Plasma Proteomics in Healthy Subjects with Differences in Tissue Glucocorticoid Sensitivity Identifies A Novel Proteomic Signature
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection of the Healthy Subject Cohort
2.2. Approval of the Study
2.3. Sample Collection
2.4. Assays
2.5. Sequencing of the NR3C1 Gene
2.6. Sample Preparation for Proteomics Analysis
2.7. LC-MS/MS Analysis
2.8. MS Data Processing
2.9. Data Processing (Methods)
3. Results
3.1. Clinical Characteristics, Hematological, Biochemical, and Endocrinological Parameters in the Most Glucocorticoid Sensitive (S) and Most Glucocorticoid Resistant (R) Healthy Subjects
3.2. The S and R Healthy Participants Did Not Harbor Any Genetic Defects in the NR3C1 Gene
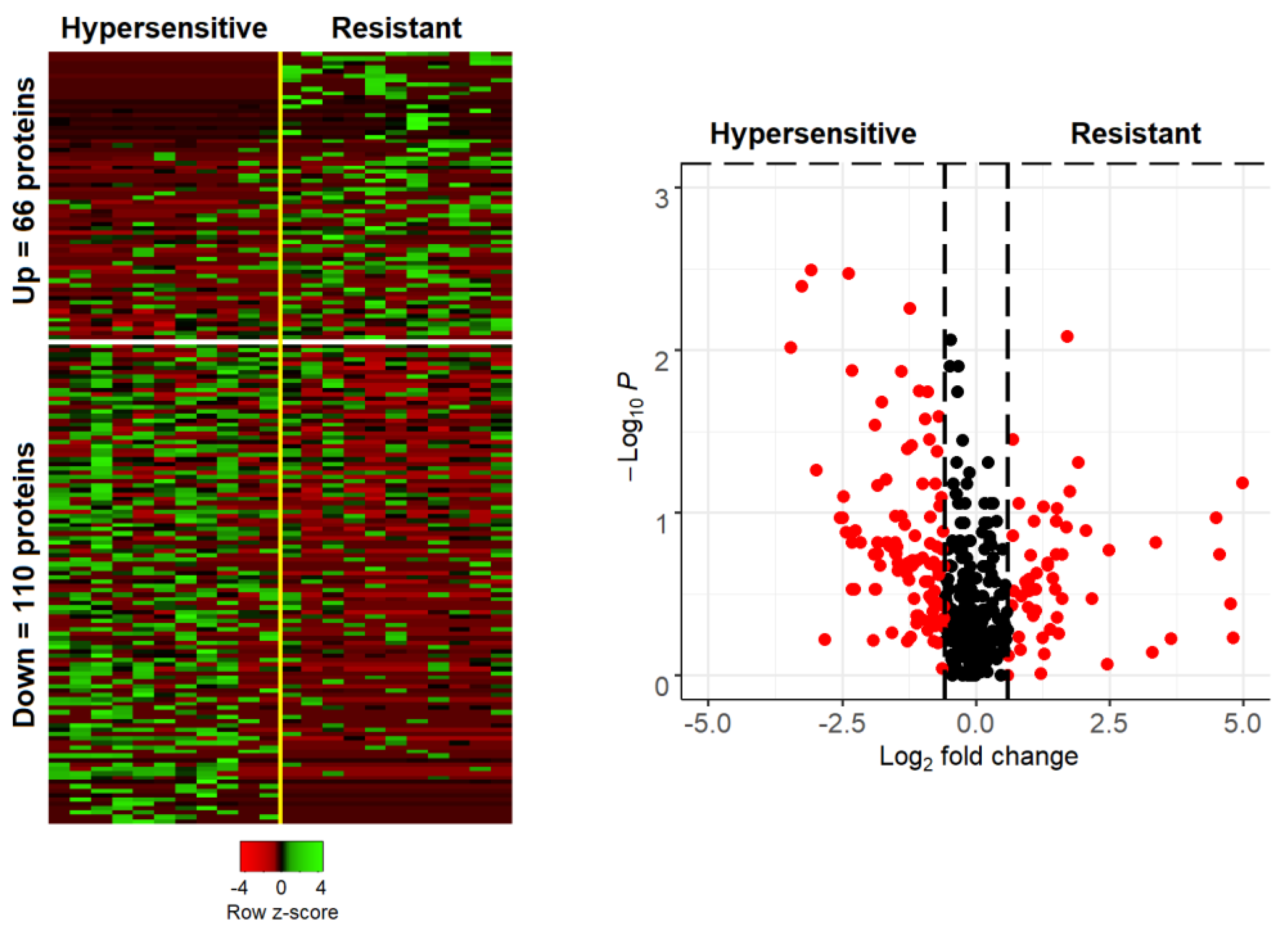
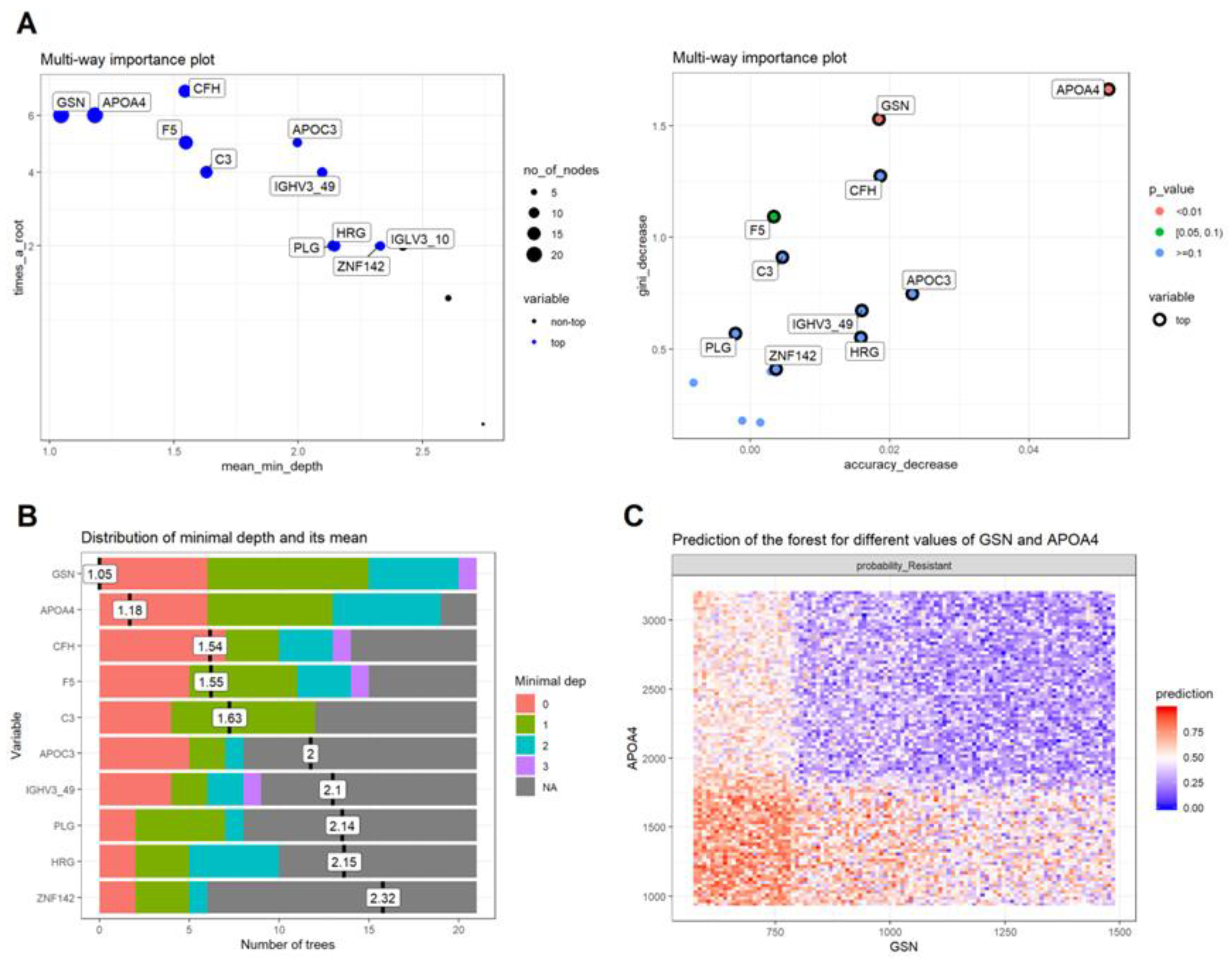
3.3. Proteomics Data Analysis
4. Discussion and Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nicolaides, N.C.; Chrousos, G.; Kino, T.; Feingold, K.R.; Anawalt, B.; Boyce, A.; Chrousos, G.; de Herder, W.W.; Dhatariya, K.; Dungan, K.; et al. Endotext [Internet]. In Glucocorticoid Receptor; MDText.com Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Kadmiel, M.; Cidlowski, J.A. Glucocorticoid receptor signaling in health and disease. Trends Pharmacol. Sci. 2013, 34, 518–530. [Google Scholar] [CrossRef]
- Weikum, E.R.; Knuesel, M.T.; Ortlund, E.A.; Yamamoto, M.T.K.K.R. Glucocorticoid receptor control of transcription: Precision and plasticity via allostery. Nat. Rev. Mol. Cell Biol. 2017, 18, 159–174. [Google Scholar] [CrossRef]
- De Bosscher, K.; Berghe, W.V.; Haegeman, G. The Interplay between the Glucocorticoid Receptor and Nuclear Factor-κB or Activator Protein-1: Molecular Mechanisms for Gene Repression. Endocr. Rev. 2003, 24, 488–522. [Google Scholar] [CrossRef]
- Langlais, D.; Couture, C.; Balsalobre, A.; Drouin, J. The Stat3/GR Interaction Code: Predictive Value of Direct/Indirect DNA Recruitment for Transcription Outcome. Mol. Cell 2012, 47, 38–49. [Google Scholar] [CrossRef]
- Weikum, E.R.; de Vera, I.M.; Nwachukwu, J.; Hudson, W.; Nettles, K.W.; Kojetin, D.J.; Ortlund, E.A. Tethering not required: The glucocorticoid receptor binds directly to activator protein-1 recognition motifs to repress inflammatory genes. Nucleic Acids Res. 2017, 45, 8596–8608. [Google Scholar] [CrossRef]
