The Impact of Public Reporting Schemes and Market Competition on Hospital Efficiency
Abstract
1. Introduction
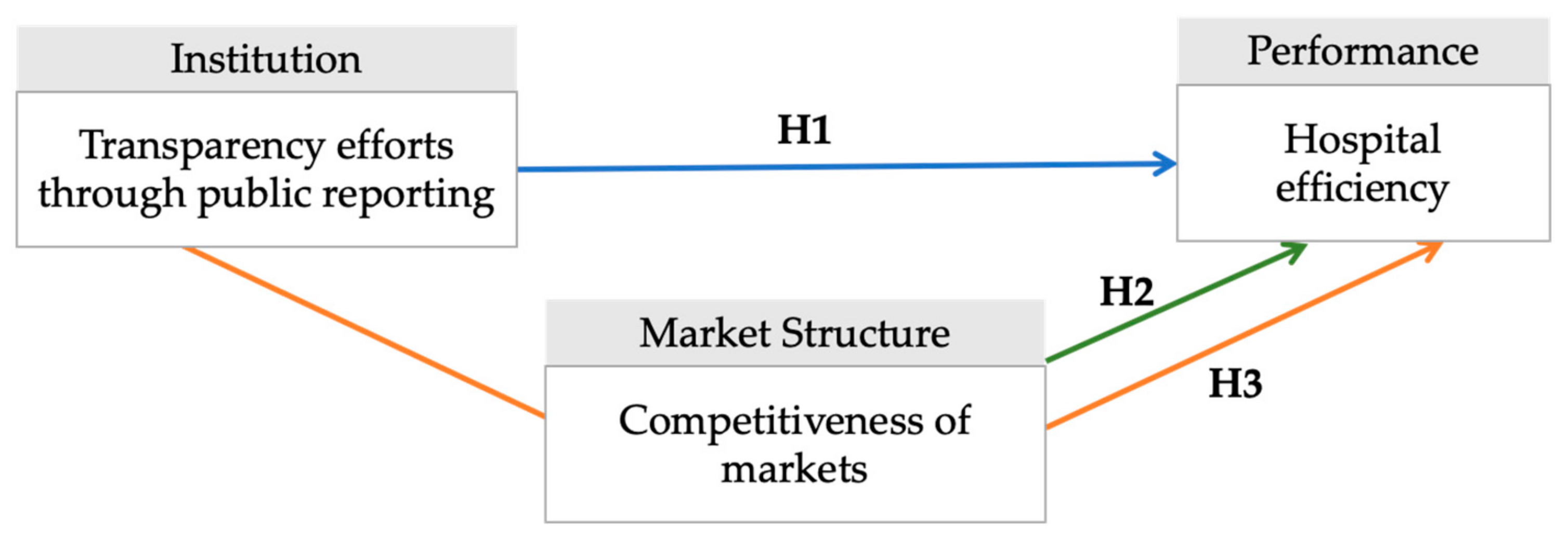
1.1. The Impact of Transparency on Hospital Efficiency
1.2. The Impact of Competition on Hospital Efficiency
1.3. The Impact of Transparency and Competition on Hospital Efficiency
2. Methods
2.1. Sample and Data Sources
2.2. Model Specification
2.3. Measures
2.3.1. Technical Efficiency
2.3.2. Transparent Environments
2.3.3. Market Competition Measures
2.3.4. Control Variables
3. Results
3.1. Descriptive Analysis
3.2. Data Envelopment Analysis of Technical Efficiency Results
3.3. Cross-Sectional Time-Series Tobit Regression Analysis Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kordzadeh, N. Toward Quality Transparency in Healthcare: Exploring Hospital-Operated Online Physician Review Systems in Northeastern United States. Health Policy Technol. 2020, 9, 56–61. [Google Scholar] [CrossRef]
- Lindenauer, P.K.; Lagu, T.; Ross, J.S.; Pekow, P.S.; Shatz, A.; Hannon, N.; Rothberg, M.B.; Benjamin, E.M. Attitudes of Hospital Leaders toward Publicly Reported Measures of Health Care Quality. JAMA Intern. Med. 2014, 174, 1904–1911. [Google Scholar] [CrossRef] [PubMed]
- Berwick, D.M.; Nolan, T.W.; Whittington, J. The Triple Aim: Care, Health, and Cost. Health Aff. 2008, 27, 759–769. [Google Scholar] [CrossRef] [PubMed]
- Hut, N. CMS Is Preparing to Make Noncompliance with Price Transparency Requirements Much More Expensive; Healthcare Financial Management Association: Westchester, IL, USA, 2021. [Google Scholar]
- Burstin, H.; Leatherman, S.; Goldmann, D. The Evolution of Healthcare Quality Measurement in the United States. J. Intern. Med. 2016, 279, 154–159. [Google Scholar] [CrossRef]
- Panzer, R.J.; Gitomer, R.S.; Greene, W.H.; Webster, P.R.; Landry, K.R.; Riccobono, C.A. Increasing Demands for Quality Measurement. JAMA 2013, 310, 1971–1980. [Google Scholar] [CrossRef]
- Dehmer, G.J.; Drozda, J.P.; Brindis, R.G.; Masoudi, F.A.; Rumsfeld, J.S.; Slattery, L.E.; Oetgen, W.J. Public Reporting of Clinical Quality Data: An Update for Cardiovascular Specialists. J. Am. Coll. Cardiol. 2014, 63, 1239–1245. [Google Scholar] [CrossRef]
- Elrod, J.K.; Fortenberry, J.L. Centers of Excellence in Healthcare Institutions: What They Are and How to Assemble Them. BMC Health Serv Res 2017, 17, 425. [Google Scholar] [CrossRef]
- Fulton, L.V.; Lasdon, L.S.; McDaniel, R.R.; Coppola, N. Including Quality, Access, and Efficiency in Healthcare Cost Models. Hosp. Top. 2008, 86, 3–17. [Google Scholar] [CrossRef]
- Warden, G.L.; Griffith, J.R. Ensuring Management Excellence in the Healthcare System. J Healthc Manag 2001, 46, 228–237. [Google Scholar] [CrossRef]
