S.P.; Caballero, O.; Kern, A.; Ratcliffe, A.; Gardner, K.L. Growth factor-rich plasma increases tendon cell proliferation and matrix synthesis on a synthetic scaffold: An in vitro study. Tissue Eng. Part A 2010, 16, 1021–1029. [Google Scholar] [CrossRef] [PubMed]
- Nishiyama, K.; Okudera, T.; Watanabe, T.; Isobe, K.; Suzuki, M.; Masuki, H.; Okudera, H.; Uematsu, K.; Nakata, K.; Kawase, T. Basic characteristics of plasma rich in growth factors (PRGF): Blood cell components and biological effects. Clin. Exp. Dent. Res. 2016, 2, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Doucet, C.; Ernou, I.; Zhang, Y.; Llense, J.R.; Begot, L.; Holy, X.; Lataillade, J.J. Platelet lysates promote mesenchymal stem cell expansion: A safety substitute for animal serum in cell-based therapy applications. J. Cell Physiol. 2005, 205, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, S.; Yu, J. Platelet-rich plasma injections: An emerging therapy for chronic discogenic low back pain. J. Spine Surg. 2018, 4, 115–122. [Google Scholar] [CrossRef]
- Sanapati, J.; Manchikanti, L.; Atluri, S.; Jordan, S.; Albers, S.L.; Pappolla, M.A.; Kaye, A.D.; Candido, K.D.; Pampati, V.; Hirsch, J.A. Do Regenerative Medicine Therapies Provide Long-Term Relief in Chronic Low Back Pain: A Systematic Review and Metaanalysis. Pain Physician 2018, 21, 515–540. [Google Scholar]
- Kubrova, E.; van Wijnen, A.J.; Qu, W. Spine Disorders and Regenerative Rehabilitation. Curr. Phys. Med. Rehabil. Rep. 2020, 8, 30–36. [Google Scholar] [CrossRef]
- Lemper, A.; Rhodes, S.; Boniface, K. Chronic Pain Management and Pregnancy a Platelet Rich Plasma Epidural Case Study. Lemper Research and Development. Available online: https://authorzilla.com/OlbN2/chronic-pain-management-and-pregnancy-a-platelet-rich-plasma.html (accessed on 1 December 2021).
- Rawson, B. Platelet-rich plasma and epidural platelet lysate: Novel treatment for lumbar disk herniation. J. Am. Osteopath. Assoc. 2020, 120, 201–207. [Google Scholar] [CrossRef]
- Kirchner, F.; Anitua, E. Intradiscal and intra-articular facet infiltrations with plasma rich in growth factors reduce pain in patients with chronic low back pain. J. Craniovertebr. Junction Spine 2016, 7, 250–256. [Google Scholar] [CrossRef]
- Jose, C.; Henry, C.; Patricia, A.; Edwin, G. Epidural plasma rich in growth factors for degenerative disc disease: A valuable alternative to conventional “palliative medicine”. Intern. Ational. J. Anesth. Clin. Med. 2019, 7, 1–6. [Google Scholar]
- Bise, S.; Dallaudiere, B.; Pesquer, L.; Pedram, M.; Meyer, P.; Antoun, M.B.; Hocquelet, A.; Silvestre, A. Comparison of interlaminar CT-guided epidural platelet-rich plasma versus steroid injection in patients with lumbar radicular pain. Eur. Radiol. 2020, 30, 3152–3160. [Google Scholar] [CrossRef]
- Xu, Z.; Wu, S.; Li, X.; Liu, C.; Fan, S.; Ma, C. Ultrasound-Guided Transforaminal Injections of Platelet-Rich Plasma Compared with Steroid in Lumbar Disc Herniation: A Prospective, Randomized, Controlled Study. Neural Plast. 2021, 2021, 5558138. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Lopez, R.; Tsai, Y.C. A Randomized Double-Blind Controlled Pilot Study Comparing Leucocyte-Rich Platelet-Rich Plasma and Corticosteroid in Caudal Epidural Injection for Complex Chronic Degenerative Spinal Pain. Pain Pract. 2020, 20, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Benitez, N. Efficacy of parasargital translaminar epidural application of growth factors derived from Platelet Rich Plasma as a treatment for unilateral root pain caused by multisegmental disc disease. Investig. Med. 2021, 13, 1. [Google Scholar]
