Sources of Care Stress of Nursing Staff for Patients with Infectious Diseases during the Prevalence of COVID-19: A Case Study of Some Regional Teaching Hospitals in Southern Taiwan
Abstract
1. Introduction
2. Materials and Methods
- (1)
- Patient Care
- (2)
- Infection Protection
- (3)
- Support System
3. Results
4. Discussion
4.1. Clinical Symptoms of Patients in Isolation Wards Cannot Be Closely Tracked
4.2. The Duration of Treatment Is Extended and the Workload Becomes Heavier
4.3. After Entering the Isolation Ward, Nursing Staff Cannot Handle Any Other Patient Who Is Ringing the Call Bell in Time
4.4. Worrying about Being Infected while Caring for Patients with Infectious Diseases
4.5. Worrying about whether the Current Protective Equipment Can Provide Protection
4.6. Not Being Familiar with the Samples of Infectious Diseases to Be Tested
4.7. Support from Family/Colleagues
4.8. Care Stress Resulting from Unfamiliarity with Infectious Diseases That Have Not Been Cared for Previously
5. Conclusions and Suggestions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benoliel, J.Q.; McCorkle, R.; Georgiadou, F.; Denton, T.; Spitzer, A. Measurement of stress in clinical nursing. Cancer Nurs. 1990, 13, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Vehedian-Azimi, A.; Hajiesmaeili, M.; Kangasnieme, M.; Fornes-Vives, J.; Hunsucker, R.L.; Radhimibashar, F.; Pourhoseingholi, M.A.; Farrokhvar, L.; Miller, A.C. Effects of Stress on Critical Care Nurses: A National Cross-Sectional Study. J. Intensive Care Med. 2019, 34, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.A.; Chung, J.W.; Wong, T.K. Learning from the severe acute respiratory syndrome (SARS) epidemic. J. Clin. Nurs. 2008, 17, 1023–1034. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Morgan, D.J.; Day, H.R.; Harris, A.D.; Furuno, J.P.; Perencevich, E.N. The impact of contact isolation on the quality of inpatient hospital care. PLoS ONE 2011, 6, e22190. [Google Scholar] [CrossRef][Green Version]
- Chen, K.T.; Twu, S.J.; Chang, H.L.; Wu, Y.C.; Chen, C.T.; Lin, T.H.; Olsen, S.J.; Dowell, S.F.; Su, I.J. SARS in Taiwan: An overview and lessons learned. Int. J. Infect. Dis. 2005, 9, 77–85. [Google Scholar] [CrossRef]
- McGrath, A.; Reid, N.; Boore, J. Occuptional stress in nursing. Int. J. Nurs. Stud. 2003, 40, 555–565. [Google Scholar] [CrossRef]
- Norouzi, R.; Dargahi, S.; Aeyadi, N.; Sarhaddi, M. The association between workplace spirituality and Job Stress with occupational ethics through mediating role of Job Enthusiasm among nurses in Zahedan City, 2017. J. Occup. Health Epidemiol. 2018, 7, 3–10. [Google Scholar] [CrossRef][Green Version]
- Lambert, V.A.; Lambert, C.E.; Misae, I. Workplace stressors, ways of copingand demographic characteristics as predictors of physical and mental health of Japanese nurses. Int. J. Nurs. Stud. 2004, 41, 85–97. [Google Scholar] [CrossRef]
- Wong, T.W.; Yau, K.Y.; Chan, L.W.; Kwong, S.Y.; Ho, M.Y.; Lau, C.C. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur. J. Emerg. Med. 2005, 12, 13–18. [Google Scholar] [CrossRef]
- Roets, L.; Ziady, L.E. The nurses’ experience of possible HIV infection after injury and/or exposure on duty. Curationis 2018, 31, 13–23. [Google Scholar] [CrossRef][Green Version]
- Maunder, R.; Hunter, J.; Vincent, L.; Bennett, J.; Peladeau, N.; Leszcz, M.; Mazzulli, T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Cmaj 2003, 168, 1245–1251. [Google Scholar]
- Chapman, R.; Styles, I. An epidemic of abuse and violence: Nurse on the front line. Accid. Emerg. Nurs. 2006, 14, 245–249. [Google Scholar] [CrossRef]
- Howard, B.E. High-Risk Aerosol-Generating Procedures in COVID-19: Respiratory Protective Equipment Considerations. Otolaryngol. Head Neck Surg. 2020, 163, 98–103. [Google Scholar] [CrossRef]
- WHO. Rational Use of Personal Protective Equipment for Coronavirus Disease 2019 (COVID-19), 2020, Interim Guidance, 27 February 2020. Available online: https://apps.who.int/iris/handle/10665/331215 (accessed on 31 January 2021).
