Hospital Construction Cost Affecting Their Lifecycle: An Italian Overview
Abstract
:1. Introduction
1.1. Healthcare System and Facilities
1.2. The Problem of Hospital Building Construction Cost
1.3. State of the Art of Healthcare Built Assets and Urgent Needs: The Case of Italy
1.4. Study Objective and Paper Structure
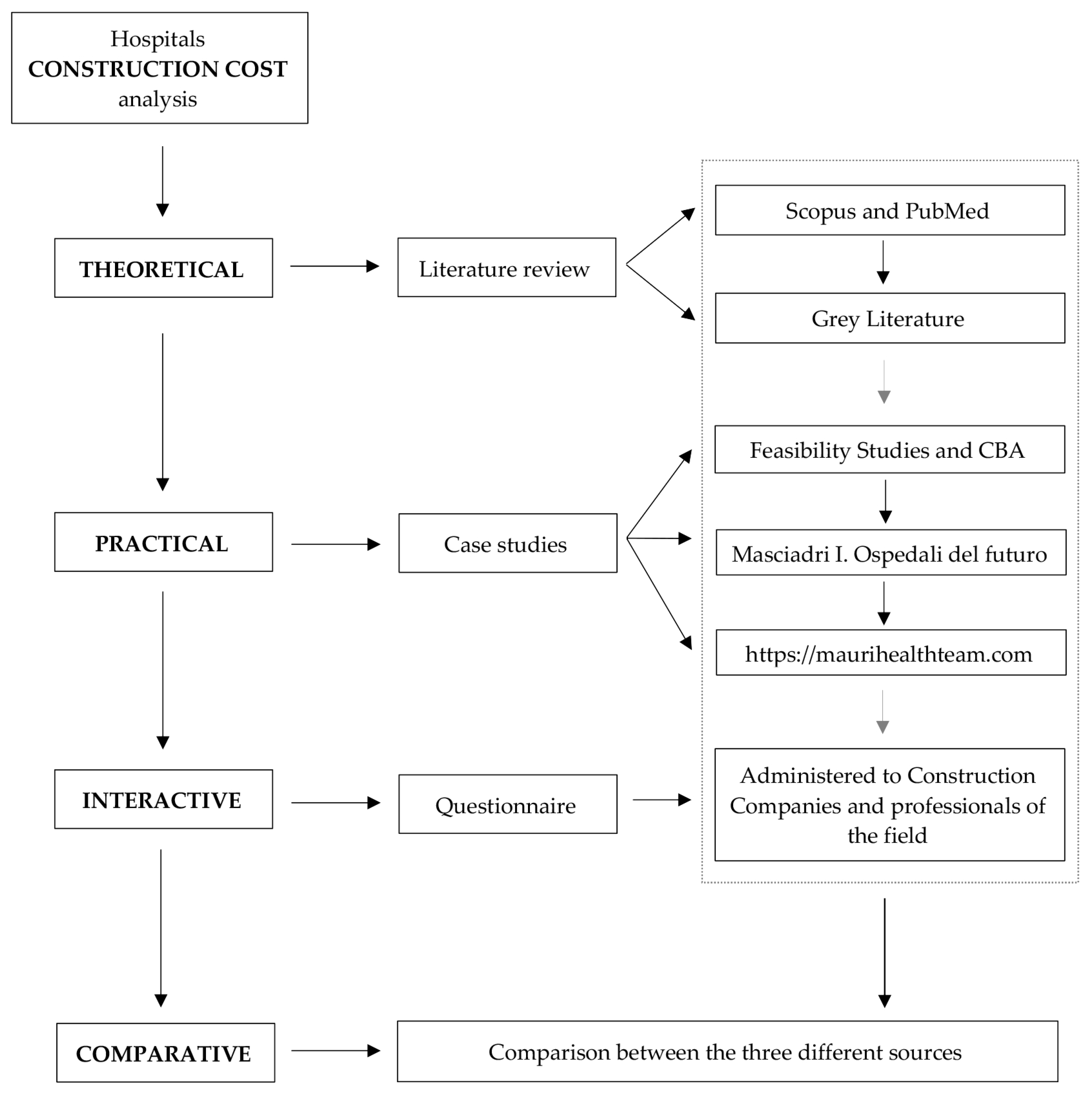
2. Materials and Methods
2.1. Theoretical Phase: Literature Review
2.2. Practical Phase: Case Studies Analysis
2.3. Interactive Phase: Questionnarie Submission
2.4. Comparison Phase
3. Results
3.1. Literature Review
3.2. Case Study Analysis
3.3. Questionnaire
4. Comparison of the Results Achieved through Different Sources
- For the complexity, the average-intensity facilities are SPOKE hospitals;
- The average beds, according to the analysis carried out in the case studies, total 450;
- The typology identified in the average attributes is the poly-block;
- The localization, whose construction cost is more similar to the Italian average (an ideal value which corresponds to 0), is Calabria;
- The technological capital state is the medium one;
- The average age of a hospital facility is indicated as 30 years.
