The Rural Nursing Workforce Hierarchy of Needs: Decision-Making concerning Future Rural Healthcare Employment
Abstract
:1. Introduction
Aim, Purpose, and Research Questions of the Study
2. Materials and Methods
2.1. Sample
2.2. Data Collection Tool
2.3. Data Collection
2.4. Data Analysis
2.5. Theoretical Frameowork to Understand the Data
2.6. Ethical Considerations
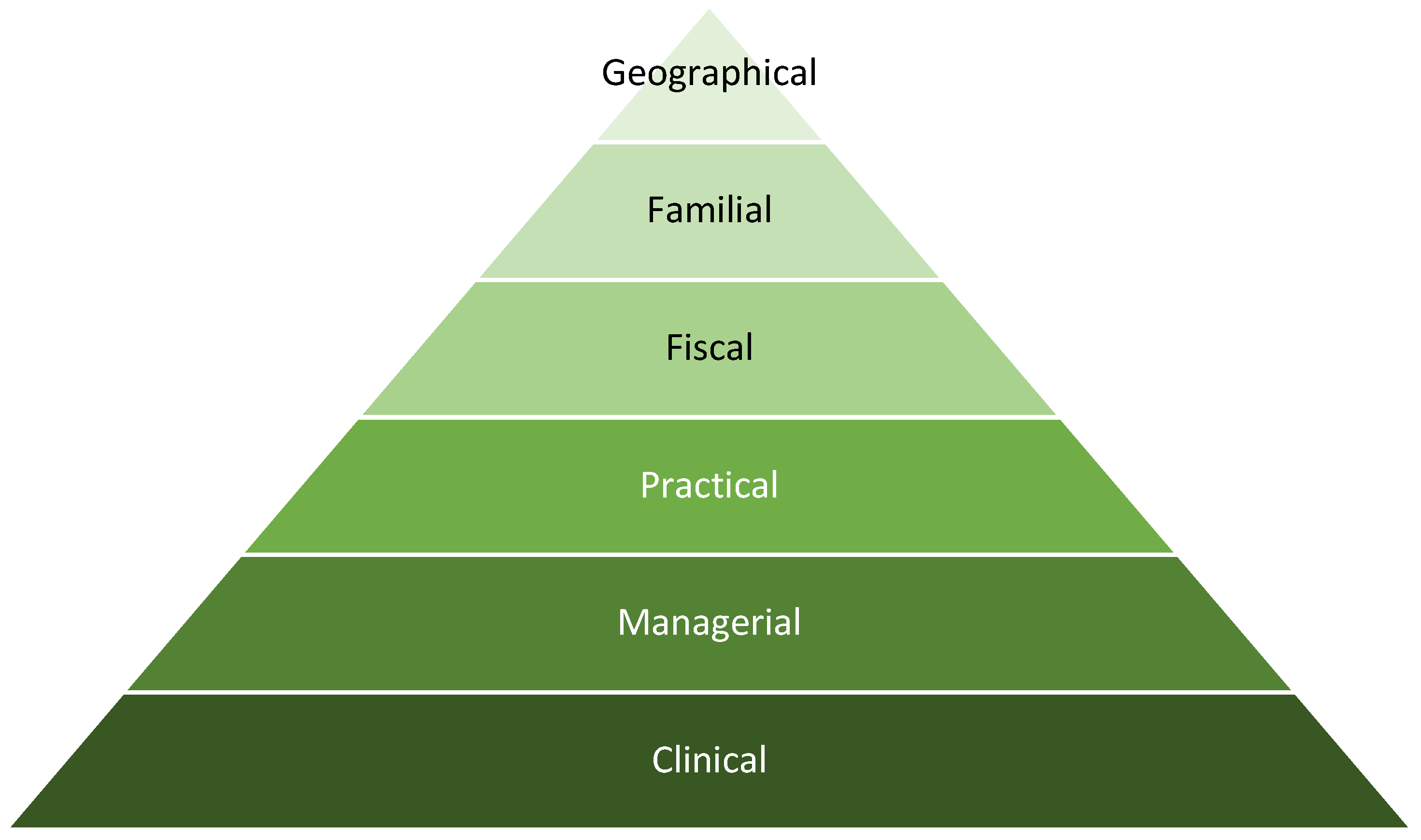
3. Results
3.1. Clinical
3.2. Managerial
3.3. Practical
3.4. Fiscal
3.5. Familial
3.6. Geographical
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Humphreys, J.; Lyle, D.; Barlow, V. Rural and Remote Health University Departments of Rural Health: Is a national network of multidisciplinary academic departments in Australia making a difference? Rural Remote Health 2018, 18, 4315. [Google Scholar]
- Strasser, R. Learning in context: Education for remote rural health care. Rural Remote Health 2016, 16. [Google Scholar] [CrossRef]
- Geyman, J.P.; Hart, L.G.; Norris, T.E.; Coombs, J.B.; Lishner, D.M. Educating generalist physicians for rural practice: How are we doing? J. Rural Health 2000, 16, 56–80. [Google Scholar] [CrossRef]
- Longenecker, R.L.; Schmitz, D. Building a community of practice in rural medical education: Growing our own together. Rural Remote Health 2017, 17, 4195. [Google Scholar] [CrossRef]
- Cleland, J.; Johnston, P.; Walker, L.; Needham, G. Attracting healthcare professionals to remote and rural medicine: Learning from doctors in training in the north of Scotland. Med. Teach. 2012, 34, e476–e482. [Google Scholar] [CrossRef] [PubMed]
- Buchan, J.; Couper, I.D.; Tangcharoensathien, V.; Thepannya, K.; Jaskiewicz, W.; Perfilieva, G.; Dolea, C. Early implementation of WHO recommendations for the retention of health workers in remote and rural areas. Bull. World Health Organ. 2013, 91, 834–840. [Google Scholar] [CrossRef] [PubMed]
- Trépanier, A.; Gagnon, M.P.; Mbemba, G.I.C.; Côté, J.; Paré, G.; Fortin, J.P.; Duplàa, E.; Courcy, F. Factors associated with intended and effective settlement of nursing students and newly graduated nurses in a rural setting after graduation: A mixed-methods review. Int. J. Nurs. Stud. 2013, 50, 314–325. [Google Scholar] [CrossRef] [PubMed]