- Kirchner, F.; Milani, I.; Martinez, A.; Kirchner-Bossi, N.; Prado, R.; Padilla, S.; Anitua, E. Plasma Rich in Growth Factors (PRGF) in the Treatment of Cervical and Lumbar Back Pain: A Retrospective Observational Clinical Study. Pain Physician 2021, 24, E649–E660. [Google Scholar]
- Machado, E.S.; Ambach, M.A.; Caldas, J.M.; Wei, J.J.; Bredemeier, M. Personalized multitarget biologic injection in the spine: Prospective case series of multitarget platelet-rich plasma for low back pain. Regen. Med. 2022, 17, 11–22. [Google Scholar] [CrossRef]
- González-Escalada, J.R.; Camba, A.; Muriel, C.; Rodríguez, M.; Contreras, D.; Barutell, C.D. Validación del índice de Lattinen para la evaluación del paciente con dolor crónico. Rev. Soc. Española Dolor 2012, 19, 181–188. [Google Scholar]
- Cohen, S.P.; Bicket, M.C.; Jamison, D.; Wilkinson, I.; Rathmell, J.P. Epidural Steroids: A Comprehensive, Evidence-Based Review. Reg. Anesth. Pain Med. 2013, 38, 175–200. [Google Scholar] [CrossRef]
- Mazzocca, A.D.; McCarthy, M.B.R.; Intravia, J.; Beitzel, K.; Apostolakos, J.; Cote, M.P.; Bradley, J.; Arciero, R.A. An In Vitro Evaluation of the Anti-Inflammatory Effects of Platelet-Rich Plasma, Ketorolac, and Methylprednisolone. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 675–683. [Google Scholar] [CrossRef]
- Stafford, M.A.; Peng, P.; Hill, D.A. Sciatica: A review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br. J. Anaesth. 2007, 99, 461–473. [Google Scholar] [CrossRef]
- Nadeau, S.; Filali, M.; Zhang, J.; Kerr, B.J.; Rivest, S.; Soulet, D.; Iwakura, Y.; de Rivero Vaccari, J.P.; Keane, R.W.; Lacroix, S. Functional recovery after peripheral nerve injury is dependent on the pro-inflammatory cytokines IL-1β and TNF: Implications for neuropathic pain. J. Neurosci. 2011, 31, 12533–12542. [Google Scholar] [CrossRef]
- Anjayani, S.; Wirohadidjojo, Y.W.; Adam, A.M.; Suwandi, D.; Seweng, A.; Amiruddin, M.D. Sensory improvement of leprosy peripheral neuropathy in patients treated with perineural injection of platelet-rich plasma. Int. J. Dermatol. 2014, 53, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, M.; Kamei, N.; Shinomiya, R.; Sunagawa, T.; Suzuki, O.; Kamoda, H.; Ohtori, S.; Ochi, M. Human platelet-rich plasma promotes axon growth in brain-spinal cord coculture. Neuroreport 2012, 23, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Bies, M.; Ashmore, Z.; Qu, W.; Hunt, C. Injectable Biologics for Neuropathic Pain: A Systematic Review. Pain Med. 2022, 23, 1733–1749. [Google Scholar] [CrossRef]
- Bansal, H.; Leon, J.; Pont, J.L.; Wilson, D.A.; Bansal, A.; Agarwal, D.; Preoteasa, I. Platelet-rich plasma (PRP) in osteoarthritis (OA) knee: Correct dose critical for long term clinical efficacy. Sci. Rep. 2021, 11, 3971. [Google Scholar] [CrossRef] [PubMed]