- Ferguson, J.K. Preventing healthcare-associated infection: Risks, healthcare systems and behavior. Intern. Med. J. 2009, 39, 574–581. [Google Scholar] [CrossRef]
- Hassan, Z.M.; Wahsheh, M.A. Knowledge and attitudes of Jordanian nurses towards patients with HIV/ AIDS: Findings from a nationwide survey. Issues Mental Health Nurs. 2011, 32, 774–784. [Google Scholar] [CrossRef]
- Costa, J.C.T.D.; Silva, R.; Ferreira, J.; Nienhaus, A. Active tuberculosis among health care workers in Portugal. J. Bras Pneumol. 2011, 37, 636–645. [Google Scholar] [CrossRef]
- Arnetz, J.E.; Goetz, C.M.; Sudan, S.; Arble, E.; Janisse, J.; Arnetz, B.B. Personal Protective Equipment and Mental Health Symptoms Among Nurses During the COVID-19 Pandemic. J. Occup. Environ. Med. 2020, 62, 892–897. [Google Scholar] [CrossRef]
- Hou, T.; Zhang, T.; Cai, W.; Xiangrui, S.X.; Chen, A.; Deng, G.; Ni, C. Social support and mental health among health care workers during Coronavirus Disease 2019 outbreak: A moderated mediation model. PLoS ONE 2020, 15, e0233831. [Google Scholar] [CrossRef]
- Okoli, C.; Pawlowski, S.D. The Delphi method as a research tool: An example, design considerations and applications. Inf. Manag. 2004, 42, 15–29. [Google Scholar] [CrossRef]
- Ishizaka, A.; Balkenborg, D.G.; Kaplan, T. Influence of aggregation and measurement scale on ranking a compromise alternative in AHP. J. Oper. Res. Soc. 2009, 62, 15–29. [Google Scholar] [CrossRef][Green Version]
- Barron, F.H.; Barrett, B.E. The efficacy of SMARTER—Simple Multi-Attribute Rating Technique Extended to Ranking. Acta Psychol. 1996, 93, 23–36. [Google Scholar] [CrossRef]
- Hall, L.M.; Angue, J.; Peter, E.; BrienPallas, L.; Wynn, F. Media portrayal of nurses’ perspectives and concerns in the SARS crisis in Toronto. J. Nurs. Sch. 2003, 35, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Nickell, L.A.; Crighton, E.J.; Tracy, C.S.; Al-Enazy, H.; Bolaji, Y.; Hanjrah, S.; Hussain, A.; Makhlouf, S.; Upshur, R.E.G. Psychosocial effects of SARS on hospital staff: Survey of a large tertiary care institution. Can. Med. Assoc. J. 2004, 170, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.Y.; Chen, S.H.; Yu, H.Y.; Lou, J.H. Job stress, achievement motivation and occupational burnout among male nurses. J. Adv. Nurs. 2010, 66, 1592–1601. [Google Scholar] [CrossRef]