- Cosgrave, C.; Maple, M.; Hussain, R. An explanation of turnover intention among early-career nursing and allied health professionals working in rural and remote Australia-findings from a grounded theory study. Rural Remote Health 2018, 18, 4511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cosgrave, C.; Malatzky, C.; Gillespie, J. Social Determinants of Rural Health Workforce Retention: A Scoping Review. Int. J. Environ. Res. Public Health 2019, 16, 314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reed, A.J.; Schmitz, D.; Baker, E.; Nukui, A.; Epperly, T. Association of "Grit" and Satisfaction in Rural and Nonrural Doctors. J. Am. Board Fam. Med. 2012, 25, 832–839. [Google Scholar] [CrossRef] [Green Version]
- Prengaman, M.; Terry, D.R.; Schmitz, D.; Baker, E. The Nursing Community Apgar Questionnaire in Rural Australia: An evidence based approach to recruiting and retaining nurses. Online J. Rural. Nurs. Health Care 2017, 17, 148–171. [Google Scholar] [CrossRef]
- Playford, D.; Moran, M.C.; Thompson, S. Factors associated with rural work for nursing and allied health graduates 15–17 years after an undergraduate rural placement through the University Department of Rural Health program. Rural Remote Health 2020, 20, 5334. [Google Scholar] [CrossRef] [PubMed]
- Lea, J.; Cruickshank, M.; Paliadelis, P.; Parmenter, G.; Sanderson, H.; Thornberry, P. The lure of the bush: Do rural placements influence student nurses to seek employment in rural settings? Collegian 2008, 15, 77–82. [Google Scholar] [CrossRef]
- Smith, T.; Sutton, K.; Pit, S.; Muyambi, K.; Terry, D.; Farthing, A.; Courtney, C.; Cross, M. Health professional students’ rural placement satisfaction and rural practice intentions: A national cross-sectional survey. Aust. J. Rural. Health 2017, 26, 26–32. [Google Scholar] [CrossRef] [Green Version]
- Sutton, K.; Waller, S.; Fisher, K.; Farthing, A.; McAnnally, K.; Russell, D.; Smith, T.; Maybery, D.; McGrail, M.; Carey, T.; et al. “Heck Yes”—Understanding the Decision to Relocate Rural Amongst Urban Nursing and Allied Health Students and Recent Graduates; Monash University Department of Rural Health: Victoria, Australia, 2016. [Google Scholar]
- Terry, D.; Peck, B.; Smith, A.; Stevenson, T.; Baker, E. Is nursing student personality important for considering a rural career? J. Health Organ. Manag. 2019, 33, 617–634. [Google Scholar] [CrossRef] [PubMed]
