MicroRNAs Dysregulation as Potential Biomarkers for Early Diagnosis of Endometriosis
Abstract
1. Introduction
2. MicroRNAs as a New Diagnostic Biomarker for Endometriosis
| Author, Reference | Sample | miRNAs | Methods | Sensitivity and Specificity (%) | Stage of Disease |
|---|---|---|---|---|---|
| Wang et al., 2013 [57] | Serum | miR-199a ↑ miR-122 ↑ miR-9 ↓ miR-145 ↓ miR-141 ↓ miR-542-3p ↓ | Taqman miRNA array; validation qRT-PCR with Sybr Green | 78.33 and 76.00 80.00 and 76.00 68.33 and 96.00 70 and 96 71.69 and 96.00 79.66 and 92.00 | I/II/III/IV |
| Jia et al., 2013 [56] | Plasma | miR-17-5p ↓ miR-20a ↓ miR-22 ↓ | Agilent human microRNA microarray; validation qRT-PCR with Sybr Green | 70.0 and 70.0 60.0 and 90.0 90.0 and 80.0 | III/IV |
| Suryawanshi et al., 2013 [59] | Plasma | miR-16 ↑ miR-191 ↑ miR-195 ↑ | RT-qPCR profiling (human MiRNome profiler kit); validation qRT-PCR with Sybr Green | 88 and 60 | NA |
| Hsu et al., 2014 [60] | Serum | miR-199a-5p ↓ | Microarray; validation Taqman qRT-PCR | NA | NA |
| Cho et al., 2015 [43] | Serum | Let-7b ↓ miR-135a ↓ | qRT-PCR with Sybr Green | NA NA | III/IV |
| Rekker et al., 2015 [54] | Plasma | miR-200a ↓ miR-141 ↓ | Taqman qRT-PCR | 90.6 and 62.5 71.9 and 70.8 | I/II/III/IV |
| Cosar, et al., 2016 [61] | Serum | miR-125b-5p ↑ miR-451a ↑ miR-3613-5p ↓ | Affymetrix microRNA microarray and qRT-PCR with Sybr Green | 100 and 96 NA NA | III/IV |
| Wang et al., 2016 [62] | Serum | miR-185-5p ↑ miR-424-3p ↑miR-15b-5p ↓ miR-20a-5p ↓ miR-30c-5p ↓ miR-99b-5p ↓ miR-127-3p ↓ | Solexa sequencing and qRT-PCR with Sybr Green | NA | I/II |
| Pateisky et al., 2018 [63] | Plasma | hsa-miR-154-5p ↓ | qPCR-based arrays | 67 and 68 | I/II/III/IV |
| Bashti et al., 2018 [58] | Plasma | miR-31 ↓ miR-145 ↑ | qRT-PCR | - | I/II/III/IV |
| Nisenblat et al., 2019 [35] | Plasma | miR-139-3p ↓ miR-155 ↓ miR-574-3p ↓ | Multiplex RT-qPCR and singleplex Taqman RT-qPCR | 70 and 57 67 and 60 73 and 53 | I/II/III/IV |
| Vanhie et al., 2019 [41] | Plasma | hsa-miR-125b-5p hsa-miR-28-5p hsa-miR-29a-3p | Small RNA-seq and RT-qPCR with Sybr Green | 78 and 37 | I/II/III/IV |
| Moustafa et al., 2020 [53] | Serum | miR-125b ↑ miR-150 ↑ miR-342 ↑ miR-451 ↑ miR-3613 ↓ let-7b ↓ | qRT-PCR with Sybr Green | 56.1 and 78.0 20.0 and 94.7 90.0 and 91.2 90.0 and 72.9 92.7 and 61.0 82.5 and 67.8 | I/II/III/IV |
| Zhang et al., 2020 [64] | Serum exosomes | miR-22-3p ↑ miR-320a ↑ | Agilent human microRNA microarray and TaqMan qRT-PCR | NA | I/II/III/IV |
| Misir et al., 2021 [39] | Serum | miR-34a-5p ↓ miR-200c ↑ | qRT-PCR | 78.95 and 49.12 100 and 100 | I/II/III/IV |
| Bendifallah et al., 2022 [55] | Plasma | A signature composed of 86 miRNAs | Small RNA-seq | 96.8 and 100 | I/II/III/IV |
| Bendifallah et al., 2022 [48] | Saliva | A signature composed of 109 miRNAs | Small RNA-seq | 96.7 and 100 | I/II/III/IV |
3. The Role of miR-200 Family Members in Endometriosis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Giudice, L.C.; Kao, L.C. Endometriosis. Lancet 2004, 364, 1789–1799. [Google Scholar] [CrossRef]
