Sleep Quality among Breast and Prostate Cancer Patients: A Comparison between Subjective and Objective Measurements
Abstract
:1. Introduction
Related Work
2. Materials and Methods
2.1. Measuring Sleep Quality Levels
- Minimum Score = 0 (better); Maximum Score = 21 (worse).
- Interpretation: PSQI < 5 associated with good sleep quality.
- PSQI ≥ 5 associated with poor sleep quality.
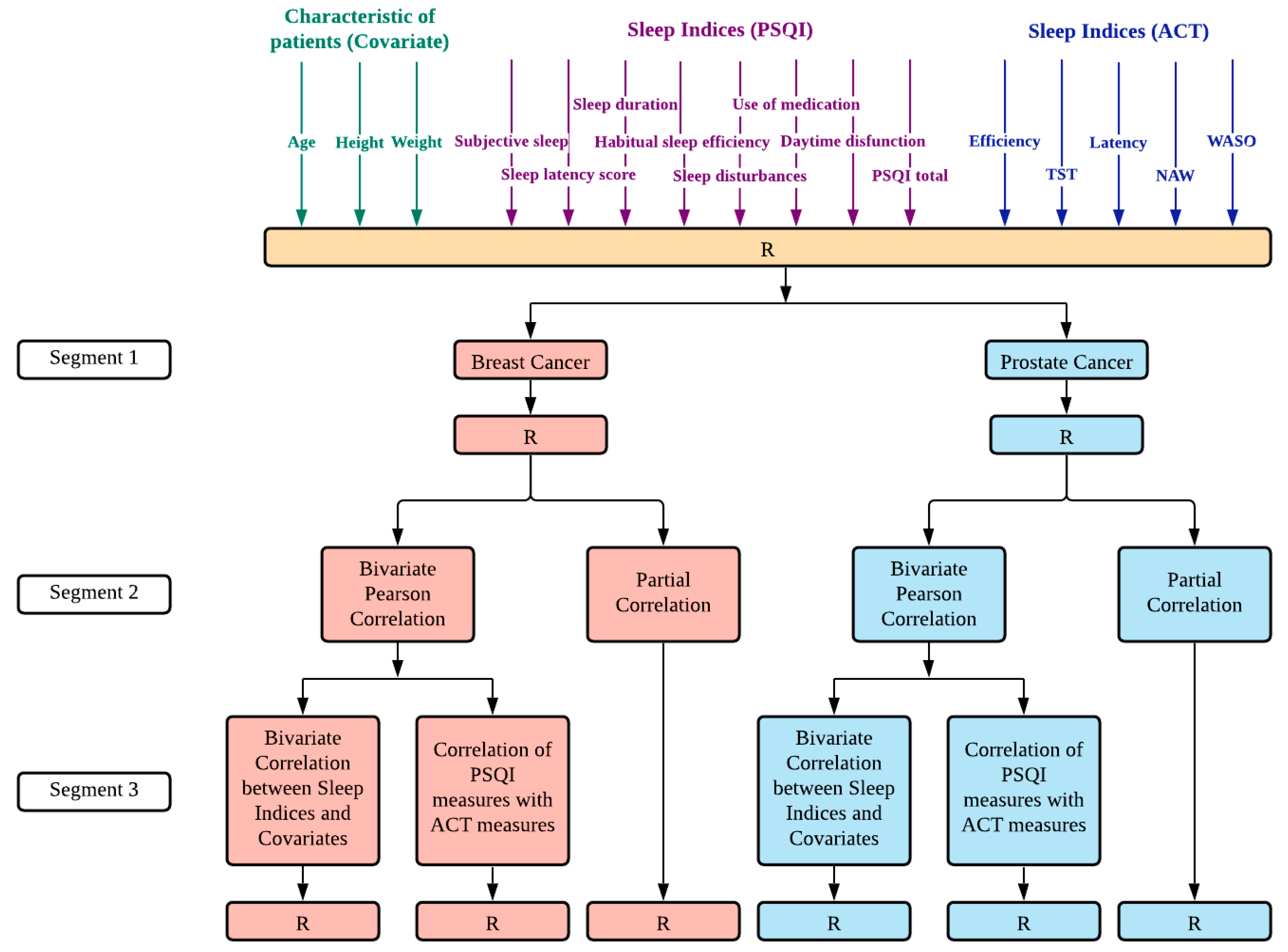
2.1.1. Data Analysis
2.1.2. Comparison of Good vs. Poor Sleep Quality
3. Results
3.1. Descriptive Characteristics
3.2. Bivariate Correlation Analysis between the Sleep Measures and the Covariates of Interest
3.3. Correlations between the Subjective and Objective Sleep Measures
3.4. Cross Tabulation for Sleep Quality Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Health and Welfare Taiwan. Ministry of Health and Welfare Announces Cancer Occurrence Data. Available online: https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=4141&pid=12682 (accessed on 3 June 2021).
