“Flower Power”: Controlled Inhalation of THC-Predominant Cannabis Flos Improves Health-Related Quality of Life and Symptoms of Chronic Pain and Anxiety in Eligible UK Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Drugs
2.3. CBPM Administration Protocol
- Fill the Mighty Medic dosing capsules with grounded cannabis flos (Figure 1B). Although the maximum capacity per capsule is 250 mg, dosing is based in both the number and frequency of inhalations rather than the absolute amount of herbal material loaded into the device. This allows an experienced patient to have more control over administration and dosing while, at the same time, adjust and standardize the amount of cannabis flos used to optimize cost–benefit.
- Turn on the device and set the temperature to 180 °C (Figure 1A). At this temperature, vapor will be composed mainly of steam, most volatile terpenes (e.g., limonene, pinene), and small amounts of THC (boiling point 157 °C) which will start decarboxylating.
- Once the target temperature is reached, patients are instructed to inhale and exhale naturally. Vapor should not be held in the lungs longer than during regular breathing. The first inhalation is typically less effective since it serves to “prime” the device and warm up the herbal material.
- After inhaling the indicated number of times (see Figure 1C), patients are advised to wait for 15–20 min and observe for side effects (such as dizziness, tachycardia, nausea, disorientation, euphoria, etc.). After this period, and in absence of side effects, patients can repeat the cycle if symptomatic control has not been achieved, increasing the temperature by 10 °C (Figure 1C).
- At 190 °C and 200 °C the vapor may feel dryer and less fragrant but will be more concentrated in cannabinoids [30]. Vaporization of cannabinoids continues at high temperatures even if vapor is not visible when exhaling, due to the exhaustion of water in the herbal material.
- The goal for this 5-day initiation protocol is to provide the prescribing doctor with clear administration instructions to share with patients so that they can experiment with the device and familiarize themselves safely with cannabis inhalation.
2.4. Patient-Reported Outcome Measures (PROMS)
2.4.1. Health-Related Quality of Life
