Associations of Warfarin Use with Risks of Ischemic Cerebrovascular Events and Major Bleeding in Patients with Hyperthyroidism-Related Atrial Fibrillation
Abstract
1. Introduction
2. Materials and Methods
2.1. Source of Data
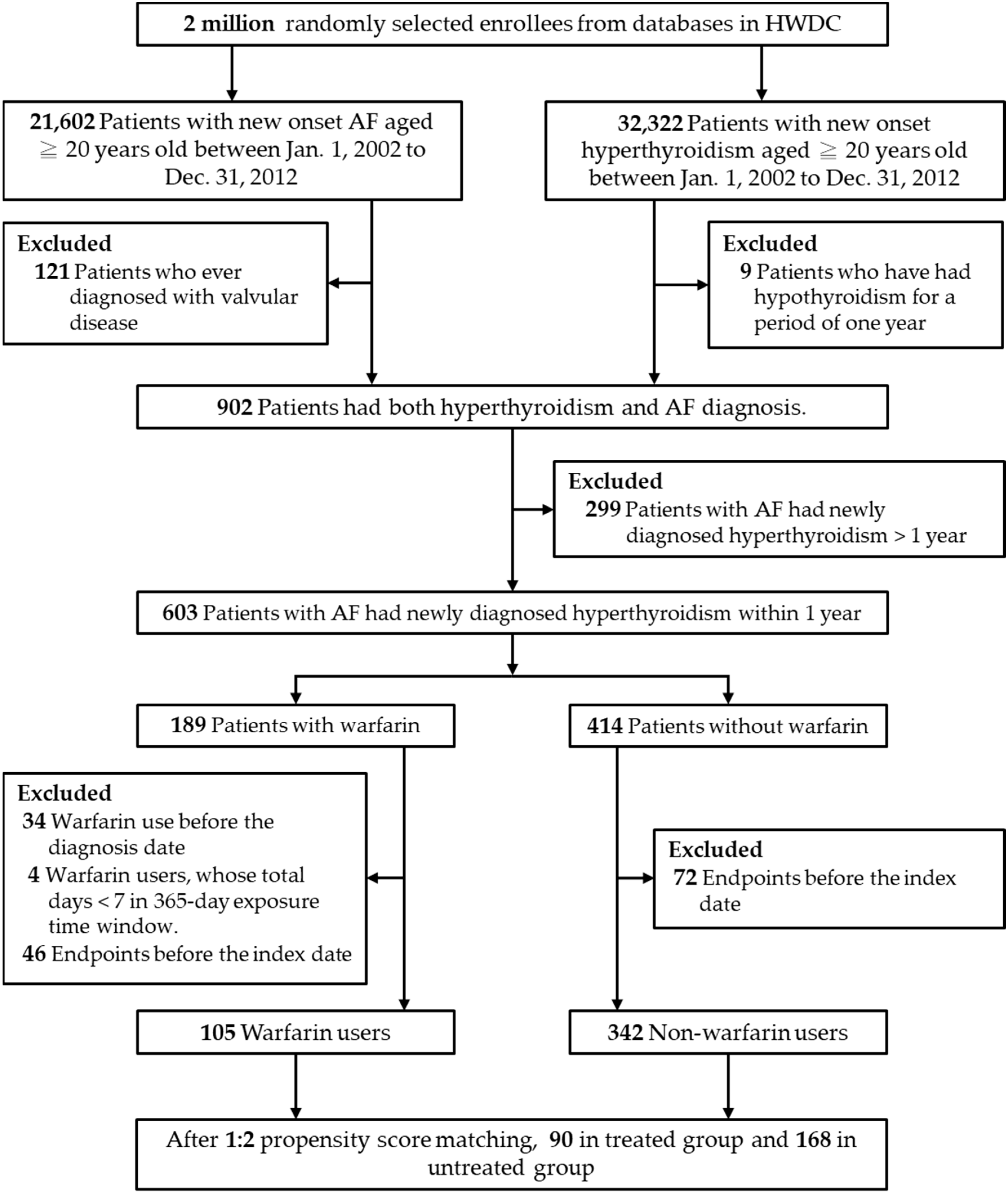
2.2. Study Population
2.3. Medication Exposure and Covariates
2.4. Outcomes
2.5. Patient and Public Involvement
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Risks of an Ischemic Stroke and Transient Ischemic Attack
3.3. Risk of Major Bleeding
3.4. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2021 Update: A Report From the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.-A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef]
- Klein, I.; Ojamaa, K. Thyroid Hormone and the Cardiovascular System. N. Engl. J. Med. 2001, 344, 501–509. [Google Scholar] [CrossRef]
- Frost, L.; Vestergaard, P.; Mosekilde, L. Hyperthyroidism and Risk of Atrial Fibrillation or Flutter: A population-based study. Arch. Intern. Med. 2004, 164, 1675–1678. [Google Scholar] [CrossRef]
- Baumgartner, C.; da Costa, B.R.; Collet, T.-H.; Feller, M.; Floriani, C.; Bauer, D.C.; Cappola, A.R.; Heckbert, S.R.; Ceresini, G.; Gussekloo, J.; et al. Thyroid Function Within the Normal Range, Subclinical Hypothyroidism, and the Risk of Atrial Fibrillation. Circulation 2017, 136, 2100–2116. [Google Scholar] [CrossRef]
- Guo, Y.; Tian, Y.; Wang, H.; Si, Q.; Wang, Y.; Lip, G.Y. Prevalence, Incidence, and Lifetime Risk of Atrial Fibrillation in China: New insights into the global burden of atrial fibrillation. Chest 2015, 147, 109–119. [Google Scholar] [CrossRef]
- Bielecka-Dabrowa, A.; Mikhailidis, D.P.; Rysz, J.; Banach, M. The mechanisms of atrial fibrillation in hyperthyroidism. Thyroid. Res. 2009, 2, 4. [Google Scholar] [CrossRef]
- Wustmann, K.; Kucera, J.P.; Zanchi, A.; Burow, A.; Stuber, T.; Chappuis, B.; Diem, P.; Delacrétaz, E. Activation of Electrical Triggers of Atrial Fibrillation in Hyperthyroidism. J. Clin. Endocrinol. Metab. 2008, 93, 2104–2108. [Google Scholar] [CrossRef]
- Chen, Y.-C.; Chen, S.-A.; Chen, Y.-J.; Chang, M.-S.; Chan, P.; Lin, C.-I. Effects of thyroid hormone on the arrhythmogenic activity of pulmonary vein cardiomyocytes. J. Am. Coll. Cardiol. 2002, 39, 366–372. [Google Scholar] [CrossRef]
- Li, Y.-G.; Pastori, D.; Farcomeni, A.; Yang, P.-S.; Jang, E.; Joung, B.; Wang, Y.-T.; Guo, Y.-T.; Lip, G.Y. A simple clinical risk score (c2hest) for predicting incident atrial fibrillation in asian subjects: Derivation in 471,446 Chinese Subjects, with internal validation and external application in 451,199 Korean subjects. Chest 2018, 155, 510–518. [Google Scholar] [CrossRef]