- Levine, A.B.; Schlosser, C.; Grewal, J.; Coope, R.; Jones, S.J.M.; Yip, S. Rise of the Machines: Advances in Deep Learning for Cancer Diagnosis. Trends Cancer 2019, 5, 157–169. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Soerjomataram, I.; Ervik, M.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.; Forman, D.; Bray, F. GLOBOCAN 2012 v1. 0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. 2013; IARC: Lyon, France, 2014. [Google Scholar]
- Ghoncheh, M.; Pournamdar, Z.; Salehiniya, H. Incidence and Mortality and Epidemiology of Breast Cancer in the World. Asian Pac. J. Cancer Prev. 2016, 17, 43–46. [Google Scholar] [CrossRef] [Green Version]
- Pernar, C.H.; Ebot, E.M.; Wilson, K.M.; Mucci, L.A. The Epidemiology of Prostate Cancer. Cold Spring Harb. Perspect. Med. 2018, 8, a030361. [Google Scholar] [CrossRef]
- Lawrence, D.P.; Kupelnick, B.; Miller, K.; Devine, D.; Lau, J. Evidence Report on the Occurrence, Assessment, and Treatment of Fatigue in Cancer Patients. J. Natl. Cancer Inst. Monogr. 2004, 2004, 40–50. [Google Scholar] [CrossRef]
- Bower, J.E.; Ganz, P.A.; Desmond, K.A.; Bernaards, C.; Rowland, J.H.; Meyerowitz, B.E.; Belin, T.R. Fatigue in long-term breast carcinoma survivors: A longitudinal investigation. Cancer 2006, 106, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Monga, U.; Kerrigan, A.J.; Thornby, J.; Monga, T.N. Prospective study of fatigue in localized prostate cancer patients undergoing radiotherapy. Radiat. Oncol. Investig. 1999, 7, 178–185. [Google Scholar] [CrossRef]
- Miaskowski, C.; Lee, K.; Dunn, L.; Dodd, M.; Aouizerat, B.E.; West, C.; Paul, S.M.; Cooper, B.; Wara, W.; Swift, P. Sleep-wake circadian activity rhythm parameters and fatigue in oncology patients prior to the initiation of radiation therapy. Cancer Nurs. 2011, 34, 255. [Google Scholar] [CrossRef] [PubMed]
- Lai, X.-Y.; Tang, Z.-M.; Zhu, X.-D.; Li, L.; Qin, X.-Y.; Lan, J.-L.; Lu, C.-P.; Lyu, Z.-C.; Liang, L.-Q.; Chen, L.-J. Sleep Disturbance and Related Factors in Patients with Nasopharyngeal Carcinoma and Their Family Caregivers Prior to the Initiation of Treatment. Sci. Rep. 2018, 8, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Langford, D.J.; Lee, K.; Miaskowski, C. Sleep disturbance interventions in oncology patients and family caregivers: A comprehensive review and meta-analysis. Sleep Med. Rev. 2012, 16, 397–414. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.R.; Fontes, F.; Pereira, S.; Gonçalves, M.; Azevedo, A.; Lunet, N. Impact of breast cancer treatments on sleep disturbances—A systematic review. Breast 2014, 23, 697–709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzalez, B.D.; Lu, Q. Sleep disturbance among Chinese breast cancer survivors living in the USA. Support. Care Cancer 2018, 26, 1695–1698. [Google Scholar] [CrossRef] [PubMed]
- Savard, J.; Simard, S.; Hervouet, S.; Ivers, H.; Lacombe, L.; Fradet, Y. Insomnia in men treated with radical prostatectomy for prostate cancer. Psychol. Oncol. 2004, 14, 147–156. [Google Scholar] [CrossRef]
