Evaluating the Impact of the Diabetes Mellitus Strategy for the National Health System: An Interrupted Time Series Analysis
Abstract
1. Introduction
1.1. Diabetes: A Major Public Health Problem
1.2. The Strategy for Diabetes Mellitus of the National Health System (SDM-NHS)
- To reduce the prevalence of overweight and obesity in the general population by promoting breastfeeding and healthier lifestyles.
- To enhance DM screening and early DM diagnosis.
- To improve the management of cardiovascular risk factors in patients with DM and appropriate metabolic control, emphasizing self-care.
- To recognize early complications.
- To reduce DM-related morbidity.
- To avoid maternal and fetal complications providing adequate pregnancy planning and follow up in women with DM.
- To promote gestational DM screening, especially in women at higher risk.
- To encourage and support DM research.
1.3. Indicators for Assessing DM Quality of Care
1.4. Evaluating Public Health Interventions
1.5. Aim of This Study
2. Materials and Methods
2.1. Data
2.2. Statistical Analysis
- Hospital discharge rates of amputations in lower limbs (LLA).
- Hospital discharge rates for stroke.
- Hospital discharge rates for episodes of initial care for acute myocardial infarction (AMI).
- Trend of the series: n1. The trend was controlled through a variable in the database that counts along the period: this variable starts on the first month of the series and continues to the end of the series.
- Intervention: interv. Binary variable with 2 values: 0 for years before 2007 and 1 for years 2007 and later.
- Interaction between intervention and trend: n1.intervn1. This variable represents interaction between trend and time, centered in the moment of the intervention.
3. Results
3.1. Stroke
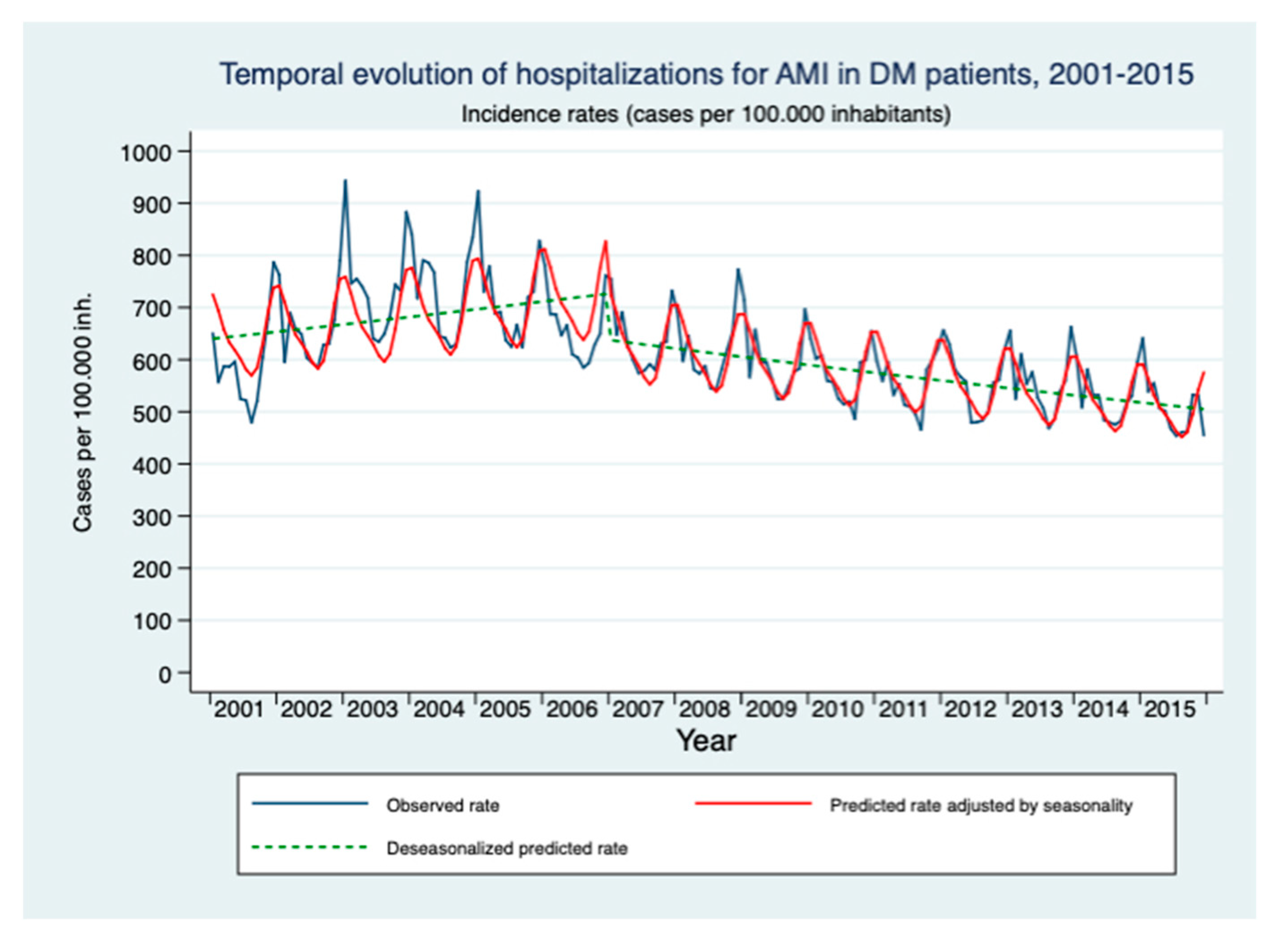
