Diagnostic Effect of Consultation Referral from Gastroenterologists to Generalists in Patients with Undiagnosed Chronic Abdominal Pain: A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
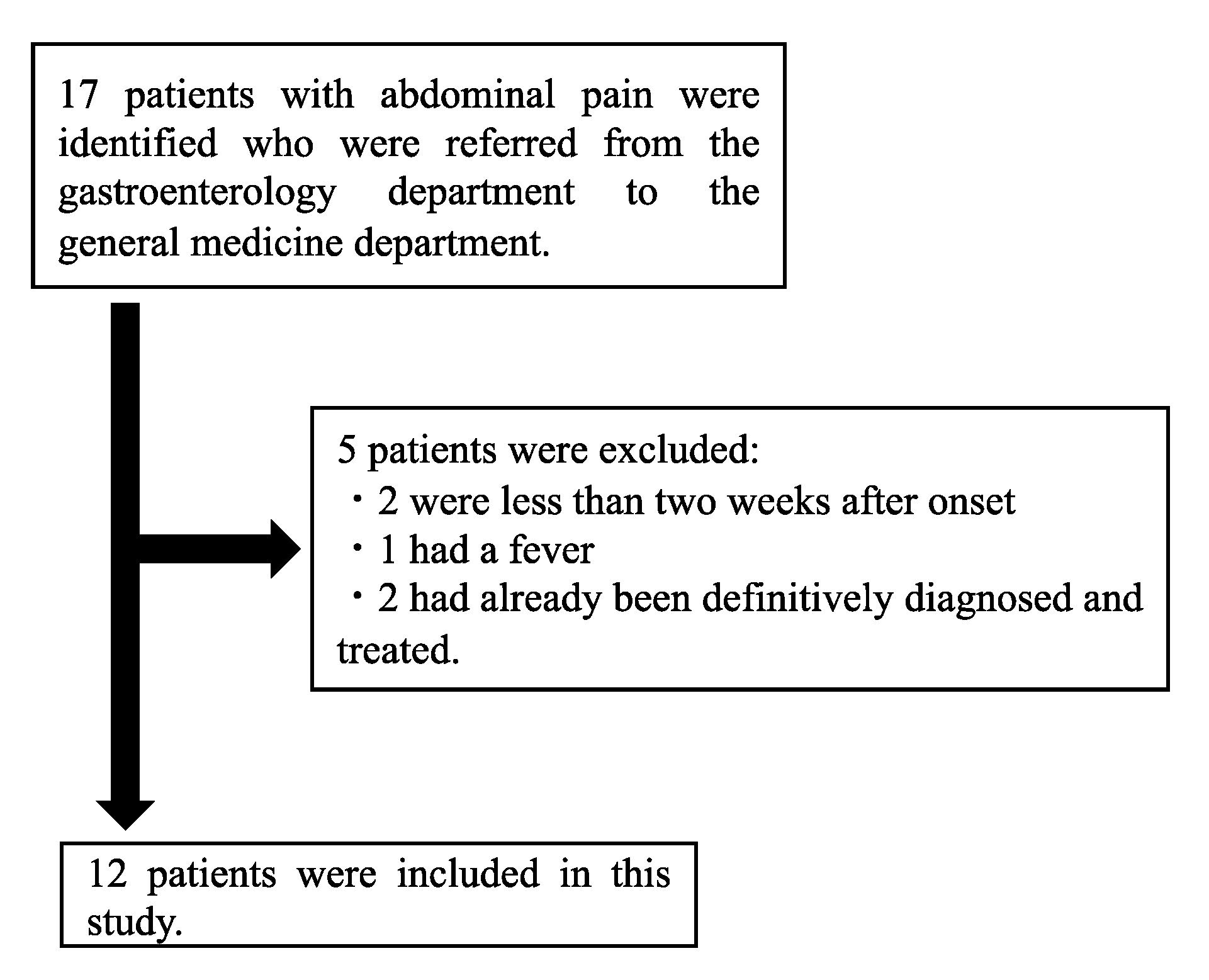
2.1. Study Design, Setting, and Subjects
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Patient Backgrounds
3.2. Diagnostic Examinations and Diagnoses at the Department of Gastroenterology
3.3. Diagnostic Examinations and Diagnoses at the Department of Diagnostic and Gereralists Medicine
3.4. Treatments and Follow Up
3.5. Abdominal Wall Pain vs. Nonabdominal Wall Pain
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Pichetshote, N.; Pimentel, M. An Approach to the Patient with Chronic Undiagnosed Abdominal Pain. Am. J. Gastroenterol. 2019, 114, 726–732. [Google Scholar] [CrossRef]
- Burger, P.M.; Westerink, J.; Vrijsen, B.E.L. Outcomes of Second Opinions in General Internal Medicine. PLoS ONE 2020, 15, e0236048. [Google Scholar] [CrossRef]
- Srinivasan, R. Chronic Abdominal Wall Pain: A Frequently Overlooked Problem. Am. J. Gastroenterol. 2002, 97, 824–830. [Google Scholar] [PubMed]
- Glissen Brown, J.R.; Bernstein, G.R.; Friedenberg, F.K.; Ehrlich, A.C. Chronic Abdominal Wall Pain: An Under-Recognized Diagnosis Leading to Unnecessary Testing. J. Clin. Gastroenterol. 2016, 50, 828–835. [Google Scholar] [CrossRef]
- Costanza, C. Chronic Abdominal Wall Pain: Clinical Features, Health Care Costs, and Long-Term Outcome. Clin. Gastroenterol. Hepatol. 2004, 2, 395–399. [Google Scholar] [CrossRef]
- Dancer, S.J.; Macpherson, S.G.; de Beaux, A.C. Protracted Diagnosis of ACNES: A Costly Exercise. J. Surg. Case Rep. 2018, 2018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mol, F.M.U.; Maatman, R.C.; De Joode, L.E.G.H.; Van Eerten, P.; Scheltinga, M.R.; Roumen, R. Characteristics of 1116 Consecutive Patients Diagnosed with Anterior Cutaneous Nerve Entrapment Syndrome (ACNES). Ann. Surg. 2021, 273, 373–378. [Google Scholar] [CrossRef] [PubMed]
- van Assen, T.; de Jager-Kievit, J.W.A.J.; Scheltinga, M.R.; Roumen, R.M.H. Chronic Abdominal Wall Pain Misdiagnosed as Functional Abdominal Pain. J. Am. Board Fam. Med. 2013, 26, 738–744. [Google Scholar] [CrossRef]
- Kasick, R.T.; Melvin, J.E.; Perera, S.T.; Perry, M.F.; Black, J.D.; Bode, R.S.; Groner, J.I.; Kersey, K.E.; Klamer, B.G.; Bai, S.; et al. A Diagnostic Time-out to Improve Differential Diagnosis in Pediatric Abdominal Pain. Diagnosis 2021, 8, 209–217. [Google Scholar] [CrossRef]
- Sam, K.M. Deformation Professionnelle Bias. In Decision Making in Emergency Medicine: Biases, Errors and Solutions; Raz, M., Pouryahya, P., Eds.; Springer: Singapore, 2021; pp. 111–116. ISBN 9789811601439. [Google Scholar]