- The visual analog score (VAS) of general health (0–100) was interpreted as a patient-reported measure of general health.
- The sum of ratings for the five dimensions of the EuroQol (5–25) was interpreted as patient-reported measure of HRQoL.
2.4.2. Mood/Depression
2.4.3. Sleep Disturbances
2.4.4. Chronic Pain
2.4.5. Anxiety
2.5. Statistical Analysis
3. Results
3.1. Participants
3.2. General Health Outcome Measures
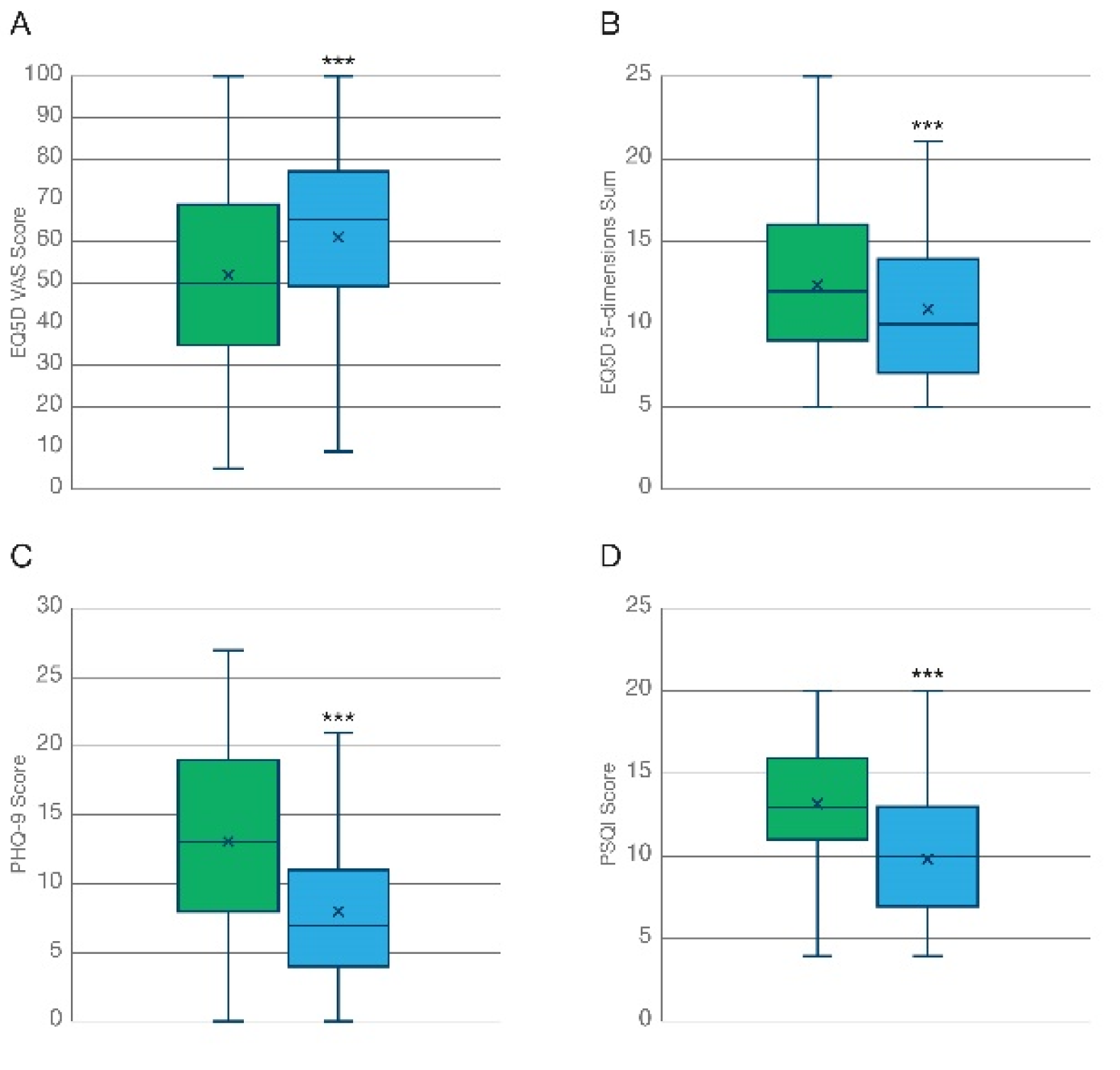
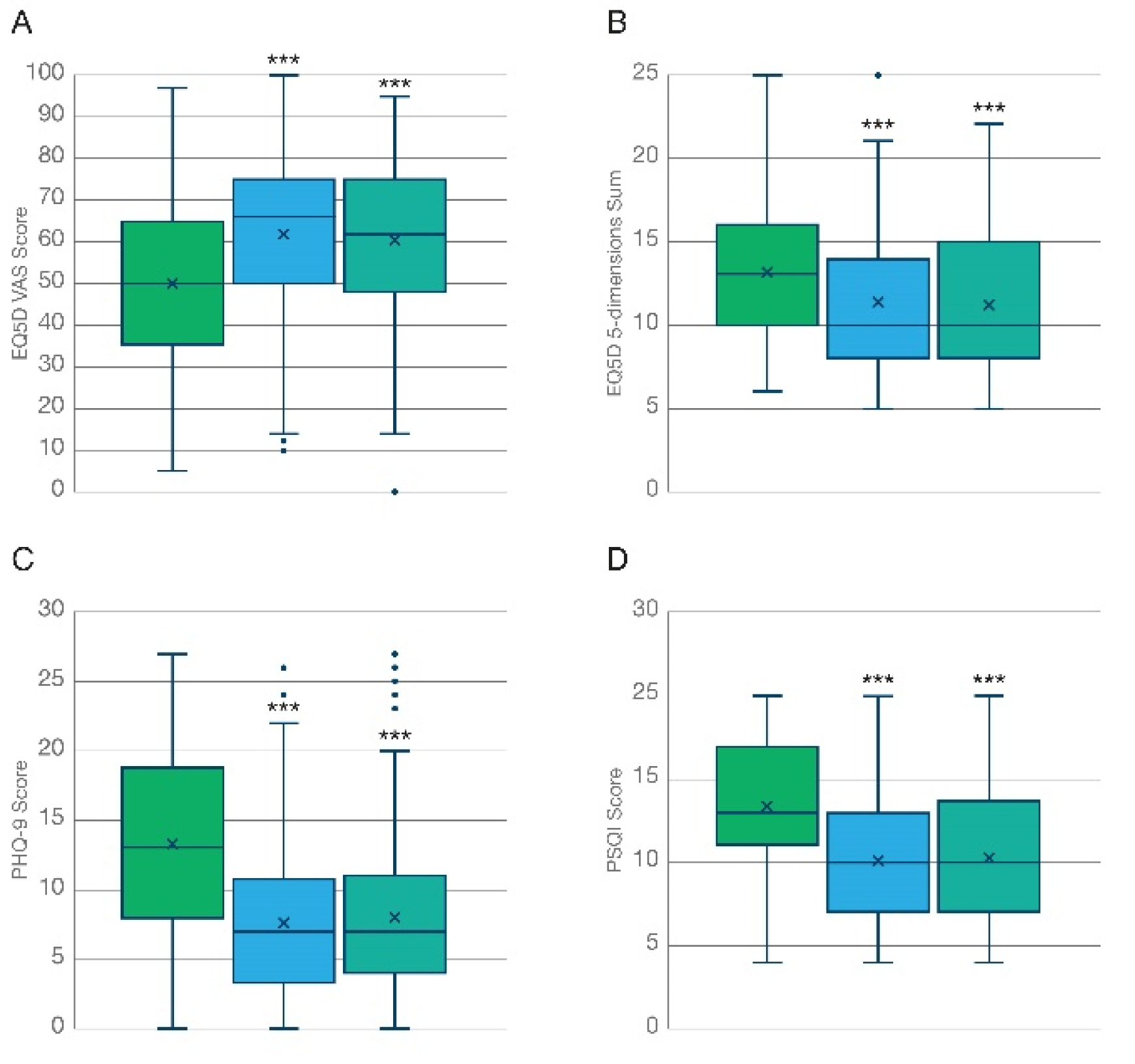
3.2.1. Health Related Quality of Life (HRQoL)
3.2.2. General Mood/Depression
3.2.3. Sleep Quality
3.3. Indication-Specific Outcome Measures
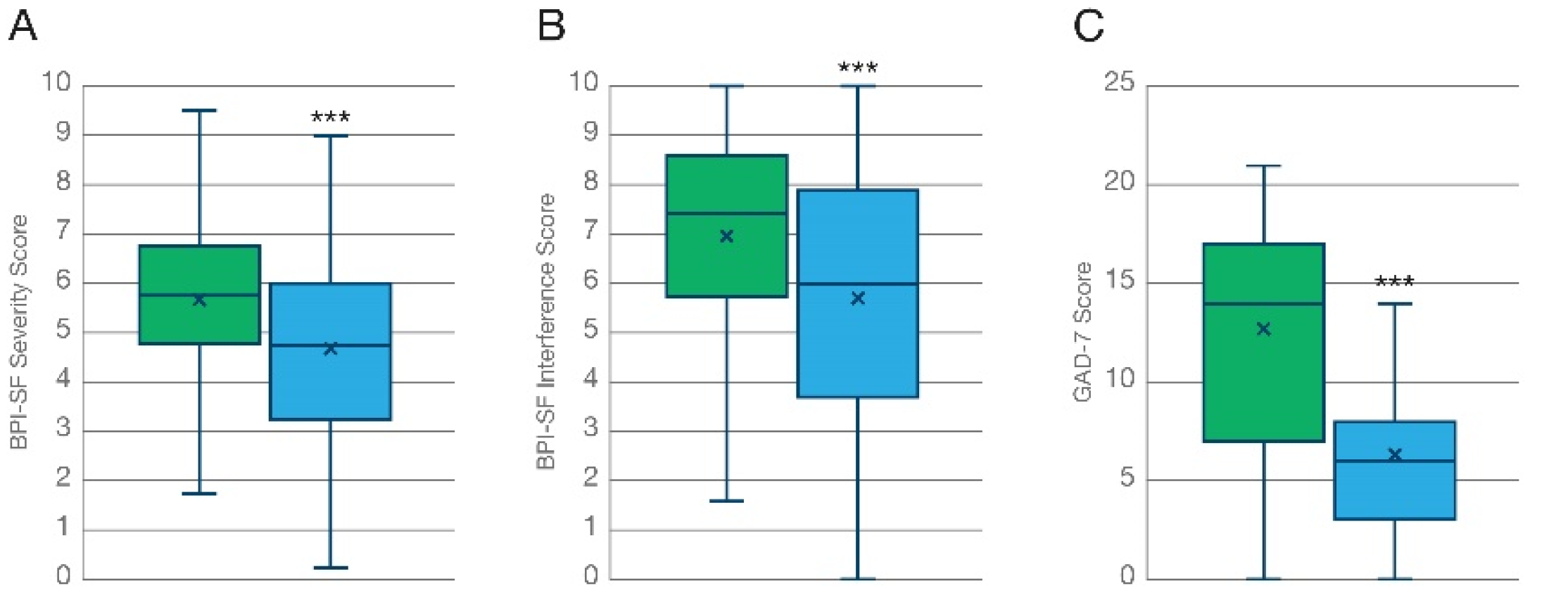
3.3.1. Pain Severity
3.3.2. Pain Interference
3.3.3. Generalized Anxiety Disorder
3.4. Adverse Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Shaughnessy, W.B. New remedy for tetanus and other convulsive disorders. Lancet 1840, 34, 539–541. [Google Scholar] [CrossRef]
- House of Lords—Science and Technology—Ninth Report. Available online: https://publications.parliament.uk/pa/ld199798/ldselect/ldsctech/151/15101.htm (accessed on 28 July 2022).