- Terry, D.; Peck, B.; Smith, A.; Stevenson, T.; Nguyen, H.; Baker, E. What Australian Nursing Students Value as Important in Undertaking Rural Practice. Online J. Rural Nurs. Health Care 2020, 20, 32–56. [Google Scholar] [CrossRef]
- Baker, E.; Schmitz, D.; MacKenzie, L.; Morris, B.; Epperly, T. Rural community variation in physician recruitment readiness. J. Health Sci. 2014, 2, 393–401. [Google Scholar]
- Terry, D.; Peck, B.; Smith, A.; Nguyen, H. Occupational Self-Efficacy and Psychological Capital Amongst Nursing Students: A Cross Sectional Study Understanding the Malleable Attributes for Success. Eur. J. Investig. Health Psychol. Educ. 2019, 10, 14. [Google Scholar] [CrossRef] [Green Version]
- Reed, A.J.; Schmitz, D.; Baker, E.; Girvan, J.; McDonald, T. Assessment of Factors for Recruiting and Retaining Medical Students to Rural Communities Using the Community Apgar Questionnaire. Fam. Med. 2017, 49, 132–136. [Google Scholar] [PubMed]
- Scott, A.; Witt, J.; Humphreys, J.; Joyce, C.; Kalb, G.; Jeon, S.-H.; McGrail, M. Getting doctors into the bush: General Practitioners’ preferences for rural location. Soc. Sci. Med. 2013, 96, 33–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wakerman, J.; Humphreys, J.; Russell, D.; Guthridge, S.; Bourke, L.; Dunbar, T.; Zhao, Y.; Ramjan, M.; Murakami-Gold, L.; Jones, M.P. Remote health workforce turnover and retention: What are the policy and practice priorities? Hum. Resour. Health 2019, 17, 99. [Google Scholar] [CrossRef]
- Buykx, P.; Humphreys, J.; Wakerman, J.; Pashen, D. Systematic review of effective retention incentives for health workers in rural and remote areas: Towards evidence-based policy. Aust. J. Rural. Health 2010, 18, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Baker, E.; Schmitz, D.; A Wasden, S.; Mackenzie, L.; Epperly, T. Assessing Community Health Center (CHC) assets and capabilities for recruiting physicians: The CHC Community Apgar Questionnaire. Rural Remote Health 2012, 12, 2179. [Google Scholar] [CrossRef]
- Schmitz, D.; Baker, E. (Eds.) Assessing Critical Access Hospital (CAH) Assets and Capabilities for Recruiting and Retaining Physicians: The North Dakota CAH Community Apgar Program. In Proceedings of the Dakota Conference on Rural and Public Health, Grand Forks, ND, USA, 30 May 2012. [Google Scholar]
