Use of Computer-Based Scenarios for Clinical Teaching: Impact on Nursing Students’ Decision-Making Skills
Abstract
:1. Introduction
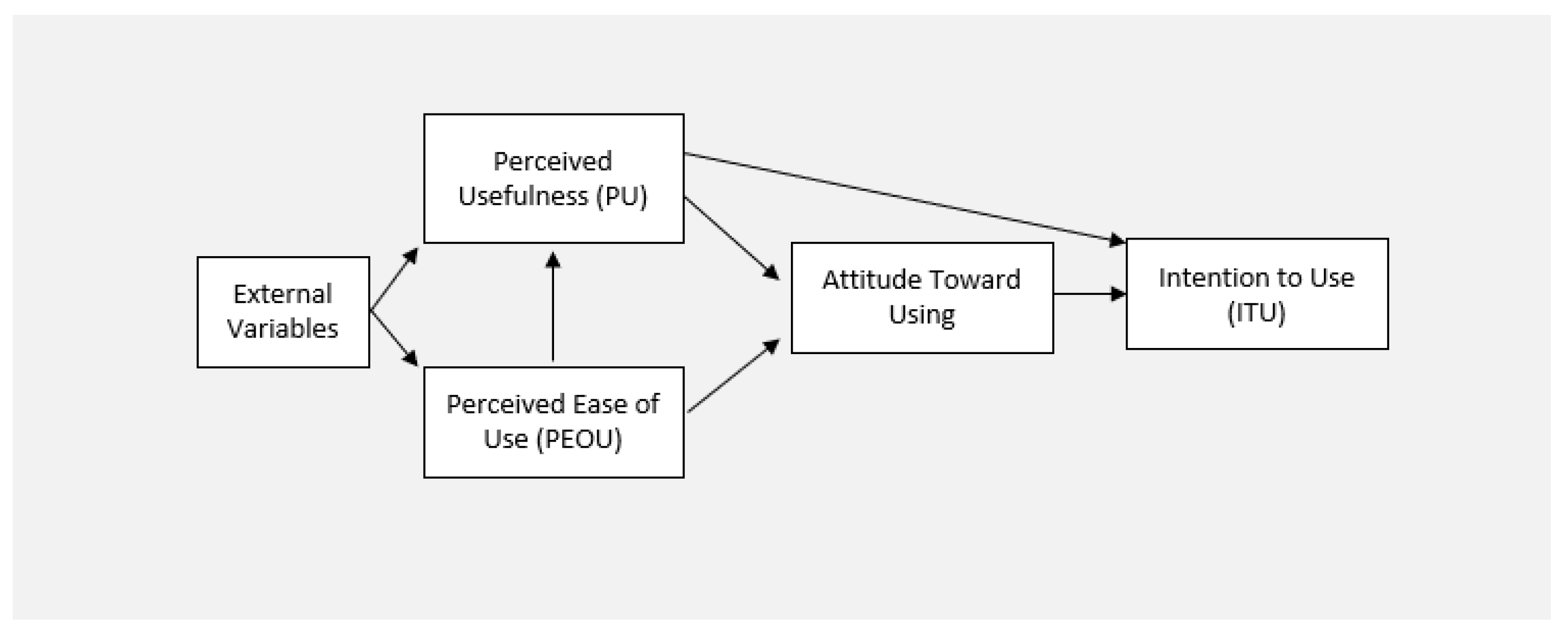
Theoretical Framework
2. Research Questions
- (a)
- What are the scores for the students’ decision-making skills using computer-based and paper-based scenarios?
- (b)
- What is the students’ feedback regarding computer-based scenarios?