- Rescheduling of Cannabis-Based Products for Medicinal Use in Humans (Accessible Version)—GOV.UK. Available online: https://www.gov.uk/government/publications/circular-0182018-rescheduling-of-cannabis-based-products-for-medicinal-use-in-humans/rescheduling-of-cannabis-based-products-for-medicinal-use-in-humans-accessible-version (accessed on 28 July 2022).
- Köstenberger, M.; Nahler, G.; Jones, T.M.; Neuwersch, S.; Likar, R. The Role of Cannabis, Cannabidiol and Other Cannabinoids in Chronic Pain. The Perspective of Physicians. J. Neuroimmune Pharmacol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Coomber, R.; Oliver, M.; Morris, C. Using Cannabis Therapeutically in the UK: A Qualitative Analysis. J. Drug Issues 2016, 33, 325–356. [Google Scholar] [CrossRef]
- Abrams, D.I.; Vizoso, H.P.; Shade, S.B.; Jay, C.; Kelly, M.E.; Benowitz, N.L. Vaporization as a Smokeless Cannabis Delivery System: A Pilot Study. Clin. Pharmacol. Ther. 2007, 82, 572–578. [Google Scholar] [CrossRef] [PubMed]
- Fraguas-Sánchez, A.I.; Torres-Suárez, A.I. Medical Use of Cannabinoids. Drugs 2018, 78, 1665–1703. [Google Scholar] [CrossRef]
- Andreae, M.H.; Carter, G.M.; Shaparin, N.; Suslov, K.; Ellis, R.J.; Ware, M.A.; Abrams, D.I.; Prasad, H.; Wilsey, B.; Indyk, D.; et al. Inhaled Cannabis for Chronic Neuropathic Pain: A Meta-Analysis of Individual Patient Data. J. Pain 2015, 16, 1221–1232. [Google Scholar] [CrossRef] [PubMed]
- Wilsey, B.; Marcotte, T.D.; Deutsch, R.; Zhao, H.; Prasad, H.; Phan, A. An Exploratory Human Laboratory Experiment Evaluating Vaporized Cannabis in the Treatment of Neuropathic Pain From Spinal Cord Injury and Disease. J. Pain 2016, 17, 982–1000. [Google Scholar] [CrossRef] [PubMed]
- Wilsey, B.; Marcotte, T.; Deutsch, R.; Gouaux, B.; Sakai, S.; Donaghe, H. Low-Dose Vaporized Cannabis Significantly Improves Neuropathic Pain. J. Pain 2013, 14, 136–148. [Google Scholar] [CrossRef]
- Ellis, R.J.; Toperoff, W.; Vaida, F.; Van Den Brande, G.; Gonzales, J.; Gouaux, B.; Bentley, H.; Atkinson, J.H. Smoked Medicinal Cannabis for Neuropathic Pain in HIV: A Randomized, Crossover Clinical Trial. Neuropsychopharmacology 2009, 34, 672–680. [Google Scholar] [CrossRef] [PubMed]
- Ware, M.A.; Wang, T.; Shapiro, S.; Robinson, A.; Ducruet, T.; Huynh, T.; Gamsa, A.; Bennett, G.J.; Collet, J.P. Smoked Cannabis for Chronic Neuropathic Pain: A Randomized Controlled Trial. CMAJ 2010, 182, E694–E701. [Google Scholar] [CrossRef]
- Ware, M.A.; Wang, T.; Shapiro, S.; Collet, J.P. Cannabis for the Management of Pain: Assessment of Safety Study (COMPASS). J. Pain 2015, 16, 1233–1242. [Google Scholar] [CrossRef]
- Corey-Bloom, J.; Wolfson, T.; Gamst, A.; Jin, S.; Marcotte, T.D.; Bentley, H.; Gouaux, B. Smoked Cannabis for Spasticity in Multiple Sclerosis: A Randomized, Placebo-Controlled Trial. CMAJ 2012, 184, 1143–1150. [Google Scholar] [CrossRef]
- Almog, S.; Aharon-Peretz, J.; Vulfsons, S.; Ogintz, M.; Abalia, H.; Lupo, T.; Hayon, Y.; Eisenberg, E. The Pharmacokinetics, Efficacy, and Safety of a Novel Selective-Dose Cannabis Inhaler in Patients with Chronic Pain: A Randomized, Double-Blinded, Placebo-Controlled Trial. Eur. J. Pain 2020, 24, 1505–1516. [Google Scholar] [CrossRef]