- Moszczynski, A.B.; Haney, C.J. Stress and coping of Canadian rural nurses caring for trauma patients who are transferred out. J. Emerg. Nurs. 2002, 28, 496–504. [Google Scholar] [CrossRef]
- McCann, T.V. Willingness to provide care and treatment for patients with HIV/AIDS. J. Adv. Nurs. 1997, 25, 1033–1039. [Google Scholar] [CrossRef]
- Hu, S.H.; Yu, Y.M.; Chang, W.Y.; Lin, Y.K. Social support and factors associated with self-efficacy among acute-care nurse practitioners. J. Clin. Nurs. 2018, 27, 876–882. [Google Scholar] [CrossRef]
- Bartram, T.; Joiner, T.A.; Stanton, P. Factors affecting the job stress and job satisfaction of Australian nurses: Implications for recruitment and retention. Contemp. Nurse 2004, 17, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Steinhardt, M.A.; Dolbier, C.L.; Gottlieb, N.H.; McCalister, K.T. The Relationship between hardiness, suspervisor support, Group cohesion, and job stress as predicitors of job satisfaction. Am. J. Health Promot. 2003, 17, 382–389. [Google Scholar] [CrossRef]
- Pinkert, C.; Faul, E.; Saxer, S.; Burgstaller, M.; Kamleithner, D.; Mayer, H. Experiences of nurses with the care of patients with dementia in acute hospitals: A secondary analysis. J. Clin. Nurs. 2018, 27, 162–172. [Google Scholar] [CrossRef]
- Taiwan Centers for Disease Control. Taiwan Epidemiology Bulletin. Available online: https://www.cdc.gov.tw/EpidemicTheme/Detail/wRe2wQO2JCW83hbs2HNztA?archiveId=JLUiHLlTbOrD_h4H8rFReA (accessed on 20 February 2021).
| Category | Item |
|---|---|
| Patient care | 1. Clinical symptoms of patients in isolation wards cannot be closely tracked. |
| 2. After entering the isolation ward, the nursing staff cannot handle any other patient who is ringing the call bell in time. | |
| 3. The duration of treatment is extended and the workload becomes heavier. | |
| 4. Care stress resulting from unfamiliarity with infectious diseases that have not been cared for previously. | |
| 5. Inconsistency in operating standards causes problems. | |
| 6. Not familiar with the samples of infectious diseases to be tested. | |
| Infection protection | 7. Worrying about whether the current protective equipment can protect you. |
| 8. Worrying about being infected while caring for patients with infectious diseases. | |