3. Materials and Methods
3.1. Research Design
3.2. Setting
3.3. Subjects
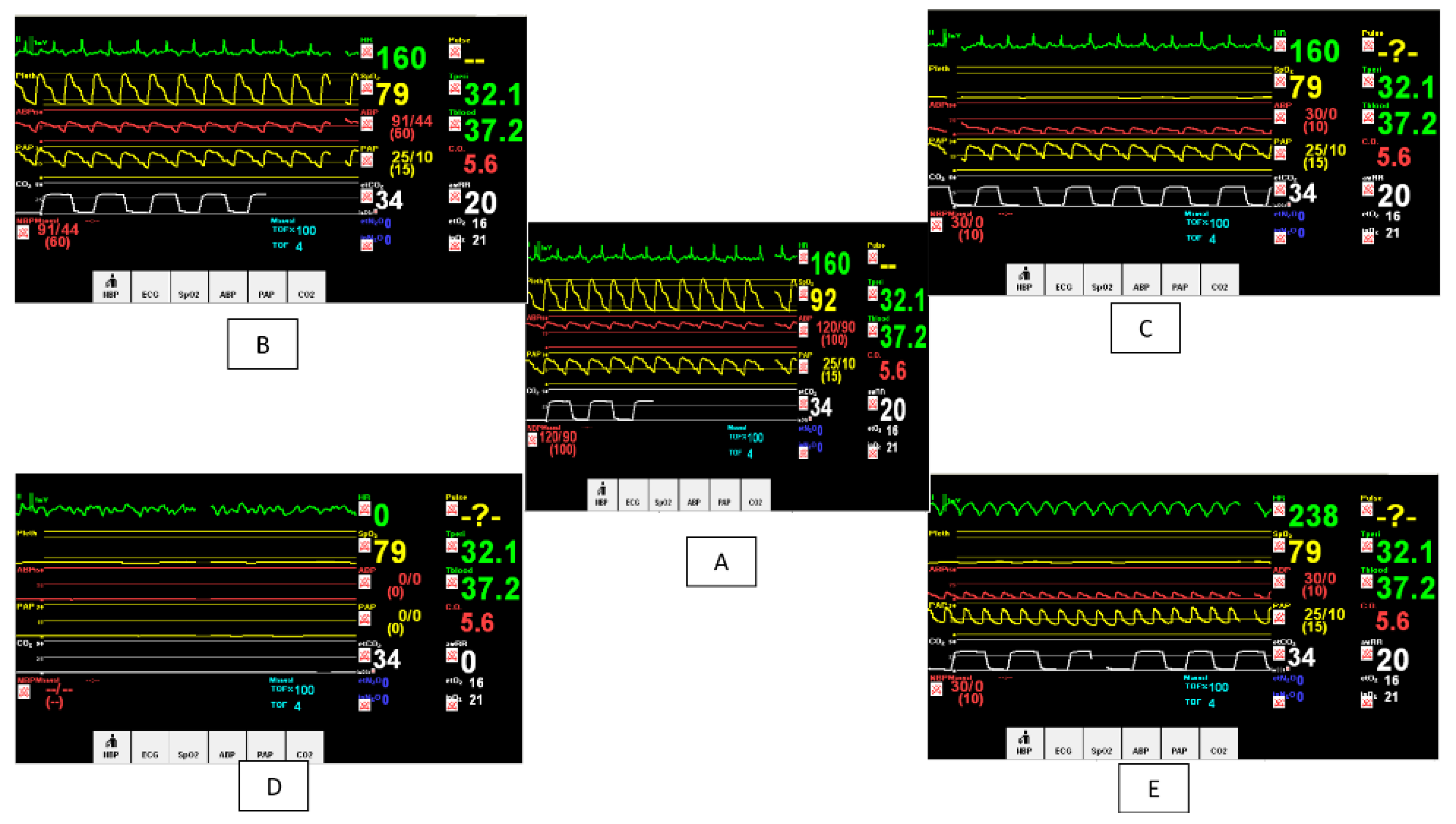
3.4. Tools
3.4.1. Tool I: “Decision Making Skills Worksheet”
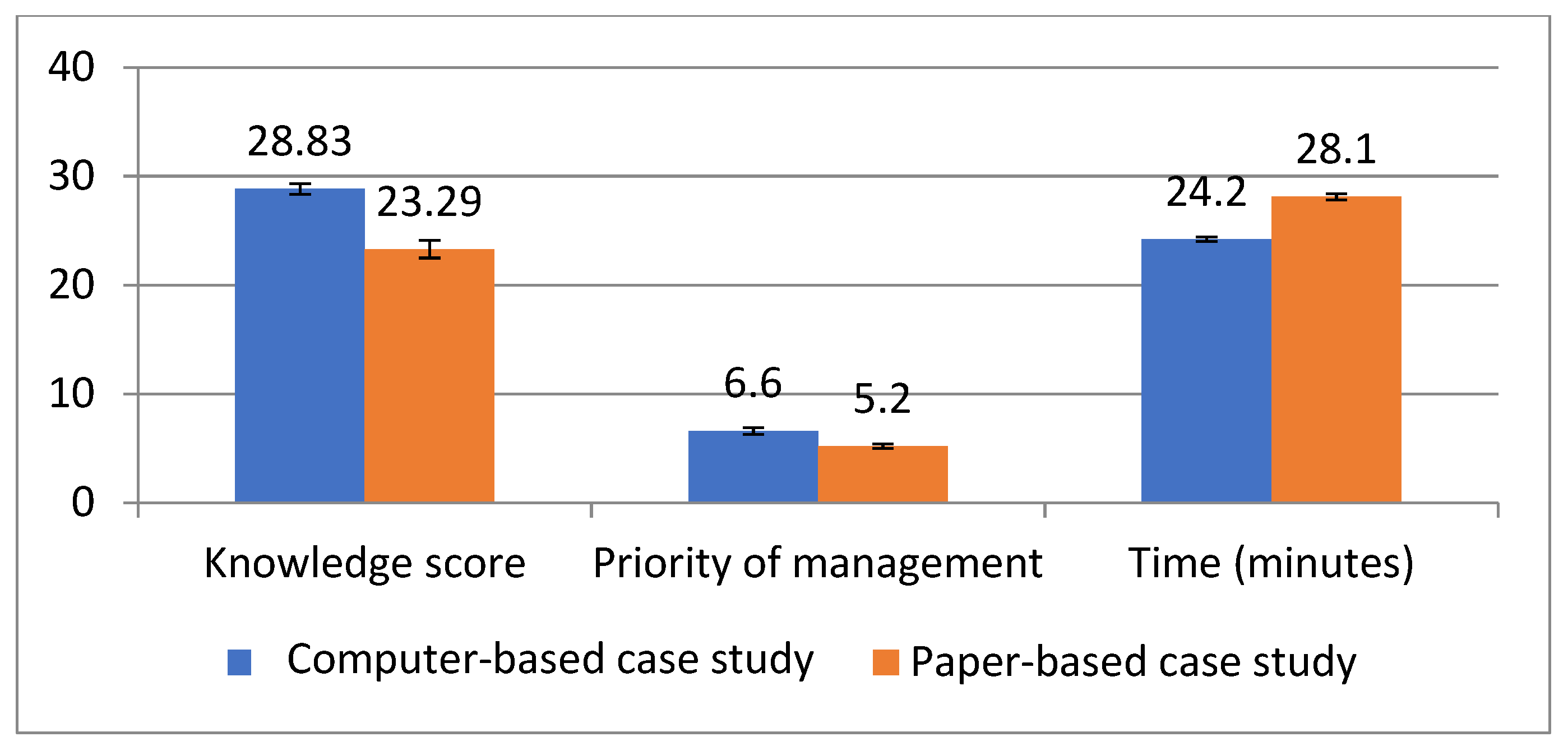
- A knowledge score with a grade given out of 25 (5 marks for each phase).
- The priority of the action: 5 marks for the overall priority of managing the symptoms according to their risk of fatality.
- The speed of response was difficult to determine, especially for the traditional group, so it was decided to evaluate the overall time taken by each student to submit the case study, given a total time of 30 min as the average criterion. One grade was deducted for each one-minute time delay, given a grade out of 10.