- Carrubba, A.R.; Ebbert, J.O.; Spaulding, A.C.; DeStephano, D.; DeStephano, C.C. Use of Cannabis for Self-Management of Chronic Pelvic Pain. J. Women’s Health 2020, 30, 1344–1351. [Google Scholar] [CrossRef]
- Stith, S.S.; Diviant, J.P.; Brockelman, F.; Keeling, K.; Hall, B.; Lucern, S.; Vigil, J.M. Alleviative Effects of Cannabis Flower on Migraine and Headache. J. Integr. Med. 2020, 18, 416–424. [Google Scholar] [CrossRef]
- Van De Donk, T.; Niesters, M.; Kowal, M.A.; Olofsen, E.; Dahan, A.; Van Velzen, M. An Experimental Randomized Study on the Analgesic Effects of Pharmaceutical-Grade Cannabis in Chronic Pain Patients with Fibromyalgia. Pain 2019, 160, 860–869. [Google Scholar] [CrossRef]
- Cuttler, C.; Spradlin, A.; McLaughlin, R.J. A Naturalistic Examination of the Perceived Effects of Cannabis on Negative Affect. J. Affect. Disord. 2018, 235, 198–205. [Google Scholar] [CrossRef]
- Stith, S.S.; Li, X.; Diviant, J.P.; Brockelman, F.C.; Keeling, K.S.; Hall, B.; Vigil, J.M. The Effectiveness of Inhaled Cannabis Flower for the Treatment of Agitation/Irritability, Anxiety, and Common Stress. J. Cannabis Res. 2020, 2, 47. [Google Scholar] [CrossRef]
- Li, X.; Diviant, J.P.; Stith, S.S.; Brockelman, F.; Keeling, K.; Hall, B.; Vigil, J.M. The Effectiveness of Cannabis Flower for Immediate Relief from Symptoms of Depression. Yale J. Biol. Med. 2020, 93, 251–264. [Google Scholar]
- Kawka, M.; Erridge, S.; Holvey, C.; Coomber, R.; Usmani, A.; Sajad, M.; Platt, M.W.; Rucker, J.J.; Sodergren, M.H. Clinical Outcome Data of First Cohort of Chronic Pain Patients Treated with Cannabis-Based Sublingual Oils in the United Kingdom: Analysis From the UK Medical Cannabis Registry. J. Clin. Pharmacol. 2021, 61, 1545–1554. [Google Scholar] [CrossRef]
- Schlag, A.K.; Lynskey, M.; Fayaz, A.; Athanasiou-Fragkouli, A.; Brandner, B.; Haja, B.; Iveson, E.; Nutt, D.J. Characteristics of People Seeking Prescribed Cannabinoids for the Treatment of Chronic Pain: Evidence From Project Twenty 21. Front. Pain Res. 2022, 3, 85. [Google Scholar] [CrossRef]
- Schlag, A.K.; O’Sullivan, S.E.; Zafar, R.R.; Nutt, D.J. Current Controversies in Medical Cannabis: Recent Developments in Human Clinical Applications and Potential Therapeutics. Neuropharmacology 2021, 191, 108586. [Google Scholar] [CrossRef]
- Sakal, C.; Lynskey, M.; Schlag, A.K.; Nutt, D.J. Developing a Real-World Evidence Base for Prescribed Cannabis in the United Kingdom: Preliminary Findings from Project Twenty21. Psychopharmacology 2021, 239, 1147–1155. [Google Scholar] [CrossRef]
- Piomelli, D.; Russo, E.B. The Cannabis Sativa Versus Cannabis Indica Debate: An Interview with Ethan Russo, MD. Cannabis Cannabinoid Res. 2016, 1, 44–46. [Google Scholar] [CrossRef]
- Deutsches Arzneibuch 2018 (DAB). In Allgemeiner Teil. Monographien Cannabisblüten-Cannabis Flos; Deutscher Apotheker Verlag: Gerlingen, Germany, 2018.