- Baker, A. Crossing the Quality Chasm: A New Health System for the 21st Century. BMJ Br. Med. J. 2001, 323, 1192. [Google Scholar] [CrossRef]
- Nigam, A.; Huising, R.; Golden, B.R. Improving Hospital Efficiency: A Process Model of Organizational Change Commitments. Med. Care Res. Rev. 2014, 71, 21–42. [Google Scholar] [CrossRef] [PubMed]
- Fraser, I.; Encinosa, W.; Glied, S. Improving Efficiency and Value in Health Care: Introduction. Health Serv. Res. 2008, 43, 1781–1786. [Google Scholar] [CrossRef]
- Fung, C.H.; Lim, Y.-W.; Mattke, S.; Damberg, C.; Shekelle, P.G. Systematic Review: The Evidence That Publishing Patient Care Performance Data Improves Quality of Care. Ann. Intern. Med. 2008, 148, 111–123. [Google Scholar] [CrossRef] [PubMed]
- Krumholz, H.M.; Keenan, P.S.; Brush, J.E., Jr.; Bufalino, V.J.; Chernew, M.E.; Epstein, A.J.; Heidenreich, P.A.; Ho, V.; Masoudi, F.A.; Matchar, D.B. Standards for Measures Used for Public Reporting of Efficiency in Health Care: A Scientific Statement from the American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research and the American College of Cardiology Foundation. Circulation 2008, 118, 1885–1893. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kohl, S.; Schoenfelder, J.; Fügener, A.; Brunner, J.O. The Use of Data Envelopment Analysis (DEA) in Healthcare with a Focus on Hospitals. Health Care Manag. Sci. 2019, 22, 245–286. [Google Scholar] [CrossRef]
- Lee, K.-H.; Yang, S.-B.; Choi, M. The Association between Hospital Ownership and Technical Efficiency in a Managed Care Environment. J. Med. Syst. 2009, 33, 307–315. [Google Scholar] [CrossRef]
- Bhat, V.N. Institutional Arrangements and Efficiency of Health Care Delivery Systems. Eur. J. Health Econ. 2005, 6, 215–222. [Google Scholar] [CrossRef] [PubMed]
- North, D.C. Institutions and Economic Theory. Am. Econ. 2016, 61, 72–76. [Google Scholar] [CrossRef]
- Zhang, X.; Tone, K.; Lu, Y. Impact of the Local Public Hospital Reform on the Efficiency of Medium-Sized Hospitals in Japan: An Improved Slacks-Based Measure Data Envelopment Analysis Approach. Health Serv. Res. 2018, 53, 896–918. [Google Scholar] [CrossRef]
- Morris, K.; Zelmer, J. Public Reporting of Performance Measures in Health Care; Canadian Policy Research Networks: Ottawa, ON, Canada, 2005. [Google Scholar]
- Shortell, S.M. Increasing Value: A Research Agenda for Addressing the Managerial and Organizational Challenges Facing Health Care Delivery in the United States. Med. Care Res. Rev. 2004, 61, 12S–30S. [Google Scholar] [CrossRef]
- Alvarez, A.; Arias, C.; Greene, W. Accounting for Unobservables in Production Models: Management and Inefficiency. Econom. Soc. 2004, 1–20. [Google Scholar]