5. Discussion and Implications of Findings
6. Conclusions and Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Full Questionnaire Addressed to the Expert Panel
| Name of the Company |
| Did the Company participated to hospitals construction in the last 10 years? |
| Would you like the questionnaire results to be anonymous? |
| In this section, it is required to insert a construction value in EUR/lm or EUR/sqm for each indicated category, according to own experience in hospital construction. | |
| External viability (EUR/lm) | Literature reference value: 800 EUR/lm |
| Distributive internal viability (EUR/lm) | Literature reference value: 600 EUR/lm |
| White sewer line connection (EUR/lm) | Literature reference value: 200 EUR/lm |
| Black sewer line connection (EUR/lm) | Literature reference value: 300 EUR/lm |
| Water connection (EUR/lm) | Literature reference value: 250 EUR/lm |
| Methane gas connection (EUR/lm) | Literature reference value: 150 EUR/lm |
| Electrical connection (EUR/lm) | Literature reference value: 100 EUR/lm |
| Telephone line connection (EUR/lm) | Literature reference value: 60 EUR/lm |
| Interior lighting work (EUR/lm) | Literature reference value: 350 EUR/lm |
| Pedestrian roads work (EUR/lm) | Literature reference value: 300 EUR/lm |
| Green areas (EUR/sqm) | Literature reference value: 40 EUR/sqm |
| In this section, the 3 different hospital complexity typologies (HUB, SPOKE, BASE) are reported, and it is required to insert a value in EUR/sqm and EUR/bed for their construction. | |
| High-complexity hospital (EUR/sqm) | Literature reference value: 2500 EUR/sqm |
| Medium-complexity hospital (EUR/sqm) | Literature reference value: 2100 EUR/sqm |
| Low-complexity hospital (EUR/sqm) | Literature reference value: 1800 EUR/sqm |
| High-complexity hospital (EUR/bed) | Literature reference value: 300,000 EUR/bed |
| Medium-complexity hospital (EUR/bed) | Literature reference value: 264,000 EUR/bed |
| Low-complexity hospital (EUR/bed) | Literature reference value: 252,000 EUR/bed |
| In this section, it is required to insert a value in EUR/sqm for each category, according to own experience in hospital construction. | |
| Hospitalization (EUR/sqm) | Literature reference value: 2040 EUR/sqm |
| Intensive therapy (EUR/sqm) | Literature reference value: 2450 EUR/sqm |
| Operating rooms (EUR/sqm) | Literature reference value: 4050 EUR/sqm |
| Diagnosis and clinic (EUR/sqm) | Literature reference value: 1650 EUR/sqm |
| Reception (EUR/sqm) | Literature reference value: 1450 EUR/sqm |
| Support and logistic services (EUR/sqm) | Literature reference value: 1450 EUR/sqm |
| Administrative and management services (EUR/sqm) | Literature reference value: 1150 EUR/sqm |
| Connective (EUR/sqm) | Literature reference value: 1150 EUR/sqm |
| Technical rooms (EUR/sqm) | Literature reference value: 1150 EUR/sqm |
| Commerce and other functions (EUR/sqm) | Literature reference value: 1400 EUR/sqm |
| External parking (EUR/sqm) | Literature reference value: 150 EUR/sqm |
| Internal parking (EUR/sqm) | Literature reference value: 1100 EUR/sqm |
| In this section, it is required to insert a value in EUR/sqm for the technological units by the hospital complexity typology, according to own experience in hospital construction | |
| High-complexity hospital (EUR/sqm) | Literature reference value: 367 EUR/sqm |
| Medium-complexity hospital (EUR/sqm) | Literature reference value: 354 EUR/sqm |
| Low-complexity hospital (EUR/sqm) | Literature reference value: 343 EUR/sqm |
| In this section, it is required to insert a value in EUR/sqm for some sanitary furniture functions, according to own experience in hospital construction. | |