- Sevilla, L.M.; Jiménez-Panizo, A.; Alegre-Martí, A.; Estébanez-Perpiñá, E.; Caelles, C.; Pérez, P. Glucocorticoid Resistance: Interference between the Glucocorticoid Receptor and the MAPK Signalling Pathways. Int. J. Mol. Sci. 2021, 22, 10049. [Google Scholar] [CrossRef]
- Nicolaides, N.C.; Kino, T.; Roberts, M.L.; Katsantoni, E.; Sertedaki, A.; Moutsatsou, P.; Psarra, A.-M.; Chrousos, G.P.; Charmandari, E. The Role of S-Palmitoylation of the Human Glucocorticoid Receptor (hGR) in Mediating the Nongenomic Glucocorticoid Actions. J. Mol. Biochem. 2017, 6, 3–12. [Google Scholar] [PubMed]
- Thiebaut, C.; Vlaeminck-Guillem, V.; Trédan, O.; Poulard, C.; Le Romancer, M. Non-genomic signaling of steroid receptors in cancer. Mol. Cell. Endocrinol. 2021, 538, 111453. [Google Scholar] [CrossRef]
- Kokkinopoulou, I.; Moutsatsou, P. Mitochondrial Glucocorticoid Receptors and Their Actions. Int. J. Mol. Sci. 2021, 22, 6054. [Google Scholar] [CrossRef] [PubMed]
- Kino, T. Single Nucleotide Variations of the Human GR Gene Manifested as Pathologic Mutations or Polymorphisms. Endocrinology 2018, 159, 2506–2519. [Google Scholar] [CrossRef] [PubMed]
- Nicolaides, N.C.; Charmandari, E. Primary Generalized Glucocorticoid Resistance and Hypersensitivity Syndromes: A 2021 Update. Int. J. Mol. Sci. 2021, 22, 10839. [Google Scholar] [CrossRef]
- Lu, N.Z.; Cidlowski, J.A. Translational Regulatory Mechanisms Generate N-Terminal Glucocorticoid Receptor Isoforms with Unique Transcriptional Target Genes. Mol. Cell 2005, 18, 331–342. [Google Scholar] [CrossRef]
- Lu, N.Z.; Collins, J.B.; Grissom, S.F.; Cidlowski, J.A. Selective Regulation of Bone Cell Apoptosis by Translational Isoforms of the Glucocorticoid Receptor. Mol. Cell. Biol. 2007, 27, 7143–7160. [Google Scholar] [CrossRef] [PubMed]
- Syed, A.P.; Greulich, F.; Ansari, S.A.; Uhlenhaut, N.H. Anti-inflammatory glucocorticoid action: Genomic insights and emerging concepts. Curr. Opin. Pharmacol. 2020, 53, 35–44. [Google Scholar] [CrossRef]
- Kino, T.; Hurt, D.E.; Ichijo, T.; Nader, N.; Chrousos, G.P. Noncoding RNA Gas5 Is a Growth Arrest– and Starvation-Associated Repressor of the Glucocorticoid Receptor. Sci. Signal. 2010, 3, ra8. [Google Scholar] [CrossRef] [PubMed]