3.2. AMI
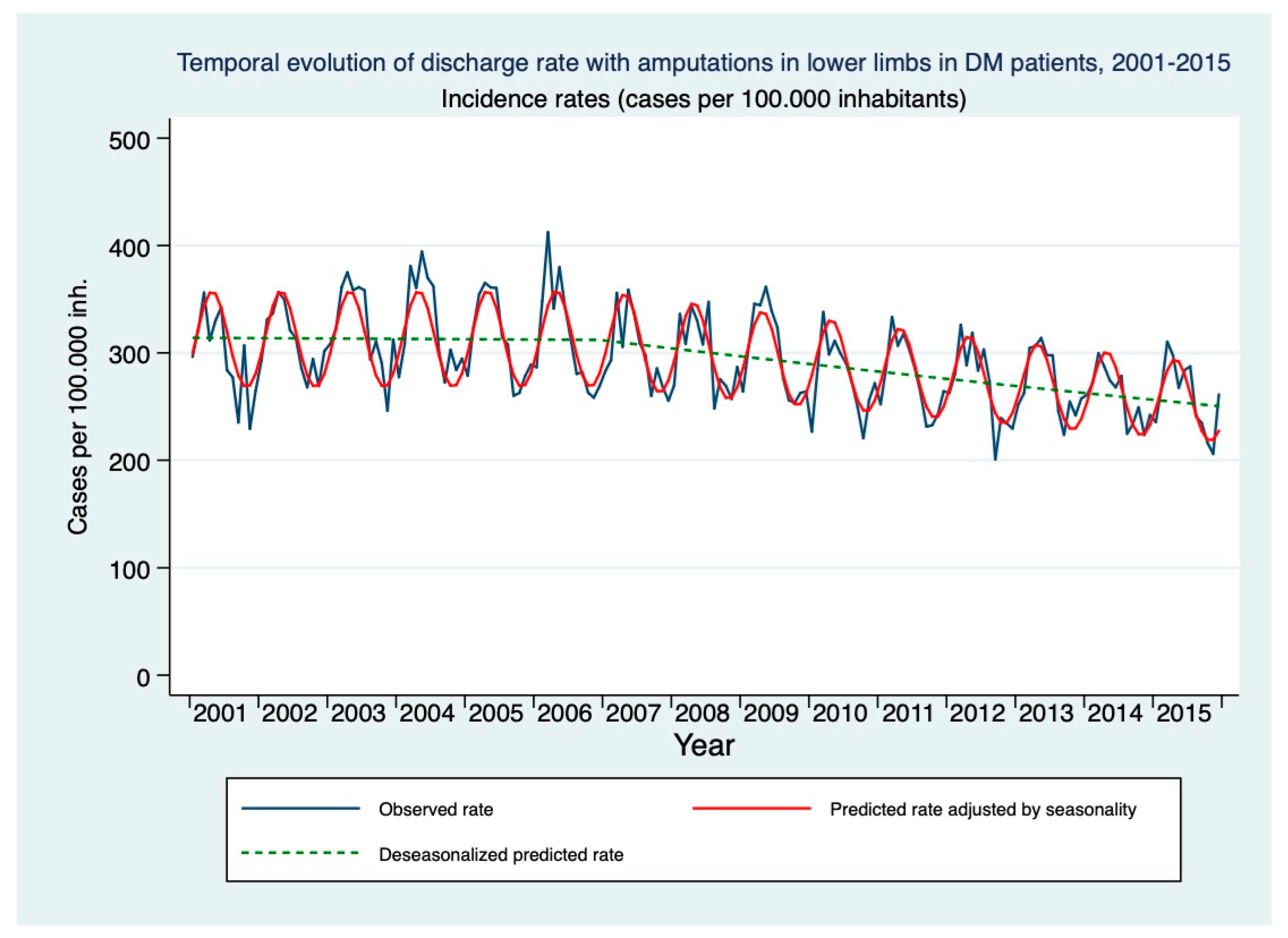
3.3. LLA
4. Discussion
4.1. Main Findings
4.2. Limitations of Observational Data
4.3. Evaluating the Impact of the SDM-NHS
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kolb, H.; Martin, S. Environmental/lifestyle factors in the pathogenesis and prevention of type 2 diabetes. BMC Med. 2017, 15, 131. [Google Scholar] [CrossRef]
- Esposito, S.; Toni, G.; Tascini, G.; Santi, E.; Berioli, M.G.; Principi, N. Environmental Factors Associated With Type 1 Diabetes. Front. Endocrinol. 2019, 10, 592. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística. Nota Técnica. Encuesta Nacional de Salud de España 2017. Principales Resultados. Ministerio de Sanidad, Consumo y Bienestar Social. 2018. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2017/ENSE17_pres_web.pdf (accessed on 14 January 2021).
- Soriguer, F.; Goday, A.; Bosch-Comas, A.; Bordiú, E.; Calle-Pascual, A.; Carmena, R.; Casamitjana, R.; Castaño, L.; Castell, C.; Catalá, M.; et al. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: The Di@bet.es Study. Diabetologia 2012, 55, 88–93. [Google Scholar] [CrossRef] [PubMed]
- CIBER. Estudio di@bet.es: Cerca de 400.000 Personas Desarrollan Diabetes Cada Año en España. Published April 2018. Available online: https://www.ciberisciii.es/noticias/estudio-di-betes-cerca-de-400000-personas-desarrollan-diabetes-cada-ano-en-espana (accessed on 29 February 2020).
- Alemán-Vega, G.; Garrido-Elustondo, S.; Del Cura-González, I.; Sarría-Santamera, A. Is a maintained glycemia between 110/125 mg/dl a risk factor in the development of diabetes? Aten. Primaria 2017, 49, 557–558. [Google Scholar] [CrossRef] [PubMed]