| Sanitary area furniture (EUR/sqm) | Literature reference value: 130 EUR/sqm |
| Services furniture (EUR/sqm) | Literature reference value: 120 EUR/sqm |
| Connective and technical room furniture (EUR/sqm) | Literature reference value: 30 EUR/sqm |
References
- WHO. Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action; World Health Organization: Geneva, Switzerland, 2007; ISBN 978-92-4-159607-7. [Google Scholar]
- OCSE. Italia: Profilo Della Sanità 2019; Lo Stato della Salute nell’UE; Osservatorio Europeo Delle Politiche e Dei Sistemi Sanitari (OECD): Brussels, Belgium, 2019. [Google Scholar]
- McKee, M.; Healy, J. (Eds.) Hospitals in a Changing Europe; European Observatory on Health Care Systems Series; Open University Press: Buckingham, UK, 2002; ISBN 978-0-335-20928-6. [Google Scholar]
- Miller, T.S. The Birth of the Hospital in the Byzantine Empire; Johns Hopkins University Press: Baltimore, MD, USA, 1997; ISBN 978-0-8018-5657-0. [Google Scholar]
- WHO. Definition of Hospital and Healthcare Services. Available online: http://www.who.int/hospitals/hospitals-in-the-health-system/en/ (accessed on 30 March 2020).
- Astley, P.; Capolongo, S.; Gola, M.; Tartaglia, A. Operative and Design Adaptability in Healthcare Facilities. J. Technol. Archit. Environ. 2015, 1, 162–170. [Google Scholar] [CrossRef]
- Brambilla, A.; Lindahl, G.; Dell’Ovo, M.; Capolongo, S. Validation of a Multiple Criteria Tool for Healthcare Facilities Quality Evaluation. Facilities 2021, 39, 434–447. [Google Scholar] [CrossRef]
- Clark, R.M.; Hakim, S. (Eds.) Public Private Partnerships: Construction, Protection, and Rehabilitation of Critical Infrastructure; Competitive Government: Public Private Partnerships Series; Springer International Publishing: Cham, Switzerland, 2019; ISBN 978-3-030-24599-3. [Google Scholar]
- Wagenaar, C.; Mens, N. Hospitals: A Design Manual; De Gruyter: Berlin, Germany, 2018; ISBN 978-3-03821-475-5. [Google Scholar]
- Brambilla, A.; Morganti, A.; Lindahl, G.; Riva, A.; Capolongo, S. Complex Projects Assessment. The Impact of Built Environment on Healthcare Staff Wellbeing. In Computational Science and Its Applications—ICCSA 2020; Gervasi, O., Murgante, B., Misra, S., Garau, C., Blečić, I., Taniar, D., Apduhan, B.O., Rocha, A.M.A.C., Tarantino, E., Torre, C.M., et al., Eds.; Lecture Notes in Computer Science; Springer International Publishing: Cham, Switzerland, 2020; Volume 12253, pp. 345–354. ISBN 978-3-030-58813-7. [Google Scholar]
- OASI—Osservatorio sulle Aziende e sul Sistema sanitario Nazionale. Rapporto OASI 2019; A Cura di CERGAS Bocconi; CERGAS: Milan, Italy, 2019. [Google Scholar]
- Lega, F.; Prenestini, A.; Mauri, M.; Bensa, G. l’Ospedale tra Presente e Futuro: Analisi, Diagnosi e Linee di Cambiamento per il Sistema Ospedaliero Italiano; EGEA: Milano, Italy, 2010; ISBN 978-88-238-4273-1. [Google Scholar]
- INAIL. La Sicurezza in Ospedale: Strumenti di Valutazione e Gestione del Rischio; INAIL-Consulenza Tecnica Accertamento Rischi e Prevenzione: Roma, Italy, 2012; ISBN 978-88-7484-263-6. [Google Scholar]
- Dell’Ovo, M.; Capolongo, S. Architectures for Health: Between Historical Contexts and Suburban Areas. Tool to Support Location Strategies. J. Technol. Archit. Environ. 2016, 12, 269–276. [Google Scholar] [CrossRef]
- Capolongo, S.; Gola, M.; Brambilla, A.; Morganti, A.; Mosca, E.I.; Barach, P. COVID-19 and Healthcare Facilities: A Decalogue of Design Strategies for Resilient Hospitals. Acta Bio Med. Atenei Parm. 2020, 91, 50–60. [Google Scholar] [CrossRef]
- Piano Nazionale Di Ripresa e Resilienza. Available online: https://www.governo.it/sites/governo.it/files/PNRR_0.pdf (accessed on 15 May 2021).