- Nezhat, C.; Falik, R.; McKinney, S.; King, L.P. Pathophysiology and management of urinary tract endometriosis. Nat. Rev. Urol. 2017, 14, 359–372. [Google Scholar] [CrossRef] [PubMed]
- Florova, M.S.; Yarmolinskaya, M.I.; Potin, V.V. Prospects of metformin in the treatment of endometriosis. J. Obstet. Women’s Dis. 2017, 66, 67–76. [Google Scholar] [CrossRef][Green Version]
- Smolarz, B.; Szyłło, K.; Romanowicz, H. Endometriosis: Epidemiology, Classification, Pathogenesis, Treatment and Genetics (Review of Literature). Int. J. Mol. Sci. 2021, 22, 10554. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Li, C.; Ying, Y.; Lv, J.; Qu, X.; McGowan, E.; Lin, Y.; Zhu, X. Metformin Alleviates Endometriosis and Potentiates Endometrial Receptivity via Decreasing VEGF and MMP9 and Increasing Leukemia Inhibitor Factor and HOXA10. Front. Pharmacol. 2022, 13, 501. [Google Scholar] [CrossRef]
- Di Guardo, F.; Shah, M.; Cerana, M.C.; Biondi, A.; Karaman, E.; Török, P.; Yela, D.A.; Giampaolino, P.; Marín-Buck, A.; Laganà, A. Management of women affected by endometriosis: Are we stepping forward? J. Endometr. Pelvic Pain Disord. 2019, 11, 77–84. [Google Scholar] [CrossRef]
- Nicolaus, K.; Reckenbeil, L.; Bräuer, D.; Sczesny, R.; Diebolder, H.; Runnebaum, I.B. Cycle-related Diarrhea and Dysmenorrhea are Independent Predictors of Peritoneal Endometriosis, Cycle-related Dyschezia is an Independent Predictor of Rectal Involvement. Geburtshilfe und Frauenheilkd. 2020, 80, 307–315. [Google Scholar] [CrossRef]
- Alkatout, I.; Wedel, T.; Maass, N. Combined treatment of endometriosis: Radical yet gentle. Aktuelle Urol. 2018, 49, 60–72. [Google Scholar]
- Freytag, D.; Peters, G.; Mettler, L.; Gitas, G.; Maass, N.; Alkatout, I. Perioperative considerations in the treatment of endometriosis. J. Turk. Gynecol. Assoc. 2021, 22, 319–325. [Google Scholar] [CrossRef]
- Mettler, L.; Ruprai, R.; Alkatout, I. Impact of Medical and Surgical Treatment of Endometriosis on the Cure of Endometriosis and Pain. BioMed Res. Int. 2014, 2014, 264653. [Google Scholar] [CrossRef]
- Missmer, S.A.; Tu, F.F.; Agarwal, S.K.; Chapron, C.; Soliman, A.M.; Chiuve, S.; Eichner, S.; Flores-Caldera, I.; Horne, A.W.; Kimball, A.B.; et al. Impact of Endometriosis on Life-Course Potential: A Narrative Review. Int. J. Gen. Med. 2021, 14, 9–25. [Google Scholar] [CrossRef] [PubMed]
- Facchin, F.; Barbara, G.; Dridi, D.; Alberico, D.; Buggio, L.; Somigliana, E.; Saita, E.; Vercellini, P. Mental health in women with endometriosis: Searching for predictors of psychological distress. Hum. Reprod. 2017, 32, 1855–1861. [Google Scholar] [CrossRef] [PubMed]
- Matloobi, M.; Amini, L.; ShahAli, S.; Haghani, H.; Tahermanesh, K.; Hassanlouei, B.; Allahqoli, L.; Alkatout, I. Effect of sex education on sexual function and sexual quality of life in women with endometriosis: A quasi-experimental study. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2022. [Google Scholar] [CrossRef] [PubMed]