3.4.2. Tool II: “Learning Abilities Feedback Questionnaire”
3.5. Procedure
3.5.1. Preliminary Phase
3.5.2. Implementation Phase
3.5.3. Final Phase
4. Results
5. Discussion
6. Limitations of the Study
7. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Harerimana, A.; Mtshali, N.G. Nursing Students’ Perceptions and Expectations Regarding the Use of Technology in Nursing Education. Afr. J. Nurs. Midwifery 2019, 21, 1–20. [Google Scholar] [CrossRef]
- Chernikova, O.; Heitzmann, N.; Stadler, M.; Holzberger, D.; Seidel, T.; Fischer, F. Simulation-Based Learning in Higher Education: A Meta-Analysis. Rev. Educ. Res. 2020, 90, 499–541. [Google Scholar] [CrossRef]
- Padilha, J.M.; Machado, P.P.; Ribeiro, A.; Ramos, J.; Costa, P. Erratum: Correction: Clinical Virtual Simulation in Nursing Education: Randomized Controlled Trial. J. Med. Internet Res. 2019, 21, e11529. [Google Scholar] [CrossRef]
- Kononowicz, A.A.; Woodham, L.A.; Georg, C.; Edelbring, S.; Stathakarou, N.; Davies, D.; Masiello, I.; Saxena, N.; Car, L.T.; Car, J.; et al. Virtual patient simulations for health professional education. Cochrane Database Syst. Rev. 2018. [Google Scholar] [CrossRef]
- Criollo-C, S.; Guerrero-Arias, A.; Jaramillo-Alcázar, Á.; Luján-Mora, S. Mobile Learning Technologies for Education: Benefits and Pending Issues. Appl. Sci. 2021, 11, 4111. [Google Scholar] [CrossRef]
- Nibbelink, C.W.; Brewer, B.B. Decision-making in nursing practice: An integrative literature review. J. Clin. Nurs. 2018, 27, 917–928. [Google Scholar] [CrossRef]
- Atkinson, D. Nursing Observation and Assessment of Patients in the Acute Medical Unit. In Nursing Observation & Assessment of Patients in the Acute Medical Unit; University of Salford: Salford, UK, 2013. [Google Scholar]
- Lesley, M.K. Policy, Pedagogy, and Research: Three Issues Affecting Content Area Literacy Courses for Secondary-Level Teacher Candidates. Lit. Res. Instr. 2013, 53, 50–71. [Google Scholar] [CrossRef]
- Stone, R.; Cooke, M.; Mitchell, M. Undergraduate nursing students’ use of video technology in developing confidence in clinical skills for practice: A systematic integrative literature review. Nurse Educ. Today 2019, 84, 104230. [Google Scholar] [CrossRef] [PubMed]
- Zitzelsberger, H.; Coffey, S.; Graham, L.; Papaconstantinou, E.; Anyinam, C.; Dodd, G.; Mangal, J. Exploring simulation utilization and simulation evaluation practices and approaches in undergraduate nursing education. In Proceedings of the INTED2016 the 10th International Technology, Education and Development Conference, Valencia, Spain, 7–9 March 2016; p. 2279. [Google Scholar] [CrossRef] [Green Version]
- Salameh, B.; Ewais, A.; Salameh, O. Integrating M-Learning in Teaching ECG Reading and Arrhythmia Management for Undergraduate Nursing Students. Int. J. Interact. Mob. Technol. 2020, 14, 82–95. [Google Scholar] [CrossRef] [Green Version]
- Parvan, K.; Hosseini, F.A.; Jasemi, M.; Thomson, B. Attitude of nursing students following the implementation of comprehensive computer-based nursing process in medical surgical internship: A quasi-experimental study. BMC Med. Inform. Decis. Mak. 2021, 21, 1–12. [Google Scholar] [CrossRef]
- Chang, C.-Y.; Kao, C.-H.; Hwang, G.-J.; Lin, F.-H. From experiencing to critical thinking: A contextual game-based learning approach to improving nursing students’ performance in Electrocardiogram training. Educ. Technol. Res. Dev. 2019, 68, 1225–1245. [Google Scholar] [CrossRef]
- Gaba, D.M. The future vision of simulation in health care. Qual. Saf. Health Care 2004, 13, i2–i10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Foronda, C.; MacWilliams, B.; McArthur, E. Interprofessional communication in healthcare: An integrative review. Nurse Educ. Pract. 2016, 19, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Alconero-Camarero, A.; Sarabia-Cobo, C.; Catalán-Piris, M.; González-Gómez, S.; González-López, J. Nursing Students’ Satisfaction: A Comparison between Medium- and High-Fidelity Simulation Training. Int. J. Environ. Res. Public Health 2021, 18, 804. [Google Scholar] [CrossRef]