- Department of Health and Social Care PM Confirms £3.7 Billion for 40 Hospitals in Biggest Hospital Building Programme in a Generation. Available online: https://www.gov.uk/government/news/pm-confirms-37-billion-for-40-hospitals-in-biggest-hospital-building-programme-in-a-generation (accessed on 15 May 2021).
- Masciadri, I. Ospedali in Italia: Progetti e Realizzazioni; I Libri di Tecnica Ospedaliera; Tecniche Nuove: Milano, Italy, 2011; ISBN 978-88-481-2441-6. [Google Scholar]
- Mauri Health Teams. Available online: http://www.maurihealthteam.com/it/home/ (accessed on 15 May 2021).
- Regione Piemonte. Il Nuovo Ospedale Unico Dell’Azienda Sanitaria Locale TO5. Studio Di Fattibilità; Regional Council of Piedmont: Torino, Italy, 2018. [Google Scholar]
- Azienda Ospedaliera—Ospedali Reuniti Marche Nord. Nuovo Ospedale Marche Nord (2014); Azienda Ospedaliera—Ospedali Reuniti Marche Nord: Pesaro, Italy, 2014. [Google Scholar]
- Regione Puglia. Studio di Fattibilità e Analisi Costi-Benefici per la Realizzazione del Nuovo Ospedale del Sud Est Barese (Monopoli-Fasano); Regional Council of Puglia: Bari, Italy, 2013. [Google Scholar]
- Valle del Serchio. Ospedale Unico della Valle del Serchio. Studio di Fattibilita’ Preliminare; Unione dei Communi Media Valle del Serchio: Borgo a Mozzano, Italy, 2011. [Google Scholar]
- Verso Il Nuovo Duchessa Di Galliera. Studio Di Fattibilità Del Nuovo Ospedale. Available online: http://www.genovaweb.org/doc/vat/Verso_il_nuovo_ospedale_Duchessa_di_Galliera.pdf (accessed on 15 May 2021).
- ASL Sanluri. Studio Di Fattibilità. Nuovo Ospedale Di San Gavino Da 200 Posti Letto; ASL Sanluri: Sanluri, Italy, 2010. [Google Scholar]
- Perino, G.; Sileno, L.; Tresalli, G. Ospedali. Costi Teorici di Costruzione e di Manutenzione; Contributo di Ricerca 263/2018; IRES—Istituto di Ricerche Economico-Sociali del Piemonte: Torino, Italy, 2018; p. 70. [Google Scholar]
- CuneoOnline. Il Costo di un Nuovo Ospedale? Dai 180 ai 200 Milioni di Euro 2018. Available online: https://www.cuneodice.it/attualita/cuneo-e-valli/il-costo-di-un-nuovo-ospedale-dai-180-ai-200-milioni-di-euro_15597.html (accessed on 15 May 2021).
- La Stampa. Il Nuovo Ospedale Unico del Vco: 120 Milioni di Euro per Una Struttura da 300 Posti Pronta in 4 Anni 2015. Available online: https://www.lastampa.it/verbano-cusio-ossola/2015/10/17/news/il-nuovo-ospedale-unico-del-vco-120-milioni-di-euro-per-una-struttura-da-300-posti-pronta-in-4-anni-1.35216091 (accessed on 15 May 2021).