- Prengaman, M.; Bigbee, J.; Baker, E.; Schmitz, D. Development of the Nursing Community Apgar Questionnaire (NCAQ): A rural nurse recruitment and retention tool. Rural Remote Health 2014, 14, 2633. [Google Scholar] [CrossRef]
- Brodie, D.A.; Andrews, G.J.; Andrews, J.P.; Thomas, B.G.; Wong, J.; Rixon, L. Working in London hospitals: Perceptions of place in nursing students’ employment considerations. Soc. Sci. Med. 2005, 61, 1867–1881. [Google Scholar] [CrossRef]
- Hemphill, E.; Kulik, C. Recruitment Ad Analysis Offers New Opportunities to Attract GPs to Short-Staffed Practices. Health Mark. Q. 2013, 30, 144–161. [Google Scholar] [CrossRef]
- Stroth, C. Job Embeddedness as a Nurse Retention Strategy for Rural Hospitals. JONA J. Nurs. Adm. 2010, 40, 32–35. [Google Scholar] [CrossRef]
- Terry, D.R.; Nguyen, H.B.; Prengaman, M.; Schmitz, D.; Baker, E. Marketing Your Rural Community: Identifying Strengths and Addressing Challenges to Recruit Rural Nurses; The University of Melbourne: Shepparton, Australia, 2017; pp. 1–66. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 24.0; IBM Corp.: Armonk, NY, USA, 2016. [Google Scholar]
- Pallant, J. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using SPSS for Windows, 4th ed.; Allen & Unwin: Crows Nest, Australia, 2011. [Google Scholar]
- Maslow, A.H. A theory of human motivation. Psychol. Rev. 1943, 50, 370–396. [Google Scholar] [CrossRef] [Green Version]
- Freitas, F.A.; Leonard, L. Maslow’s hierarchy of needs and student academic success. Teach. Learn. Nurs. 2011, 6, 9–13. [Google Scholar] [CrossRef]
- Benson, S.G.; Dundis, S. Understanding and motivating health care employees: Integrating Maslow’s hierarchy of needs, training and technology. J. Nurs. Manag. 2003, 11, 315–320. [Google Scholar] [CrossRef]
- Zalenski, R.J.; Raspa, R. Maslow’s hierarchy of needs: A framework for achieving human potential in hospice. J. Palliat. Med. 2006, 9, 1120–1127. [Google Scholar] [CrossRef]
- Urwiler, R.; Frolick, M.N. The IT value hierarchy: Using Maslow’s hierarchy of needs as a metaphor for gauging the maturity level of information technology use within competitive organizations. Inf. Syst. Manag. 2008, 25, 83–88. [Google Scholar] [CrossRef]
- Tikkanen, I. Maslow’s hierarchy and food tourism in Finland: Five cases. Br. Food J. 2007, 109, 721–734. [Google Scholar] [CrossRef]
- Maslow, A.H. The Maslow Business Reader; Stephens, D.C., Ed.; John Wiley & Sons: New York, NY, USA, 2000. [Google Scholar]