- Kononowicz, A.A.; Woodham, L.A.; Edelbring, S.; Stathakarou, N.; Davies, D.; Saxena, N.; Car, L.T.; Carlstedt-Duke, J.; Car, J.; Zary, N. Virtual Patient Simulations in Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e14676. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.-M.; Liaw, S.-S. An Analysis of Learners’ Intentions Toward Virtual Reality Learning Based on Constructivist and Technology Acceptance Approaches. Int. Rev. Res. Open Distrib. Learn. 2018, 19. [Google Scholar] [CrossRef] [Green Version]
- Seo, J.H.; Malone, E.; Beams, B.; Pine, M. Toward Constructivist Approach Using Virtual Reality in Anatomy Education. In Digital Anatomy; Springer: Berlin/Heidelberg, Germany, 2021; pp. 343–366. [Google Scholar] [CrossRef]
- Aiello, P.; D’Elia, F.; Di Tore, S.; Sibilio, M. A Constructivist Approach to Virtual Reality for Experiential Learning. E-Learning Digit. Media 2012, 9, 317–324. [Google Scholar] [CrossRef]
- Guze, P.A. Using Technology to Meet the Challenges of Medical Education. Trans. Am. Clin. Climatol. Assoc. 2015, 126, 260–270, PMCID: PMC4530721. [Google Scholar]
- Arrogante, O.; González-Romero, G.M.; López-Torre, E.M.; Carrión-García, L.; Polo, A. Comparing formative and summative simulation-based assessment in undergraduate nursing students: Nursing competency acquisition and clinical simulation satisfaction. BMC Nurs. 2021, 20, 92. [Google Scholar] [CrossRef]
- Buljac-Samardzic, M.; Doekhie, K.D.; Van Wijngaarden, J.D.H. Interventions to improve team effectiveness within health care: A systematic review of the past decade. Hum. Resour. Health 2020, 18, 2. [Google Scholar] [CrossRef] [Green Version]
- La Cerra, C.; Dante, A.; Caponnetto, V.; Franconi, I.; Gaxhja, E.; Petrucci, C.; Alfes, C.M.; Lancia, L. Effects of high-fidelity simulation based on life-threatening clinical condition scenarios on learning outcomes of undergraduate and postgraduate nursing students: A systematic review and meta-analysis. BMJ Open 2019, 9, e025306. [Google Scholar] [CrossRef]
- Saied, H. The Impact of Simulation on Pediatric Nursing Students’ Knowledge, Self-Efficacy, Satisfaction, and Confidence. J. Educ. Pract. 2017, 8, 95–102. [Google Scholar]
- Aljohani, M.S.; Tubaishat, A.; Shaban, I. The effect of simulation experience on Saudi nursing students’ advance cardiac life support knowledge. Int. J. Afr. Nurs. Sci. 2019, 11, 100172. [Google Scholar] [CrossRef]
- Abraham, B.K.; Abdeldafie, S.Y. Attitude of Nursing Students towards Computer Assisted Learning in a Selected Nursing College, Hafar al Batin, Saudi Arabia. Int. J. Innov. Res. Med. Sci. 2017, 2. [Google Scholar] [CrossRef]
- Verkuyl, M.; Betts, L.; Sivaramalingam, S. Nursing Students’ Perceptions Using an Interactive Digital Simulation Table: A Usability Study. Simul. Gaming 2019, 50, 202–213. [Google Scholar] [CrossRef]
- Awad, M.S.; Abdullah, M.K.; Ibrahim, R.; Abdulla, R.K. Nursing Students’ Attitudes toward Simulation Technology in Nursing Education. Int. J. Emerg. Technol. Learn. 2019, 14, 31–45. [Google Scholar] [CrossRef] [Green Version]
- Choi, H.; Lee, U.; Jeon, Y.S.; Kim, C. Efficacy of the computer simulation-based, interactive communication education program for nursing students. Nurse Educ. Today 2020, 91, 104467. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, W.A.; Kulikowich, J.M. Online Learning Self-Efficacy in Students with and Without Online Learning Experience. Am. J. Distance Educ. 2016, 30, 180–191. [Google Scholar] [CrossRef]