- Pochini, A.C.; Antonioli, E.; Bucci, D.Z.; Sardinha, L.R.; Andreoli, C.V.; Ferretti, M.; Ejnisman, B.; Goldberg, A.C.; Cohen, M. Analysis of cytokine profile and growth factors in platelet-rich plasma obtained by open systems and commercial columns. Einstein 2016, 14, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Benoist, M. The natural history of lumbar disc herniation and radiculopathy. Jt. Bone Spine 2002, 69, 155–160. [Google Scholar] [CrossRef]
- Macki, M.; Hernandez-Hermann, M.; Bydon, M.; Gokaslan, A.; McGovern, K.; Bydon, A. Spontaneous regression of sequestrated lumbar disc herniations: Literature review. Clin. Neurol. Neurosurg. 2014, 120, 136–141. [Google Scholar] [CrossRef]
- Magalon, J.; Chateau, A.L.; Bertrand, B.; Louis, M.L.; Silvestre, A.; Giraudo, L.; Veran, J.; Sabatier, F. DEPA classification: A proposal for standardising PRP use and a retrospective application of available devices. BMJ Open Sport Exerc. Med. 2016, 2, e000060. [Google Scholar] [CrossRef]
- Pourcho, A.M.; Smith, J.; Wisniewski, S.J.; Sellon, J.L. Intraarticular Platelet-Rich Plasma Injection in the Treatment of Knee Osteoarthritis: Review and Recommendations. Am. J. Phys. Med. Rehabil. 2014, 93, S108–S121. [Google Scholar] [CrossRef]
- Marx, R.E. Platelet-Rich Plasma (PRP): What Is PRP and What Is Not PRP? Implant. Dent. 2001, 10, 225–228. [Google Scholar] [CrossRef]
- Fadadu, P.P.; Mazzola, A.J.; Hunter, C.W.; Davis, T.T. Review of concentration yields in commercially available platelet-rich plasma (PRP) systems: A call for PRP standardization. Reg. Anesth. Pain Med. 2019, 44, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Murthy, N.S.; Geske, J.R.; Shelerud, R.A.; Wald, J.T.; Diehn, F.E.; Thielen, K.R.; Kaufmann, T.J.; Morris, J.M.; Lehman, V.T.; Amrami, K.K.; et al. The effectiveness of repeat lumbar transforaminal epidural steroid injections. Pain Med. 2014, 15, 1686–1694. [Google Scholar] [CrossRef] [PubMed]
- Komori, H.; Shinomiya, K.; Nakai, O.; Yamaura, I.; Takeda, S.; Furuya, K. The Natural History of Herniated Nucleus Pulposus With Radiculopathy. Spine 1996, 21, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Goodman, B.S.; Posecion, L.W.; Mallempati, S.; Bayazitoglu, M. Complications and pitfalls of lumbar interlaminar and transforaminal epidural injections. Curr. Rev. Musculoskelet Med. 2008, 1, 212–222. [Google Scholar] [CrossRef] [PubMed]
- McGrath, J.M.; Schaefer, M.P.; Malkamaki, D.M. Incidence and characteristics of complications from epidural steroid injections. Pain Med. 2011, 12, 726–731. [Google Scholar] [CrossRef] [PubMed]
- Diehn, F.E.; Murthy, N.S.; Maus, T.P. Science to Practice: What Causes Arterial Infarction in Transforaminal Epidural Steroid Injections, and Which Steroid Is Safest? Radiology 2016, 279, 657–659. [Google Scholar] [CrossRef] [PubMed]
- Da Fonseca, L.; Santos, G.S.; Huber, S.C.; Setti, T.M.; Setti, T.; Lana, J.F. Human platelet lysate—A potent (and overlooked) orthobiologic. J. Clin. Orthop. Trauma 2021, 21, 101534. [Google Scholar] [CrossRef] [PubMed]
- Wen, Y.-H.; Lee, C.-F.; Chen, Y.-J.; Chang, G.-J.; Chong, K.-Y. Risks in Induction of Platelet Aggregation and Enhanced Blood Clot Formation in Platelet Lysate Therapy: A Pilot Study. J. Clin. Med. 2022, 11, 3972. [Google Scholar] [CrossRef]