- Siu, C.-W.; Pong, V.; Zhang, X.; Chan, Y.-H.; Jim, M.-H.; Liu, S.; Yiu, K.-H.; Kung, A.W.; Lau, C.-P.; Tse, H.-F. Risk of ischemic stroke after new-onset atrial fibrillation in patients with hyperthyroidism. Heart Rhythm 2009, 6, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.-H.; Hai, J.; Yeung, C.-Y.; Lip, G.Y.; Lam, K.S.-L.; Tse, H.F.; Siu, C.-W. Benefit of Anticoagulation Therapy in Hyperthyroidism-Related Atrial Fibrillation. Clin. Cardiol. 2015, 38, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Friberg, L.; Rosenqvist, M.; Lip, G.Y. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182,678 patients with atrial fibrillation: The Swedish Atrial Fibrillation cohort study. Eur. Heart J. 2012, 33, 1500–1510. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.; Hansen, J.M. Stroke in thyrotoxicosis with atrial fibrillation. Stroke 1988, 19, 15–18. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.-H.; Wu, L.-S.; See, L.-C.; Liu, J.-R.; Chang, S.-H.; Chao, T.-F.; Yeh, Y.-H.; Kuo, C.-T.; Lee, H.-F.; Lip, G.Y.H. Direct Oral Anticoagulants in Atrial Fibrillation Patients With Concomitant Hyperthyroidism. J. Clin. Endocrinol. Metab. 2020, 105, 2893–2904. [Google Scholar] [CrossRef]
- Gorenek, B.; Boriani, G.; Dan, G.-A.; Fauchier, L.; Fenelon, G.; Huang, H.; Kudaiberdieva, G.; Lip, G.Y.H.; Mahajan, R.; Potpara, T.; et al. European Heart Rhythm Association (EHRA) position paper on arrhythmia management and device therapies in endocrine disorders, endorsed by Asia Pacific Heart Rhythm Society (APHRS) and Latin American Heart Rhythm Society (LAHRS). Eur. 2018, 20, 895–896. [Google Scholar] [CrossRef]
- Andrade, J.G.; Aguilar, M.; Atzema, C.; Bell, A.; Cairns, J.A.; Cheung, C.C.; Cox, J.L.; Dorian, P.; Gladstone, D.J.; Healey, J.S.; et al. The 2020 Canadian Cardiovascular Society/Canadian Heart Rhythm Society Comprehensive Guidelines for the Management of Atrial Fibrillation. Can. J. Cardiol. 2020, 36, 1847–1948. [Google Scholar] [CrossRef]
- Chao, T.-F.; Lip, G.Y.; Liu, C.-J.; Lin, Y.-J.; Chang, S.-L.; Lo, L.-W.; Hu, Y.-F.; Tuan, T.-C.; Liao, J.-N.; Chung, F.-P.; et al. Relationship of Aging and Incident Comorbidities to Stroke Risk in Patients With Atrial Fibrillation. J. Am. Coll. Cardiol. 2018, 71, 122–132. [Google Scholar] [CrossRef]
- Chan, W.S.H. Taiwan’s healthcare report 2010. EPMA J. 2010, 1, 563–585. [Google Scholar] [CrossRef]
- Chang, S.-H.; Chou, I.-J.; Yeh, Y.-H.; Chiou, M.-J.; Wen, M.-S.; Kuo, C.-T.; See, L.-C.; Kuo, C.-F. Association Between Use of Non–Vitamin K Oral Anticoagulants With and Without Concurrent Medications and Risk of Major Bleeding in Nonvalvular Atrial Fibrillation. JAMA 2017, 318, 1250–1259. [Google Scholar] [CrossRef]