- Guglielmino, L.M. Development of the Self-Directed Learning Readiness Scale. Ph.D. Thesis, University of Georgia, Athens, GA, USA, 1978. [Google Scholar]
- Chang, Y.M.; Lai, C.L. Exploring the experiences of nursing students in using immersive virtual reality to learn nursing skills. Nurse Educ. Today 2020, 97, 104670. [Google Scholar] [CrossRef]
- Abdelhafez, A.I.; Elcokany, N.M.; Ghaly, A.S.; Akhter, F. Learning Environment Stressors and Coping Styles among Nursing Students. Int. J. Nurs. Educ. 2021, 12. [Google Scholar] [CrossRef]
- Alfaro-LeFevre, R. Nursing Process and Clinical Reasoning. Nurs. Educ. Perspect. 2012, 33, 7. [Google Scholar] [CrossRef]
- Pritchard, M. Making effective clinical decisions: A framework for nurse practitioners. Br. J. Nurs. 2006, 15, 128–130. [Google Scholar] [CrossRef]
- Lambie, A.; Schwend, K.; Scholl, A. Utilization of the Nursing Process to Foster Clinical Reasoning During a Simulation Experience. SAGE Open 2015, 5, 2158244015617516. [Google Scholar] [CrossRef] [Green Version]
- Hamilton, C.L. Progression of Clinical Self-Efficacy Among Baccalaureate Nursing Students. In Walden Dissertations and Doctoral Studies Collection; Walden University: Minneapoli, MN, USA, 2018; Volume 4. [Google Scholar]
- Valencia-Vallejo, N.; López-Vargas, O.; Sanabria-Rodríguez, L. Self-Efficacy in Computer-Based Learning Environments: A Bibliometric Analysis. Psychology 2016, 7, 1839–1857. [Google Scholar] [CrossRef] [Green Version]
- Moos, D.C.; Azevedo, R. Learning With Computer-Based Learning Environments: A Literature Review of Computer Self-Efficacy. Rev. Educ. Res. 2009, 79, 576–600. [Google Scholar] [CrossRef] [Green Version]
- Harding, M.M.; Snyder, J.S.; Barbara, A. Preusser Winningham and Preusser’s Critical Thinking Cases in Nursing: Medical-Surgical, Pediatric, Maternity, and Psychiatric Case Studies; Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Darling-Hammond, L.; Flook, L.; Cook-Harvey, C.; Barron, B.; Osher, D. Implications for educational practice of the science of learning and development. Appl. Dev. Sci. 2019, 24, 97–140. [Google Scholar] [CrossRef] [Green Version]
- Kiernan, L.C. Evaluating competence and confidence using simulation technology. Nursing 2018, 48, 45–52. [Google Scholar] [CrossRef]
- Foronda, C.L.; Fernandez-Burgos, M.; Nadeau, C.; Kelley, C.N.; Henry, M.N. Virtual Simulation in Nursing Education: A Systematic Review Spanning 1996 to 2018. Simul. Health J. Soc. Simul. Health 2020, 15, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Haowen, J.; Vimalesvaran, S.; Kyaw, B.M.; Car, L.T. Virtual reality in medical students’ education: A scoping review protocol. BMJ Open 2021, 11, e046986. [Google Scholar] [CrossRef] [PubMed]
- Cobbett, S.; Snelgrove-Clarke, E. Virtual versus face-to-face clinical simulation in relation to student knowledge, anxiety, and self-confidence in maternal-newborn nursing: A randomized controlled trial. Nurse Educ. Today 2016, 45, 179–184. [Google Scholar] [CrossRef]
- William, A.; Vidal, V.L.; John, P. Traditional Instruction versus Virtual Reality Simulation: A Comparative Study of Phlebotomy Training among Nursing Students in Kuwait. J. Educ. Pract. 2016, 7, 18–25. [Google Scholar]
- Sattar, M.U.; Palaniappan, S.; Lokman, A.; Hassan, A.; Shah, N.; Riaz, Z. Effects of Virtual Reality training on medical students’ learning motivation and competency. Pak. J. Med. Sci. 2019, 35, 852–857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hannans, J.; Nevins, C. Transitioning to Online Facilitation of Immersive vr Simulations; DeNoyelles, A.A., Albrecht, S., Bauer, Wyatt, S., Eds.; Available online: https://topr.online.ucf.edu/transitioning-to-online-facilitation-of-immersive-vr-simulations/ (accessed on 5 August 2021).