- Kimball, A.B.; Gieler, U.; Linder, D.; Sampogna, F.; Warren, R.B.; Augustin, M. Psoriasis: Is the impairment to a patient’s life cumulative? J. Eur. Acad. Dermatol. Venereol. JEADV 2010, 24, 989–1004. [Google Scholar] [CrossRef]
- Ballard, K.; Lowton, K.; Wright, J. What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertil. Steril. 2006, 86, 1296–1301. [Google Scholar] [CrossRef]
- Alkatout, I.; Meinhold-Heerlein, I.; Keckstein, J.; Mettler, L. Endometriosis: A concise practical guide to current diagnosis and treatment. J. Turk. Gynecol. Assoc. 2018, 19, 173–175. [Google Scholar] [CrossRef]
- D’Hooghe, T.; Mihalyi, A.; Simsa, P.; Kyama, C.; Peeraer, K.; De Loecker, P.; Meeuwis, L.; Segal, L.; Meuleman, C. Why We Need a Noninvasive Diagnostic Test for Minimal to Mild Endometriosis with a High Sensitivity. Gynecol. Obstet. Investig. 2006, 62, 136–138. [Google Scholar] [CrossRef]
- Leyland, N.; Casper, R.; Laberge, P.; Singh, S.S. Endometriosis: Diagnosis and management. J. Obstet. Gynaecol. Can. JOGC 2010, 32 (Suppl. 2), S1–S32. [Google Scholar] [CrossRef]
- Mabrouk, M.; Raimondo, D.; Parisotto, M.; Del Forno, S.; Arena, A.; Seracchioli, R. Pelvic floor dysfunction at transperineal ultrasound and voiding alteration in women with posterior deep endometriosis. Int. Urogynecology J. 2019, 30, 1527–1532. [Google Scholar] [CrossRef]
- Berker, B.; Seval, M. Problems with the Diagnosis of Endometriosis. Women’s Health 2015, 11, 597–601. [Google Scholar] [CrossRef]
- Horne, A.W.; Daniels, J.; Hummelshoj, L.; Cox, E.; Cooper, K.G. Surgical removal of superficial peritoneal endometriosis for managing women with chronic pelvic pain: Time for a rethink? BJOG Int. J. Obstet. Gynaecol. 2019, 126, 1414–1416. [Google Scholar] [CrossRef] [PubMed]
- Hudson, N. The missed disease? Endometriosis as an example of ‘undone science’. Reprod Biomed. Soc. Online 2022, 14, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Gratton, S.-M.; Choudhry, A.J.; Chen, I. Is laparoscopic visualization sufficient for the diagnosis of endometrisis? J. Obstet. Gynaecol. Can. 2019, 41, 718. [Google Scholar] [CrossRef]
- Mettler, L.; Schollmeyer, T.; Lehmann-Willenbrock, E.; Schüppler, U.; Schmutzler, A.; Shukla, D.; Zavala, A.; Lewin, A. Accuracy of laparoscopic diagnosis of endometriosis. JSLS J. Soc. Laparoendosc. Surg. 2003, 7, 15–18. [Google Scholar] [CrossRef][Green Version]
- Gratton, S.-M.; Choudhry, A.J.; Vilos, G.A.; Vilos, A.; Baier, K.; Holubeshen, S.; Medor, M.C.; Mercier, S.; Nguyen, V.; Chen, I. Diagnosis of Endometriosis at Laparoscopy: A Validation Study Comparing Surgeon Visualization with Histologic Findings. J. Obstet. Gynaecol. Can. 2022, 44, 135–141. [Google Scholar] [CrossRef]
- Walter, A.J.; Hentz, J.G.; Magtibay, P.M.; Cornella, J.L.; Magrina, J.F. Endometriosis: Correlation between histologic and visual findings at laparoscopy. Am. J. Obstet. Gynecol. 2001, 184, 1407–1413. [Google Scholar] [CrossRef]