- Tsai, C.-T.; Liao, J.-N.; Chiang, C.-E.; Lin, Y.-J.; Chang, S.-L.; Lo, L.-W.; Hu, Y.-F.; Tuan, T.-C.; Chung, F.-P.; Chao, T.-F.; et al. Association of Ischemic Stroke, Major Bleeding, and Other Adverse Events with Warfarin Use vs Non–vitamin K Antagonist Oral Anticoagulant Use in Patients with Atrial Fibrillation With a History of Intracranial Hemorrhage. JAMA Netw. Open 2020, 3, e206424. [Google Scholar] [CrossRef] [PubMed]
- Man, K.-M.; Chen, K.-B.; Chen, H.-Y.; Chiang, J.-H.; Su, Y.-C.; Man, S.S.; Xie, D.-D.; Wang, Y.; Zhang, Z.-Q.; Bi, L.-K.; et al. Hyperthyroidism is not a significant risk of benign prostatic hyperplasia: A nationwide population-based study. Medicine 2018, 97, e12459. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.-Y.; Chen, C.-H.; Li, C.-Y.; Lai, M.-L. Validating the diagnosis of acute ischemic stroke in a National Health Insurance claims database. J. Formos. Med. Assoc. 2015, 114, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Sung, S.-F.; Hsieh, C.-Y.; Lin, H.-J.; Chen, Y.-W.; Yang, Y.-H.K.; Li, C.-Y. Validation of algorithms to identify stroke risk factors in patients with acute ischemic stroke, transient ischemic attack, or intracerebral hemorrhage in an administrative claims database. Int. J. Cardiol. 2016, 215, 277–282. [Google Scholar] [CrossRef]
- Cheng, C.-L.; Kao, Y.-H.Y.; Lin, S.-J.; Lee, C.-H.; Lai, M.L. Validation of the national health insurance research database with ischemic stroke cases in Taiwan. Pharmacoepidemiol. Drug Saf. 2011, 20, 236–242. [Google Scholar] [CrossRef]
- Austin, P.C. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm. Stat. 2011, 10, 150–161. [Google Scholar] [CrossRef]
- Austin, P.C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 2009, 28, 3083–3107. [Google Scholar] [CrossRef]
- Lin, D.Y.; Wei, L.J. The Robust Inference for the Cox Proportional Hazards Model. J. Am. Stat. Assoc. 1989, 84, 1074–1078. [Google Scholar] [CrossRef]
- Nakazawa, H.; Lythall, D.; Noh, J.; Ishikawa, N.; Sugino, K.; Ito, K.; Hardman, S. Is there a place for the late cardioversion of atrial fibrillation?. A long-term follow-up study of patients with post-thyrotoxic atrial fibrillation. Eur. Heart J. 2000, 21, 327–333. [Google Scholar] [CrossRef]
- Lin, Y.-S.; Tsai, H.-Y.; Lin, C.-Y.; Wu, V.C.-C.; Chen, T.-H.; Yang, T.-Y.; Aboyans, V.; Chen, M.-C. Risk of Thromboembolism in Non-Valvular Atrial Fibrillation With or Without Clinical Hyperthyroidism. Glob. Heart 2021, 16, 45. [Google Scholar] [CrossRef]
- Chiang, C.-E.; Wu, T.-J.; Ueng, K.-C.; Chao, T.-F.; Chang, K.-C.; Wang, C.-C.; Lin, Y.-J.; Yin, W.-H.; Kuo, J.-Y.; Lin, W.-S.; et al. 2016 Guidelines of the Taiwan Heart Rhythm Society and the Taiwan Society of Cardiology for the management of atrial fibrillation. J. Formos. Med. Assoc. 2016, 115, 893–952. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Yang, P.-S.; Jang, E.; Yu, H.T.; Kim, T.-H.; Uhm, J.-S.; Kim, J.-Y.; Sung, J.-H.; Pak, H.-N.; Lee, M.