- Lanz, C.; Mattsson, J.; Soydaner, U.; Brenneisen, R. Medicinal Cannabis: In Vitro Validation of Vaporizers for the Smoke-Free Inhalation of Cannabis. PLoS ONE 2016, 11, e0147286. [Google Scholar] [CrossRef]
- Carrara, L.; Giroud, C.; Concha-Lozano, N. Development of a Vaping Machine for the Sampling of THC and CBD Aerosols Generated by Two Portable Dry Herb Cannabis Vaporisers. Med. Cannabis Cannabinoids 2020, 3, 84–94. [Google Scholar] [CrossRef]
- Pomahacova, B.; Van Der Kooy, F.; Verpoorte, R. Cannabis Smoke Condensate III: The Cannabinoid Content of Vaporised Cannabis Sativa. Inhal. Toxicol. 2009, 21, 1108–1112. [Google Scholar] [CrossRef]
- Devlin, N.J.; Shah, K.K.; Feng, Y.; Mulhern, B.; van Hout, B. Valuing Health-Related Quality of Life: An EQ-5D-5L Value Set for England. Health Econ. 2018, 27, 7–22. [Google Scholar] [CrossRef]
- Rancans, E.; Trapencieris, M.; Ivanovs, R.; Vrublevska, J. Validity of the PHQ-9 and PHQ-2 to Screen for Depression in Nationwide Primary Care Population in Latvia. Ann. Gen. Psychiatry 2018, 17, 33. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Keller, S.; Bann, C.M.; Dodd, S.L.; Schein, J.; Mendoza, T.R.; Cleeland, C.S. Validity of the Brief Pain Inventory for Use in Documenting the Outcomes of Patients with Noncancer Pain. Clin. J. Pain 2004, 20, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Jordan, P.; Shedden-Mora, M.C.; Löwe, B. Psychometric Analysis of the Generalized Anxiety Disorder Scale (GAD-7) in Primary Care Using Modern Item Response Theory. PLoS ONE 2017, 12, e0182162. [Google Scholar] [CrossRef]
- Smith, M.T.; Haythornthwaite, J.A. How Do Sleep Disturbance and Chronic Pain Inter-Relate? Insights from the Longitudinal and Cognitive-Behavioral Clinical Trials Literature. Sleep Med. Rev. 2004, 8, 119–132. [Google Scholar] [CrossRef]
- Grotenhermen, F. Pharmacokinetics and Pharmacodynamics of Cannabinoids. Clin. Pharmacokinet. 2003, 42, 327–360. [Google Scholar] [CrossRef] [PubMed]
- Lavie-Ajayi, M.; Shvartzman, P. Restored Self: A Phenomenological Study of Pain Relief by Cannabis. Pain Med. 2019, 20, 2086–2093. [Google Scholar] [CrossRef]
- MacCallum, C.A.; Russo, E.B. Practical Considerations in Medical Cannabis Administration and Dosing. Eur. J. Intern. Med. 2018, 49, 12–19. [Google Scholar] [CrossRef]
- Wang, Y.; Jacques, J.; Li, Z.; Sibille, K.; Cook, R. Health Outcomes among Adults Initiating Medical Cannabis for Chronic Pain: A 3-Month Prospective Study Incorporating Ecological Momentary Assessment (EMA). Cannabis (Res. Soc. Marijuana) 2021, 4, 69–83. [Google Scholar] [CrossRef]
- Gruber, S.A.; Smith, R.T.; Dahlgren, M.K.; Lambros, A.M.; Sagar, K.A. No Pain, All Gain? Interim Analyses from a Longitudinal, Observational Study Examining the Impact of Medical Cannabis Treatment on Chronic Pain and Related Symptoms. Exp. Clin. Psychopharmacol. 2021, 29, 147–156. [Google Scholar] [CrossRef]
- Moreno-Sanz, G.; Madiedo, A.; Hernandez, P.; Kratz, J.; Aizpurua-Olaizola, O.; Brown, M.R.D.; López, J.R.; Patiño, J.; Mendivelso, F.O. Sex-Dependent Prescription Patterns and Clinical Outcomes Associated with the Use of Two Oral Cannabis Formulations in the Multimodal Management of Chronic Pain Patients in Colombia. Front. Pain Res. 2022, 3, 854795. [Google Scholar] [CrossRef]
- Wade, D.T.; Makela, P.; Robson, P.; House, H.; Bateman, C. Do Cannabis-Based Medicinal Extracts Have General or Specific Effects on Symptoms in Multiple Sclerosis? A Double-Blind, Randomized, Placebo-Controlled Study on 160 Patients. Mult. Scler. 2004, 10, 434–441. [Google Scholar] [CrossRef]