| Author, Year | Country | Study Design | Study Funding | N of Subjects | Product and Volume Injected, Site | Subject Age | Injection Guidance and Site | Follow-Up | Outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Lemper et al., 2012 [17] | USA | Case report | None reported | 1 | 9 mL of PRP with 18 mL of PPP into cervical epidural space; trigger point and lumbar epidural injection volume not specified | 35-year-old female, 10 W pregnant | Bilaterally C4-C6 epidural injections + in surrounding trigger points. Lumbar epidural injection 1 M later (level not specified). | 3 M | 1st injection: Cervical: pain improved by 50% next day and further at 1 W, reported better relief compared to prior ESIs 2nd injection: Lumbar: Pain completely resolved at 3 M. No AEs, delivered healthy child |
| Bhatia et al., 2016 [4] | India | Prospective uncontrolled study | None reported | 10 | 5 mL of PRP | All subjects < 65 Y | Fluoroscopy-guided interlaminar lumbar epidural injection | 3 M | Gradual improvement of VAS scores (avg 39.3% at 3 M), MODQ index (to <30%) and SLRT (<70) at 3 W and 3 M in all subjects. No AEs reported. |
| Kirchner et al., 2016 [19] | Spain | Prospective uncontrolled study | No funding. COI: Dr. Anitua is scientific director at BTI, who developed PRGF-Endoret technology | 86 | PRGF 4 mL into disc, 2 mL peri-durally, other into facet joint | 47 females (median 58) 39 males (median 55) | 4 mL intradiscal 0.5 mL intra-articular facet 2 mL transforaminal epidural lumbar injection of PRGF, fluoroscopic guidance | 6 M | At 6 M 90.7% of patients showed an excellent VAS score (0–3), 8.1% showed a moderate improvement (3.1–6.5), 1.2% no improvement (6.6–10). |
| Centeno et al., 2017 [6] | USA | Retrospective study | Funded by Regenexx, LLC and the Centeno-Schultz Clinic. | 470 | PL: Injection of 3–5 mL of PL (50% PL, 25% of 4% lidocaine, 25%100–200 ng/mL hydrocortisone) | Mean 53.6 (SD 13.5) | Fluoroscopy-guided transforaminal or interlaminar lumbar injection | 24 M | Subjects treated with PL reported significantly lower NPS (by AVG of 51% at 24 M) and FRI change scores at all time points 1 M–24 M (on AVG by 39.7%). FRI improvement met MCID at every time point except at 1 M. SANE improved in 72.7–77.1% subjects across time points. Total of 6.3% of subjects had mild AEs related to the procedure, no SAEs. |
| Correa et al., 2019 [20] | Colombia | Prospective uncontrolled study | Not reported | 250 | PRGF 10 mL in cervical or 12 mL in lumbar spine | Range 18–70 | Epidural cervical level 30% (C6-C7) or lumbar level 70% (L4-L5 or L5-S1) Repeat injections at 6–8 W. | 12 M | Mean VAS improved in 85% of patients (from AVG 8/10 to 2/10) at 12 M, MACNAB criteria improved from poor at baseline to excellent at 12 M. Opioid rescue use decreased from 96% at baseline to 0% at 12 M. 15% did not have improvement but no symptom worsening. No AEs reported. |
| Rawson et al., 2019 [18] | USA | Case report | No funding | 2 | 1 mL of PRP to posterior spinal ligament and facet joints per structure 3 mL of PL into epidural space | S1: 31 S2: 38 | Both subjects: PRP in posterior spinal ligaments and facet joints Subject 1: L4-5 interlaminar epidural injection of PL and S1 repeat injection Subject 2: L4-5 interlaminar epidural injection under fluoroscopic guidance x2 | 6 M | S1: Post-procedural pain for 3 D. At 4 W 50% pain relief. Repeat injection at S1 level at 4 W. Since 2nd injection complete symptoms resolution maintained at 6 M. MRI revealed incomplete resorption of disk herniation. S2: 1–2 D of postprocedure pain. 3 M after injection complete resolution of pain and function. No reported AEs. Repeated lumbar MRI showed almost complete resorption of disk material, with no evidence of ongoing neural impingement |