-H.; et al. Increased risk of ischemic stroke and systemic embolism in hyperthyroidism-related atrial fibrillation: A nationwide cohort study. Am. Heart J. 2021, 242, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Bisson, A.; Fauchier, G.; Bodin, A.; Herbert, J.; Ducluzeau, P.H.; Lip, G.Y.H.; Fauchier, L. Yearly Incidence of Stroke and Bleeding in Atrial Fibrillation with Concomitant Hyperthyroidism: A National Discharge Database Study. J. Clin. Med. 2022, 11, 1342. [Google Scholar] [CrossRef] [PubMed]
- Bang, O.Y.; On, Y.K.; Lee, M.-Y.; Jang, S.-W.; Han, S.; Han, S.; Won, M.-M.; Park, Y.-J.; Lee, J.-M.; Choi, H.-Y.; et al. The risk of stroke/systemic embolism and major bleeding in Asian patients with non-valvular atrial fibrillation treated with non-vitamin K oral anticoagulants compared to warfarin: Results from a real-world data analysis. PLoS ONE 2020, 15, e0242922. [Google Scholar] [CrossRef] [PubMed]
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2019, 74, 104–132. [Google Scholar] [CrossRef]
- Hohnloser, S.H.; Pajitnev, D.; Pogue, J.; Healey, J.S.; Pfeffer, M.A.; Yusuf, S.; Connolly, S.J. Incidence of Stroke in Paroxysmal Versus Sustained Atrial Fibrillation in Patients Taking Oral Anticoagulation or Combined Antiplatelet Therapy: An ACTIVE W Substudy. J. Am. Coll. Cardiol. 2007, 50, 2156–2161. [Google Scholar] [CrossRef]
| Characteristic (n, %) | Before PSM | After PSM | ||||||
|---|---|---|---|---|---|---|---|---|
| Warfarin Users | Warfarin Nonusers | p Value | SMD | Warfarin Users | Warfarin Nonusers | p Value | SMD | |
| N = 105 | N = 342 | N = 90 | N = 168 | |||||
| Age, years (mean ± SD) | 60.1 ± 12.9 | 57.4 ± 14.5 | 0.088 | 0.197 | 59.9 ± 13.5 | 59.2 ± 14.6 | 0.699 | 0.051 |
| Aged ≥ 65 years | 40 (38.1) | 111 (32.5) | 0.285 | 0.118 | 36 (40.0) | 64 (38.1) | 0.765 | 0.039 |
| Gender: Male | 48 (45.7) | 124 (36.3) | 0.082 | 0.118 | 38 (42.2) | 75 (44.6) | 0.709 | 0.039 |
| CHA2DS2-VASc (mean ± SD) | 2.0 ± 1.6 | 1.7 ± 1.4 | 0.080 | 0.205 | 2.1 ± 1.6 | 1.8 ± 1.5 | 0.171 | 0.178 |
| Hypertension | 38 (36.2) | 93 (27.2) | 0.076 | 0.194 | 32 (35.6) | 43 (25.6) | 0.093 | 0.218 |
| Diabetes mellitus | 22 (21.0) | 44 (12.9) | 0.041 | 0.217 | 18 (20.0) | 27 (16.1) | 0.428 | 0.102 |
| Hyperlipidemia | 9 (8.6) | 36 (10.5) | 0.560 | −0.067 | 9 (10.0) | 20 (11.9) | 0.644 | −0.061 |
| Chronic kidney disease | 3 (2.9) | 17 (5.0) | 0.433 | −0.109 | 2 (2.2) | 4 (2.4) | 0.936 | −0.011 |
| Congestive heart failure | 38 (36.2) | 58 (17.0) | <0.0001 | 0.446 | 35 (38.9) | 44 (26.2) | 0.035 | 0.274 |
| Myocardial infarction | 0 | 10 (2.9) | 0.126 | −0.245 | 0 | 0 | NA | NA |
| Peripheral vascular disease | 4 (3.8) | 4 (1.2) | 0.092 | 0.170 | 3 (3.3) | 4 (2.4) | 0.698 | 0.057 |