- Martín Martínez, M.; Carmona Alférez, R.; Prado Galbarro, F. Incidence and prevalence of diabetes in an adult population of Madrid (Spain): A study using computerized medical records in primary care. Gac. Sanit. 2013, 27, 284–285. [Google Scholar] [CrossRef][Green Version]
- Forbes, J.M.; Cooper, M.E. Mechanisms of Diabetic Complications. Physiol. Rev. 2013, 93, 137–188. [Google Scholar] [CrossRef] [PubMed]
- Dal Canto, E.; Ceriello, A.; Rydén, L.; Ferrini, M.; Hansen, T.B.; Schnell, O.; Standl, E.; Beulens, J.W. Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications. Eur. J. Prev. Cardiol. 2019, 26 (Suppl. 2), 25–32. [Google Scholar] [CrossRef]
- Kosiborod, M.; Gomes, M.B.; Nicolucci, A.; Pocock, S.; Rathmann, W.; Shestakova, M.V.; Watada, H.; Shimomura, I.; Chen, H.; Cid-Ruzafa, J.; et al. Vascular complications in patients with type 2 diabetes: Prevalence and associated factors in 38 countries (the DISCOVER study program). Cardiovasc. Diabetol. 2018, 17, 150. [Google Scholar] [CrossRef] [PubMed]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Prevalence of cardiovascular disease in type 2 diabetes: A systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc. Diabetol. 2018, 17, 83. [Google Scholar] [CrossRef] [PubMed]
- De Ferranti, S.D.; De Boer, I.H.; Fonseca, V.; Fox, C.S.; Golden, S.H.; Lavie, C.J.; Magge, S.N.; Marx, N.; McGuire, D.K.; Orchard, T.J.; et al. Type 1 Diabetes Mellitus and Cardiovascular Disease. Circulation 2014, 130, 1110–1130. [Google Scholar] [CrossRef] [PubMed]
- Boulton, A.J. The diabetic foot. Medicine 2019, 47, 100–105. [Google Scholar] [CrossRef]
- OECD. Cardiovascular Disease and Diabetes: Policies for Better Care and Quality of Care. Nota de País: España. 2015. Available online: https://www.oecd.org/spain/Cardiovascular-Disease-and-Diabetes-Policies-for-Better-Health-and-Quality-of-Care-Spain-In-Spanish.pdf (accessed on 14 January 2021).