- Dirksen, S.R.; Epstein, D.R.; Hoyt, M.A. Insomnia, depression, and distress among outpatients with prostate cancer. Appl. Nurs. Res. 2009, 22, 154–158. [Google Scholar] [CrossRef]
- Otte, J.L.; Carpenter, J.S.; Manchanda, S.; Rand, K.L.; Skaar, T.C.; Weaver, M.T.; Chernyak, Y.; Zhong, X.; Igega, C.; Landis, C. Systematic review of sleep disorders in cancer patients: Can the prevalence of sleep disorders be ascertained? Cancer Med. 2014, 4, 183–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carpenter, J.S.; Elam, J.L.; Ridner, S.H.; Carney, P.H.; Cherry, G.J.; Cucullu, H.L. Sleep, Fatigue, and Depressive Symptoms in Breast Cancer Survivors and Matched Healthy Women Experiencing Hot Flashes. Oncol. Nurs. Forum 2004, 31, 591–598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fortner, B.V.; Stepanski, E.J.; Wang, S.C.; Kasprowicz, S.; Durrence, H. Sleep and Quality of Life in Breast Cancer Patients. J. Pain Symptom Manag. 2002, 24, 471–480. [Google Scholar] [CrossRef]
- Hershman, D.L.; Unger, J.M.; Wright, J.D.; Ramsey, S.D.; Till, C.; Tangen, C.M.; Barlow, W.E.; Blanke, C.D.; Thompson, I.M.; Hussain, M. Adverse Health Events Following Intermittent and Continuous Androgen Deprivation in Patients With Metastatic Prostate Cancer. JAMA Oncol. 2016, 2, 453–461. [Google Scholar] [CrossRef]
- Koskderelioglu, A.; Gedizlioglu, M.; Ceylan, Y.; Gunlusoy, B.; Kahyaoglu, N. Quality of sleep in patients receiving androgen deprivation therapy for prostate cancer. Neurol. Sci. 2017, 61, 1079–1451. [Google Scholar] [CrossRef]
- Mitteldorf, D.; Nelms, J. Are prostate cancer treatments correlated to sleep distress? J. Clin. Oncol. 2018, 36, 347. [Google Scholar] [CrossRef]
- Orr, W.C. Utilization of Polysomnography in the Assessment of Sleep Disorders. Med. Clin. N. Am. 1985, 69, 1153–1167. [Google Scholar] [CrossRef]
- De Weerd, A.W. Actigraphy, the alternative way? Front. Psychiatry 2014, 5, 155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richardson, S.J. A comparison of tools for the assessment of sleep pattern disturbance in critically ill adults. Dimens. Crit. Care Nurs. DCCN 1997, 16, 226–242, quiz 240-2. [Google Scholar] [CrossRef]
- Beck, S.L.; Schwartz, A.L.; Towsley, G.; Dudley, W.; Barsevick, A. Psychometric evaluation of the Pittsburgh sleep quality index in cancer patients. J. Pain Symptom Manag. 2004, 27, 140–148. [Google Scholar] [CrossRef]
- Landry, G.J.; Best, J.R.; Liu-Ambrose, T. Measuring sleep quality in older adults: A comparison using subjective and objective methods. Front. Aging Neurosci. 2015, 7, 166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carney, C.E.; Buysse, D.J.; Ancoli-Israel, S.; Edinger, J.D.; Krystal, A.D.; Lichstein, K.L.; Morin, C.M. The Consensus Sleep Diary: Standardizing Prospective Sleep Self-Monitoring. Sleep 2012, 35, 287–302. [Google Scholar] [CrossRef] [Green Version]