| Chronic obstructive pulmonary disease | 14 (13.3) | 37 (10.8) | 0.478 | 0.077 | 13 (14.4) | 21 (12.5) | 0.660 | 0.057 |
| Rheumatic disease | 0 | 3 (0.9) | 1.000 | −0.133 | 0 | 2 (1.2) | 0.544 | −0.155 |
| Thromboembolism | 0 | 1 (0.3) | 1.000 | −0.077 | 0 | 0 | NA | NA |
| Cardiomyopathy | 4 (3.8) | 5 (1.5) | 0.224 | 0.147 | 4 (4.4) | 3 (1.8) | 0.243 | 0.154 |
| Any malignancy including leukemia | 0 | 5 (1.5) | 0.596 | −0.172 | 0 | 3 (1.8) | 0.554 | −0.191 |
| Cerebrovascular disease | 2 (1.9) | 4 (1.2) | 0.629 | 0.060 | 2 (2.2) | 3 (1.8) | 1.000 | 0.031 |
| Amiodarone | 20 (19.1) | 50 (14.6) | 0.275 | 0.119 | 19 (21.1) | 24 (14.3) | 0.161 | 0.180 |
| Aspirin | 38 (36.2) | 105 (30.7) | 0.292 | 0.117 | 35 (38.9) | 50 (29.8) | 0.137 | 0.193 |
| Clopidogrel | 3 (2.9) | 9 (2.6) | 1.000 | 0.014 | 3 (3.3) | 2 (1.2) | 0.346 | 0.145 |
| NSAIDs | 10 (9.5) | 34 (9.9) | 0.900 | −0.014 | 9 (10.0) | 18 (10.7) | 0.858 | −0.023 |
| Statins | 6 (5.7) | 16 (4.7) | 0.668 | 0.047 | 6 (6.7) | 9 (5.4) | 0.668 | 0.055 |
| After PSM | |||
|---|---|---|---|
| Warfarin Users | Warfarin Nonusers | p Value | |
| N = 90 | N = 168 | ||
| Stroke/TIA | |||
| Events (%) | 19 (21.1) | 21 (12.5) | 0.069 |
| Mean follow-up time (months, SD) | 79.8 (43.1) | 86.0 (41.1) | 0.254 |
| aHR (95% CI) a | 1.16 (0.52–2.56) | Reference | 0.717 |
| Major bleeding | |||
| Events (%) | 39 (43.3) | 64 (38.1) | 0.413 |
| Mean follow-up time (months, SD) | 65.0 (45.5) | 65.3 (43.7) | 0.958 |
| aHR (95% CI) b | 0.91 (0.56–1.47) | Reference | 0.702 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, S.-D.; Lin, S.-J.; Ray, C.-Y.; Lin, F.-T.; Lin, W.-C.; Wang, L.-H. Associations of Warfarin Use with Risks of Ischemic Cerebrovascular Events and Major Bleeding in Patients with Hyperthyroidism-Related Atrial Fibrillation. Biomedicines 2022, 10, 2670. https://doi.org/10.3390/biomedicines10112670
Liu S-D, Lin S-J, Ray C-Y, Lin F-T, Lin W-C, Wang L-H. Associations of Warfarin Use with Risks of Ischemic Cerebrovascular Events and Major Bleeding in Patients with Hyperthyroidism-Related Atrial Fibrillation. Biomedicines. 2022; 10(11):2670. https://doi.org/10.3390/biomedicines10112670
Chicago/Turabian StyleLiu, Sian-De, Shwu-Jiuan Lin, Chin-Ying Ray, Fang-Tsyr Lin, Weei-Chin Lin, and Li-Hsuan Wang. 2022. "Associations of Warfarin Use with Risks of Ischemic Cerebrovascular Events and Major Bleeding in Patients with Hyperthyroidism-Related Atrial Fibrillation" Biomedicines 10, no. 11: 2670. https://doi.org/10.3390/biomedicines10112670
APA StyleLiu, S.-D., Lin, S.-J., Ray, C.-Y., Lin, F.-T., Lin, W.-C., & Wang, L.-H. (2022). Associations of Warfarin Use with Risks of Ischemic Cerebrovascular Events and Major Bleeding in Patients with Hyperthyroidism-Related Atrial Fibrillation. Biomedicines, 10(11), 2670. https://doi.org/10.3390/biomedicines10112670