- International Diabetes Federation. IDF Diabetes Atlas [Internet]. 9th ed. Brussels, Belgium. 2019. Available online: https://www.diabetesatlas.org (accessed on 14 January 2021).
- Cho, N.; Shaw, J.E.; Karuranga, S.; Huang, Y.D.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Bastida, J.; Boronat, M.; Moreno, J.O.; Schurer, W. Costs, outcomes and challenges for diabetes care in Spain. Global. Health 2013, 9, 17. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Estrategia en Diabetes del Sistema Nacional de Salud. 2007. Available online: https://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/pdf/excelencia/cuidadospaliativos-diabetes/DIABETES/estrategia_diabetes_sistema_nacional_salud.pdf (accessed on 14 January 2021).
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Estrategia en Diabetes del Sistema Nacional de Salud. Actualización. 2012. Available online: https://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/pdf/excelencia/cuidadospaliativos-diabetes/DIABETES/Estrategia_en_diabetes_del_SNS_Accesible.pdf (accessed on 14 January 2021).
- Rothe, U.; Manuwald, U.; Kugler, J.; Schulze, J. Quality criteria/key components for high quality of diabetes management to avoid diabetes-related complications. J. Public Health 2020. [Google Scholar] [CrossRef]
- Rosengren, A. Cardiovascular disease in diabetes type 2: Current concepts. J. Intern. Med. 2018, 284, 240–253. [Google Scholar] [CrossRef]
- Vesa, C.M.; Popa, L.; Popa, A.R.; Rus, M.; Zaha, A.A.; Bungau, S.; Tit, D.M.; Corb Aron, R.A.; Zaha, D.C. Current Data Regarding the Relationship between Type 2 Diabetes Mellitus and Cardiovascular Risk Factors. Diagnostics 2020, 10, 314. [Google Scholar] [CrossRef] [PubMed]
- Sarría-Santamera, A. Diseños y metodologías para evaluar el impacto de las intervenciones. Rev. Esp. Cardiol. 2020, 73, 689. [Google Scholar] [CrossRef]
- Penfold, R.B.; Zhang, F. Use of Interrupted Time Series Analysis in Evaluating Health Care Quality Improvements. Acad. Pediatr. 2013, 13 (Suppl. 6), S38–S44. [Google Scholar] [CrossRef] [PubMed]
- Bernal, J.L.; Cummins, S.; Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Int. J. Epidemiol. 2017, 46, 348–355. [Google Scholar] [CrossRef]
- Navarro, A.; Utzet, F.; Puig, P.; Caminal, J.; Martín, M. La distribución binomial negativa frente a la de Poisson en el análisis de fenómenos recurrentes. Gac. Sanit. 2001, 15, 447–452. [Google Scholar] [CrossRef][Green Version]
- Harding, J.L.; Pavkov, M.E.; Magliano, D.J.; Shaw, J.E.; Gregg, E.W. Global trends in diabetes complications: A review of current evidence. Diabetologia 2019, 62, 3–16. [Google Scholar] [CrossRef]
- Claessen, H.; Avalosse, H.; Guillaume, J.; Narres, M.; Kvitkina, T.; Arend, W.; Morbach, S.; Lauwers, P.; Nobels, F.; Boly, J.; et al. Decreasing rates of major lower-extremity amputation in people with diabetes but not in those without: A nationwide study in Belgium. Diabetologia 2018, 61, 1966–1977. [Google Scholar] [CrossRef]
- Gæde, P.; Lund-Andersen, H.; Parving, H.-H.; Pedersen, O. Effect of a Multifactorial Intervention on Mortality in Type 2 Diabetes. N. Engl. J. Med. 2008, 358, 580–591. [Google Scholar] [CrossRef]
- Gupta, A.; Kumar, V. Multidisciplinary Approach to Prevent Limb Amputation in Diabetic Patients. J. Endocrinol. Metab. 2019, 9, 120–126. Available online: https://www.jofem.org/index.php/jofem/article/view/615/284284393 (accessed on 14 January 2021). [CrossRef]
- Apelqvist, J.; Larsson, J. What is the most effective way to reduce incidence of amputation in the diabetic foot? Diabetes Metab. Res. Rev. 2000, 16 (Suppl. 1), S75–S83. [Google Scholar] [CrossRef]
- Available online: https://ec.europa.eu/health/ph_projects/2005/action1/docs/action1_2005_frep_11_en.pdf (accessed on 14 January 2021).