| Bise et al., 2020 [21] | France | Non-randomized comparative study | No funding | 60 (30 ESI, 30 PRP) | 2.5 mL of PRP | ESI—50 (SD 16) PRP 59 (SD 15) | CT-guided interlaminar lumbar epidural injections | 6 W | A statistically significant improvement found in both groups (decrease by 35%) at 6 W. ODI median decreased by 25%. No significant difference was observed in the decrease in NRS and ODI scores between the two groups at 6 W. No SAEs. |
| Xu et al., 2021 [22] | China | RCT | No funding | 124 (61 in PRP group, 63 in ESI group) | PRP: 3 mL of PRP Steroid: 3 mL steroid + anesthetic | PRP: 56 (44.5–60) Steroid: 56 (50–59) | Ultrasound-guided lumbar transforaminal epidural injection | 12 M | Statistically significant improvement in VAS, PPT, ODI and SF-36 at 1 M and maintained at 12 M. No significant intergroup differences in outcomes. No AEs reported. |
| Ruiz-Lopez et al., 2021 [23] | Spain, Taiwan | RCT, double blind | No funding | 50 (25 in triamcinolone group, 25 in PRP group) | LR-PRP: LR-PRP 16.5 mL + 3 mL contrast Steroid: 20 mL of triamcinolone (60 mg) + 3.5 mL contrast | LR-PRP group 68 (13.06) Steroid group 61 (12.6) | Fluoroscopy-guided caudal epidural injection S3-S4 level | 6 M | There was a significant reduction in the VAS score in both groups. VAS score was lower at 1 M in the ESI group, but scores were lower in the LR-PRP group at 3 M and 6 M. SF-36 at 6 M showed significant improvement in the LR-PRP group. No AEs reported. |
| Benítez Núñez et al., 2021 [24] | Cuba | RCT | No funding | 93 (46 in PRP group, 47 in ESI group) | 5 mL of autologous ozonized PRP or 5 mL mixture including bupivacaine and 40 mg of triamcinolone | 85% of subjects were between 18–45, 15% were older than 45 | Fluoroscopy-guided lumbar interlaminar epidural injection. Repeat injections after 1 W. | 12 M | There was a gradual improvement in the Lattinen Index score for the PRP group, maintained at 12 M. In the ESI group, there was rapid improvement in Lattinen Index score at 1 w-1 M with subsequent worsening at 3–12 M. No radiological improvement in either group. Mild AEs were 5× higher in the ESI group. |
| Kirchner et al., 2021 [25] | Spain | Retrospective Observational Study | No funding. COI: Dr. Anitua is scientific director at BTI, who developed PRGF-Endoret technology | 65 (18 with cervical and 47 with lumbar back pain) | Cervical epidural: 1.5 mL Lumbar epidural: 2 mL | Cervical pain: mean 54 Lumbar pain: mean 51 | Cervical injections: 1. Intraosseous (11% pts) 2. Intradiscal (100% pts, 2–4 discs) 3. Facet joint (44% pts) 4. Epidural (80% pts) Lumbar injections: 1. Intraosseous (9.4% pts) 2. Intradiscal (100% pts, 1–4 discs) 3. Facet joint (74%) 4. Epidural (83% pts) All pts received at least 2 injections (1 M apart) Fluoroscopy-guided | 1–24 M | Statistically significant Improvements in all 9 scores (without stratification) and 99% subjects had symptoms improvement after stratification. MCID was achieved in all subgroups for NRS (2 points decrease) and ODI. No SAEs. |