- Littner, M.; Hirshkowitz, M.; Kramer, M.; Kapen, S.; Anderson, W.M.; Bailey, D.; Berry, R.B.; Davila, D.; Johnson, S.; Kushida, C.; et al. Practice Parameters for Using Polysomnography to Evaluate Insomnia: An Update. Sleep 2003, 26, 754–760. [Google Scholar] [CrossRef] [Green Version]
- Ancoli-Israel, S.; Cole, R.; Alessi, C.; Chambers, M.; Moorcroft, W.; Pollak, C.P. The Role of Actigraphy in the Study of Sleep and Circadian Rhythms. Sleep 2003, 26, 342–392. [Google Scholar] [CrossRef] [Green Version]
- Kanady, J.C.; Drummond, S.P.A.; Mednick, S. Actigraphic assessment of a polysomnographic-recorded nap: A validation study. J. Sleep Res. 2011, 20, 214–222. [Google Scholar] [CrossRef]
- Marino, M.; Li, Y.; Rueschman, M.N.; Winkelman, J.W.; Ellenbogen, J.M.; Solet, J.M.; Dulin, H.; Berkman, L.F.; Buxton, O.M. Measuring Sleep: Accuracy, Sensitivity, and Specificity of Wrist Actigraphy Compared to Polysomnography. Sleep 2013, 36, 1747–1755. [Google Scholar] [CrossRef]
- Grandner, M.A.; Kripke, D.F.; Yoon, I.-Y.; Youngstedt, S.D. Criterion validity of the Pittsburgh Sleep Quality Index: Investigation in a non-clinical sample. Sleep Biol. Rhythms 2006, 4, 129–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grutsch, J.F.; Wood, P.A.; Du-Quiton, J.; Reynolds, J.L.; Lis, C.G.; Levin, R.D.; Daehler, M.A.; Gupta, D.; Quiton, D.F.T.; Hrushesky, W.J. Validation of actigraphy to assess circadian organization and sleep quality in patients with advanced lung cancer. J. Circadian Rhythm. 2011, 9, 4. [Google Scholar] [CrossRef] [Green Version]
- Kreutz, C.; Müller, J.; Schmidt, M.E.; Steindorf, K. Comparison of subjectively and objectively assessed sleep problems in breast cancer patients starting neoadjuvant chemotherapy. Support. Care Cancer 2021, 29, 1015–1023. [Google Scholar] [CrossRef]
- Kuo, T.B.J.; Li, J.-Y.; Chen, C.-Y.; Lin, Y.-C.; Tsai, M.-W.; Lin, S.-P.; Yang, C.C.H. Influence of Accelerometer Placement and/or Heart Rate on Energy Expenditure Prediction during Uphill Exercise. J. Mot. Behav. 2017, 50, 127–133. [Google Scholar] [CrossRef]
- Smith, M.T.; McCrae, C.S.; Cheung, J.; Martin, J.L.; Harrod, C.G.; Heald, J.L.; Carden, K.A. Use of Actigraphy for the Evaluation of Sleep Disorders and Circadian Rhythm Sleep-Wake Disorders: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2018, 14, 1231–1237. [Google Scholar] [CrossRef] [Green Version]
- Martin, J.L.; Hakim, A.D. Wrist Actigraphy. Chest 2011, 139, 1514–1527. [Google Scholar] [CrossRef]
- Gorny, S.; Allen, R.; Krausman, D.; Earley, C. Parametric analyses of factors affecting accuracy for detection of wake epochs after sleep onset based on wrist activity data. Sleep Res. 1996, 25, 490. [Google Scholar]
- Tsai, P.-S.; Wang, S.-Y.; Wang, M.-Y.; Su, C.-T.; Yang, T.-T.; Huang, C.-J.; Fang, S.-C. Psychometric Evaluation of the Chinese Version of the Pittsburgh Sleep Quality Index (CPSQI) in Primary Insomnia and Control Subjects. Qual. Life Res. 2005, 14, 1943–1952. [Google Scholar] [CrossRef] [PubMed]