- Strachota, E.; Normandin, P.; O’Brien, N.; Clary, M.; Krukow, B. Reasons Registered Nurses Leave or Change Employment Status. JONA J. Nurs. Adm. 2003, 33, 111–117. [Google Scholar] [CrossRef]
- Fields, B.E.; Bell, J.F.; Bigbee, J.L.; Thurston, H.; Spetz, J. Registered nurses’ preferences for rural and urban jobs: A discrete choice experiment. Int. J. Nurs. Stud. 2018, 86, 11–19. [Google Scholar] [CrossRef]
- Kramer, M.; Brewer, B.B.; Maguire, P. Impact of Healthy Work Environments on New Graduate Nurses’ Environmental Reality Shock. West. J. Nurs. Res. 2011, 35, 348–383. [Google Scholar] [CrossRef]
- Papastavrou, E.; Dimitriadou, M.; Tsangari, H.; Andreou, C. Nursing students’ satisfaction of the clinical learning environment: A research study. BMC Nurs. 2016, 15, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Kenny, P.; Reeve, R.; Hall, J. Satisfaction with nursing education, job satisfaction, and work intentions of new graduate nurses. Nurse Educ. Today 2015, 36, 230–235. [Google Scholar] [CrossRef]
- Hoeve, Y.T.; Castelein, S.; Jansen, G.; Roodbol, P. Dreams and disappointments regarding nursing: Student nurses’ reasons for attrition and retention. A qualitative study design. Nurse Educ. Today 2017, 54, 28–36. [Google Scholar] [CrossRef]
- Hamshire, C.; Jack, K.; Forsyth, R.; Langan, A.M.; Harris, W.E. The wicked problem of healthcare student attrition. Nurs. Inq. 2019, 26, e12294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, A.; Rahman, R.; Jiaqing, O. A crisis in the countryside—Barriers to nurse recruitment and retention in rural areas of high-income countries: A qualitative meta-analysis. J. Rural. Stud. 2019, 72, 153–163. [Google Scholar] [CrossRef]
- Terry, D.; Peck, B.; Baker, E. Self-efficacy, grit and perceptions of rural employment: What changes occur after graduation? Online J. Rural. Nurs Health Care 2021, 21. in press. [Google Scholar]
- Foster, K.I.; Benavides-Vaello, S.; Katz, J.R.; Eide, P. Using the Generative Nursing Model to Reframe Nursing Student Transition to Practice. Nurse Educ. 2012, 37, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Rockers, P.C.; Jaskiewicz, W.; Kruk, M.E.; Phathammavong, O.; Vangkonevilay, P.; Paphassarang, C.; Phachanh, I.T.; Wurts, L.; Tulenko, K. Differences in preferences for rural job postings between nursing students and practicing nurses: Evidence from a discrete choice experiment in Lao People’s Democratic Republic. Hum. Resour. Health 2013, 11, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Student Enrolments | 2018 | 2019 | 2020 |