| 9. Fear of being contaminated while wearing or taking off protective equipment. | |
| 10. It is inconvenient and inflexible to work in isolation clothes and gloves. | |
| 11. When you are alone with a patient in an isolation ward, you will worry about your own safety. | |
| 12. Fear of spreading an infection to your family. | |
| Support system | 13. Support from family/colleagues. |
| 14. Support from patients’ families and assistance from the medical team. |
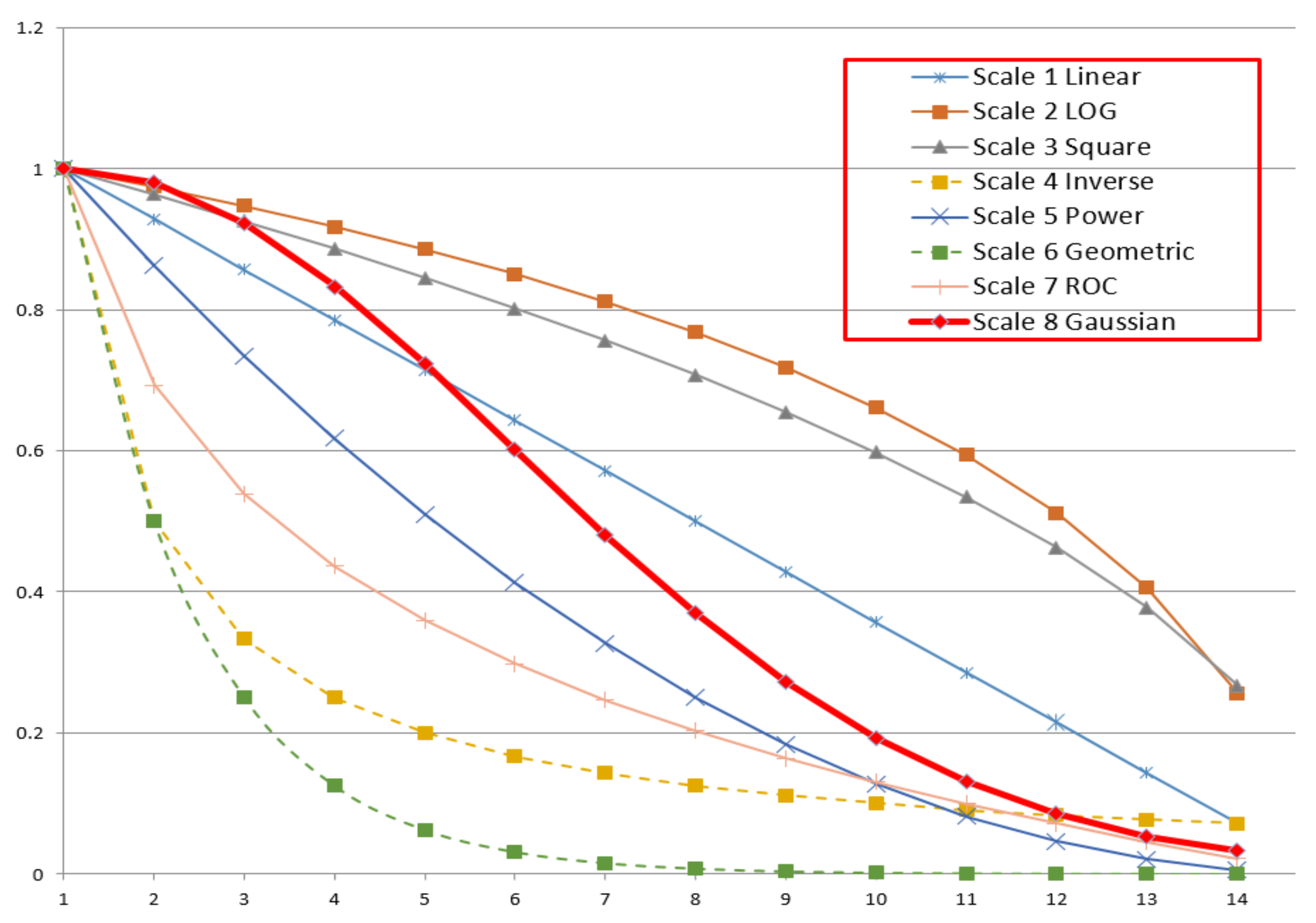
| No | Scale | Value | Weight (Wm) |
|---|---|---|---|
| 1 | Linear (Saaty, 1977) | Vm = (Np + 1 − m) | Wm = Vm/V1 |
| 2 | Logarithmic | Vm = | Wm = Vm/V1 |
| 3 | Root Square (Harker and Vargas, 1987) | Vm = | Wm = Vm/V1 |
| 4 | Inverse Linear (Ma and Zheng, 1991) | Np/m | Wm = Vm/V1 |
| 5 | Power (Harker and Vargas, 1987) | Vm = (Np + 1 − m)2 | Wm = Vm/V1 |
| 6 | Geometric (Lootsma, 1989) | Vm = | Wm = Vm/V1 |
| 7 | Rank-Order Centroid (ROC) | Vm = | Wm = Vm/V1 |
| 8 | Gaussian Function | Vm = c = −(Np − 1)2/ln(1/(Nt − 1)) | Wm = Vm |
| No | Scale | V1/VNp |
|---|---|---|
| 1 | Linear (Saaty, 1977) | 14 |
| 2 | Logarithmic | 3.91 |
| 3 | Root Square (Harker and Vargas,1987) | 3.74 |
| 4 | Inverse Linear (Ma and Zheng, 1991) | 14 |
| 5 | Power (Harker and Vargas,1987) | 196 |
| 6 | Geometric (Lootsma, 1989) | 8192 |
| 7 | ROC | 45.52 |
| 8 | Gaussian function | 31 |
| Item | Respondent | |||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | F | |
| 1 | 5 | 5 | 2 | 2 | 1 | 1 |
| 2 | 1 | 1 | 5 | 3 | 2 | 3 |
| 3 | 2 | 3 | 1 | 1 | 4 | 2 |
| 4 | 4 | 2 | 3 | 5 | 5 | 4 |
| 5 | 3 | 4 | 4 | 4 | 3 | 5 |
| Respondent | Average | Index | ||||||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | |||
| 1 | 0.2 | 0.2 | 0.904 | 0.904 | 1 | 1 | 0.713 | 3 |
| 2 | 1 | 1 | 0.2 | 0.669 | 0.904 | 0.669 | 0.740 | 2 |
| 3 | 0.904 | 0.669 | 1 | 1 | 0.404 | 0.904 | 0.814 | 1 |
| 4 | 0.404 | 0.904 | 0.669 | 0.2 | 0.2 | 0.404 | 0.464 | 4 |
| 5 | 0.669 | 0.404 | 0.404 | 0.404 | 0.669 | 0.2 | 0.458 | 5 |
| Attribute of Item | Average Weight | Ranking |
|---|---|---|
| 1. Clinical symptoms of patients in isolation wards cannot be closely tracked. | 0.934 | 1 |
| 3. The duration of treatment is extended and the workload becomes heavier. | 0.780 | 2 |