- Ferrari, D.A. Market Oriented Reforms of Health Services: A Non-Parametric Analysis. Serv. Ind. J. 2006, 26, 1–13. [Google Scholar] [CrossRef]
- Preyra, C.; Pink, G. Scale and Scope Efficiencies through Hospital Consolidations. J. Health Econ. 2006, 25, 1049–1068. [Google Scholar] [CrossRef] [PubMed]
- Chua, C.L.; Palangkaraya, A.; Yong, J. Hospital Competition, Technical Efficiency and Quality. Econ. Rec. 2011, 87, 252–268. [Google Scholar] [CrossRef]
- Bates, L.J.; Mukherjee, K.; Santerre, R.E. Market Structure and Technical Efficiency in the Hospital Services Industry: A DEA Approach. Med. Care Res. Rev. 2006, 63, 499–524. [Google Scholar] [CrossRef]
- Kim, Y.; Lee, K.-H.; Choi, S.W. Multifaced Evidence of Hospital Performance in Pennsylvania. Healthcare 2021, 9, 670. [Google Scholar] [CrossRef]
- Enthoven, A.C.; Tollen, L.A. Competition In Health Care: It Takes Systems to Pursue Quality and Efficiency. Health Aff. 2005, 24, W5–W420. [Google Scholar] [CrossRef]
- Cooper, Z.; Gibbons, S.; Jones, S.; McGuire, A. Does Hospital Competition Improve Efficiency? An Analysis of the Recent Market-Based Reforms to the English NHS; London School of Economics and Political Science: London, UK, 2010. [Google Scholar]
- Hollingsworth, B. The Measurement of Efficiency and Productivity of Health Care Delivery. Health Econ 2008, 17, 1107–1128. [Google Scholar] [CrossRef]
- Hollingsworth, B.; Street, A. The Market for Efficiency Analysis of Health Care Organisations. Health Econ. 2006, 15, 1055–1059. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-H.; Park, J.; Lim, S.; Park, S.-C. Has Competition Increased Hospital Technical Efficiency? Health Care Manag. 2015, 34, 106–112. [Google Scholar] [CrossRef]
- Zwanziger, J.; Melnick, G.A.; Mann, J.; Simonson, L. How Hospitals Practice Cost Containment with Selective Contracting and the Medicare Prospective Payment System. Med. Care 1994, 32, 1153–1162. [Google Scholar] [CrossRef] [PubMed]
- Mukamel, D.B.; Zwanziger, J.; Bamezai, A. Hospital Competition, Resource Allocation and Quality of Care. BMC Health Serv. Res. 2002, 2, 10. [Google Scholar] [CrossRef]
- Wu, B.; Jung, J.; Kim, H.; Polsky, D. Entry Regulation and the Effect of Public Reporting: Evidence from Home Health Compare. Health Econ. 2019, 28, 492–516. [Google Scholar] [CrossRef]
- Dranove, D.; Satterthwaite, M.A. Monopolistic Competition When Price and Quality Are Imperfectly Observable. RAND J. Econ. 1992, 518–534. [Google Scholar] [CrossRef]
- Zhao, X. Competition, Information, and Quality: Evidence from Nursing Homes. J. Health Econ. 2016, 49, 136–152. [Google Scholar] [CrossRef] [PubMed]
- Chou, S.-Y.; Deily, M.E.; Li, S.; Lu, Y. Competition and the Impact of Online Hospital Report Cards. J. Health Econ. 2014, 34, 42–58. [Google Scholar] [CrossRef]