- Powell, D.; Pacula, R.L.; Jacobson, M. Do Medical Marijuana Laws Reduce Addictions and Deaths Related to Pain Killers? J. Health Econ. 2018, 58, 29–42. [Google Scholar] [CrossRef] [PubMed]
- Bachhuber, M.A.; Arnsten, J.H.; Cunningham, C.O.; Sohler, N. Does Medical Cannabis Use Increase or Decrease the Use of Opioid Analgesics and Other Prescription Drugs? J. Addict. Med. 2018, 12, 259–261. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Round, J.M.; Hanlon, J.G.; Hyshka, E.; Dyck, J.R.B.; Eurich, D.T. Generalized Anxiety Disorder 7-Item (GAD-7) Scores in Medically Authorized Cannabis Patients-Ontario and Alberta, Canada. Can. J. Psychiatry. 2022, 67, 470–480. [Google Scholar] [CrossRef] [PubMed]
- Walter, C.; Oertel, B.G.; Felden, L.; Kell, C.A.; Nöth, U.; Vermehren, J.; Kaiser, J.; Deichmann, R.; Lötsch, J. Brain Mapping-Based Model of Δ 9-Tetrahydrocannabinol Effects on Connectivity in the Pain Matrix. Neuropsychopharmacology 2016, 41, 1659–1669. [Google Scholar] [CrossRef] [PubMed]
- Weizman, L.; Dayan, L.; Brill, S.; Nahman-Averbuch, H.; Hendler, T.; Jacob, G.; Sharon, H. Cannabis Analgesia in Chronic Neuropathic Pain Is Associated with Altered Brain Connectivity. Neurology 2018, 91, E1285–E1294. [Google Scholar] [CrossRef]
- De Vita, M.J.; Moskal, D.; Maisto, S.A.; Ansell, E.B. Association of Cannabinoid Administration with Experimental Pain in Healthy Adults: A Systematic Review and Meta-Analysis. JAMA Psychiatry 2018, 75, 1118–1127. [Google Scholar] [CrossRef] [PubMed]
- Raymundi, A.M.; Da Silva, T.R.; Sohn, J.M.B.; Bertoglio, L.J.; Stern, C.A. Effects of ∆ 9-Tetrahydrocannabinol on Aversive Memories and Anxiety: A Review from Human Studies. BMC Psychiatry 2020, 20, 420. [Google Scholar] [CrossRef] [PubMed]
- Robinson, O.J.; Krimsky, M.; Lieberman, L.; Allen, P.; Vytal, K.; Grillon, C. The Dorsal Medial Prefrontal (Anterior Cingulate) Cortex—Amygdala Aversive Amplification Circuit in Unmedicated Generalised and Social Anxiety Disorders: An Observational Study. Lancet Psychiatry 2014, 1, 294–302. [Google Scholar] [CrossRef]
- Marsicano, G.; Wotjak, C.T.; Azad, S.C.; Bisogno, T.; Rammes, G.; Cascioll, M.G.; Hermann, H.; Tang, J.; Hofmann, C.; Zieglgänsberger, W.; et al. The Endogenous Cannabinoid System Controls Extinction of Aversive Memories. Nature 2002, 418, 530–534. [Google Scholar] [CrossRef] [PubMed]
- Phan, K.L.; Angstadt, M.; Golden, J.; Onyewuenyi, I.; Popovska, A.; De Wit, H. Cannabinoid Modulation of Amygdala Reactivity to Social Signals of Threat in Humans. J. Neurosci. 2008, 28, 2313–2319. [Google Scholar] [CrossRef]
- Jugl, S.; Sajdeya, R.; Morris, E.J.; Goodin, A.J.; Brown, J.D. Much Ado about Dosing: The Needs and Challenges of Defining a Standardized Cannabis Unit. Med. Cannabis Cannabinoids 2021, 4, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Itin, C.; Domb, A.J.; Hoffman, A. A Meta-Opinion: Cannabinoids Delivered to Oral Mucosa by a Spray for Systemic Absorption Are Rather Ingested into Gastro-Intestinal Tract: The Influences of Fed / Fasting States. Expert Opin. Drug Deliv. 2019, 16, 1031–1035. [Google Scholar] [CrossRef]
- Monte, A.A.; Shelton, S.K.; Mills, E.; Saben, J.; Hopkinson, A.; Sonn, B.; Devivo, M.; Chang, T.; Fox, J.; Brevik, C.; et al. Acute Illness Associated with Cannabis Use, by Route of Exposure: An Observational Study. Ann. Intern. Med. 2019, 170, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Blonde, L.; Khunti, K.; Harris, S.B.; Meizinger, C.; Skolnik, N.S. Interpretation and Impact of Real-World Clinical Data for the Practicing Clinician. Adv. Ther. 2018, 35, 1763–1774. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.D.; Goodin, A.J. Evidence in Context: High Risk of Bias in Medical Cannabis and Cannabinoid Clinical Trials Dictates the Need for Cautious Interpretation. Med. Cannabis Cannabinoids 2021, 4, 63–66. [Google Scholar] [CrossRef] [PubMed]