| 2. After entering the isolation ward, the nursing staff cannot handle any other patient who is ringing the call bell in time. | 0.774 | 3 |
| 8. Worrying about being infected while caring for patients with infectious diseases. | 0.716 | 4 |
| 7. Worrying about whether the current protective equipment can protect you. | 0.587 | 5 |
| 6. Not familiar with the samples of infectious diseases to be tested. | 0.577 | 6 |
| 13. Support from family/colleagues. | 0.555 | 7 |
| 4. Care stress resulting from unfamiliarity with infectious diseases that have not been cared for previously. | 0.466 | 8 |
| 9. Fear of being contaminated while wearing or taking off protective equipment. | 0.448 | 9 |
| 11. When you are alone with a patient in an isolation ward, you will worry about your own safety. | 0.433 | 10 |
| 5. Inconsistency in operating standards causes problems. | 0.420 | 11 |
| 9. Fear of spreading an infection to your family. | 0.244 | 12 |
| 14. Support from patients’ families and assistance from the medical team. | 0.200 | 13 |
| 10. It is inconvenient and inflexible to work in isolation clothes and gloves. | 0.091 | 14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Y.; Yu, L. Sources of Care Stress of Nursing Staff for Patients with Infectious Diseases during the Prevalence of COVID-19: A Case Study of Some Regional Teaching Hospitals in Southern Taiwan. Healthcare 2021, 9, 462. https://doi.org/10.3390/healthcare9040462
Huang Y, Yu L. Sources of Care Stress of Nursing Staff for Patients with Infectious Diseases during the Prevalence of COVID-19: A Case Study of Some Regional Teaching Hospitals in Southern Taiwan. Healthcare. 2021; 9(4):462. https://doi.org/10.3390/healthcare9040462
Chicago/Turabian StyleHuang, Yichao, and Lichen Yu. 2021. "Sources of Care Stress of Nursing Staff for Patients with Infectious Diseases during the Prevalence of COVID-19: A Case Study of Some Regional Teaching Hospitals in Southern Taiwan" Healthcare 9, no. 4: 462. https://doi.org/10.3390/healthcare9040462
APA StyleHuang, Y., & Yu, L. (2021). Sources of Care Stress of Nursing Staff for Patients with Infectious Diseases during the Prevalence of COVID-19: A Case Study of Some Regional Teaching Hospitals in Southern Taiwan. Healthcare, 9(4), 462. https://doi.org/10.3390/healthcare9040462