- Suleiman, S. The Abdominal Wall: An Overlooked Source of Pain. Am. Fam. Physician 2001, 64, 431–438. [Google Scholar] [PubMed]
- Kamboj, A.K.; Hoversten, P.; Oxentenko, A.S. Chronic Abdominal Wall Pain: A Common Yet Overlooked Etiology of Chronic Abdominal Pain. Mayo Clin. Proc. 2019, 94, 139–144. [Google Scholar] [CrossRef] [Green Version]
- Gray, D.W.; Dixon, J.M.; Seabrook, G.; Collin, J. Is Abdominal Wall Tenderness a Useful Sign in the Diagnosis of Non-Specific Abdominal Pain? Ann. R. Coll. Surg. Engl. 1988, 70, 233–234. [Google Scholar]
- Thomson, H.; Francis, D.M.A. Abdominal-wall tenderness: A useful sign in the acute abdomen. Lancet 1977, 310, 1053–1054. [Google Scholar] [CrossRef]
- Hall, P.N.; Lee, A.P.B. Rectus Nerve Entrapment Causing Abdominal Pain. Br. J. Surg. 1988, 75, 917. [Google Scholar] [CrossRef] [PubMed]
- Sweetser, S. Abdominal Wall Pain: A Common Clinical Problem. Mayo Clin. Proc. 2019, 94, 347–355. [Google Scholar] [CrossRef] [Green Version]
- Greenbaum, D.S.; Greenbaum, R.B.; Joseph, J.G.; Natale, J.E. Chronic Abdominal Wall Pain. Diagnostic Validity and Costs. Dig. Dis. Sci. 1994, 39, 1935–1941. [Google Scholar] [CrossRef] [PubMed]
- Naimer, S.A. Abdominal Cutaneous Nerve Entrapment Syndrome: The Cause of Localized Abdominal Pain in a Young Pregnant Woman. J. Emerg. Med. 2018, 54, e87–e90. [Google Scholar] [CrossRef] [PubMed]
- Koop, H.; Koprdova, S.; Schürmann, C. Chronic Abdominal Wall Pain: A Poorly Recognized Clinical Problem. Dtsch. Aerzteblatt Online 2016, 113, 51. [Google Scholar] [CrossRef] [Green Version]
- Singla, M.; Laczek, J.T. A Stick and a Burn: Our Approach to Abdominal Wall Pain. Am. J. Gastroenterol. 2020, 115, 645–647. [Google Scholar] [CrossRef] [PubMed]
- Takada, T.; Ikusaka, M.; Ohira, Y.; Noda, K.; Tsukamoto, T. Diagnostic Usefulness of Carnett’s Test in Psychogenic Abdominal Pain. Intern. Med. 2011, 50, 213–217. [Google Scholar] [CrossRef] [Green Version]
- Msonda, H.T.; Laczek, J.T. Medical Evacuation for Unrecognized Abdominal Wall Pain: A Case Series. Mil. Med. 2015, 180, e605–e607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindsetmo, R.-O.; Stulberg, J. Chronic Abdominal Wall Pain—A Diagnostic Challenge for the Surgeon. Am. J. Surg. 2009, 198, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Shian, B.; Larson, S.T. Abdominal Wall Pain: Clinical Evaluation, Differential Diagnosis, and Treatment. Am. Fam. Physician 2018, 98, 429–436. [Google Scholar] [PubMed]