| Gender | Total | |||
|---|---|---|---|---|
| Male | Female | Non-Binary | ||
| Participants | ||||
| Sample: N (%) | 267 (77.6) | 76 (22.1) | 1 (0.3) | 344 (100) |
| Age: Mean ± SD | 38.3 ± 10.6 | 38.6 ± 9.89 | 42 ± 0.0 | 38.4 ± 10.4 |
| Previous Experience with Cannabis: N (%) | 259 (97.0) | 69 (90.8) | 1 (100) | 329 (95.6) |
| Intention of treating their primary condition with cannabis: N (%) | 205 (76.8) | 56 (73.7) | 1 (100) | 262 (76.1) |
| Frequency of cannabis use: N (%) | ||||
| Weekly | 2 (0.75) | 1 (1.32) | 0 | 3 (0.87) |
| A few times a week | 29 (10.9) | 12 (15.8) | 0 | 41 (11.9) |
| Once a day | 160 (59.9) | 41 (53.9) | 1 (100) | 202 (58.7) |
| Multiple times a day | 15 (5.62) | 3 (3.95) | 0 | 18 (5.23) |
| Did not answer the question | 61 (22.8) | 19 (25.0) | 0 | 80 (23.2) |
| Primary Condition: N (%) | ||||
| Chronic painful conditions | 134 (50.2) | 40 (52.6) | 1 (100) | 175 (50.8) |
| Anxiety-related disorders | 74 (27.7) | 13 (17.1) | 0 | 87 (25.3) |
| ADHD | 19 (7.12) | 5 (6.58) | 0 | 24 (6.98) |
| PTSD | 12 (4.49) | 9 (11.8) | 0 | 21 (6.10) |
| Other Mental Health | 14 (5.24) | 4 (5.26) | 0 | 18 (5.23) |
| Insomnia | 8 (3.00) | 2 (2.63) | 0 | 10 (2.91) |
| Autism Spectrum Disorder | 2 (0.75) | 0 | 0 | 2 (0.58) |
| Epilepsy | 0 | 1 (2.33) | 0 | 1 (0.52) |
| Other | 4 (1.50) | 1 (1.32) | 0 | 5 (1.45) |
| General Health EQ5D VAS Score | Health-Related QoL EQ5D 5-Dimensions SUM | Mood/Depression PHQ-9 Score | Quality of Sleep PSQI Score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean T = 0 | Mean T = 3 | Mean Diff | Mean T = 0 | Mean T = 3 | Mean Diff | Mean T = 0 | Mean T = 3 | Diff Mean | Mean T = 0 | Mean T = 3 | Mean Diff | |
| Anxiety (N = 107) | 57.10 | 69.55 | 12.4 | 10.07 | 8.31 | 1.76 | 13.72 | 6.58 | 7.14 | 12.31 | 9.16 | 3.15 |
| Chronic Pain (N = 174) | 47.35 | 54.33 | 6.98 * | 14.24 | 12.94 | 1.30 | 12.78 | 9.42 | 3.36 ** | 13.51 | 10.79 | 2.72 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno-Sanz, G.; Madiedo, A.; Lynskey, M.; Brown, M.R.D. “Flower Power”: Controlled Inhalation of THC-Predominant Cannabis Flos Improves Health-Related Quality of Life and Symptoms of Chronic Pain and Anxiety in Eligible UK Patients. Biomedicines 2022, 10, 2576. https://doi.org/10.3390/biomedicines10102576
Moreno-Sanz G, Madiedo A, Lynskey M, Brown MRD. “Flower Power”: Controlled Inhalation of THC-Predominant Cannabis Flos Improves Health-Related Quality of Life and Symptoms of Chronic Pain and Anxiety in Eligible UK Patients. Biomedicines. 2022; 10(10):2576. https://doi.org/10.3390/biomedicines10102576
Chicago/Turabian StyleMoreno-Sanz, Guillermo, Alvaro Madiedo, Michael Lynskey, and Matthew R. D. Brown. 2022. "“Flower Power”: Controlled Inhalation of THC-Predominant Cannabis Flos Improves Health-Related Quality of Life and Symptoms of Chronic Pain and Anxiety in Eligible UK Patients" Biomedicines 10, no. 10: 2576. https://doi.org/10.3390/biomedicines10102576
APA StyleMoreno-Sanz, G., Madiedo, A., Lynskey, M., & Brown, M. R. D. (2022). “Flower Power”: Controlled Inhalation of THC-Predominant Cannabis Flos Improves Health-Related Quality of Life and Symptoms of Chronic Pain and Anxiety in Eligible UK Patients. Biomedicines, 10(10), 2576. https://doi.org/10.3390/biomedicines10102576