- Hardy, R.S.; Raza, K.; Cooper, M.S. Therapeutic glucocorticoids: Mechanisms of actions in rheumatic diseases. Nat. Rev. Rheumatol. 2020, 16, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Yasir, M.; Goyal, A.; Bansal, P.; Sonthalia, S. Corticosteroid adverse effects. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Aebersold, R.; Mann, M. Mass-spectrometric exploration of proteome structure and function. Nature 2016, 537, 347–355. [Google Scholar] [CrossRef]
- Quax, R.A.; Manenschijn, L.; Koper, J.W.; Hazes, J.M.; Lamberts, S.W.J.; Van Rossum, E.F.C.; Feelders, R.A. Glucocorticoid sensitivity in health and disease. Nat. Rev. Endocrinol. 2013, 9, 670–686. [Google Scholar] [CrossRef]
- Donn, R.; Berry, A.; Stevens, A.; Farrow, S.; Betts, J.; Stevens, R.; Clayton, C.; Wang, J.; Warnock, L.; Worthington, J.; et al. Use of gene expression profiling to identify a novel glucocorticoid sensitivity determining gene, BMPRII. FASEB J. 2006, 21, 402–414. [Google Scholar] [CrossRef]
- Nicolaides, N.; Ioannidi, M.-K.; Koniari, E.; Papageorgiou, I.; Bartzeliotou, A.; Sertedaki, A.; Klapa, M.; Charmandari, E. Untargeted Plasma Metabolomics Unravels a Metabolic Signature for Tissue Sensitivity to Glucocorticoids in Healthy Subjects: Its Implications in Dietary Planning for a Healthy Lifestyle. Nutrients 2021, 13, 2120. [Google Scholar] [CrossRef]
- Nicolaides, N.C.; Polyzos, A.; Koniari, E.; Lamprokostopoulou, A.; Papageorgiou, I.; Golfinopoulou, E.; Papathanasiou, C.; Sertedaki, A.; Thanos, D.; Chrousos, G.P.; et al. Transcriptomics in tissue glucocorticoid sensitivity. Eur. J. Clin. Investig. 2019, 49, e13129. [Google Scholar] [CrossRef] [PubMed]
- Wiśniewski, J.R.; Zougman, A.; Nagaraj, N.; Mann, M. Universal sample preparation method for proteome analysis. Nat. Methods 2009, 6, 359–362. [Google Scholar] [CrossRef]
- Latosinska, A.; Vougas, K.; Makridakis, M.; Klein, J.; Mullen, W.; Abbas, M.; Stravodimos, K.; Katafigiotis, I.; Merseburger, A.S.; Zoidakis, J.; et al. Comparative Analysis of Label-Free and 8-Plex iTRAQ Approach for Quantitative Tissue Proteomic Analysis. PLoS ONE 2015, 10, e0137048. [Google Scholar] [CrossRef] [PubMed]