| Case #Age Sex | Duration of Symptoms | Number of Medical Institutions | Presenting Features | Diagnostic Workups, Working Diagnoses, and Treatments before Referral to Generalists | Additional Diagnostic Workups, Revised Diagnosis, Treatments, and Outcome after Referral to Generalists |
|---|---|---|---|---|---|
| 1 71 F | More than 10 years | 3 | Epigastric pain with back pain. Not related to eating or posture. Tenderness of the xiphoid process. | Workups: Labs, CT, EGD Diagnosis: Functional dyspepsia Treatments: Acotiamide hydrochloride hydrate, Chinese herbal medicine (Rikkunshito) | Additional workups: None Diagnosis: Xiphoidynia Treatments: NSAIDs Outcome: Symptoms did not improve during 6-week follow up |
| 2 66 F | 1 year | 2 | Left flank pain with back pain. Not related to eating or posture. Tenderness of lateral edge of the left rectus abdominis and left erector spinae. Positive Carnett’s sign. | Workups: Labs, CT (twice), MRCP (twice), ultrasound (twice), EGD, colonoscopy Diagnosis: functional dyspepsia Treatments: Acotiamide hydrochloride hydrate | Additional workups: Thoracic spinal MRI Diagnosis: ACNES. Treatments: Acetaminophen, NSAIDs, eperisone hydrochloride, tender point infiltrations. Outcome: Symptoms did not improve during 5-week follow up |
| 3 86 F | 10 years | Unidentified | Left lower quadrant pain. Exacerbated by getting up and straining. Very localized tenderness in the left lower quadrant. Positive Carnett’s sign. | Workups: Labs, CT, MRCP, EGD (twice), colonoscopy (twice) Diagnosis: None Treatments: Acetaminophen, NSAIDs, pregabalin | Additional workups: None Diagnosis: ACNES Treatments: Exercise Outcome: No follow up |
| 4 73 M | 2 years | Unidentified | Epigastric squeezing pain. No tenderness. Not related to eating. Negative Carnett’s sign. | Workups: Labs, CT, EGD, colonoscopy Diagnosis: None Treatments: Laxatives | Additional workups: Lumber spinal MRI Diagnosis: None Treatments: None Outcome: Symptom persisted for 3 years |
| 5 69 M | 1 year | 2 | Right upper quadrant pain. Induced by twisting the body to the left. | Workups: Labs, ultrasound, CT, EGD Diagnosis: Functional dyspepsia Treatments: Acotiamide hydrochloride hydrate, esomeprazole, magnesium hydrate | Additional workups: None Diagnosis: Myofascial pain Treatments: None Outcome: No follow up |
| 6 45 F | 1 year | 1 | Left upper quadrant pain with headache and stiff shoulders. Exacerbated by prolonged sitting. Tenderness in left 12th rib. | Workups: Labs, ultrasound, EGD Diagnosis: Functional dyspepsia, GERD Treatments: Acotiamide hydrochloride hydrate, Chinese herbal medicine (Rikkunshito), vonoprazan fumarate | Additional workups: None Diagnosis: Iron deficiency Treatments: Iron supplementation Outcome: Symptoms improved after 1 month |