|---|---|---|---|
| First year enrolments | 862 | 921 | 978 |
| Second year enrolments | 788 | 931 | 953 |
| Third year enrolments | 388 | 501 | 416 |
| Total enrolments (Actual) | 2038 | 2353 | 2347 |
| Demographic Information | Frequency | ||||||
|---|---|---|---|---|---|---|---|
| 2018 | 2019 | 2020 | Total | ||||
| n | (%) | n | (%) | n | (%) | n | |
| Year of program (n = 804) | |||||||
| 61 | 29.61% | 94 | 34.18% | 134 | 41.49% | 289 |
| 71 | 34.47% | 104 | 37.82% | 102 | 31.58% | 277 |
| 70 | 33.98% | 77 | 28.00% | 45 | 13.93% | 192 |
| 4 | 1.94% | 0 | 0.00% | 42 | 13.00% | 46 |
| Gender (n = 804) | |||||||
| 181 | 87.86% | 199 | 72.36% | 248 | 76.78% | 628 |
| 21 | 10.19% | 22 | 8.00% | 31 | 9.60% | 74 |
| 0 | 0.00% | 2 | 0.73% | 2 | 0.62% | 4 |
| 4 | 1.94% | 52 | 18.91% | 42 | 13.00% | 98 |
| Age (years) (n = 804) | |||||||
| 24 | 11.65% | 14 | 5.09% | 57 | 17.65% | 95 |
| 55 | 26.70% | 84 | 30.55% | 88 | 27.24% | 227 |
| 59 | 28.64% | 78 | 28.36% | 95 | 29.41% | 232 |
| 43 | 20.87% | 46 | 16.73% | 64 | 19.81% | 153 |
| 9 | 4.37% | 23 | 8.36% | 19 | 5.88% | 51 |
| 16 | 7.77% | 30 | 10.91% | 0 | 0.00% | 46 |
| Born in Australia (n = 804) | |||||||
| 163 | 79.13% | 164 | 59.64% | 160 | 49.54% | 487 |
| 39 | 18.93% | 59 | 21.45% | 121 | 37.46% | 219 |
| 4 | 1.94% | 52 | 18.91% | 42 | 13.00% | 98 |
| Marital status (n = 878) | |||||||
| 72 | 34.95% | 73 | 26.55% | 104 | 32.20% | 249 |
| 112 | 54.37% | 127 | 46.18% | 150 | 46.44% | 389 |
| 11 | 5.34% | 12 | 4.36% | 17 | 5.26% | 40 |
| 6 | 2.91% | 2 | 0.73% | 10 | 3.10% | 18 |
| 5 | 2.43% | 61 | 22.18% | 42 | 13.00% | 108 |
| Highest level of education (n = 804) | |||||||
| 29 | 14.08% | 66 | 24.00% | 112 | 39.86% | 207 |
| 141 | 68.45% | 123 | 44.73% | 126 | 44.84% | 390 |
| 34 | 16.50% | 25 | 9.09% | 38 | 13.52% | 97 |
| 2 | 0.97% | 4 | 1.45% | 5 | 1.78% | 11 |
| 0 | 0.00% | 57 | 20.73% | 42 | 13.00% | 99 |
| Employment status (n = 804) | 281 | ||||||
| 36 | 17.48% | 29 | 10.55% | 20 | 6.19% | 85 |
| 57 | 27.67% | 88 | 32.00% | 66 | 20.43% | 211 |
| 80 | 38.83% | 103 | 37.45% | 126 | 39.01% | 309 |
| 22 | 10.68% | 38 | 13.82% | 29 | 8.98% | 89 |