| Machado et al., 2021 [26] | Brazil | Prospective, Uncontrolled Study | No funding | 46 | 2 mL of PRP for foraminal injections, 5 mL for caudal epidural injection, (2 mL for each facet joint, 2 mL for each site of paravertebral muscles and 1 mL for intradiscal injection) | 55.1 (SD 15.2) | Injection sites determined by exam and imaging. Fluoroscopy-guided transforaminal or caudal epidural (76%) and intradiscal (22%) injection. Fluoroscopy and US for facet (98%) and IM (100%) injections. | 12 M | VAS improved at 2 W and RMDQ at 12 W and both were sustained at 52 W. Mean VAS decreased by 35% and RMDQ by 40% at 52 W. Pain medication use decreased at 52 W. Opioid medication use was significantly decreased and number of subjects taking them decreased from 35 to 12 after the procedure. No AEs observed. Total of 3 subjects underwent spine surgery in 1 Y. |
| Author | Year | Selection | Comparability | Exposure/Outcome |
|---|---|---|---|---|
| Bhatia et al. | 2016 | ** | - | ** |
| Correa et al. | 2019 | ** | - | * |
| Bise et al. | 2020 | *** | * | * |
| Centeno et al. | 2017 | ** | - | * |
| Machado et al. | 2022 | ** | - | ** |
| Kirchner et al. | 2016 | ** | - | ** |
| Kirchner et al. | 2021 | ** | - | ** |
| Certainty Assessment | № of Patients | Certainty | Importance | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| № of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | PRP or PL or PRGF/Total | Steroids/Total | ||
| Pain (Follow-up: Range 6 Weeks to 12 Months) | ||||||||||
| 12 | RCTs and non-randomized controlled trials | Serious a | Serious b,c | Serious b,c | Serious d | None | 1092/1257 (86.7%) | 165/1257 | ⨁◯◯◯ Very low | IMPORTANT |
| Functional scores | ||||||||||
| 12 | RCTs and non-randomized controlled trials | Serious a | Serious b,c | Serious b,c | Serious d | None | 1092/1257 (86.7%) | 165/1257 | ⨁◯◯◯ Very low | IMPORTANT |
| Safety | ||||||||||
| 12 | RCTs and non-randomized controlled trials | Serious a | Serious b,c | Serious b,c | Serious d | None | 1092/1257 (86.7%) | 165/1257 | ⨁◯◯◯ Very low | CRITICAL |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kubrova, E.; Martinez Alvarez, G.A.; Her, Y.F.; Pagan-Rosado, R.; Qu, W.; D’Souza, R.S. Platelet Rich Plasma and Platelet-Related Products in the Treatment of Radiculopathy—A Systematic Review of the Literature. Biomedicines 2022, 10, 2813. https://doi.org/10.3390/biomedicines10112813
Kubrova E, Martinez Alvarez GA, Her YF, Pagan-Rosado R, Qu W, D’Souza RS. Platelet Rich Plasma and Platelet-Related Products in the Treatment of Radiculopathy—A Systematic Review of the Literature. Biomedicines. 2022; 10(11):2813. https://doi.org/10.3390/biomedicines10112813
Chicago/Turabian StyleKubrova, Eva, Gabriel A. Martinez Alvarez, Yeng F. Her, Robert Pagan-Rosado, Wenchun Qu, and Ryan S. D’Souza. 2022. "Platelet Rich Plasma and Platelet-Related Products in the Treatment of Radiculopathy—A Systematic Review of the Literature" Biomedicines 10, no. 11: 2813. https://doi.org/10.3390/biomedicines10112813
APA StyleKubrova, E., Martinez Alvarez, G. A., Her, Y. F., Pagan-Rosado, R., Qu, W., & D’Souza, R. S. (2022). Platelet Rich Plasma and Platelet-Related Products in the Treatment of Radiculopathy—A Systematic Review of the Literature. Biomedicines, 10(11), 2813. https://doi.org/10.3390/biomedicines10112813