| 7 19 M | 2–3 years | 1 | Epigastric and left lower quadrant pain with tenderness. Gradual onset. Not related to eating. Pain did not occur in the supine position. Negative Carnett’s sign. | Workups: Labs, ultrasound, CT, EGD Diagnosis: Functional dyspepsia Treatments: Acotiamide hydrochloride hydrate, esomeprazole, magnesium hydrate, dimethicone | Additional workups: None Diagnosis: None Treatments: None Outcome: Symptoms did not improve during 2-week follow up |
| 8 68 F | 4.5 years | 2 | Lower abdominal dull pain with tenderness. Gradual onset. | Workups: Labs, ultrasound, CT, EGD, colonoscopy, PET-CT Diagnosis: Functional dyspepsia Treatments: Acotiamide hydrochloride hydrate, esomeprazole, magnesium hydrate | Additional workups: None Diagnosis: Chronic pelvic pain Treatments: Pregabalin and magnesium oxide Outcome: No visits after 1-year follow up |
| 9 76 M | 10 years | 1 | Left abdominal pain. Not related to eating or posture. Tenderness 5 cm outside the navel. Positive Carnett’s sign. | Workups: Labs, CT, EGD, colonoscopy Diagnosis: None Treatments: None | Additional workups: Cervical and thoracic spinal MRI Diagnosis: ACNES. Treatments: Tender point infiltrations and neurectomy Outcome: Initial symptom improved but some other pain occurred |
| 10 15 M | 7 months | 2–3 | Lower abdominal pain with tenderness. Acute onset. Not related to eating or posture. No tenderness. | Workups: Labs, CT, colonoscopy Diagnosis: Irritable bowel syndrome Treatments: NSAIDs, tramadol hydrochloride, acetaminophen, ramosetron hydrochloride, escitalopram oxalate, sulpiride | Additional workups: Labs Diagnosis: None Treatments: Acetaminophen Outcome: Symptoms did not improve during 3-week follow up |
| 11 23 M | 3 months | 2 | Left upper quadrant pain with left back pain and heartburn. Acute onset. Exacerbated by eating. | Workups: Labs, abdominal X-ray, CT, EGD, colonoscopy Diagnosis: GERD, functional dyspepsia, irritable bowel syndrome Treatments: Vonoprazan fumarate, acotiamide hydrochloride hydrate, trimebutine maleate | Additional workups: None Diagnosis: None (suspicious of superior mesenteric artery syndrome) Treatments: Increasing calorie intake Outcome: No visits after 1-month follow up |
| 12 40 M | 2 weeks | 2 | Right flank tingling pain to the back. Acute onset. Not related to eating.No skin rash. Negative Carnett’s sign. | Workups: Labs, CT Diagnosis: None Treatments: Acetaminophen and pregabalin | Additional workups: None Diagnosis: Herpes zoster Treatments: Increasing the dose of acetaminophen. Outcome: No follow up |
| Abdominal Wall Pain | Nonabdominal Wall Pain | p Value * | |