- Sobolewska-Wlodarczyk, A.; Wlodarczyk, M.; Banasik, J.; Gasiorowska, A.; Wisniewska-Jarosinska, M.; Fichna, J. Sleep disturbance and disease activity in adult patients with inflammatory bowel diseases. J. Physiol. Pharmacol. Off. J. Pol. Physiol. Soc. 2018, 69, 423–428. [Google Scholar]
- Kaaz, K.; Szepietowski, J. Influence of Itch and Pain on Sleep Quality in Patients with Hidradenitis Suppurativa. Acta Derm. Venereol. 2018, 98, 757–761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, D.; Dongying, C.; Fang, B. Measurements and status of sleep quality in patients with cancers. Support. Care Cancer 2018, 26, 405–414. [Google Scholar] [CrossRef]
- Sitnick, S.L.; Goodlin-Jones, B.L.; Anders, T.F. The Use of Actigraphy to Study Sleep Disorders in Preschoolers: Some Concerns about Detection of Nighttime Awakenings. Sleep 2008, 31, 395–401. [Google Scholar] [CrossRef]
- Kang, H. The prevention and handling of the missing data. Korean J. Anesthesiol. 2013, 64, 402–406. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Fontes, F.; Gonçalves, M.; Maia, S.; Pereira, S.; Severo, M.; Lunet, N. Reliability and validity of the Pittsburgh Sleep Quality Index in breast cancer patients. Support. Care Cancer 2017, 25, 3059–3066. [Google Scholar] [CrossRef] [Green Version]
- Jakobsen, G.; Engstrøm, M.; Thronæs, M.; Løhre, E.T.; Kaasa, S.; Fayers, P.; Hjermstad, M.J.; Klepstad, P. Sleep quality in hospitalized patients with advanced cancer: An observational study using self-reports of sleep and actigraphy. Support. Care Cancer 2019, 28, 2015–2023. [Google Scholar] [CrossRef] [PubMed]
- Dhruva, A.; Paul, S.M.; Cooper, B.A.; Lee, K.; West, C.; Aouizerat, B.E.; Dunn, L.B.; Swift, P.S.; Wara, W.; Miaskowski, C. A Longitudinal Study of Measures of Objective and Subjective Sleep Disturbance in Patients with Breast Cancer Before, During, and After Radiation Therapy. J. Pain Symptom Manag. 2012, 44, 215–228. [Google Scholar] [CrossRef] [PubMed]
- Beck, S.L.; Berger, A.M.; Barsevick, A.M.; Wong, B.; Stewart, K.A.; Dudley, W.N. Sleep quality after initial chemotherapy for breast cancer. Support. Care Cancer 2010, 18, 679–689. [Google Scholar] [CrossRef] [Green Version]
- Madsen, M.T.; Huang, C.; Gögenur, I. Actigraphy for measurements of sleep in relation to oncological treatment of patients with cancer: A systematic review. Sleep Med. Rev. 2015, 20, 73–83. [Google Scholar] [CrossRef]
- Rogers, L.Q.; Courneya, K.S.; Oster, R.A.; Anton, P.M.; Robbs, R.S.; Forero, A.; McAuley, E. Physical activity and sleep quality in breast cancer survivors: A randomized trial. Med. Sci. Sports Exerc. 2017, 49, 2009. [Google Scholar] [CrossRef] [PubMed]
- Otte, J.L.; Payne, J.K.; Carpenter, J.S. Nighttime Variability in Wrist Actigraphy. J. Nurs. Meas. 2011, 19, 105–114. [Google Scholar] [CrossRef]