- Gravelle, H.; Sivey, P. Imperfect Information in a Quality-Competitive Hospital Market. J. Health Econ. 2010, 29, 524–535. [Google Scholar] [CrossRef]
- Stiles, R.A.; Mick, S.S.; Wise, C.G. The Logic of Transaction Cost Economics in Health Care Organization Theory. Health Care Manag. Rev. 2001, 26, 85–92. [Google Scholar] [CrossRef]
- Singh, S.R.; Cramer, G.R.; Young, G.J. The Magnitude of a Community’s Health Needs and Nonprofit Hospitals’ Progress in Meeting Those Needs: Are We Faced with a Paradox? Public Health Rep. 2017, 133, 75–84. [Google Scholar] [CrossRef]
- Harrison, J.P.; Meyer, S. Measuring Efficiency among US Federal Hospitals. Health Care Manag. 2014, 33, 117–127. [Google Scholar] [CrossRef]
- Su, E.C.-Y.; Hsiao, C.-H.; Chen, Y.-T.; Yu, S.-H. An Examination of COVID-19 Mitigation Efficiency among 23 Countries. Healthcare 2021, 9, 755. [Google Scholar] [CrossRef]
- Czypionka, T.; Kraus, M.; Mayer, S.; Röhrling, G. Efficiency, Ownership, and Financing of Hospitals: The Case of Austria. Health Care Manag. Sci. 2014, 17, 331–347. [Google Scholar] [CrossRef]
- Baker, L.C. Measuring Competition in Health Care Markets. Health Serv. Res. 2001, 36, 223. [Google Scholar]
- Skinner, J.S.; Fisher, E.S.; Wennberg, J. The efficiency of Medicare. In Analyses in the Economics of Aging; University of Chicago Press: Chicago, IL, USA, 2005; pp. 129–160. [Google Scholar]
- Mendez, C.M.; Harrington, D.W.; Christenson, P.; Spellberg, B. Impact of Hospital Variables on Case Mix Index as a Marker of Disease Severity. Popul. Health Manag. 2014, 17, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.-C.; Jiang, L.; Phillips, C.D.; Ohsfeldt, R.L. Rural-Urban Differences in Health Care Expenditures: Empirical Data from US Households. Adv. Public Health 2014. [CrossRef]
- Cho, N.-E.; Hong, K. A Kitchen with Too Many Cooks: Factors Associated with Hospital Profitability. Sustainability 2018, 10, 323. [Google Scholar] [CrossRef]
- Horwitz, J.R.; Nichols, A. Hospital Ownership and Medical Services: Market Mix, Spillover Effects, and Nonprofit Objectives. J. Health Econ. 2009, 28, 924–937. [Google Scholar] [CrossRef] [PubMed]
- Grabowski, D.C.; Hirth, R.A. Competitive Spillovers across Non-Profit and for-Profit Nursing Homes. J. Health Econ. 2003, 22, 1–22. [Google Scholar] [CrossRef]
- Patel, K.; Rushefsky, M.E. Healthcare Politics and Policy in America. Public Integr. 2014, 17, 94–96. [Google Scholar]
- Harrison, J.P.; Coppola, M.N.; Wakefield, M. Efficiency of Federal Hospitals in the United States. J. Med. Syst. 2004, 28, 411–422. [Google Scholar] [CrossRef] [PubMed]