- Darwish, A.M.; Hassanin, A.S.I. Epidemiology and risk factors associated with laparoscopically diagnosed typical and atypical endometriosis among Egyptian women. Middle East Fertil. Soc. J. 2006, 11, 196–201. [Google Scholar]
- Koninckx, P.R. Is mild endometriosis a condition occurring intermittently in all women? Hum. Reprod. 1994, 9, 2202–2205. [Google Scholar] [CrossRef]
- Szubert, M.; Suzin, J.; Wierzbowski, T.; Kowalczyk-Amico, K. CA-125 concentration in serum and peritoneal fluid in patients with endometriosis–preliminary results. Arch. Med. Sci. 2012, 8, 504–508. [Google Scholar] [CrossRef]
- Anastasi, E.; Manganaro, L.; Granato, T.; Benedetti Panici, P.; Frati, L.; Porpora, M.G. Is CA72-4 a useful biomarker in differential diagnosis between ovarian endometrioma and epithelial ovarian cancer? Dis. Markers 2013, 35, 331–335. [Google Scholar] [CrossRef]
- Abrão, M.S.; Podgaec, S.; Pinotti, J.A.; de Oliveira, R.M. Tumor markers in endometriosis. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 1999, 66, 19–22. [Google Scholar] [CrossRef]
- Rokhgireh, S.; Kashi, A.M.; Chaichian, S.; Delbandi, A.-A.; Allahqoli, L.; Ahmadi-Pishkuhi, M.; Khodaverdi, S.; Alkatout, I. The Diagnostic Accuracy of Combined Enolase/Cr, CA125, and CA19-9 in the Detection of Endometriosis. BioMed Res. Int. 2020, 2020, 5208279. [Google Scholar] [CrossRef] [PubMed]
- Telimaa, S.; Kauppila, A.; Rönnberg, L.; Suikkari, A.M.; Seppälä, M. Elevated serum levels of endometrial secretory protein PP14 in patients with advanced endometriosis. Suppression by treatment with danazol and high-dose medroxyprogesterone acetate. Am. J. Obstet. Gynecol. 1989, 161, 866–871. [Google Scholar] [CrossRef]
- Medl, M.; Ogris, E.; Peters-Engl, C.; Mierau, M.; Buxbaum, P.; Leodolter, S. Serum levels of the tumour-associated trypsin inhibitor in patients with endometriosis. BJOG Int. J. Obstet. Gynaecol. 1997, 104, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Nisenblat, V.; Sharkey, D.J.; Wang, Z.; Evans, S.F.; Healey, M.; Teague, E.M.C.O.; Print, C.G.; A Robertson, S.; Hull, M.L. Plasma miRNAs Display Limited Potential as Diagnostic Tools for Endometriosis. J. Clin. Endocrinol. Metab. 2019, 104, 1999–2022. [Google Scholar] [CrossRef] [PubMed]
- Liston, A.; Linterman, M.; Lu, L.-F. MicroRNA in the Adaptive Immune System, in Sickness and in Health. J. Clin. Immunol. 2010, 30, 339–346. [Google Scholar] [CrossRef]
- Monnaka, V.U.; Hernandes, C.; Heller, D.; Podgaec, S. Overview of miRNAs for the non-invasive diagnosis of endometriosis: Evidence, challenges and strategies. Syst. Rev. 2021, 19, eRW5704. [Google Scholar] [CrossRef]
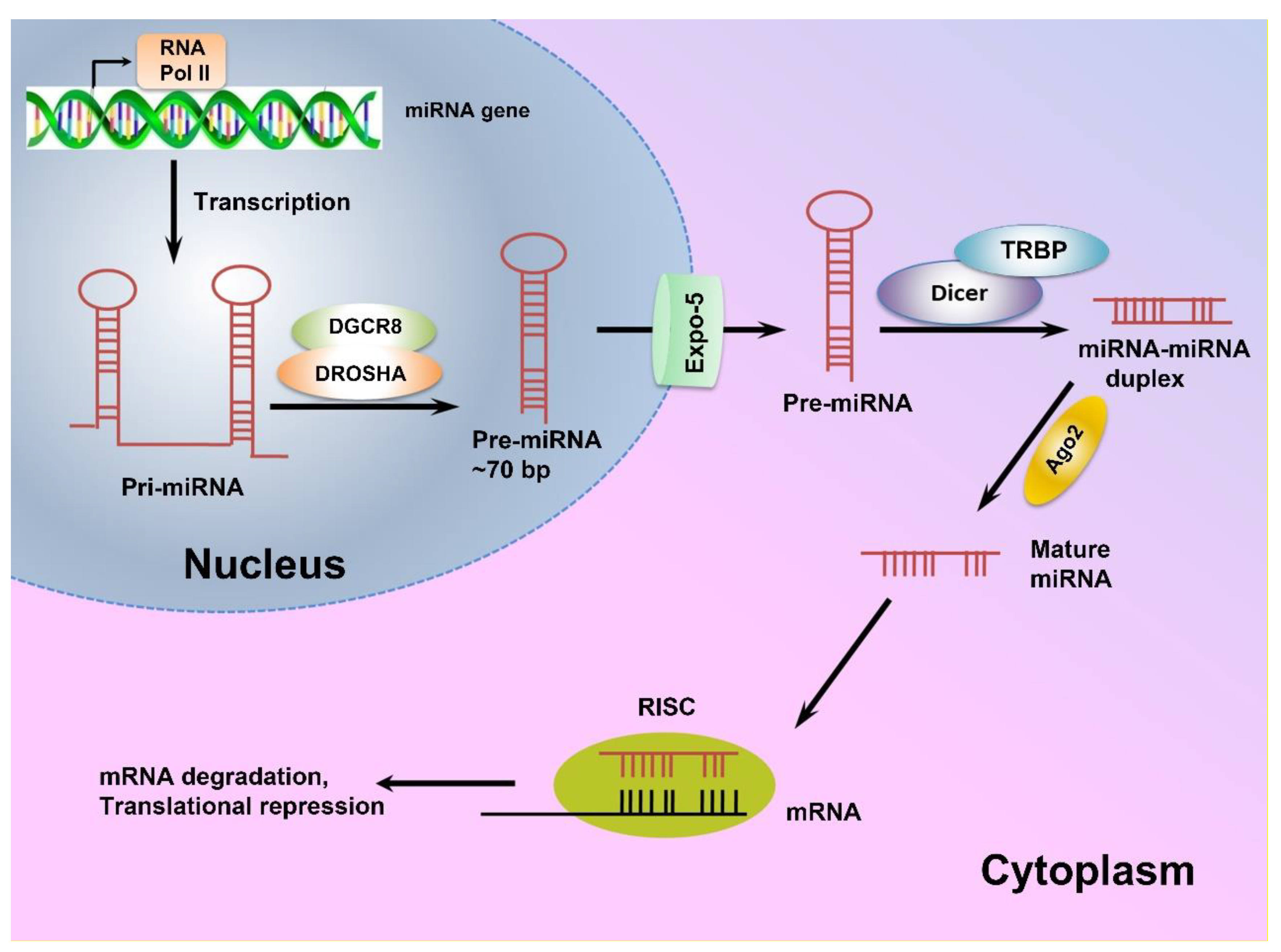
- Wahid, F.; Shehzad, A.; Khan, T.; Kim, Y.Y. MicroRNAs: Synthesis, mechanism, function, and recent clinical trials. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2010, 1803, 1231–1243. [Google Scholar] [CrossRef]