- Berger, A.M.; Wielgus, K.K.; Young-McCaughan, S.; Fischer, P.; Farr, L.; Lee, K.A. Methodological Challenges When Using Actigraphy in Research. J. Pain Symptom Manag. 2008, 36, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Dean, G.E.; Redeker, N.S.; Wang, Y.-J.; Rogers, A.E.; Dickerson, S.S.; Steinbrenner, L.M.; Gooneratne, N.S. Sleep, Mood, and Quality of Life in Patients Receiving Treatment for Lung Cancer. Oncol. Nurs. Forum 2013, 40, 441–451. [Google Scholar] [CrossRef] [Green Version]
- Parliament, E. Directive 2002/58/EC of the European Parliament and of the Council of 12 July 2002 concerning the processing of personal data and the protection of privacy in the electronic communications sector. Off. J. Eur. Communities 2002, 201, 37–47, At 37 (Directive on Privacy and Electronic Communications) 2002. [Google Scholar]
- Parliament, E. Directive 95/46/EC on the protection of individuals with regard to the processing of personal data and on the free movement of such data. Off. J. Eur. Communities 1995, 281, 31. [Google Scholar]
- Mountford, N.; Zubiete, E.D.; Kessie, T.; Garcia-Zapirain, B.; Nuño-Solinis, R.; Coyle, D.; Munksgaard, K.B.; Fernandez-Luque, L.; Romero, O.R.; Fernandez, M.M.; et al. Activating Technology for Connected Health in Cancer: Protocol for a Research and Training Program. JMIR Res. Protoc. 2018, 7, e14. [Google Scholar] [CrossRef] [PubMed]

| Breast Cancer (n = 16) | Prostate Cancer (n = 15) | |||
|---|---|---|---|---|
| Variable | Mean (SD) | Range | Mean (SD) | Range |
| Age (years) | 60.0000 (8.79) | 45.00–76.00 | 75.13(12.65) | 59.00–99.00 |
| Height (cm) | 156.2125 (5.26) | 148.20–163.00 | 165.23 (8.43) | 141.00–180.00 |
| Weight (kg) | 60.17 (9.83) | 49.00–85.00 | 70.84 (6.39) | 59.00–80.00 |
| (PSQI) What time to bed (time in hh:mm) | 21:54 (5:10) | 20:00–2:30 | 22:24 (1:12) | 20:00–24:00 |
| (PSQI) What time out of bed (time in h:mm) | 6:58 (1:05) | 5:00–8:30 | 6:09 (0:53) | 4:30–8:00 |
| (PSQI) Subjective sleep quality (score, 0–3) | 1.13 (0.72) | 0–3 | 1 (0.854) | 0–2 |
| (PSQI) Sleep latency score (score, 0–3) | 0.73 (1.03) | 0–3 | 1.00 (0.85) | 0–2 |
| (PSQI) Sleep duration (score, 0–3) | 0.56 (0.63) | 0–2 | 1.13 (1.19) | 0–3 |
| (PSQI) Habitual sleep efficiency (score, 0–3) | 0.13 (0.34) | 0–1 | 0.60 (0.91) | 0–3 |
| (PSQI) Sleep disturbances (score, 0–3) | 1.38 (0.50) | 1–2 | 0.40 (0.63) | 0–2 |
| (PSQI) Use of medication (score, 0–3) | 0.31 (0.79) | 0–3 | 1.60 (0.63) | 1–3 |
| (PSQI) Daytime dysfunction (score, 0–3) | 0.38 (0.81) | 0–3 | 0.93 (1.22) | 0–3 |
| (PSQI) Total hours of sleep (time in h:mm) | 7:33 (1:29) | 5:00–10:30 | 7:14 (1:29) | 4:00–10:00 |
| PSQI Total (score, 0–21) | 4.88 (2.28) | 2–9 | 5.93 (1.62) | 4–10 |
| ACT efficiency (score, 0–100) | 71.4475 (9.23) | 55.82–85.90 | 62.26 (12.32) | 41.57–84.94 |
| ACT TST (time in h:mm:ss) | 5:46:33 (1:20:30) | 3:17:21–7:35:22 | 4:50:13 (1:14:37) | 2:43:20–6:49:54 |