- Bottero, M.; Caprioli, C.; Oppio, A. A Literature Review on Construction Costs Estimation: Hot Topics and Emerging Trends. In Appraisal and Valuation; Green Energy and Technology Series; Morano, P., Oppio, A., Rosato, P., Sdino, L., Tajani, F., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 117–131. ISBN 978-3-030-49578-7. [Google Scholar]
- Caprioli, C.; Bottero, M. Addressing Complex Challenges in Transformations and Planning: A Fuzzy Spatial Multicriteria Analysis for Identifying Suitable Locations for Urban Infrastructures. Land Use Policy 2021, 102, 105147. [Google Scholar] [CrossRef]
- Dell’Anna, F.; Vergerio, G.; Corgnati, S.; Mondini, G. A New Price List for Retrofit Intervention Evaluation on Some Archetypical Buildings. Valori E Valutazioni 2019, 22, 3–17. [Google Scholar]


| N. | Region | City | Source | Hospital Case Study |
|---|---|---|---|---|
| 1 | Piedmont | Moncalieri | Feasibility Study (2018) [20] * | Nuovo Ospedale Unico dell’Azienda Sanitaria Locale TO5 |
| 2 | Marche | Pesaro | Feasibility Study (2014) [21] * | Nuovo Ospedale Marche Nord |
| 3 | Apulia | Monopoli-Fasano | Feasibility Study and CBA (2013) [22] * | Ospedale del Sud Est Barese |
| 4 | Tuscany | Lucca | Preliminary Feasibility Study (2011) [23] * | Ospedale Unico della Valle del Serchio |
| 5 | Liguria | Genoa | Feasibility Study (2010) [24] * | Ospedale Galliera |
| 6 | Sardinia | San Gavino | Feasibility Study (2010) [25] * | Nuovo Ospedale di San Gavino |
| 7 | Lombardy | Brescia | (ongoing) [19] | Fondazione Poliambulanza |
| 8 | Emilia-Romagna | Bologna | (2016) [18] | Ospedale S. Orsola Malpighi |
| 9 | Lombardy | Monza Brianza | (2011) [18] | Ospedale di Vimercate |
| 10 | Lombardy | Milan | (2010) [18,19] | Ospedale di Legnano |
| 11 | Umbria | Perugia | (2008) [18,19] | Ospedale di Gubbio e Gualdo Tadino |
| 12 | Lazio | Roma | (2008) [18] | Policlinico Universitario Campus Bio-medico |
| 13 | Apulia | Bari | (2006) [18] | Ospedale Miulli |
| 14 | Lombardy | Rozzano | (2005) [19] | Istituto Clinico Humanitas |
| Hospital Type | Unit Costs by Square Meter (EUR/Sqm) Unit Costs by Beds (EUR/Bed) | ||
|---|---|---|---|
| Minimum | Reference | Maximum | |
| High complexity | 2000 EUR/sqm 240,000 EUR/bed | 2200 EUR/sqm 264,000 EUR/bed | 2500 EUR/sqm 300,000 EUR/sqm |
| Medium complexity | 1900 EUR/sqm 228,000 EUR/bed | 2100 EUR/sqm 252,000 EUR/bed | 2400 EUR/sqm 288,000 EUR/bed |
| Low complexity | 1800 EUR/sqm 216,000 EUR/bed | 2000 EUR/sqm 240,000 EUR/bed | 2300 EUR/sqm 276,000 EUR/bed |
| Hospital 1 [27] | 1900 EUR/sqm 292,000 EUR/bed | ||
| Hospital 2 [28] | 2040 EUR/sqm N.A. EUR/bed | ||
| N. | Region | City | Hospital | EUR/Sqm | EUR/Bed |
|---|---|---|---|---|---|
| 1 | Piedmont | Moncalieri | Nuovo Ospedale Unico dell’Azienda Sanitaria Locale TO5 Nuovo Ospedale Marche Nord | EUR 1747.4 | EUR 241,651.27 |
| 2 | Marche | Pesaro | Ospedale del Sud Est Barese Ospedale Unico della Valle del Serchio | EUR 1658.18 | EUR 229,541.53 |
| 3 | Apulia | Monopoli-Fasano | Ospedale Galliera Nuovo Ospedale di San Gavino | EUR 1588.38 | EUR 190,605.35 |
| 4 | Tuscany | Lucca | Fondazione Poliambulanza Ospedale S. Orsola Malpighi | EUR 2145.60 | EUR 300,384.00 |