- Misir, S.; Hepokur, C.; Oksasoglu, B.; Yildiz, C.; Yanik, A.; Aliyazicioglu, Y. Circulating serum miR-200c and miR-34a-5p as diagnostic biomarkers for endometriosis. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 102092. [Google Scholar] [CrossRef]
- La Ferlita, A.; Battaglia, R.; Andronico, F.; Caruso, S.; Cianci, A.; Purrello, M.; Di Pietro, C. Non-coding RNAs in endometrial physiopathology. Int. J. Mol. Sci. 2018, 19, 2120. [Google Scholar] [CrossRef]
- Vanhie, A.O.D.; Peterse, D.; Beckers, A.; Cuéllar, A.; Fassbender, A.; Meuleman, C.; Mestdagh, P.; D’Hooghe, T. Plasma miRNAs as biomarkers for endometriosis. Hum. Reprod. 2019, 34, 1650–1660. [Google Scholar] [CrossRef] [PubMed]
- Shu, J.; E Silva, B.V.R.; Gao, T.; Xu, Z.; Cui, J. Dynamic and Modularized MicroRNA Regulation and Its Implication in Human Cancers. Sci. Rep. 2017, 7, 13356. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Mutlu, L.; Grechukhina, O.; Taylor, H.S. Circulating microRNAs as potential biomarkers for endometriosis. Fertil. Steril. 2015, 103, 1252–1260.e1. [Google Scholar] [CrossRef]
- Agrawal, S.; Tapmeier, T.T.; Rahmioglu, N.; Kirtley, S.; Zondervan, K.T.; Becker, C.M. The miRNA Mirage: How Close Are We to Finding a Non-Invasive Diagnostic Biomarker in Endometriosis? A Systematic Review. Int. J. Mol. Sci. 2018, 19, 599. [Google Scholar] [CrossRef] [PubMed]
- Ohlsson Teague, E.M.C.; Print, C.G.; Hull, M.L. The role of microRNAs in endometriosis and associated reproductive conditions. Hum. Reprod. Update 2010, 16, 142–165. [Google Scholar] [CrossRef]
- O’Carroll, D.; Schaefer, A. General Principals of miRNA Biogenesis and Regulation in the Brain. Neuropsychopharmacology 2013, 38, 39–54. [Google Scholar] [CrossRef]
- Korpal, M.; Lee, E.S.; Hu, G.; Kang, Y. The miR-200 Family Inhibits Epithelial-Mesenchymal Transition and Cancer Cell Migration by Direct Targeting of E-cadherin Transcriptional Repressors ZEB1 and ZEB2. J. Biol. Chem. 2008, 283, 14910–14914. [Google Scholar] [CrossRef]
- Bendifallah, S.; Suisse, S.; Puchar, A.; Delbos, L.; Poilblanc, M.; Descamps, P.; Golfier, F.; Jornea, L.; Bouteiller, D.; Touboul, C.; et al. Salivary MicroRNA Signature for Diagnosis of Endometriosis. J. Clin. Med. 2022, 11, 612. [Google Scholar] [CrossRef]
- Humphries, B.; Yang, C. The microRNA-200 family: Small molecules with novel roles in cancer development, progression and therapy. Oncotarget 2015, 6, 6472–6498. [Google Scholar] [CrossRef]
- Boils, A.B.; Marí-Alexandre, J.; Gilabert, J.; Sánchez-Izquierdo, D.; España, F.; Estellés, A.; Gilabert-Estellés, J. MicroRNA expression profile in endometriosis: Its relation to angiogenesis and fibrinolytic factors. Hum. Reprod. 2014, 29, 978–988. [Google Scholar] [CrossRef]
- Ohlsson Teague, E.M.C.; Van der Hoek, K.H.; Van der Hoek, M.B.; Perry, N.; Wagaarachchi, P.; Robertson, S.A.; Print, C.G.; Hull, L.M. MicroRNA-regulated pathways associated with endometriosis. Mol. Endocrinol. 2009, 23, 265–275. [Google Scholar] [CrossRef]