- Bindea, G.; Mlecnik, B.; Hackl, H.; Charoentong, P.; Tosolini, M.; Kirilovsky, A.; Fridman, W.-H.; Pagès, F.; Trajanoski, Z.; Galon, J. ClueGO: A Cytoscape plug-in to decipher functionally grouped gene ontology and pathway annotation networks. Bioinformatics 2009, 25, 1091–1093. [Google Scholar] [CrossRef]
- Huang, B.F.; Boutros, P.C. The parameter sensitivity of random forests. BMC Bioinform. 2016, 17, 331. [Google Scholar] [CrossRef]
- Petkovic, D.; Altman, R.; Wong, M.; Vigil, A. Improving the explainability of Random Forest classifier user centered approach. Biocomputing 2018, 23, 204–205. [Google Scholar] [CrossRef]
- Chrousos, G.P. Stress and disorders of the stress system. Nat. Rev. Endocrinol. 2009, 5, 374–381. [Google Scholar] [CrossRef]
- Nicolaides, N.C.; Kyratzi, E.; Lamprokostopoulou, A.; Chrousos, G.P.; Charmandari, E. Stress, the Stress System and the Role of Glucocorticoids. Neuroimmunomodulation 2015, 22, 6–19. [Google Scholar] [CrossRef]
- Nicolaides, N.C.; Charmandari, E.; Kino, T.; Chrousos, G.P. Stress-Related and Circadian Secretion and Target Tissue Actions of Glucocorticoids: Impact on Health. Front. Endocrinol. 2017, 8, 70. [Google Scholar] [CrossRef] [PubMed]
- Agorastos, A.; Nicolaides, N.C.; Bozikas, V.P.; Chrousos, G.P.; Pervanidou, P. Multilevel Interactions of Stress and Circadian System: Implications for Traumatic Stress. Front. Psychiatry 2020, 10, 1003. [Google Scholar] [CrossRef] [PubMed]
- Isidori, A.M.; Minnetti, M.; Sbardella, E.; Graziadio, C.; Grossman, A.B. Mechanisms in Endocrinology: The spectrum of haemostatic abnormalities in glucocorticoid excess and defect. Eur. J. Endocrinol. 2015, 173, R101–R113. [Google Scholar] [CrossRef] [PubMed]
- Lang, F.; Gawaz, M.; Borst, O. The serum- & glucocorticoid-inducible kinase in the regulation of platelet function. Acta Physiol. 2014, 213, 181–190. [Google Scholar] [CrossRef]
- Karamouzis, I.; Berardelli, R.; D’Angelo, V.; Fussotto, B.; Zichi, C.; Giordano, R.; Settanni, F.; Maccario, M.; Ghigo, E.; Arvat, E. Enhanced oxidative stress and platelet activation in patients with Cushing’s syndrome. Clin. Endocrinol. 2014, 82, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Duverger, N.; Tremp, G.; Caillaud, J.-M.; Emmanuel, F.; Castro, G.; Fruchart, J.-C.; Steinmetz, A.; Denèfle, P. Protection Against Atherogenesis in Mice Mediated by Human Apolipoprotein A-IV. Science 1996, 273, 966–968. [Google Scholar] [CrossRef] [PubMed]
- Lingenhel, A.; Eder, C.; Zwiauer, K.; Stangl, H.; Kronenberg, F.; Patsch, W.; Strobl, W. Decrease of plasma apolipoprotein A-IV during weight reduction in obese adolescents on a low fat diet. Int. J. Obes. 2004, 28, 1509–1513. [Google Scholar] [CrossRef][Green Version]
- Li, G.H.; Arora, P.D.; Chen, Y.; McCulloch, C.A.; Liu, P. Multifunctional roles of gelsolin in health and diseases. Med. Res. Rev. 2010, 32, 999–1025. [Google Scholar] [CrossRef]
- Hirko, A.C.; Meyer, E.M.; King, M.A.; Hughes, J.A. Peripheral Transgene Expression of Plasma Gelsolin Reduces Amyloid in Transgenic Mouse Models of Alzheimer’s Disease. Mol. Ther. 2007, 15, 1623–1629. [Google Scholar] [CrossRef]
- Matsuoka, Y.; Saito, M.; Lafrancois, J.; Saito, M.; Gaynor, K.; Olm, V.; Wang, L.; Casey, E.; Lu, Y.; Shiratori, C.; et al. Novel Therapeutic Approach for the Treatment of Alzheimer’s Disease by Peripheral Administration of Agents with an Affinity to β-Amyloid. J. Neurosci. 2003, 23, 29–33. [Google Scholar] [CrossRef]
- Yang, W.; Chauhan, A.; Mehta, S.; Mehta, P.; Gu, F.; Chauhan, V. Trichostatin A increases the levels of plasma gelsolin and amyloid beta-protein in a transgenic mouse model of Alzheimer’s disease. Life Sci. 2014, 99, 31–36. [Google Scholar] [CrossRef]
| Group | Sample Code | Sex | Weight (kg) | Height (m) | BMI (kg/m2) | Cortisol (nmol/L) | ACTH (pg/mL) |
|---|---|---|---|---|---|---|---|
| Glucocorticoid Sensitive (S) | 1 | F | 58 | 1.64 | 21.6 | 18.6 | <1.0 |
| 2 | F | 62 | 1.75 | 20.2 | 22.2 | 1.4 | |
| 3 | M | 70 | 1.77 | 22.3 | 23.1 | 6.2 | |
| 4 | F | 45 | 1.50 | 20,0 | 24.5 | <1.0 | |
| 5 | M | 70 | 1.85 | 20.5 | 26.2 | 2.9 | |
| 6 | F | 55 | 1.64 | 20.4 | 32.3 | <1.0 | |
| 7 | F | 48 | 1.57 | 19.5 | 34.2 | 5.1 | |
| 8 | M | 80 | 1.78 | 25.2 | 36.1 | <1.0 | |
| 9 | M | 70 | 1.82 | 21.1 | 39.7 | 2.0 | |
| 10 | M | 52 | 1.71 | 17.8 | 51.3 | <1.0 | |
| 11 | M | 81 | 1.87 | 23.2 | 69.5 | 7.6 | |
| Glucocorticoid Resistant (R) | 1 | F | 52 | 1.59 | 20.6 | 834.0 | 35.3 |
| 2 | F | 56 | 1.68 | 19.8 | 720.9 | 38.1 | |
| 3 | F | 59 | 1.55 | 24.6 | 690.8 | 46.0 | |
| 4 | M | 93 | 1.86 | 26.9 | 644.2 | 42.2 | |
| 5 | M | 53 | 1.68 | 18.8 | 599.0 | 32.8 | |
| 6 | F | 47 | 1.54 | 19.8 | 597.9 | 23.7 | |
| 7 | F | 59 | 1.70 | 20.4 | 579.4 | 39.9 | |
| 8 | F | 58 | 1.65 | 21.3 | 565.3 | 16.1 | |
| 9 | F | 58 | 1.7 | 20.1 | 556.2 | 29.9 | |
| 10 | M | 70 | 1.72 | 23.7 | 537.4 | 30.9 | |
| 11 | M | 77 | 1.88 | 21.8 | 520.6 | 12.4 |
| Parameter | Glucocorticoid Sensitive (n = 11) | Glucocorticoid Resistant (n = 11) | * p |
|---|---|---|---|
| Age (year) | 25.27 ± 1.17 | 27.55 ± 2.03 | 0.478 |
| Weight (kg) | 62.82 ± 3.72 | 62.00 ± 3.98 | 0.847 |
| Height (cm) | 1.72 ± 0.04 | 1.69 ± 0.03 | 0.519 |
| BMI (kg/m2) | 21.07 ± 0.60 | 21.62 ± 0.74 | 0.797 |
| ACTH (pg/mL) | 33.16 ± 5.67 | 27.64 ± 4.65 | 0.519 |
| CORT (μg/dL) | 23.13 ± 1.70 | 18.98 ± 3.06 | 0.270 |
| IGF-I (ng/mL) | 259.18 ± 23.97 | 251.36 ± 20.15 | 0.699 |
| IGFBP-3 (μg/mL) | 5.30 ± 0.31 | 5.17 ± 0.37 | 0.562 |
| TSH (μUI/mL) | 2.79 ± 0.28 | 2.05 ± 0.33 | 0.101 |
| T3 (ng/dL) | 102.26 ± 8.33 | 102.02 ± 7.19 | 0.982 |
| FT4 (ng/dL) | 1.12 ± 0.04 | 1.06 ± 0.03 | 0.261 |
| Anti-TPO (IU/mL) | 10.43 ± 0.21 | 11.11 ± 0.78 | 0.652 |
| Anti-TG (IU/mL) | 20.00 ± 0.00 | 20.00 ± 0.00 | 0.999 |
| LH (mUI/mL) | 10.11 ± 4.50 | 6.44 ± 0.69 | 0.699 |
| FSH (mUI/mL) | 5.22 ± 0.83 | 4.05 ± 0.70 | 0.300 |
| DHEAS (μg/dL) | 238.62 ± 44.03 | 248.58 ± 34.68 | 0.562 |
| Androstenedione (ng/mL) | 2.89 ± 0.28 | 3.20 ± 0.35 | 0.502 |
| PRL (ng/mL) | 24.94 ± 2.65 | 21.55 ± 2.75 | 0.193 |
| SHBG (nmol/L) | 65.12 ± 8.42 | 46.17 ± 5.09 | 0.175 |
| PTH (pg/mL) | 34.15 ± 4.59 | 38.51 ± 5.40 | 0.562 |
| 25-Hydroxy-Vitamin D (ng/mL) | 16.06 ± 2.38 | 14.02 ± 2.56 | 0.652 |
| Insulin (μUI/mL) | 6.71 ± 0.81 | 13.72 ± 4.22 | 0.116 |
| Glucose (mg/dL) | 73.20 ± 1.99 | 74.75 ± 4.80 | 0.965 |
| Urea (mg/dL) | 27.70 ± 2.06 | 32.50 ± 2.90 | 0.203 |
| Cholesterol (mg/dL) | 157.40 ± 5.34 | 156.75 ± 5.30 | 0.965 |
| HDL (mg/dL) | 49.50 ± 2.21 | 52.88 ± 2.86 | 0.315 |
| LDL (mg/dL) | 90.70 ± 5.63 | 87.63 ± 4.78 | 0.762 |
| Triglycerides (mg/dL) | 69.40 ± 9.48 | 74.25 ± 5.66 | 0.315 |
| ApoA1 (mg/dL) | 158.40 ± 2.54 | 167.63 ± 5.32 | 0.237 |
| ApoB (mg/dL) | 75.50 ± 4.55 | 71.38 ± 2.73 | 0.515 |
| Lpa (mg/dL) | 21.84 ± 11.82 | 25.79 ± 9.66 | 0.460 |
| Hct (%) | 43.09 ± 1.07 | 44.64 ± 2.32 | 0.748 |
| WBC (×103/μL) | 6.72 ± 0.49 | 7.09 ± 0.52 | 0.612 |
| PLT (×103/μL) | 236.55 ± 22.11 | 233.09 ± 32.56 | 0.847 |
| Protein | Description | p Value | Present |
|---|---|---|---|
| KIF28P | Kinesin-like protein KIF28P | 0.015762 | Only in resistant |
| MRPS34 | 28S ribosomal protein S34, mitochondrial | 0.015762 | Only in resistant |
| PRPF8 | Pre-mRNA-processing-splicing factor 8 | 0.015762 | Only in resistant |
| MYH11 | Myosin-11 | 0.03591 | Only in resistant |
| MLH1 | DNA mismatch repair protein Mlh1 | 0.03591 | Only in resistant |
| ARHGAP21 | Rho GTPase-activating protein 21 | 0.03591 | Only in resistant |
| EMC10 | ER membrane protein complex subunit 10 | 0.03591 | Only in resistant |
| ZSWIM9 | Uncharacterized protein ZSWIM9 | 0.03591 | Only in resistant |
| FANCB | Fanconi anemia group B protein | 0.03591 | Only in resistant |
| CDADC1 | Cytidine and dCMP deaminase domain-containing protein 1 | 0.03591 | Only in resistant |
| ACSS3 | Acyl-CoA synthetase short-chain family member 3, mitochondrial | 0.03591 | Only in resistant |
| IGHV3-66 | Immunoglobulin heavy variable 3-66 | 0.03591 | Only in sensitive |
| IGLV5-39 | Immunoglobulin lambda variable 5-39 | 0.03591 | Only in sensitive |
| LCP1 | Plastin-2 | 0.03591 | Only in sensitive |
| DOCK4 | Dedicator of cytokinesis protein 4 | 0.03591 | Only in sensitive |
| SLC38A3 | Sodium-coupled neutral amino acid transporter 3 | 0.03591 | Only in sensitive |
| RTN4 | Reticulon-4 | 0.03591 | Only in sensitive |
| CFAP97 | Cilia- and flagella-associated protein 97 | 0.03591 | Only in sensitive |
| POLK | DNA polymerase kappa | 0.03591 | Only in sensitive |
| ANKRD50 | Ankyrin repeat domain-containing protein 50 | 0.03591 | Only in sensitive |
| Reactome Pathway | p Value | % Associated Genes | Associated Genes Found |
|---|---|---|---|
| Erythrocytes take up oxygen and release carbon dioxide | 7.07 × 10−5 | 33.3 | (CA1, CA2, HBA1) |
| G-protein mediated events | 0.004559 | 5.5 | (CAMKK2, ITPR1, ITPR2) |
| PLC beta mediated events | 0.004452 | 5.6 | (CAMKK2, ITPR1, ITPR2) |
| DAG and IP3 signaling | 0.002614 | 7.1 | (CAMKK2, ITPR1, ITPR2) |
| Signaling by VEGF | 0.000892 | 4.7 | (CDH5, CRK, ITGB3, ITPR1, ITPR2) |
| VEGFA-VEGFR2 Pathway | 0.0007 | 5.1 | (CDH5, CRK, ITGB3, ITPR1, ITPR2) |
| Platelet activation, signaling and aggregation | 1.5 × 10−6 | 4.6 | (CRK, F8, FLNA, ITGB3, ITPR1, ITPR2, PFN1, PPBP, QSOX1, RARRES2, TUBA4A, VCL) |
| Fcgamma receptor (FCGR) dependent phagocytosis | 0.002295 | 4.7 | (CRK, FCGR3A, ITPR1, ITPR2) |
| Platelet degranulation | 1.18 × 10−6 | 7.0 | (F8, FLNA, ITGB3, PFN1, PPBP, QSOX1, RARRES2, TUBA4A, VCL) |
| Response to elevated platelet cytosolic Ca2+ | 1.1 × 10−6 | 6.7 | (F8, FLNA, ITGB3, PFN1, PPBP, QSOX1, RARRES2, TUBA4A, VCL) |
| Role of phospholipids in phagocytosis | 0.000858 | 12.0 | (FCGR3A, ITPR1, ITPR2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nicolaides, N.C.; Makridakis, M.; Stroggilos, R.; Lygirou, V.; Koniari, E.; Papageorgiou, I.; Sertedaki, A.; Zoidakis, J.; Charmandari, E. Plasma Proteomics in Healthy Subjects with Differences in Tissue Glucocorticoid Sensitivity Identifies A Novel Proteomic Signature. Biomedicines 2022, 10, 184. https://doi.org/10.3390/biomedicines10010184
Nicolaides NC, Makridakis M, Stroggilos R, Lygirou V, Koniari E, Papageorgiou I, Sertedaki A, Zoidakis J, Charmandari E. Plasma Proteomics in Healthy Subjects with Differences in Tissue Glucocorticoid Sensitivity Identifies A Novel Proteomic Signature. Biomedicines. 2022; 10(1):184. https://doi.org/10.3390/biomedicines10010184
Chicago/Turabian StyleNicolaides, Nicolas C., Manousos Makridakis, Rafael Stroggilos, Vasiliki Lygirou, Eleni Koniari, Ifigeneia Papageorgiou, Amalia Sertedaki, Jerome Zoidakis, and Evangelia Charmandari. 2022. "Plasma Proteomics in Healthy Subjects with Differences in Tissue Glucocorticoid Sensitivity Identifies A Novel Proteomic Signature" Biomedicines 10, no. 1: 184. https://doi.org/10.3390/biomedicines10010184
APA StyleNicolaides, N. C., Makridakis, M., Stroggilos, R., Lygirou, V., Koniari, E., Papageorgiou, I., Sertedaki, A., Zoidakis, J., & Charmandari, E. (2022). Plasma Proteomics in Healthy Subjects with Differences in Tissue Glucocorticoid Sensitivity Identifies A Novel Proteomic Signature. Biomedicines, 10(1), 184. https://doi.org/10.3390/biomedicines10010184