| 11 | 5.34% | 17 | 6.18% | 82 | 25.39% | 110 |
| Current after-tax income (AUD) a week (n = 804) | |||||||
| 85 | 41.26% | 94 | 34.18% | 70 | 21.67% | 249 |
| 65 | 31.55% | 110 | 40.00% | 114 | 35.29% | 289 |
| 26 | 12.62% | 40 | 14.55% | 45 | 13.93% | 111 |
| 3 | 1.46% | 5 | 1.82% | 8 | 2.48% | 16 |
| 23 | 11.17% | 0 | 0.00% | 27 | 8.36% | 50 |
| 4 | 1.94% | 26 | 9.45% | 59 | 18.27% | 89 |
| Where participant grew up (n = 804) | |||||||
| 10 | 4.95% | 17 | 6.18% | 37 | 11.46% | 64 |
| 48 | 23.76% | 47 | 17.09% | 64 | 19.81% | 159 |
| 45 | 22.28% | 50 | 18.18% | 47 | 14.55% | 142 |
| 60 | 29.70% | 79 | 28.73% | 86 | 26.63% | 225 |
| 30 | 14.85% | 23 | 8.36% | 30 | 9.29% | 83 |
| 9 | 4.46% | 7 | 2.55% | 17 | 5.26% | 33 |
| 4 | 1.94% | 69 | 25.09% | 79 | 24.46% | 162 |
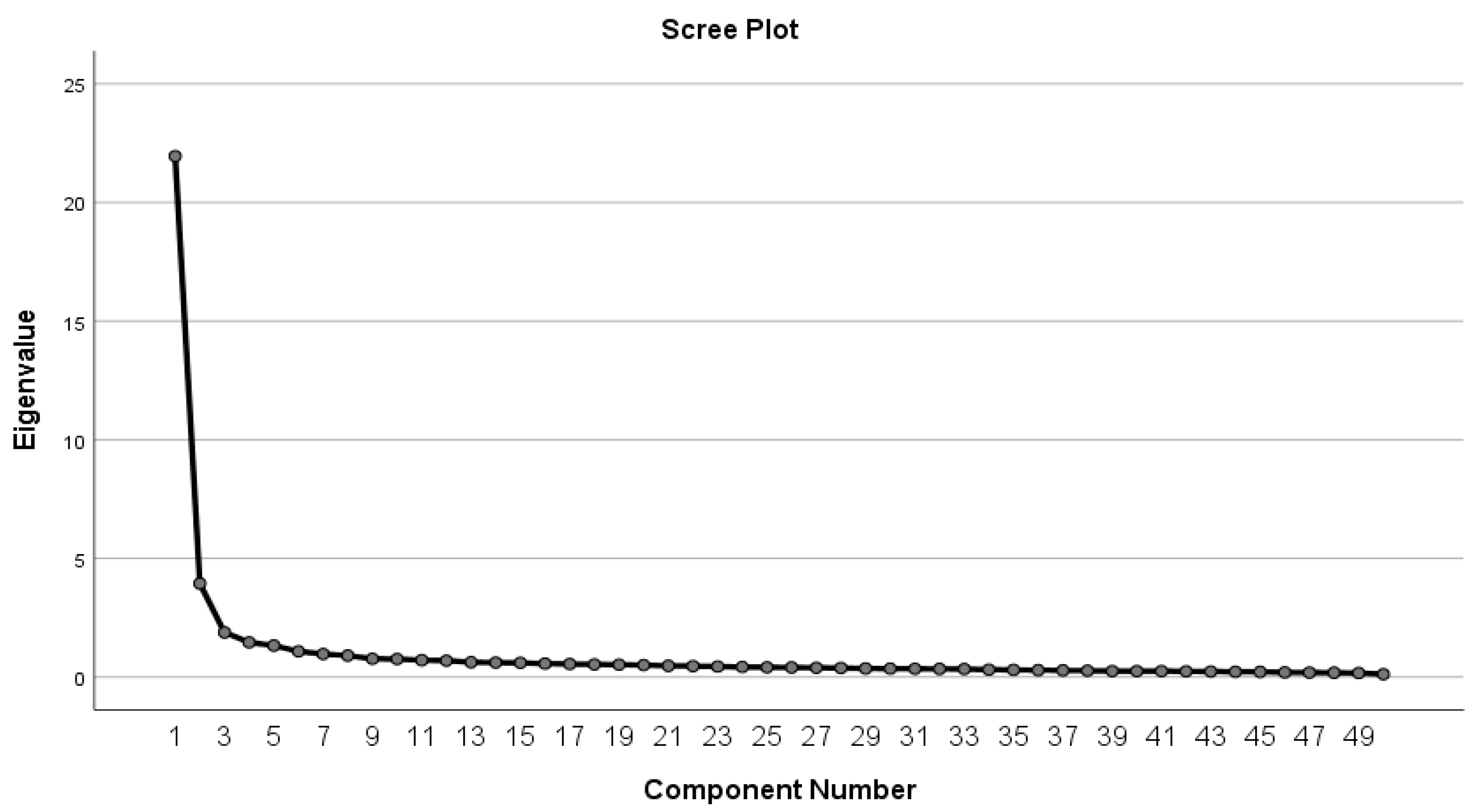
| Component | Initial Eigenvalues | Extraction Sums of Squared Loadings | Rotation Sums of Squared Loadings | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | |
| 1 | 21.952 | 43.904 | 43.904 | 21.952 | 43.904 | 43.904 | 11.897 | 23.794 | 23.794 |
| 2 | 3.943 | 7.885 | 51.789 | 3.943 | 7.885 | 51.789 | 4.998 | 9.995 | 33.789 |
| 3 | 1.878 | 3.756 | 55.546 | 1.878 | 3.756 | 55.546 | 4.595 | 9.191 | 42.980 |
| 4 | 1.461 | 2.921 | 58.467 | 1.461 | 2.921 | 58.467 | 4.573 | 9.146 | 52.126 |
| 5 | 1.324 | 2.648 | 61.115 | 1.324 | 2.648 | 61.115 | 3.340 | 6.681 | 58.807 |
| 6 | 1.082 | 2.164 | 63.279 | 1.082 | 2.164 | 63.279 | 2.236 | 4.473 | 63.279 |
| Factor | Clinical 1 | Fiscal 2 | Practical 3 | Geographical 4 | Managerial 5 | Familial 6 |
|---|---|---|---|---|---|---|
| Emphasis on patient safety/high-quality care | 0.834 | |||||
| Positive relationships/communication among nurse generations | 0.800 | |||||
| Positive workplace culture/supportive working environment that fosters mentoring | 0.790 | |||||
| Job satisfaction morale level | 0.754 | |||||
| Autonomy/respect | 0.753 | |||||
| Manageable workload/increased time with patients | 0.720 | |||||
| Effective partnership between medical and nursing staff | 0.702 | |||||
| Nurse empowerment | 0.635 | |||||
| Ethical climate | 0.635 | |||||
| Evidence-based practice | 0.634 | |||||
| Thorough orientation/preceptorship | 0.629 | |||||
| Acceptance of nurses new to area | 0.626 | |||||
| Nursing workforce adequacy and stability | 0.626 | |||||
