Socio-Epidemiological Factors with Negative Impact on Infant Morbidity, Mortality Rates, and the Occurrence of Birth Defects
Abstract
1. Introduction
2. Sources of Information and Aim of the Study
3. Birth Defects and Causal Factors
4. Parents’ Socio-Occupational Status and Lifestyle
5. Recommended Nutrition during Pregnancy
6. Antenatal Diagnosis and Therapeutic Abortion
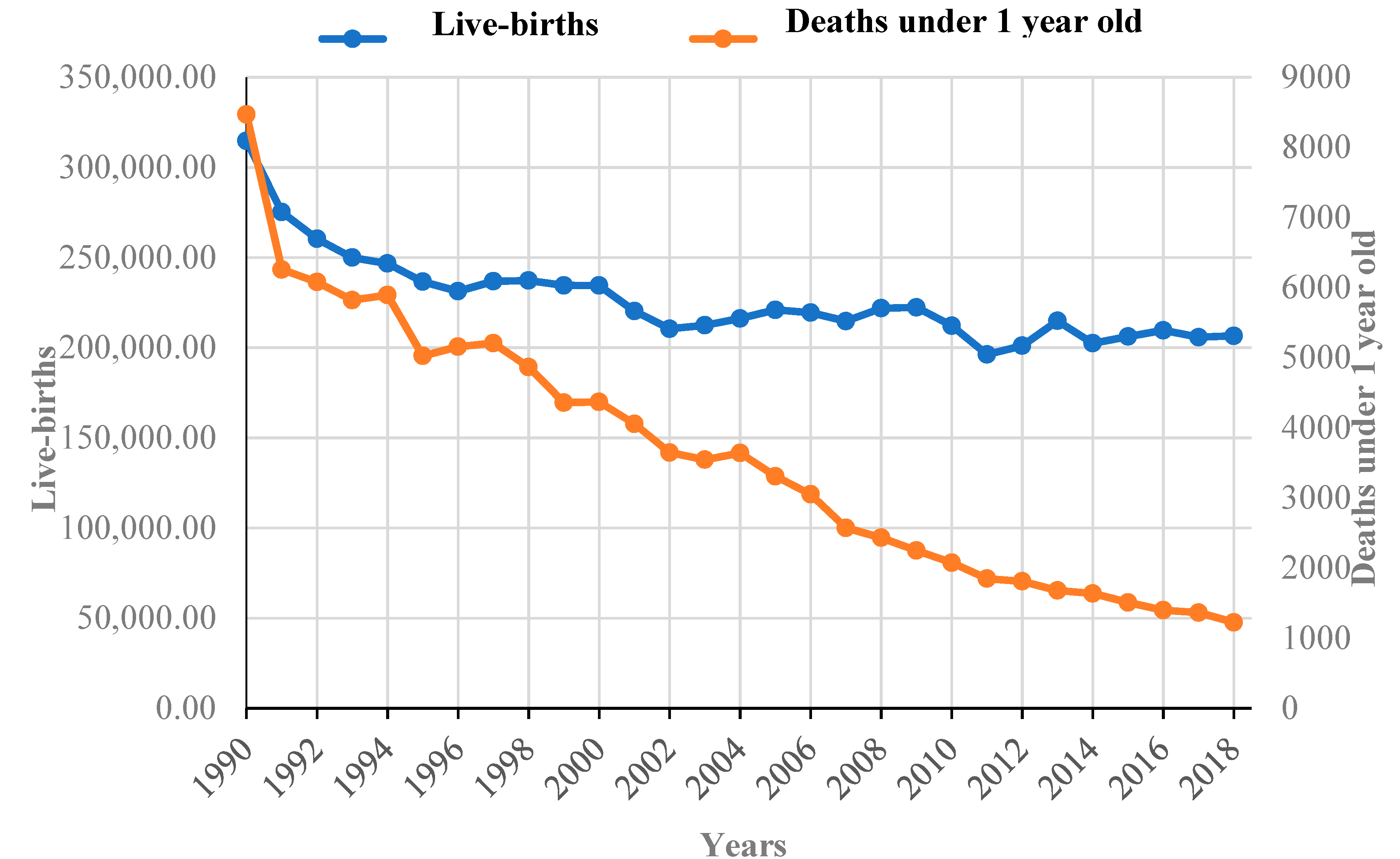
7. Preventive Measures to Reduce Perinatal Mortality and Long-Term Morbidity
8. Neonatal Morbidity and Mortality Rates in Romania
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Schneider, M.C.; Castillo-Salgado, C.; Loyola-Elizondo, E.; Bacallao, J.; Mujica, O.J.; Vidaurre, M.; Alleyne, G. Trends in infant mortality inequalities in the Americas: 1955–1995. J. Epidemiol. Community Health 2002, 56, 538–541. [Google Scholar] [CrossRef]
- Hertel-Fernandez, A.W.; Giusti, A.E.; Sotelo, J.M. The Chilean infant mortality decline: Improvement for whom? Socioeconomic and geographic inequalities in infant mortality, 1990–2005. Bull. World Health Organ. 2007, 85, 798–804. [Google Scholar] [PubMed]
- WHO. Make Every Mother and Child Count; The World Health Report 2005; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Lawn, J.; Cousens, S.; Bhutta, Z.; Darmstadt, G.; Martines, J.; Paul, V. Why are 4 million newborn babies dying each year? Lancet 2004, 364, 399–401. [Google Scholar] [CrossRef]
- Bhutta, Z.A.; Das, J.K.; Bahl, R.; Lawn, J.E.; Salam, R.A.; Paul, V.K.; Sankar, M.J.; Blencowe, H.; Rizvi, A.; Chou, V.B.; et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet 2014, 384, 347–370. [Google Scholar] [CrossRef]
- Wang, H.; Liddell, C.A.; Coates, M.M.; Mooney, M.D.; Levitz, C.E.; Schumacher, A.E.; Apfel, H.; Iannarone, M.; Phillips, B.; Lofgren, K.T.; et al. Global, regional, and national levels of neonatal, infant, and under- 5 mortality during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 957–979. [Google Scholar] [CrossRef]
- Lawn, J.E.; Blencowe, H.; Oza, S.; You, D.; Lee, A.C.; Waiswa, P.; Lalli, M.; Bhutta, Z.; Barros, A.J.; Christian, P.; et al. Every Newborn: Progress, priorities, and potential beyond survival. