Healthcare Safety Nets during the COVID-19 Pandemic Based on Double Diamond Model: A Concept Analysis
Abstract
1. Introduction
1.1. Necessity of the Study
1.2. Purpose
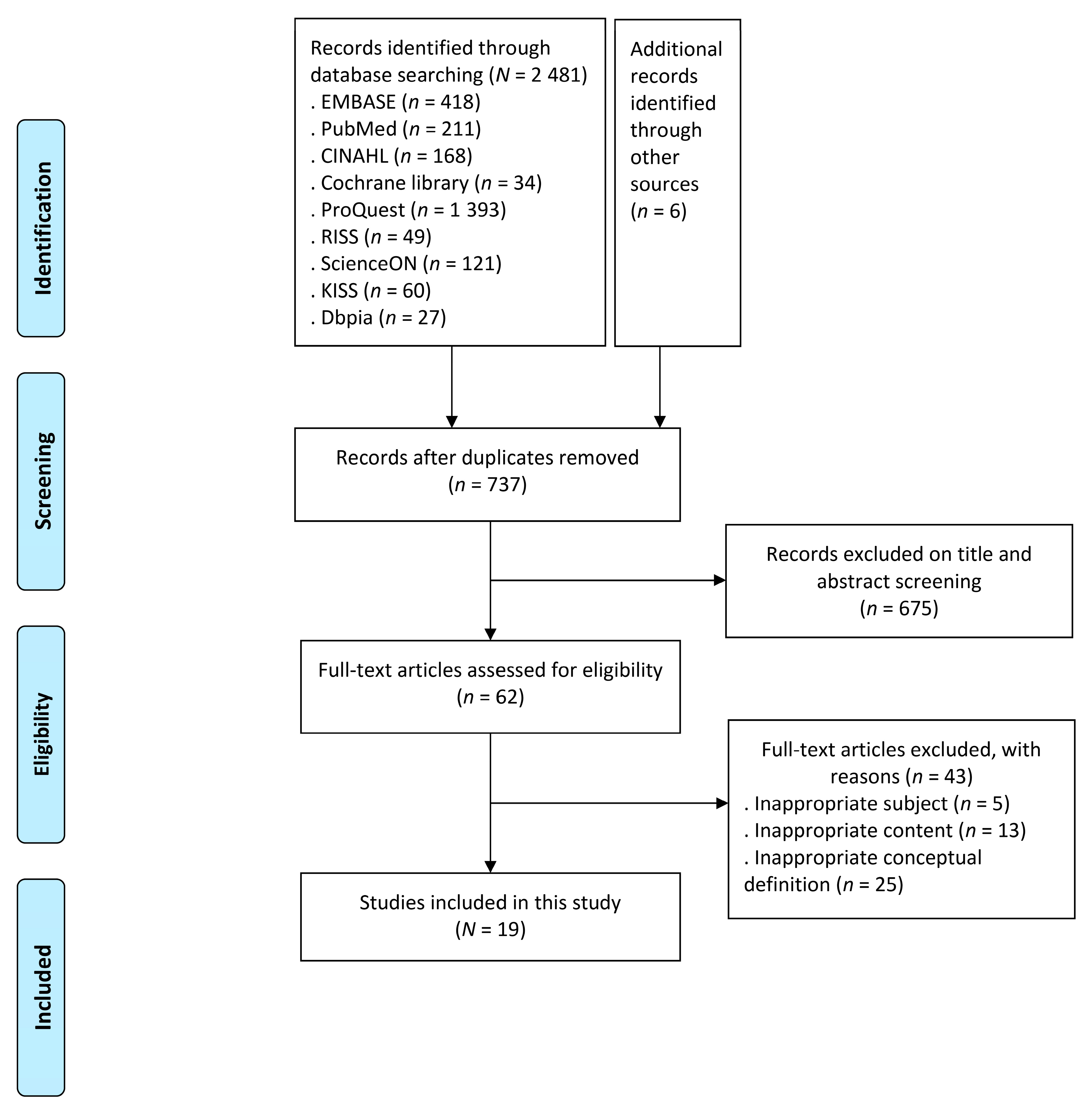
2. Methods
2.1. Study Design
2.2. Study Details
- Select the concept.
- Determine the purpose of the concept analysis.
- Identify the range of use of the concept.
- Identify the attributes of the concept.
- Present a model case of the concept.
- Present additional cases of the concept (borderline, contrary, and/or related cases).
- Identify antecedents and consequences of the concept.
- Define empirical referents of the concept.
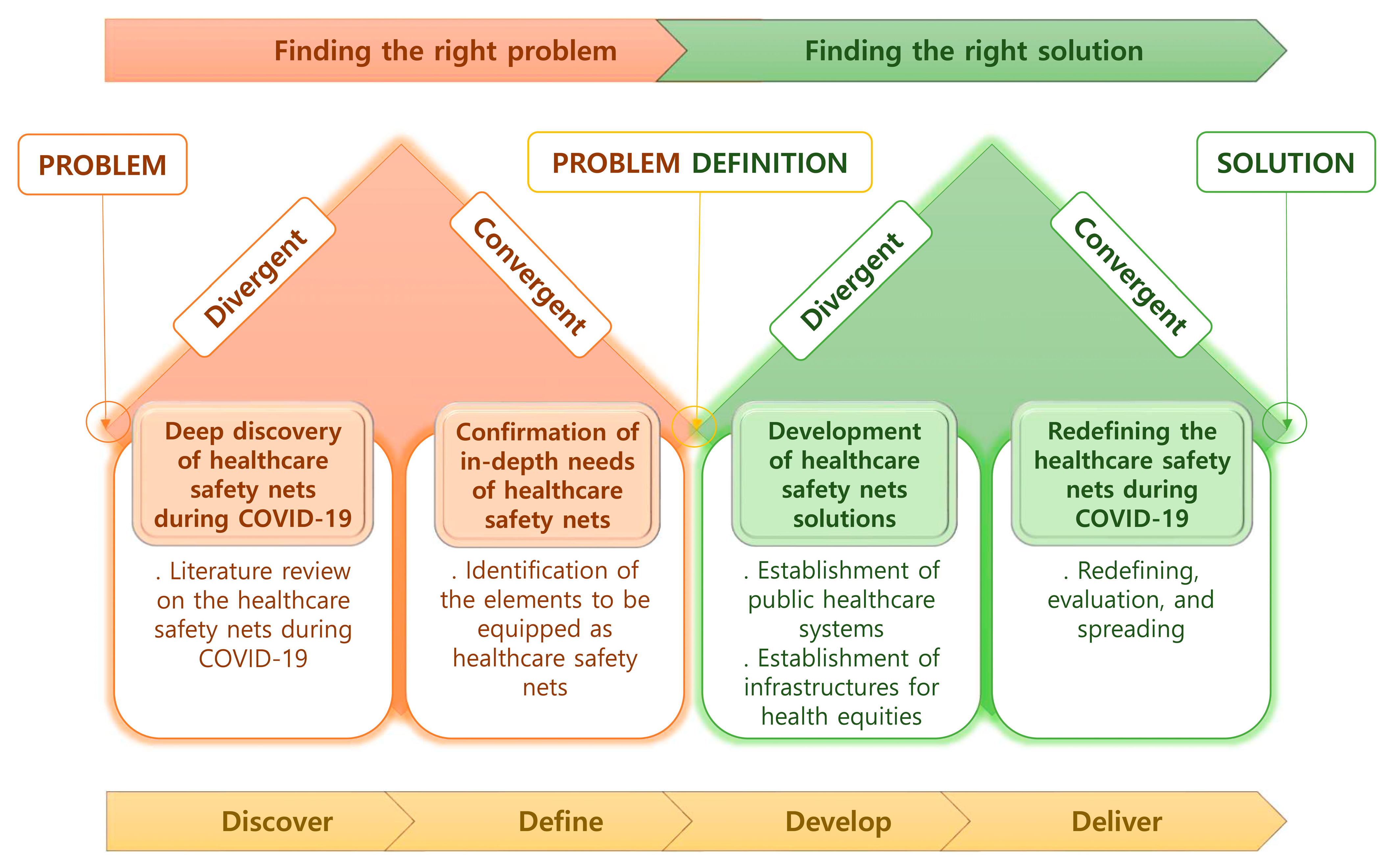
2.3. Study Framework
- (1)
- Discover: deep discovery of healthcare safety nets during COVID-19
- (2)
- Define: confirmation of in-depth needs of healthcare safety nets
- (3)
- Develop: development of healthcare safety nets solutions
- (4)
- Deliver: redefining the healthcare safety nets during COVID-19
3. Results
3.1. Literature Review of Healthcare Safety Nets
3.1.1. Lexical Definition
3.1.2. Range of Use of the Concept
3.2. Tentative Criteria for and Attributes of Healthcare Safety Nets
3.2.1. Conceptual Definitions of Healthcare Safety Nets in the Literature
- Supporting the provision of essential care and healthcare systems (A1, A2, A6, A9, A13, A15)
- Supporting education (A3)
- Coordinating the medical and public health and policy response (A4, A10, A12)
- Improving patients’ outcomes related to disease and clinical severity (A5)
- Improving the rapid screening and treatment of COVID-19 patients (A6, A7, A19)
- Preserving the capabilities of hospitals and healthcare workers (A6, A18)
- Providing appropriate personal protective equipment (A7, A19)
- Use of telemedicine/telephone meetings (A7, A8)
- Increasing medicine and materials (A11, A16)
- Addressing social imbalances to improve health and well-being (A14)
- Monitoring the incidence and imbalance of the disease burden (A17)
3.2.2. Attributes of a Healthcare Safety Net
- (1)
- Capacity
- (2)
- Accessibility
- (3)
- Health Equality
- (4)
- Education
3.3. Construction of a Model Case of the Concept
3.4. Additional Cases of the Concept
3.4.1. Borderline Case
3.4.2. Contrary Case
3.4.3. Related Case
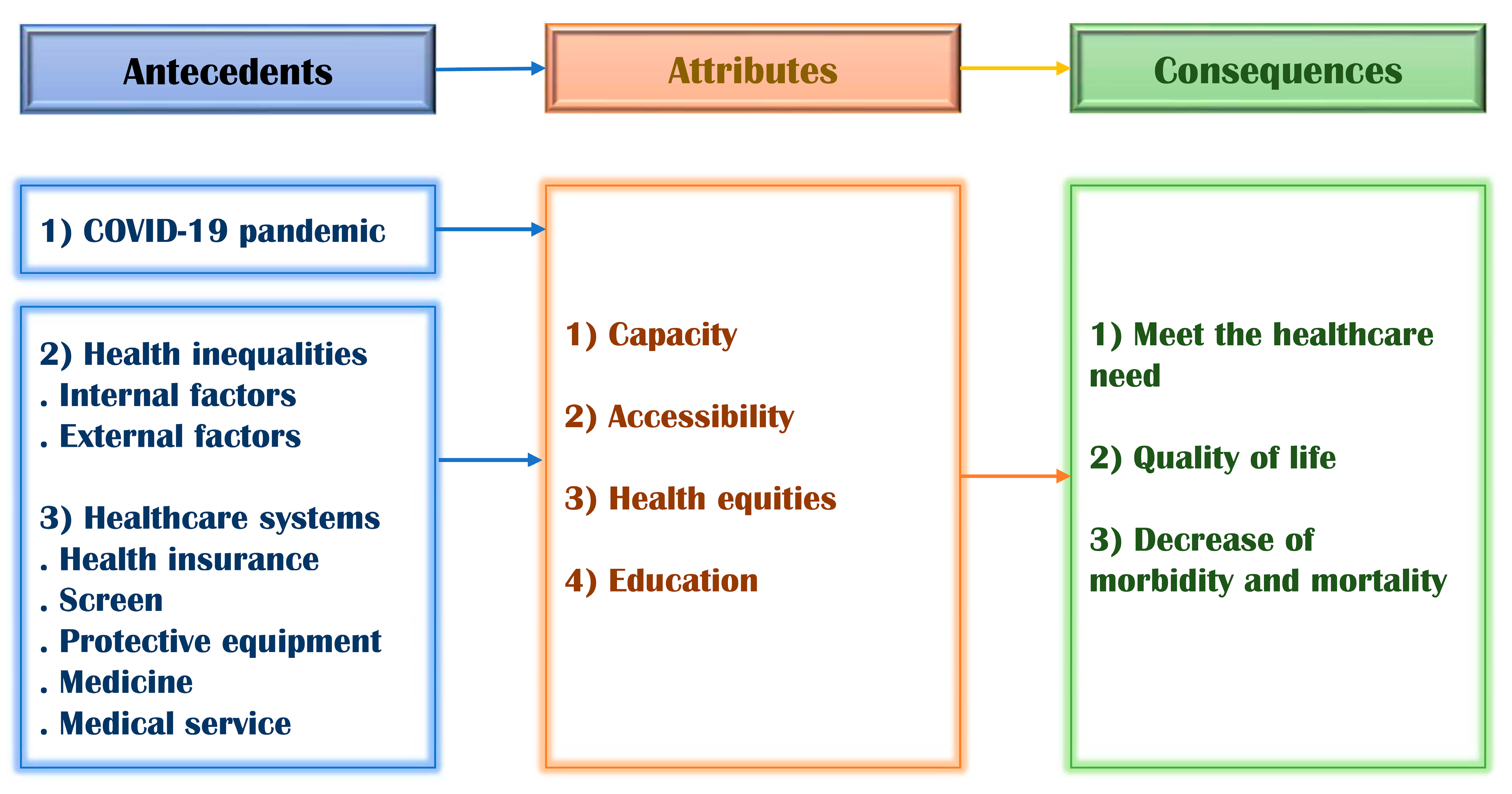
3.5. Identification of Antecedents and Consequences of a Healthcare Safety Net
3.5.1. Antecedents
- COVID-19 pandemic
- Health inequality
- Internal factors
- External factors
- Healthcare systems
- Health insurance
- Screening
- Protective equipment
- Medicine
- Medical services
3.5.2. Consequences
- Meet the healthcare need
- Quality of life
- Decrease in morbidity and mortality
3.6. Empirical Criterion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Burström, B.; Tao, W. Social determinants of health and inequalities in COVID-19. Eur. J. Public Health 2020, 30, 617–618. [Google Scholar] [CrossRef]
- MacKian, S. A review of health seeking behaviour: Problems and prospects. Health Systems Development Programme. Health Policy Plan. 2003, 19, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Yun, G. The 2021 outlook for Healthcare Policy. Health Welf. Policy Forum 2021, 291, 9–22. Available online: http://repository.kihasa.re.kr/bitstream/201002/36867/1/2021.01.No.291.02.pdf (accessed on 2 January 2021).
- Mullangi, S.; Knudsen, J.; Chokshi, D.A. Shoring Up the US Safety Net in the Era of Coronavirus Disease 2019. JAMA Health Forum 2020, 1, e200730. [Google Scholar] [CrossRef]
- Bachireddy, C.; Chen, C.; Dar, M. Securing the Safety Net and Protecting Public Health During a Pandemic: Medicaid’s Response to COVID-19. JAMA 2020, 323, 2009–2010. [Google Scholar] [CrossRef]
- Wanberg, C.R.; Csillag, B.; Douglass, R.P.; Zhou, L.; Pollard, M.S. Socioeconomic status and well-being during COVID-19: A resource-based examination. J. Appl. Psychol. 2020, 105, 1382–1396. [Google Scholar] [CrossRef]
- Mena, G.E.; Martinez, P.P.; Mahmud, A.S.; Marquet, P.A.; Buckee, C.O.; Santillana, M. Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile. Science 2021, 372, eabg5298. [Google Scholar] [CrossRef]
- Lee, D.; Lee, J. Testing on the move: South Korea’s rapid response to the COVID-19 pandemic. Transp. Res. Interdiscip. Perspect. 2020, 5, 100111. [Google Scholar] [CrossRef]
- Yoon, M.S.; Feyissa, I.F.; Suk, S.-W. Panic and Trust during COVID-19: A Cross-Sectional Study on Immigrants in South Korea. Healthcare 2021, 9, 199. [Google Scholar] [CrossRef]
- Coronavirus Disease (COVID-19) Pandemic: Numbers at a Glance. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 24 June 2021).
- Kwak, K. A Study on Establishment of Social Safety Net for Solitary Elderly. Master’s Thesis, Dongguk University Seoul, Seoul, Korea, 2007. [Google Scholar]
- Shin, Y. Health care safety net in Korea: Issues and policy options. In Proceedings of the Health Welf Policy Forum; Korea Institute for Health and Social Affairs: Seoul, Korea, 2009; pp. 17–28. [Google Scholar]
- Lee, S. Policy Directions and Challenges for Coronavirus Infections-19 Response—Focusing on the Health and Medical Industry aspects. Health Welf. Issue Focus 2020, 386, 1–7. Available online: https://kiss.kstudy.com/search/detail_page.asp?key=3778666 (accessed on 28 May 2020).
- Jang, K.-S.; Chung, K.-H.; Kim, Y.-H. A Literature Review of Research on Medical Service Design in Korea. J. Korean Acad. Nurs. Adm. 2018, 24, 85–96. [Google Scholar] [CrossRef][Green Version]
- Design Council. The Design Process; What is the Double Diamond? London: Design Council. 2015. Available online: https://www.designcouncil.org.uk/news-opinion/what-framework-innovation-design-councils-evolved-double-diamond (accessed on 17 March 2015).
- Kwon, J.O.; Lee, E.N.; Bae, S.H. Concept Analysis of Health Inequalities. J. Korean Acad. Nurs. Adm. 2015, 21, 20–31. [Google Scholar] [CrossRef][Green Version]
- Lee, N.; Lee, H.-J. South Korean Nurses’ Experiences with Patient Care at a COVID-19-Designated Hospital: Growth after the Frontline Battle against an Infectious Disease Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 9015. [Google Scholar] [CrossRef] [PubMed]
- Galehdar, N.; Toulabi, T.; Kamran, A.; Heydari, H. Exploring nurses’ perception about the care needs of patients with COVID-19: A qualitative study. BMC Nurs. 2020, 19, 119. [Google Scholar] [CrossRef]
- Walker, L.O.; Avant, K.C. Strategies for Theory Construction in Nursing; Pearson/Prentice Hall: Upper Saddle River, NJ, USA, 2005; Volume 4. [Google Scholar]
- Bela, H.B. Designing Social Systems in a Changing World; Springer: New York, NY, USA, 1996. [Google Scholar]
- Keyes, C.L. Mental health as a complete state: How the salutogenic perspective completes the picture. Bridg. Occup. Organ. Public Health 2014, 179–192. [Google Scholar] [CrossRef]
- Sartorius, N. The meanings of health and its promotion. Croat. Med. J. 2006, 47, 662–664. [Google Scholar] [PubMed]
- Plucinski, M.M.; Ngonghala, C.N.; Bonds, M.H. Health safety nets can break cycles of poverty and disease: A stochastic ecological model. J. R. Soc. Interface 2011, 8, 1796–1803. [Google Scholar] [CrossRef][Green Version]
- Taylor, T.B. Threats to the health care safety net. Acad. Emerg. Med. 2001, 8, 1080–1087. [Google Scholar] [CrossRef] [PubMed]
- Gül, Ü. COVID-19 and dermatology. Turk. J. Med. Sci. 2020, 50, 1751–1759. [Google Scholar] [CrossRef]
- Sung, E.L.; Hwa, J.L. Policy improvement plan for establishing a health and safety net for women affected by violence. Seoul Found. Women Fam. 2011, 1–301. Available online: http://210.105.40.199/items/show/16351 (accessed on 1 September 2011).
- Sarkar, U.; Chen, A.H. Beyond Survival to Transformation: Investing in Safety-Net Innovation to Address The Impacts Of COVID-19. Health Affairs Blog 2020. [Google Scholar] [CrossRef]
- Park, E.J. Post-corona Age, public institutions seek social safety nets. J. Korea Soc. Local Public Enterp. Conf. 2020, 17–36. Available online: http://scholar.dkyobobook.co.kr/searchDetail.laf?barcode=4010028125193 (accessed on 28 December 2020).
- Saint-Louis, M. Safety Huddles: A Safety Net for Nurses Amid the COVID-19 Pandemic. 2020. Available online: https://www.myamericannurse.com/safety-huddles-a-safety-net-for-nurses-amid-the-covid-19-pandemic/ (accessed on 16 December 2020).
- World Health Organization. Health Equity Monitor. Available online: https://www.who.int/gho/health_equity/about/en/ (accessed on 1 November 2020).
- Cho, S.-I. Health equity. Korean Med Assoc. 2015, 58, 1104–1107. [Google Scholar] [CrossRef]
- Lopez, L., 3rd; Hart, L.H., 3rd; Katz, M.H. Racial and Ethnic Health Disparities Related to COVID-19. JAMA 2021, 325, 719–720. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.; Knudsen, J.; Jackson, H.; Wallach, A.B.; Bouton, M.; Natsui, S.; Philippou, C.; Karim, E.; Silvestri, D.M.; Avalone, L.; et al. Staying Connected In The COVID-19 Pandemic: Telehealth At The Largest Safety-Net System In The United States. Health Aff. 2020, 39, 1437–1442. [Google Scholar] [CrossRef] [PubMed]
- Schmitt-Grohé, S.; Teoh, K.; Uribe, M. COVID-19: Testing Inequality in New York City; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Misa, N.Y.; Perez, B.; Basham, K.; Fisher-Hobson, E.; Butler, B.; King, K.; White, D.A.E.; Anderson, E.S. Racial/ethnic disparities in COVID-19 disease burden & mortality among emergency department patients in a safety net health system. Am. J. Emerg. Med. 2020. [Google Scholar] [CrossRef]
- Blumenthal, D.; Fowler, E.J.; Abrams, M.; Collins, S.R. Covid-19—Implications for the Health Care System. N. Engl. J. Med. 2020, 383, 1483–1488. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, P.; Sommers, B.D.; Joynt Maddox, K.E. Essential but Undefined—Reimagining How Policymakers Identify Safety-Net Hospitals. N. Engl. J. Med. 2020, 383, 2593–2595. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.; Shin, H.; Hwang, D.; Kim, H.; Kim, J. Establishment of the Health Care Safety Net and Policy Task; Institute for Health and Social Affairs: Seoul, Korea, 2006; ISBN 978-89-8187-396-7. [Google Scholar]
- Bryan, A.F.; Tsai, T.C. Health Insurance Profitability During the COVID-19 Pandemic. Ann. Surg. 2021, 273, e88–e90. [Google Scholar] [CrossRef]
- Sadasivaiah, S.; Shaffer, E.; Enanoria, W.; Su, G.; Goldman, S.; Scarafia, J.; Lee, T.; Yu, A.; Goldman, L.E.; Ratanawongsa, N. Informatics response to address the COVID-19 pandemic in a safety net healthcare system. JAMIA Open 2021, ooaa057. [Google Scholar] [CrossRef]
- Napoleon, S.C.; Maynard, M.A.; Almonte, A.; Cormier, K.; Bertrand, T.; Ard, K.L.; Chan, P.A. Considerations for STI Clinics During the COVID-19 Pandemic. Sex Transm. Dis. 2020, 47, 431–433. [Google Scholar] [CrossRef]
- Cheng, T.L.; Moon, M.; Artman, M.; On behalf of the Pediatric Policy Council. Shoring up the safety net for children in the COVID-19 pandemic. Pediatric Res. 2020, 88, 349–351. [Google Scholar] [CrossRef] [PubMed]
- Dhanda, S.; Osborne, V.; Lynn, E.; Shakir, S. Postmarketing studies: Can they provide a safety net for COVID-19 vaccines in the UK? BMJ Evid. Based Med. 2020. [Google Scholar] [CrossRef]
- Peynetti Velázquez, P.; Gupta, G.; Gupte, G.; Carson, N.J.; Venter, J. Rapid implementation of telepsychiatry in a safety-net health system during COVID-19 using Lean. NEJM Catal. Innov. Care Deliv. 2020, 1. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0319 (accessed on 17 July 2020).
- Long, B.; Brady, W.J.; Koyfman, A.; Gottlieb, M. Cardiovascular complications in COVID-19. Am. J. Emerg. Med. 2020, 38, 1504–1507. [Google Scholar] [CrossRef] [PubMed]
- Bambra, C.; Riordan, R.; Ford, J.; Matthews, F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health 2020, 74, 964–968. [Google Scholar] [CrossRef]
- Zandian, H.; Alipouri Sakha, M.; Nasiri, E.; Zahirian Moghadam, T. Nursing work intention, stress, and professionalism in response to the COVID-19 outbreak in Iran: A cross-sectional study. Work 2021, 68, 969–979. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Lin, G.; Tang, L.; Yu, L.; Zhou, Z. Special attention to nurses’ protection during the COVID-19 epidemic. Crit. Care 2020, 24, 120. [Google Scholar] [CrossRef] [PubMed]
- McGilton, K.S.; Krassikova, A.; Boscart, V.; Sidani, S.; Iaboni, A.; Vellani, S.; Escrig-Pinol, A. Nurse Practitioners Rising to the Challenge During the Coronavirus Disease 2019 Pandemic in Long-Term Care Homes. Gerontologist 2021, 61, 615–623. [Google Scholar] [CrossRef]
- Kim, H.; Choi, E.; Park, S.; Kim, E. Factors Influencing Preventive Behavior against Coronavirus Disease 2019 (COVID-19) among Medically Inclined College Students. J. Korean Acad. Fundam. Nurs. 2020, 27, 428–437. [Google Scholar] [CrossRef]
- Liu, S.Y.; Kang, X.L.; Wang, C.H.; Chu, H.; Jen, H.J.; Lai, H.J.; Shen, S.H.; Liu, D.; Chou, K.R. Protection procedures and preventions against the spread of coronavirus disease 2019 in healthcare settings for nursing personnel: Lessons from Taiwan. Aust. Crit. Care 2021, 34, 182–190. [Google Scholar] [CrossRef]
- González-Gil, M.T.; González-Blázquez, C.; Parro-Moreno, A.I.; Pedraz-Marcos, A.; Palmar-Santos, A.; Otero-García, L.; Navarta-Sánchez, M.V.; Alcolea-Cosín, M.T.; Argüello-López, M.T.; Canalejas-Pérez, C.; et al. Nurses’ perceptions and demands regarding COVID-19 care delivery in critical care units and hospital emergency services. Intensive Crit. Care Nurs. 2021, 62, 102966. [Google Scholar] [CrossRef]
- Kavanagh, K.T.; Pare, J.; Pontus, C. COVID-19: Through the eyes through the front line, an international perspective. Antimicrob. Resist. Infect. Control. 2020, 9, 179. [Google Scholar] [CrossRef]
- Shon, C. The Response of the Seoul Municipal Hospitals against COVID-19 and Its Implications for Public Hospitals. Korea J. Hosp. Manag. 2020, 25, 38–52. [Google Scholar]
- Park, B.J. Epidemiological Characteristics of COVID-19 and Effective Preparation for the Second Outbreak. J. Health Tech. Assess. 2020, 8, 1–8. [Google Scholar]
- Kim, J. Ipmlication of the COVID-19 pandemic on health equity and healthy cities. Korean J. Health Educ. Promot. 2020, 37, 81–89. [Google Scholar] [CrossRef]
- Alberti, P.M.; Lantz, P.M.; Wilkins, C.H. Equitable pandemic preparedness and rapid response: Lessons from COVID-19 for pandemic health equity. J. Health Politics Policy Law 2020, 45, 921–935. [Google Scholar] [CrossRef]
- Chowkwanyun, M.; Reed, A.L. Racial Health Disparities and Covid-19—Caution and Context. N. Engl. J. Med. 2020, 383, 201–203. [Google Scholar] [CrossRef]
- Kim, E.A. Social Distancing and Public Health Guidelines at Workplaces in Korea: Responses to Coronavirus Disease-19. Saf. Health Work 2020, 11, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S. For a sustainable COVID-19 response policy. Korean J. Public Health 2020, 57, 25–37. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19) Situation Reports. World Health Organization, 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ (accessed on 30 July 2020).
- Triukose, S.; Nitinawarat, S.; Satian, P.; Somboonsavatdee, A.; Chotikarn, P.; Thammasanya, T.; Wanlapakorn, N.; Sudhinaraset, N.; Boonyamalik, P.; Kakhong, B.; et al. Effects of public health interventions on the epidemiological spread during the first wave of the COVID-19 outbreak in Thailand. PLoS ONE 2021, 16, e0246274. [Google Scholar] [CrossRef]
| Author (Year) | Conceptual Definition | |
|---|---|---|
| A1 | Bryan A.F. (2021) | Supporting individual beneficiaries and surgical and physician practices, hospitals, and healthcare systems |
| A2 | Chatterjee P. (2020) | Providing essential care to patients regardless of their insurance coverage, financial circumstances, or immigration status |
| A3 | Bauer K.W. (2021) | Improving emergency food access, access to the program, program’s data systems, and supporting early childcare and education |
| A4 | Sadasivaiah S. (2020) | Coordinating the medical and public health response to COVID-19 |
| A5 | Hsu H.E. (2020) | Improving patient outcomes related to disease and clinical severity, such as age, race/ethnicity, homelessness, and underlying medical conditions, and easing the burden on the health care system from COVID-19 |
| A6 | Bachireddy C. (2020) | Improving the rapid screening and treatment of COVID-19 patients, easing the burden on the healthcare system, preserving the capabilities of hospitals and healthcare workers |
| A7 | Napoleon S.C. (2020) | Screening patients for possible exposures and/or symptoms of COVID-19, providing appropriate personal protective equipment to all staff when possible, and using telemedicine/telephone meetings |
| A8 | Bhaskar S. (2020) | Integral part of the public health response during COVID-19, and telemedicine serves as a safety net in the public health response |
| A9 | Velázquez P.P. (2020) | Ensuring a timely, equitable, safe, and appropriate approach to quality care for all patients |
| A10 | Bambra C. (2020) | Correcting public policy responses such as social protection and public service expansion and pursuit of green inclusive growth strategies |
| A11 | Dhanda S. (2020) | Increasing the vaccination rate of the population |
| A12 | Cheng T.L. (2020) | Public health and safety net infrastructure |
| A13 | Lau J. (2020) | Keeping staff and patients safe, managing limited resources, maintaining access to treatment, and proactively meeting the needs of the most vulnerable residents |
| A14 | Lopez L. (2021) | Providing clinicians, healthcare systems, scientists, and policy makers the opportunity to address social imbalances to improve health and well-being |
| A15 | Anand P. (2020) | Providing coverage to low-income individuals who are uninsured, or not eligible for other insurance options |
| A16 | Zumla A. (2020) | Creating of Biobank and access to biological materials |
| A17 | Misa N.Y. (2020) | Monitoring the incidence and imbalance of disease |
| A18 | Blumenthal D. (2020) | Improving the capacity for collective action to protect the public’s health |
| A19 | Kendzerska T. (2021) | Optimizing the distribution of personal protective equipment and staff to urgently treat individuals with COVID-19, and protecting patients |
| Dimension | Sub-Dimension | Key Findings in Reviewed Literature | |
|---|---|---|---|
| antecedents | COVID-19 pandemic | Shock/shutdown/closure/crisis/financial downturn (A1), closed/motivated rapid (A3), exposure (A5, A10, A19), skyscraping death (A8), lockdown/inequalities in prevalence and mortality rates (A10), crisis (A12, A19), disaster (A13), invasion (A15), disproportionate burden and mortality (A17) | |
| Health inequalities | Internal factors | Disproportionately/postpone/treat/loss/bankruptcy (A1), gap (A3, A6), lack of consistent/restriction (A3), rely on care/limited health literacy (A4), barrier/limit (A4, A6, A8, A9, A13, A17, A19), race and ethnic health disparities (A5, A14, A17), insufficient or no healthcare insurance (A10) | |
| External factors | Vulnerably/excludes (A3), minority/homelessness/illness/clinical severity (A5), higher risk/lack of personal protective/limited staff to screen/limited resources/limited laboratory services (A7), inequalities in morbidity and mortality rates/unequal experience/deprived area/disadvantage (A10), educational and technological disparities (A12), lack of staff (A13), minority (A14) | ||
| Health care systems | Health insurance | Support of individual beneficiaries/surgical and physician practices/hospitals and healthcare systems (A1), health insurance (A1, A2, A9, A12, A13, A15), coverage (A1, A2, A6, A13, A14, A15, A18) | |
| Screen | Monitoring/services (A3), expanding testing (A4), screening procedure (A7), screening patients (A7, A14) Detection of outbreaks, disparities in disease burden, and surveillance (A17) | ||
| Protective equipment | Medical equipment (A6), protective equipment (A7), protect/multisystem (A12), protect equipment (A19) | ||
| Medicine | Vaccine and medicines (A11), medications (A19) | ||
| Medical service | Authority/treatment (A6), telehealth services (A6, A13), health care services/improve infection control efforts (A7, A19), network/collaboration (A8), care delivery/prioritize timely (A9), delivery system (A13), share (A13, A19) | ||
| Attributes | Capacity | Flex/hospital capacity (A1), maximize/expand/equity (A4), preserving/rapidly expanding/supporting care (A6), improved health systems capacity (A6, A10, A18), hotline (A13), emergency department (A17, A19) | |
| Accessibility | Baseline system (A2), prioritized (A3, A7), access to test (A4), urgent care (A4, A19), utilization (A5), ease/flexibility in location of service (A6), access to healthcare service/relationship (A7), contact (A7,12), telehealth implementation/telemedicine/moved to (A8, A19), conveniently/assessing the efficacy of vaccine (A11), access to primary care (A13, A15) | ||
| Health equalities | Essential care (A1, A2), vital (A2), primary site of care (A2, A4, A19), normal/benefit (A3), control/eligible for (A6), collaboration/multidisciplinary/quality care (A9), quality/healthcare resource allocation (A10), balancing (A11), triaged (A19) | ||
| Education | Recommended (A7), instruction (A9), public health education (A14) | ||
| Consequences | Meet the health care need | Avoid prolonged hospitalization (A5), improved healthcare access/treatment quality (A10), cooperation/healthy individuals (A11), management/connection (A13), paradigm shift (A16), consistent(A19) | |
| Quality of life | Promote health (A4), adoption (A13), health and well-being (A14), Quality of life (A16) | ||
| Decrease morbidity and mortality | Life expectancy (A5), reducing morbidity and mortality (A11, A12, A16), prevent end organ damage/governing protective or deleterious outcomes (A16) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, B.-M.; Lee, H.-J. Healthcare Safety Nets during the COVID-19 Pandemic Based on Double Diamond Model: A Concept Analysis. Healthcare 2021, 9, 1014. https://doi.org/10.3390/healthcare9081014
Park B-M, Lee H-J. Healthcare Safety Nets during the COVID-19 Pandemic Based on Double Diamond Model: A Concept Analysis. Healthcare. 2021; 9(8):1014. https://doi.org/10.3390/healthcare9081014
Chicago/Turabian StylePark, Bom-Mi, and Hyun-Jung Lee. 2021. "Healthcare Safety Nets during the COVID-19 Pandemic Based on Double Diamond Model: A Concept Analysis" Healthcare 9, no. 8: 1014. https://doi.org/10.3390/healthcare9081014
APA StylePark, B.-M., & Lee, H.-J. (2021). Healthcare Safety Nets during the COVID-19 Pandemic Based on Double Diamond Model: A Concept Analysis. Healthcare, 9(8), 1014. https://doi.org/10.3390/healthcare9081014