- Huerta, T.R.; Harle, C.A.; Ford, E.W.; Diana, M.L.; Menachemi, N. Measuring Patient Satisfaction’s Relationship to Hospital Cost Efficiency: Can Administrators Make a Difference? Health Care Manag. Rev. 2016, 41, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Noh, S.; Janousek, C.L.; Park, J.H. State Strategies to Address Medicaid Prescription Spending: Negotiated Pricing vs. Price Transparency. Health Econ. Policy Law 2021, 16, 201–215. [Google Scholar] [CrossRef]
- Austin, J.M.; Jha, A.K.; Romano, P.S.; Singer, S.J.; Vogus, T.J.; Wachter, R.M.; Pronovost, P.J. National Hospital Ratings Systems Share Few Common Scores and May Generate Confusion Instead of Clarity. Health Aff. 2015, 34, 423–430. [Google Scholar] [CrossRef]
- Curfman, G.D. All-Payer Claims Databases after Gobeille. Health Affairs. 2017, 058995. [Google Scholar] [CrossRef]
- Ivancevich, J.; Konopaske, R.; Matteson, M. Organizational Behavior and Management; McGraw-Hill Higher Education: New York, NY, USA, 2013; ISBN 978-0-07-749938-9. [Google Scholar]
- Neprash, H.T.; McWilliams, J.M. Provider Consolidation and Potential Efficiency Gains: A Review of Theory and Evidence. Antitrust. Law J. 2019, 82, 551–578. [Google Scholar]
- Grabowski, D.C.; Town, R.J. Does Information Matter? Competition, Quality, and the Impact of Nursing Home Report Cards. Health Serv. Res. 2011, 46, 1698–1719. [Google Scholar] [CrossRef]
- Bloom, N.; Genakos, C.; Sadun, R.; van Reenen, J. Management Practices across Firms and Countries. Acad. Manag. Perspect. 2012, 26, 12–33. [Google Scholar] [CrossRef]
- Halasyamani, L.K.; Davis, M.M. Conflicting Measures of Hospital Quality: Ratings from “Hospital Compare” versus “Best Hospitals”. J. Hosp. Med. Off. Publ. Soc. Hosp. Med. 2007, 2, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Harrison, J.P.; Sexton, C. The Paradox of the Not-for-Profit Hospital. Health Care Manag. 2004, 23, 192–204. [Google Scholar] [CrossRef]
| Variables | Description |
|---|---|
| Dependent Variable | |
| Technical efficiency | Efficiency scores derived from the DEA method using outputs and inputs. |
| 1. Output Variables | |
| (1) Outpatient visits | Total number of outpatient visits |
| (2) Inpatient days | Total number of inpatient days |
| (3) Surgeries | Total number of surgeries |
| (4) Residents | Total number of residents (FTEs) |
| 2. Input Variables | |
| (1) Operating expenses | Total operating expenses excluding payroll and benefit |
| (2) Hospital beds | Total number of beds in a hospital |
| (3) Doctor of Medicine | Total FTEs of MDs and DOs |
| (4) Registered Nurse | Total FTEs of RNs |
| (5) Other FTEs | Total number of other FTEs excluding trainees |
| Independent Variables | |
| 1. Transparent environment | |
| (1) APCD Adoption (1/0) | If a state adopted APCD = 1, otherwise = 0 |
| (2) Data Availability | A ratio for the number of hospitals that successfully reported their performance and the total number of hospitals in a county (=the number of successfully reported hospitals/total number of hospitals in a county) |
| 2. Competition (HHI) | The weighted (by hospital patient shares) hospital referral region-based HHIs for each hospital (=(each hospital’s number of adjusted admissions/total number of adjusted admissions in an HRR)2) |
| Control Variables | |
| 1. Case Mix Index (CMI) | Case-Mix-Index from CMS |
| 2. Size | The number of hospital beds |
| 3. Urban | Location (urban = 1, others = 0) |
| 4. Ownership | Hospital ownership type (Nonprofit = 1, For-profit = 0) |
| 5. Teaching affiliation | Teaching hospital (Teaching = 1, Non-teaching = 0) |
| 6. Medicare discharge (%) | The ratio of Medicare discharges out of total discharge |
| 7. Medicaid discharge (%) | The ratio of Medicaid discharges out of total discharge |
| 8. Nonprofit market share (%) | The market share of nonprofit hospitals in a county based on the total number of beds |
| 9. Uninsured (%) | The uninsured rate of population under age 65 in a county |
| 10. Lobbying efforts ($) | The total amount of money that AHA subsidiaries spent on lobbying efforts in a state |
| Hospitals | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
|---|---|---|---|---|---|---|---|---|
| Efficient | (#) | 76 | 69 | 72 | 63 | 74 | 55 | 61 |
| (%) | 2.14% | 1.98% | 2.07% | 1.84% | 2.17% | 1.61% | 1.78% | |
| Mean | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Inefficient | (#) | 3474 | 3422 | 3414 | 3360 | 3333 | 3371 | 3361 |
| (%) | 97.86% | 98.02% | 97.93% | 98.16% | 97.83% | 98.39% | 98.22% | |
| Mean | 0.5321 | 0.5191 | 0.5187 | 0.5593 | 0.5346 | 0.4723 | 0.5375 | |
| Overall | (#) | 3550 | 3491 | 3486 | 3423 | 3407 | 3426 | 3422 |
| Mean | 0.5421 | 0.5286 | 0.5286 | 0.5674 | 0.5447 | 0.4808 | 0.5457 |
| Variables/Year | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|
| Observations | 3550 | 3491 | 3486 | 3423 | 3407 | 3426 | 3422 |
| Efficiency | 0.5421 | 0.5286 | 0.5286 | 0.5674 | 0.5447 | 0.4808 | 0.5457 |
| APCD (#) | 16 | 18 | 20 | 22 | 22 | 22 | 23 |
| Data Availability (%) | 0.8578 | 0.8576 | 0.8596 | 0.8945 | 0.7880 | 0.7558 | 0.7524 |
| Market Competition | 0.0229 | 0.0237 | 0.0239 | 0.0244 | 0.0246 | 0.0246 | 0.0246 |
| CMI | 1.4659 | 1.4746 | 1.4833 | 1.4976 | 1.5247 | 1.5515 | 1.5583 |
| Bed size (#) | 179 | 181 | 181 | 181 | 182 | 182 | 182 |
| Urban (#) | 530 | 509 | 492 | 465 | 467 | 462 | 460 |
| Nonprofit (#) | 2742 | 2708 | 2723 | 2695 | 2686 | 2698 | 2724 |
| Teaching affiliation (#) | 878 | 877 | 883 | 896 | 927 | 924 | 915 |
| Medicare discharge | 0.5050 | 0.5029 | 0.5078 | 0.5131 | 0.5125 | 0.5124 | 0.5159 |
| Medicaid discharge | 0.1673 | 0.1674 | 0.1658 | 0.1774 | 0.1817 | 0.1826 | 0.1842 |