|---|---|---|---|
| Age (years) | 70 (66.75–74.75) | 34 (20–62.25) | 0.09 |
| Male | 3/6 (50%) | 4/6 (66.7%) | >0.99 |
| Period of illness (months) | 66 (12–120) | 18 (8.25–28.5) | 0.46 |
| Number of visited medical institutions | 2 (2–2) | 2 (1–2) | 0.40 |
| Characteristics of abdominal pain | |||
| Related to eat | Yes: 0/6 (0%) No: 4/6 (66.7%) Unknown: 2/6 (33.3%) | Yes: 1/6 (16.7%) No: 3/6 (50.0%) Unknown: 2/6 (33.3%) | >0.99 |
| Related to postures | Yes: 2/6 (33.3%) No: 3/6 (50.0%) Unknown: 1/6 (16.7%) | Yes: 2/6 (33.3%) No: 1/6 (16.7%) Unknown: 3/6 (50.0%) | 0.77 |
| Tests conducted | |||
| Labs | 6/6 (100%) | 6/6 (100%) | |
| Ultrasound | 2/6 (33.3%) | 3/6 (50.0%) | |
| Abdominal X-ray | 0/6 (0%) | 1/6 (16.7%) | |
| MRCP | 2/6 (33.3%) | 0/6 (0%) | |
| EGD | 5/6 (83.3%) | 5/6 (83.3%) | |
| Colonoscopy | 3/6 (50.0%) | 4/6 (66.7%) | |
| Tentative diagnosis before referral | 0.55 | ||
| Functional dyspepsia | 3/6 (50.0%) | 4/6 (66.7%) | |
| GERD | 0/6 (0%) | 2/6 (33.3%) | |
| Irritable bowel syndrome | 0/6 (0%) | 2/6 (33.3%) | |
| None | 3/6 (50.0%) | 0/6 (0%) | |
| Carnett’s sign | 0.32 | ||
| Positive | 3/6 (50.0%) | 0/6 (0%) | |
| Negative | 1/6 (16.7%) | 2/6 (33.3%) | |
| Unknown | 2/6 (33.3%) | 4/6 (66.7%) | |
| Final diagnosis | ACNES: 3/6 (50.0%) Myofascial pain: 1/6 (16.7%) Xiphoidynia: 1/6 (16.7%) Herpes zoster: 1/6 (16.7%) | Chronic pelvic pain: 1/6 (16.7%) Iron deficiency: 1/6 (16.7%) Unknown: 4/6 (66.7%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawamura, R.; Harada, Y.; Shimizu, T. Diagnostic Effect of Consultation Referral from Gastroenterologists to Generalists in Patients with Undiagnosed Chronic Abdominal Pain: A Retrospective Study. Healthcare 2021, 9, 1150. https://doi.org/10.3390/healthcare9091150
Kawamura R, Harada Y, Shimizu T. Diagnostic Effect of Consultation Referral from Gastroenterologists to Generalists in Patients with Undiagnosed Chronic Abdominal Pain: A Retrospective Study. Healthcare. 2021; 9(9):1150. https://doi.org/10.3390/healthcare9091150
Chicago/Turabian StyleKawamura, Ren, Yukinori Harada, and Taro Shimizu. 2021. "Diagnostic Effect of Consultation Referral from Gastroenterologists to Generalists in Patients with Undiagnosed Chronic Abdominal Pain: A Retrospective Study" Healthcare 9, no. 9: 1150. https://doi.org/10.3390/healthcare9091150
APA StyleKawamura, R., Harada, Y., & Shimizu, T. (2021). Diagnostic Effect of Consultation Referral from Gastroenterologists to Generalists in Patients with Undiagnosed Chronic Abdominal Pain: A Retrospective Study. Healthcare, 9(9), 1150. https://doi.org/10.3390/healthcare9091150