- Gæde, P.; Oellgaard, J.; Carstensen, B.; Rossing, P.; Lund-Andersen, H.; Parving, H.H.; Pedersen, O. Years of life gained by multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: 21 years follow-up on the Steno-2 randomised trial. Diabetologia 2016, 59, 2298–2307. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Sistema Nacional de Salud. España 2012. 2012. Available online: www.msssi.gob.es (accessed on 14 January 2021).
- Linden, A. Challenges to validity in single-group interrupted time series analysis. J. Eval. Clin. Pract. 2017, 23, 413–418. [Google Scholar] [CrossRef]
- Antentas, J.M.; Vivas, E. Impacto de la crisis en el derecho a una alimentación sana y saludable. Informe SESPAS 2014. Gac. Sanit. 2014, 28 (Suppl. 1), 58–61. [Google Scholar] [CrossRef] [PubMed]
- Knai, C.; Nolte, E.; Brunn, M.; Elissen, A.; Conklin, A.; Pedersen, J.P.; Brereton, L.; Erler, A.; Frølich, A.; Flamm, M.; et al. Reported barriers to evaluation in chronic care: Experiences in six European countries. Health Policy 2013, 110, 220–228. [Google Scholar] [CrossRef]
- Ravaut, M.; Sadeghi, H.; Leung, K.K.; Volkovs, M.; Kornas, K.; Harish, V.; Watson, T.; Lewis, G.F.; Weisman, A.; Poutanen, T.; et al. Predicting adverse outcomes due to diabetes complications with machine learning using administrative health data. NPJ Digit Med. 2021, 4, 24. [Google Scholar] [CrossRef] [PubMed]
- Lix, L.M.; Yogendran, M.S.; Shaw, S.Y.; Burchill, C.; Metge, C.; Bond, R. Population-based data sources for chronic disease surveillance. Chronic Dis. Can. 2008, 29, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Riedl, R.; Robausch, M.; Berghold, A. The Evaluation of the Effectiveness of Austrians Disease Management Program in Patients with Type 2 Diabetes Mellitus—A Population-Based Retrospective Cohort Study. PLoS ONE 2016, 11, e0161429. [Google Scholar] [CrossRef] [PubMed]
- Stock, S.; Drabik, A.; Büscher, G.; Graf, C.; Ullrich, W.; Gerber, A.; Lauterbach, K.W.; Lüngen, M. German diabetes management programs improve quality of care and curb costs. Health Aff. 2010, 29, 2197–2205. [Google Scholar] [CrossRef] [PubMed]

| Year | Total Hospital Discharges | Women (%) | Mean Age (Years ± SD) | Discharges with Stroke Diagnosis (%) | Discharges with AMI Diagnostic (%) | Discharges with LLA (%) |
|---|---|---|---|---|---|---|
| 2001 | 319,894 | 49.10% | 70 ± 13 | 9072 (2.84%) | 11,856 (3.71%) | 6001 (1.88%) |
| 2002 | 336,368 | 48.60% | 70 ± 13 | 8961 (2.66%) | 13,417 (3.99%) | 6373 (1.89%) |
| 2003 | 383,294 | 47.90% | 70 ± 13 | 9790 (2.55%) | 15,435 (4.03%) | 6777 (1.77%) |
| 2004 | 404,420 | 47.50% | 71 ± 13 | 9871 (2.44%) | 15,857 (3.92%) | 7058 (1.75%) |