| 5 | Liguria | Genova | Ospedale di Vimercate Ospedale di Legnano | EUR 1805.51 | EUR 272,669.39 |
| 6 | Sardinia | San Gavino | Ospedale di Gubbio e Gualdo Tadino Policlinico Universitario Campus Bio-medico | EUR 1400.97 | EUR 243,761.95 |
| 7 | Apulia | S. Giovanni Rotondo | Ospedale Miulli | EUR 2090.91 | EUR 230,000.00 |
| 8 | Emilia Romagna | Bologna | Nuovo Ospedale Unico dell’Azienda Sanitaria Locale TO5 Nuovo Ospedale Marche Nord | EUR 1903.21 | EUR 265,097.90 |
| 9 | Lombardy | Vimercate | Ospedale del Sud Est Barese Ospedale Unico della Valle del Serchio | EUR 1873.38 | EUR 295,222.80 |
| 10 | Lombardy | Milano | Ospedale Galliera Nuovo Ospedale di San Gavino | EUR 2166.54 | EUR 275,740.88 |
| 11 | Umbria | Perugia | Fondazione Poliambulanza Ospedale S. Orsola Malpighi | EUR 1696.15 | EUR 213,681.18 |
| 12 | Lazio | Roma | Ospedale di Vimercate Ospedale di Legnano | EUR 2391.28 | EUR 347,504.46 |
| 13 | Apulia | Bari | Ospedale di Gubbio e Gualdo Tadino Policlinico Universitario Campus Bio-medico | EUR 1932.42 | EUR 220,449.11 |
| 14 | Lombardy | Rozzano | Ospedale Miulli | EUR 2211.13 | EUR 224,678.83 |
| Cost (EUR/Sqm) | Cost (EUR/Bed) | ||||
|---|---|---|---|---|---|
| Average | Minimum | Maximum | Average | Minimum | Maximum |
| EUR 1863.7 | EUR 1598.09 | EUR 2167.85 | EUR 257,779.87 | EUR 218,095.51 | EUR 319,296.15 |
| Contribution | Cost (EUR/Sqm) | Cost (EUR/Bed) | ||||
|---|---|---|---|---|---|---|
| Average | Minimum | Maximum | Average | Minimum | Maximum | |
| Gray Literature | EUR 2100.00 | EUR 1800.00 | EUR 2500.00 | EUR 252,000.00 | EUR 216,000.00 | EUR 300,000.00 |
| Feasibility Studies | EUR 1724.43 | EUR 1400.97 | EUR 2145.60 | EUR 246,435.58 | EUR 190,605.35 | EUR 300,384.00 |
| Case Studies | EUR 2033.13 | EUR 1696.15 | EUR 2391.28 | EUR 259,046.90 | EUR 213,681.18 | EUR 347,504.46 |
| Panel Investigation | EUR 1832.86 | EUR 1697.14 | EUR 1966.67 | EUR 267,857.14 | EUR 250,000.00 | EUR 310,000.00 |
| Conclusion | EUR 1863.47 | EUR 1598.09 | EUR 2167.85 | EUR 257,779.87 | EUR 218,095.51 | EUR 319,296.15 |
| Factor | Minimum | Medium | Maximum |
|---|---|---|---|
| Complexity | −9% | SPOKE | 9% |
| Beds | 3% | 450 | −3% |
| Typology | −6% | Poly-block | 6% |
| Localization | −12% | Calabria | 12% |
| Technology | −5% | Medium | 5% |
| Maintenance and Management | −36% | 30 | 45% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sdino, L.; Brambilla, A.; Dell’Ovo, M.; Sdino, B.; Capolongo, S. Hospital Construction Cost Affecting Their Lifecycle: An Italian Overview. Healthcare 2021, 9, 888. https://doi.org/10.3390/healthcare9070888
Sdino L, Brambilla A, Dell’Ovo M, Sdino B, Capolongo S. Hospital Construction Cost Affecting Their Lifecycle: An Italian Overview. Healthcare. 2021; 9(7):888. https://doi.org/10.3390/healthcare9070888
Chicago/Turabian StyleSdino, Leopoldo, Andrea Brambilla, Marta Dell’Ovo, Benedetta Sdino, and Stefano Capolongo. 2021. "Hospital Construction Cost Affecting Their Lifecycle: An Italian Overview" Healthcare 9, no. 7: 888. https://doi.org/10.3390/healthcare9070888
APA StyleSdino, L., Brambilla, A., Dell’Ovo, M., Sdino, B., & Capolongo, S. (2021). Hospital Construction Cost Affecting Their Lifecycle: An Italian Overview. Healthcare, 9(7), 888. https://doi.org/10.3390/healthcare9070888