| Nonprofit market share | 0.8040 | 0.8054 | 0.8087 | 0.8097 | 0.8105 | 0.8117 | 0.8146 |
| Uninsured (%) | 17.16 | 16.81 | 16.61 | 13.41 | 10.88 | 9.95 | 10.20 |
| Lobbying ($) | 148,710 | 140,679 | 139,641 | 155,372 | 154,846 | 156,208 | 213,769 |
| Slacks/Year | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|
| Efficient hospital (#) | 76 | 69 | 72 | 63 | 74 | 55 | 61 |
| Inefficient hospital (#) | 3474 | 3422 | 3414 | 3360 | 3333 | 3371 | 3361 |
| Average Slack of Input | |||||||
| Expenses ($, million) | 5.04 | 6.75 | 2.59 | 9.02 | 7.52 | 10.85 | 3.4 |
| Beds (#) | 0.19 | 0.14 | 0.2 | 0.14 | 0.17 | 0.21 | 0.18 |
| Doctor of Medicine (FTEs) | 8.47 | 10.78 | 8.73 | 6.12 | 9.39 | 3.51 | 10.3 |
| Registered Nurse (FTEs) | 46.13 | 23.6 | 7.04 | 42.16 | 31.39 | 26.36 | 29.89 |
| Other (FTEs) | 43.14 | 38.29 | 82.41 | 28.39 | 39.38 | 42.7 | 27.77 |
| Efficiency | Coefficient | Std. Error | |
|---|---|---|---|
| APCD | −0.0419 | *** | 0.0153 |
| Data Availability | 0.0132 | 0.0103 | |
| HHI | −0.0469 | * | 0.026 |
| APCD * HHI | 0.0273 | 0.0346 | |
| Data Availability * HHI | 0.0495 | *** | 0.0175 |
| CMI | 0.0178 | *** | 0.00675 |
| Bed (#) | 0.000033 | ** | 0.000013 |
| Urban (#) | 0.0256 | *** | 0.00617 |
| Nonprofit (#) | 0.0143 | *** | 0.00525 |
| Teaching affiliation (#) | 0.0459 | *** | 0.00472 |
| Medicare discharge (%) | −0.0175 | *** | 0.00516 |
| Medicaid discharge (%) | 0.0342 | *** | 0.0111 |
| Nonprofit market share (%) | 0.0402 | *** | 0.00866 |
| Uninsured (%) | −0.00111 | *** | 0.00033 |
| Lobbying ($ million) | −0.0223 | *** | 0.00629 |
| 2012 | −0.0142 | *** | 0.00208 |
| 2013 | −0.0145 | *** | 0.00211 |
| 2014 | 0.0182 | *** | 0.00243 |
| 2015 | −0.00563 | * | 0.00309 |
| 2016 | −0.0701 | *** | 0.00344 |
| 2017 | −0.00435 | 0.00342 | |
| Constant | 0.465 | *** | 0.0169 |
| rho | 0.7097284 | ||
| Log likelihood | 19,629.255 | ||
| Wald | 2357.03 | *** | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, A.; Lee, K.-H. The Impact of Public Reporting Schemes and Market Competition on Hospital Efficiency. Healthcare 2021, 9, 1031. https://doi.org/10.3390/healthcare9081031
Han A, Lee K-H. The Impact of Public Reporting Schemes and Market Competition on Hospital Efficiency. Healthcare. 2021; 9(8):1031. https://doi.org/10.3390/healthcare9081031
Chicago/Turabian StyleHan, Ahreum, and Keon-Hyung Lee. 2021. "The Impact of Public Reporting Schemes and Market Competition on Hospital Efficiency" Healthcare 9, no. 8: 1031. https://doi.org/10.3390/healthcare9081031
APA StyleHan, A., & Lee, K.-H. (2021). The Impact of Public Reporting Schemes and Market Competition on Hospital Efficiency. Healthcare, 9(8), 1031. https://doi.org/10.3390/healthcare9081031