- Gao, S.; Liu, S.; Gao, Z.-M.; Deng, P.; Wang, D.-B. Reduced microRNA-451 expression in eutopic endometrium contributes to the pathogenesis of endometriosis. World J. Clin. Cases 2019, 7, 2155–2164. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, S.; Burn, M.; Mamillapalli, R.; Nematian, S.; Flores, V.; Taylor, H.S. Accurate diagnosis of endometriosis using serum microRNAs. Am. J. Obstet. Gynecol. 2020, 223, 557.e1–557.e11. [Google Scholar] [CrossRef] [PubMed]
- Rekker, K.; Saare, M.; Roost, A.M.; Kaart, T.; Sõritsa, D.; Karro, H.; Sõritsa, A.; Simón, C.; Salumets, A.; Peters, M. Circulating miR-200–family micro-RNAs have altered plasma levels in patients with endometriosis and vary with blood collection time. Fertil. Steril. 2015, 104, 938–946.e2. [Google Scholar] [CrossRef]
- Bendifallah, S.; Dabi, Y.; Suisse, S.; Jornea, L.; Bouteiller, D.; Touboul, C.; Puchar, A.; Daraï, E. MicroRNome analysis generates a blood-based signature for endometriosis. Sci. Rep. 2022, 12, 4051. [Google Scholar] [CrossRef] [PubMed]
- Jia, S.Z.; Yang, Y.; Lang, J.; Sun, P.; Leng, J. Plasma miR-17-5p, miR-20a and miR-22 are down-regulated in women with endometriosis. Hum. Reprod. 2013, 28, 322–330. [Google Scholar] [CrossRef]
- Wang, W.-T.; Zhao, Y.-N.; Han, B.-W.; Hong, S.-J.; Chen, Y.-Q. Circulating MicroRNAs Identified in a Genome-Wide Serum MicroRNA Expression Analysis as Noninvasive Biomarkers for Endometriosis. J. Clin. Endocrinol. Metab. 2013, 98, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Bashti, O.; Noruzinia, M.; Garshasbi, M.; Abtahi, M. miR-31 and miR-145 as potential non-invasive regulatory biomarkers in patients with endometriosis. Cell J. 2018, 20, 84. [Google Scholar] [PubMed]
- Suryawanshi, S.; Vlad, A.M.; Lin, H.-M.; Mantia-Smaldone, G.; Laskey, R.; Lee, M.; Lin, Y.; Donnellan, N.; Klein-Patel, M.; Lee, T.; et al. Plasma MicroRNAs as Novel Biomarkers for Endometriosis and Endometriosis-Associated Ovarian Cancer. Clin. Cancer Res. 2013, 19, 1213–1224. [Google Scholar] [CrossRef]
- Hsu, C.-Y.; Hsieh, T.-H.; Tsai, C.-F.; Tsai, H.-P.; Chen, H.-S.; Chang, Y.; Chuang, H.-Y.; Lee, J.-N.; Hsu, Y.-L.; Tsai, E.-M. miRNA-199a-5p regulates VEGFA in endometrial mesenchymal stem cells and contributes to the pathogenesis of endometriosis. J. Pathol. 2013, 232, 330–343. [Google Scholar] [CrossRef]
- Cosar, E.; Mamillapalli, R.; Ersoy, G.S.; Cho, S.; Seifer, B.; Taylor, H.S. Serum microRNAs as diagnostic markers of endometriosis: A comprehensive array-based analysis. Fertil. Steril. 2016, 106, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Huang, W.; Ren, C.; Zhao, M.; Jiang, X.; Fang, X.; Xia, X. Analysis of Serum microRNA Profile by Solexa Sequencing in Women with Endometriosis. Reprod. Sci. 2016, 23, 1359–1370. [Google Scholar] [CrossRef] [PubMed]
- Pateisky, P.; Pils, D.; Szabo, L.; Kuessel, L.; Husslein, H.; Schmitz, A.; Wenzl, R.; Yotova, I. hsa-miRNA-154-5p expression in plasma of endometriosis patients is a potential diagnostic marker for the disease. Reprod. Biomed. Online 2018, 37, 449–466. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Li, H.; Yuan, M.; Li, D.; Sun, C.; Wang, G. Serum Exosomal MicroRNAs as Potential Circulating Biomarkers for Endometriosis. Dis. Markers 2020, 2020, 2456340. [Google Scholar] [CrossRef] [PubMed]