| 2005 | 428,470 | 47.10% | 71 ± 13 | 10,016 (2.34%) | 16,176 (3.78%) | 7034 (1.64%) |
| 2006 | 442,867 | 46.90% | 71 ± 13 | 8930 (2.02%) | 15,312 (3.46%) | 7321 (1.65%) |
| 2007 | 474,985 | 46.30% | 71 ± 13 | 9251 (1.95%) | 15,561 (3.28%) | 7333 (1.54%) |
| 2008 | 500,947 | 46.00% | 72 ± 13 | 9513 (1.9%) | 15,652 (3.12%) | 7604 (1.52%) |
| 2009 | 527,659 | 45.50% | 72 ± 13 | 9421 (1.79%) | 15,925 (3.02%) | 7968 (1.51%) |
| 2010 | 543,567 | 45.10% | 72 ± 13 | 9577 (1.76%) | 15,886 (2.92%) | 7657 (1.41%) |
| 2011 | 558,721 | 44.70% | 72 ±13 | 9560 (1.71%) | 15,858 (2.84%) | 7963 (1.43%) |
| 2012 | 571,454 | 44.40% | 73 ± 13 | 9408 (1.65%) | 16,250 (2.84%) | 7909 (1.38%) |
| 2013 | 585,253 | 44.00% | 73 ± 13 | 9832 (1.68%) | 16,545 (2.83%) | 8085 (1.38%) |
| 2014 | 603,186 | 43.80% | 73 ± 13 | 10,007 (1.66%) | 15,989 (2.65%) | 7858 (1.3%) |
| 2015 | 621,665 | 43.50% | 73 ± 13 | 9825 (1.58%) | 16,050 (2.58%) | 7973 (1.28%) |
| Total | 7,302,750 | 45.70% | 72 ± 13 | 143,034 (1.96%) | 231,769 (3.17%) | 110,914 (1.52%) |
| Indicators of Complications in Diabetes Mellitus | RR (95% CI) | ||
|---|---|---|---|
| Stroke | AMI | LLA | |
| Pre-Strategy Trend | 0.998 (0.997–0.998) | 1.002 (1.001–1.003) | 1.000 (0.999–1.001) |
| Level change after Strategy | 0.917 (0.886–0.951) | 0.874 (0.839–0.911) | |
| Trend change after Strategy | 0.996 (0.995–0.997) | 0.998 (0.997–0.999) | |
| Basal level | 0.005 (0.005–0.005) | 0.006 (0.006–0.007) | 0.003 (0.003–0.003) |
| All models were seasonally adjusted | |||
| Rates × 100.000 inhabitants | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Touya, M.; Carmona, R.; Sarría-Santamera, A. Evaluating the Impact of the Diabetes Mellitus Strategy for the National Health System: An Interrupted Time Series Analysis. Healthcare 2021, 9, 873. https://doi.org/10.3390/healthcare9070873
González-Touya M, Carmona R, Sarría-Santamera A. Evaluating the Impact of the Diabetes Mellitus Strategy for the National Health System: An Interrupted Time Series Analysis. Healthcare. 2021; 9(7):873. https://doi.org/10.3390/healthcare9070873
Chicago/Turabian StyleGonzález-Touya, Marta, Rocío Carmona, and Antonio Sarría-Santamera. 2021. "Evaluating the Impact of the Diabetes Mellitus Strategy for the National Health System: An Interrupted Time Series Analysis" Healthcare 9, no. 7: 873. https://doi.org/10.3390/healthcare9070873
APA StyleGonzález-Touya, M., Carmona, R., & Sarría-Santamera, A. (2021). Evaluating the Impact of the Diabetes Mellitus Strategy for the National Health System: An Interrupted Time Series Analysis. Healthcare, 9(7), 873. https://doi.org/10.3390/healthcare9070873