| ACT Latency (time in h:mm:ss) | 0:32:21 (0:26:06) | 0:03:44–1:44:18 | 0:30:15 (0:26:51) | 0:02:05–1:50:32 |
| ACT NAW (number of awakenings) | 12.80 (4.34) | 6.60–20.86 | 13.06(3.30) | 7.86–20.43 |
| ACT WASO (time in h:mm:ss) | 1:52:22 (0:49:40) | 0:51:16–3:17:16 | 2:07:37 (0:36:45) | 1:05:41–3:35:25 |
| Breast Cancer | Prostate Cancer | |||||
|---|---|---|---|---|---|---|
| Sleep Indices | Covariates | Covariates | ||||
| Age | Height | Weight | Age | Height | Weight | |
| Subjective sleep quality (PSQI) | −0.042 | −0.145 | −0.232 | 0.087 | 0.185 | −0.088 |
| Sleep latency score (PSQI) | −0.319 | −0.357 | −0.475 | 0.251 | 0.070 | 0.235 |
| Sleep duration (PSQI) | 0.193 | −0.004 | −0.148 | −0.231 | 0.007 | 0.116 |
| Habitual sleep efficiency (PSQI) | 0.333 | 0.121 | −0.170 | −0.382 | 0.033 | 0.359 |
| Sleep disturbances (PSQI) | 0.091 | 0.366 | 0.119 | 0.096 | −0.020 | 0.024 |
| Use of medication (PSQI) | 0.105 | −0.384 | −0.178 | 0.250 | 0.192 | 0.011 |
| Daytime dysfunction (PSQI) | −0.122 | 0.310 | 0.336 | 0.154 | 0.057 | −0.497 |
| PSQI Total | −0.070 | −0.319 | −0.416 | 0.219 | 0.318 | 0.209 |
| ACT efficiency | −0.238 | 0.062 | −0.059 | 0.060 | −0.161 | −0.270 |
| ACT TST | −0.180 | 0.107 | −0.177 | 0.099 | −0.142 | −0.043 |
| ACT Latency | 0.077 | 0.064 | 0.025 | −0.001 | 0.193 | 0.182 |
| ACT NAW | 0.079 | 0.020 | −0.032 | 0.229 | −0.212 | −0.254 |
| ACT WASO | 0.223 | 0.000 | −0.055 | −0.127 | 0.210 | 0.308 |
| PSQI Measures—Breast Cancer | ||||||||
|---|---|---|---|---|---|---|---|---|
| ACT Measures | Subjective Sleep Quality | Sleep Latency Score | Sleep Duration | Habitual Sleep Efficiency | Sleep Disturbances | Use of Medication | Daytime Dysfunction | PSQI Total |
| ACT efficiency | 0.281/0.254 | 0.062/−0.128 | 0.230/0.366 | 0.156/0.261 | 0.108/0.012 | −0.263/−0.320 | 0.521 */0.654 * | 0.480/0.504 |
| ACT TST | 0.311/0.261 | 0.308/0.248 | −0.534 */−0.604 * | 0.444/0.502 | 0.149/0.016 | −0.021/−0.033 | −0.017/0.049 | 0.196/0.084 |
| ACT Latency | 0.100/0.190 | 0.254/0.523 | −0.225/−0.322 | −0.046/−0.054 | −0.196/−0.149 | 0.110/0.195 | −0.477/−0.645 * | −0.198/−0.097 |
| ACT NAW | −0.134/−0.188 | −0.018/−0.039 | −0.388/−0.457 | 0.259/0.195 | 0.081/−0.017 | −0.098/−0.137 | −0.251/−0.227 | −0.299/−0.453 |
| ACT WASO | −0.158/−0.187 | 0.014/0.132 | −0.487/−0.663 * | 0.225/0.084 | 0.195/0.198 | 0.361/0.392 | −0.287/−0.258 | −0.209//−0288 |
| ACT measures | PSQI Measures—Prostate Cancer | |||||||
| ACT efficiency | −0.294/−0.318 | −0.172/−0.105 | −0.152/−0.144 | −0.045/0.037 | 0.442/0.474 | 0.356/0.440 | −0.116/−0.286 | 0.026/0.148 |
| ACT TST | −0.105/−0.090 | 0.015/0.003 | −0.501/−0.509 | −0.109/−0.099 | 0.626 */0.628 * | 0.304/0.340 | −0.001/0.006 | 0.105/0.149 |
| ACT Latency | 0.414/0.415 | 0.097/0.024 | −0.022/−0.020 | −0.163/−0.221 | −0.212/−0.231 | −0.449/−0.568 | 0.384/0.541 | −0.102/−0.255 |
| ACT NAW | −0.087/−0.101 | −0.071/−0.066 | −0.228/−0.190 | −0.104/0.017 | −0.321/−0.353 | 0.211/0.229 | 0.044/−0.071 | −0.219/−0.214 |