| Moving allowance | 0.754 | |||||
| Benefits | 0.748 | |||||
| Salary | 0.664 | |||||
| Shift differential | 0.624 | |||||
| Cost of living | 0.620 | |||||
| Housing availability/affordability | 0.552 | |||||
| Image of rural health care and positive image of job environment | 0.679 | |||||
| Community health/nursing services | 0.624 | |||||
| Sense of reciprocity between nurses and community | 0.620 | |||||
| Welcome and recruitment program | 0.609 | |||||
| Distance education access | 0.600 | |||||
| Demographics/patient mix | 0.761 | |||||
| Social networking | 0.754 | |||||
| Recreational opportunities | 0.688 | |||||
| Access to larger community | 0.687 | |||||
| Size of community | 0.639 | |||||
| Nurses involved in selecting/implementing new technology/equipment | 0.606 | |||||
| Professional development opportunities/career ladders | 0.568 | |||||
| Teaching/mentoring opportunities, involvement/challenge of multiple roles | 0.552 | |||||
| Schools | 0.788 | |||||
| Spousal/partner satisfaction | 0.624 | |||||
| Day care | 0.557 | |||||
| Percentage (%) of variance explained | 43.904 | 7.885 | 3.756 | 2.921 | 2.648 | 2.164 |
| Component | Number of Items | Mean Score |
|---|---|---|
| Clinical | 13 | 3.675 |
| Managerial | 3 | 3.483 |
| Practical | 5 | 3.421 |
| Fiscal | 6 | 3.319 |
| Familial | 3 | 3.082 |
| Geographical | 5 | 2.954 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Terry, D.; Peck, B.; Baker, E.; Schmitz, D. The Rural Nursing Workforce Hierarchy of Needs: Decision-Making concerning Future Rural Healthcare Employment. Healthcare 2021, 9, 1232. https://doi.org/10.3390/healthcare9091232
Terry D, Peck B, Baker E, Schmitz D. The Rural Nursing Workforce Hierarchy of Needs: Decision-Making concerning Future Rural Healthcare Employment. Healthcare. 2021; 9(9):1232. https://doi.org/10.3390/healthcare9091232
Chicago/Turabian StyleTerry, Daniel, Blake Peck, Ed Baker, and David Schmitz. 2021. "The Rural Nursing Workforce Hierarchy of Needs: Decision-Making concerning Future Rural Healthcare Employment" Healthcare 9, no. 9: 1232. https://doi.org/10.3390/healthcare9091232
APA StyleTerry, D., Peck, B., Baker, E., & Schmitz, D. (2021). The Rural Nursing Workforce Hierarchy of Needs: Decision-Making concerning Future Rural Healthcare Employment. Healthcare, 9(9), 1232. https://doi.org/10.3390/healthcare9091232