- Cavallari, I.; Ciccarese, F.; Sharova, E.; Urso, L.; Raimondi, V.; Silic-Benussi, M.; D’Agostino, D.M.; Ciminale, V. The miR-200 Family of microRNAs: Fine Tuners of Epithelial-Mesenchymal Transition and Circulating Cancer Biomarkers. Cancers 2021, 13, 5874. [Google Scholar] [CrossRef]
- Kong, D.; Li, Y.; Wang, Z.; Banerjee, S.; Ahmad, A.; Kim, H.R.C.; Sarkar, F.H. miR-200 regulates PDGF-D-mediated epithelial–mesenchymal transition, adhesion, and invasion of prostate cancer cells. Stem Cells 2009, 27, 1712–1721. [Google Scholar] [CrossRef]
- Bilyk, O.; Coatham, M.; Jewer, M.; Postovit, L.-M. Epithelial-to-Mesenchymal Transition in the Female Reproductive Tract: From Normal Functioning to Disease Pathology. Front. Oncol. 2017, 7, 145. [Google Scholar] [CrossRef]
- Konrad, L.; Dietze, R.; Riaz, M.A.; Scheiner-Bobis, G.; Behnke, J.; Horné, F.; Hoerscher, A.; Reising, C.; Meinhold-Heerlein, I. Epithelial–mesenchymal transition in endometriosis—When does it happen? J. Clin. Med. 2020, 9, 1915. [Google Scholar] [CrossRef]
- Peinado, H.; Olmeda, D.; Cano, A. Snail, Zeb and bHLH factors in tumour progression: An alliance against the epithelial phenotype? Nat. Rev. Cancer 2007, 7, 415–428. [Google Scholar] [CrossRef]
- Cochrane, D.R.; Howe, E.; Spoelstra, N.S.; Richer, J.K. Loss of miR-200c: A Marker of Aggressiveness and Chemoresistance in Female Reproductive Cancers. J. Oncol. 2009, 2010, 821717. [Google Scholar] [CrossRef]
- Choi, P.-W.; Bahrampour, A.; Ng, S.-K.; Liu, S.K.; Qiu, W.; Xie, F.; Kuo, W.P.; Kwong, J.; Hales, K.H.; Hales, D.B.; et al. Characterization of miR-200 family members as blood biomarkers for human and laying hen ovarian cancer. Sci. Rep. 2020, 10, 20071. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, P.T.; Mainigi, M.; Word, R.A.; Kraus, W.L.; Mendelson, C. miR-200 Regulates Endometrial Development during Early Pregnancy. Mol. Endocrinol. 2016, 30, 977–987. [Google Scholar] [CrossRef]
- Kaller, M.; Hermeking, H. Interplay between transcription factors and microRNAs regulating epithelial-mesenchymal transitions in colorectal cancer. In Non-Coding RNAs in Colorectal Cancer; Springer: Berlin/Heidelberg, Germany, 2016; pp. 71–92. [Google Scholar]
- Hu, W.; Xie, Q.; Xu, Y.; Tang, X.; Zhao, H. Integrated Bioinformatics Analysis Reveals Function and Regulatory Network of miR-200b-3p in Endometriosis. BioMed Res. Int. 2020, 2020, 3962953. [Google Scholar] [CrossRef]
- Park, S.-M.; Gaur, A.B.; Lengyel, E.; Peter, M.E. The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes Dev. 2008, 22, 894–907. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Chen, Y.; Zhao, Y.; Xu, C.; Zhang, A.; Zhang, Q.; Wang, D.; He, J.; Hua, W.; Duan, P. miR-200c suppresses endometriosis by targeting MALAT1 in vitro and in vivo. Stem Cell Res. Ther. 2017, 8, 251. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhang, M.; Zhang, T.; Deng, J.; Xia, X.; Fang, X. microRNA-141 inhibits TGF-β1-induced epithelial-to-mesenchymal transition through inhibition of the TGF-β1/SMAD2 signalling pathway in endometriosis. Arch. Gynecol. Obstet. 2020, 301, 707–714. [Google Scholar] [CrossRef]