| ACT WASO | 0.023/0.026 | 0.061/−0.012 | −0.071/−0.112 | 0.194/−0.112 | −0.223/−0.241 | −0.014/−0.047 | 0.080/0.260 | 0.018/−0.095 |
| PSQI Sleep Category | ||||
|---|---|---|---|---|
| Category | Breast Cancer | |||
| Good | Poor | Total | ||
| ACT | Good | 0 | 1 | 1 |
| Poor | 8 | 1 | 9 | |
| Average | 2 | 4 | 6 | |
| Total | 10 | 6 | 16 | |
| p value | 0.027 | |||
| X2 | 7.253 | |||
| Prostate Cancer | ||||
| ACT | Good | 0 | 0 | 0 |
| Poor | 4 | 8 | 12 | |
| Average | 2 | 1 | 3 | |
| Total | 6 | 9 | 15 | |
| p value | 0.693 | |||
| X2 | 0.156 | |||
| Breast Cancer | ||||
| Variable | Underestimate on PSQI n = 5 | Accurate on PSQI n = 1 | Overestimate on PSQI n = 10 | p value |
| Mean (SD) or n (%) | Mean (SD) or n (%) | Mean (SD) or n (%) | ||
| Age | 59.60 (8.20366) | 56 (-) | 60.60 (9.83418) | 0.891 |
| Height | 156.54 (4.96065) | 150 (-) | 156.67 (5.53374) | 0.507 |
| Weight | 55.36 (5.36172) | 49 (-) | 63.70 (10.38214) | 0.152 |
| Prostate Cancer | ||||
| Underestimate on PSQI n = 1 | Accurate on PSQI n = 8 | Overestimate on PSQI n = 6 | p value | |
| Mean (SD) or n (%) | Mean (SD) or n (%) | Mean (SD) or n (%) | ||
| Age | 99.00 (-) | 75.25 (11.39862) | 71.00 (11.48913) | 0.118 |
| Height | 163.10 (-) | 167.88 (2.86294) | 162.07 (12.79166) | 0.461 |
| Weight | 69.90 (-) | 71.79 (7.49027) | 69.73 (5.74584) | 0.849 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barsasella, D.; Syed-Abdul, S.; Malwade, S.; Kuo, T.B.J.; Chien, M.-J.; Núñez-Benjumea, F.J.; Lai, G.-M.; Kao, R.-H.; Shih, H.-J.; Wen, Y.-C.; et al. Sleep Quality among Breast and Prostate Cancer Patients: A Comparison between Subjective and Objective Measurements. Healthcare 2021, 9, 785. https://doi.org/10.3390/healthcare9070785
Barsasella D, Syed-Abdul S, Malwade S, Kuo TBJ, Chien M-J, Núñez-Benjumea FJ, Lai G-M, Kao R-H, Shih H-J, Wen Y-C, et al. Sleep Quality among Breast and Prostate Cancer Patients: A Comparison between Subjective and Objective Measurements. Healthcare. 2021; 9(7):785. https://doi.org/10.3390/healthcare9070785
Chicago/Turabian StyleBarsasella, Diana, Shabbir Syed-Abdul, Shwetambara Malwade, Terry B. J. Kuo, Ming-Jen Chien, Francisco J. Núñez-Benjumea, Gi-Ming Lai, Ruey-Ho Kao, Hung-Jen Shih, Yu-Ching Wen, and et al. 2021. "Sleep Quality among Breast and Prostate Cancer Patients: A Comparison between Subjective and Objective Measurements" Healthcare 9, no. 7: 785. https://doi.org/10.3390/healthcare9070785
APA StyleBarsasella, D., Syed-Abdul, S., Malwade, S., Kuo, T. B. J., Chien, M.-J., Núñez-Benjumea, F. J., Lai, G.-M., Kao, R.-H., Shih, H.-J., Wen, Y.-C., Li, Y.-C., Carrascosa, I. P., Bai, K.-J., Broekhuizen, Y. C. B., & Jaspers, M. W. M. (2021). Sleep Quality among Breast and Prostate Cancer Patients: A Comparison between Subjective and Objective Measurements. Healthcare, 9(7), 785. https://doi.org/10.3390/healthcare9070785