- Bliss, M.; Aitken, L.M. Does simulation enhance nurses’ ability to assess deteriorating patients? Nurse Educ. Pr. 2018, 28, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.-Q.; Leng, Y.-F.; Ge, J.-F.; Wang, D.-W.; Li, C.; Chen, B.; Sun, Z.-L. Effectiveness of Virtual Reality in Nursing Education: Meta-Analysis. J. Med. Internet Res. 2020, 22, e18290. [Google Scholar] [CrossRef]
- Vlachopoulos, D.; Makri, A. The effect of games and simulations on higher education: A systematic literature review. Int. J. Educ. Technol. High. Educ. 2017, 14, 22. [Google Scholar] [CrossRef]
- Curtin, L.B.; Finn, L.A.; Czosnowski, Q.A.; Whitman, C.B.; Cawley, M.J. Computer-based Simulation Training to Improve Learning Outcomes in Mannequin-based Simulation Exercises. Am. J. Pharm. Educ. 2011, 75, 113. [Google Scholar] [CrossRef]
- Campos, N.; Nogal, M.; Caliz, C.; Juan, A.A. Simulation-based education involving online and on-campus models in different European universities. Int. J. Educ. Technol. High. Educ. 2020, 17, 8. [Google Scholar] [CrossRef] [Green Version]
- Saab, M.M.; Landers, M.; Murphy, D.; O’Mahony, B.; Cooke, E.; O’Driscoll, M.; Hegarty, J. Nursing students’ views of using virtual reality in healthcare: A qualitative study. J. Clin. Nurs. 2021. [Google Scholar] [CrossRef]
| Feedback of Learning Abilities | Computer-Based Case Study | |
|---|---|---|
| No. of Students with Positive Feedback (SA and A) | No. of Students with Negative Feedback (SD and D) | |
| No. (%) | No. (%) | |
| General Learning Abilities | ||
| Increasing motivation for learning | 74 (94.4%) | 4 (5.1%) |
| Demonstrating clinical reasoning skills | 73 (94.6%) | 5 (5.4%) |
| Authentication of learning | 72 (92.3%) | 6 (7.7%) |
| Enhancing fast decision-making | 77 (98.7%) | 1 (1.3%) |
| Application of class-gained learning | 75 (96.1%) | 3 (3.9%) |
| Not yielding feeling of stress and nervousness | 77 (98.7%) | 1 (1.3%) |
| Empowering control over learning | 77 (98.7%) | 1 (1.3%) |
| Increasing self-confidence in problem-solving and decision-making abilities | 75 (96.1%) | 3 (3.9%) |
| Not yielding the feeling of being lost | 77 (98.7%) | 1 (1.3%) |
| Nursing-Specific Abilities | ||
| Deepening of knowledge about medical diagnosis and nursing case management | 76 (97.4%) | 2 (2.6%) |
| Improving understanding of the complexity of nursing care | 75 (96.1%) | 3 (3.9%) |
| Gaining understanding of future professional role | 75 (96.1%) | 3 (3.9%) |
| Increasing critical analysis and ability to reach nursing diagnosis | 77 (98.7%) | 1 (1.3%) |
| Prioritizing nursing diagnosis scientifically | 76 (97.4%) | 2 (2.6%) |
| Individualizing each case nursing interventions | 76 (97.4%) | 2 (2.6%) |
| Fostering patient response evaluation | 77 (98.7%) | 1 (1.3%) |
| Linkage of concepts and principles from nursing and other sciences in clinical decision-making | 76 (97.4%) | 2 (2.6%) |
| Recognizing patient deterioration early | 72 (92.3%) | 6 (7.7%) |
| Understanding the individual’s entire complex situation | 77 (98.7%) | 1 (1.3%) |
| Recognizing holistic perspective of the patient’s life world | 75 (96.1%) | 3 (3.9%) |
| Total Feedback Score | Mean | SD | t-Test (p) |
|---|---|---|---|
| General learning abilities | 3.16 | 0.26 | 88 (0 *) |
| Nursing-specific abilities | 3.71 | 0.37 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elcokany, N.M.; Abdelhafez, A.I.; Samuel Sharaby, V.M.; Belal, S. Use of Computer-Based Scenarios for Clinical Teaching: Impact on Nursing Students’ Decision-Making Skills. Healthcare 2021, 9, 1228. https://doi.org/10.3390/healthcare9091228
Elcokany NM, Abdelhafez AI, Samuel Sharaby VM, Belal S. Use of Computer-Based Scenarios for Clinical Teaching: Impact on Nursing Students’ Decision-Making Skills. Healthcare. 2021; 9(9):1228. https://doi.org/10.3390/healthcare9091228
Chicago/Turabian StyleElcokany, Nermine M., Amal Ismael Abdelhafez, Vivian Magdi Samuel Sharaby, and Safia Belal. 2021. "Use of Computer-Based Scenarios for Clinical Teaching: Impact on Nursing Students’ Decision-Making Skills" Healthcare 9, no. 9: 1228. https://doi.org/10.3390/healthcare9091228
APA StyleElcokany, N. M., Abdelhafez, A. I., Samuel Sharaby, V. M., & Belal, S. (2021). Use of Computer-Based Scenarios for Clinical Teaching: Impact on Nursing Students’ Decision-Making Skills. Healthcare, 9(9), 1228. https://doi.org/10.3390/healthcare9091228