- Zhang, Y.; Yan, J.; Pan, X. miR-141-3p affects apoptosis and migration of endometrial stromal cells by targeting KLF-12. Pflügers Arch.-Eur. J. Physiol. 2019, 471, 1055–1063. [Google Scholar] [CrossRef]
- Wang, D.; Luo, Y.; Wang, G.; Yang, Q. CircATRNL1 promotes epithelial–mesenchymal transition in endometriosis by upregulating Yes-associated protein 1 in vitro. Cell Death Dis. 2020, 11, 594. [Google Scholar] [CrossRef]
- Wei, Z.; Zhang, M.; Zhang, X.; Fang, X.; Li, L. Hsa_circ_0063526 promotes the development of endometriosis by sponging miRNA-141-5p. Res. Sq. 2021. [Google Scholar] [CrossRef]
- Dong, L.; Zhang, L.; Liu, H.; Xie, M.; Gao, J.; Zhou, X.; Zhao, Q.; Zhang, S.; Yang, J. Circ_0007331 knock-down suppresses the progression of endometriosis via miR-200c-3p/HiF-1α axis. J. Cell. Mol. Med. 2020, 24, 12656–12666. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, Z.; Xiong, W.; Zhang, L.; Xiong, Y.; Li, N.; He, H.; Du, Y.; Liu, Y. Hypoxia-inducible factor-1α promotes endometrial stromal cells migration and invasion by upregulating autophagy in endometriosis. Reproduction 2017, 153, 809–820. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.; Zhou, Z. Berberine inhibits the proliferation, invasion and migration of endometrial stromal cells by downregulating miR-429. Mol. Med. Rep. 2021, 23, 1–8. [Google Scholar] [CrossRef] [PubMed]
 : Inhibition,
: Inhibition,  : Stimulation.
: Stimulation.
 : Inhibition,
: Inhibition,  : Stimulation.
: Stimulation.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghasemi, F.; Alemzadeh, E.; Allahqoli, L.; Alemzadeh, E.; Mazidimoradi, A.; Salehiniya, H.; Alkatout, I. MicroRNAs Dysregulation as Potential Biomarkers for Early Diagnosis of Endometriosis. Biomedicines 2022, 10, 2558. https://doi.org/10.3390/biomedicines10102558
Ghasemi F, Alemzadeh E, Allahqoli L, Alemzadeh E, Mazidimoradi A, Salehiniya H, Alkatout I. MicroRNAs Dysregulation as Potential Biomarkers for Early Diagnosis of Endometriosis. Biomedicines. 2022; 10(10):2558. https://doi.org/10.3390/biomedicines10102558
Chicago/Turabian StyleGhasemi, Fahimeh, Effat Alemzadeh, Leila Allahqoli, Esmat Alemzadeh, Afrooz Mazidimoradi, Hamid Salehiniya, and Ibrahim Alkatout. 2022. "MicroRNAs Dysregulation as Potential Biomarkers for Early Diagnosis of Endometriosis" Biomedicines 10, no. 10: 2558. https://doi.org/10.3390/biomedicines10102558
APA StyleGhasemi, F., Alemzadeh, E., Allahqoli, L., Alemzadeh, E., Mazidimoradi, A., Salehiniya, H., & Alkatout, I. (2022). MicroRNAs Dysregulation as Potential Biomarkers for Early Diagnosis of Endometriosis. Biomedicines, 10(10), 2558. https://doi.org/10.3390/biomedicines10102558





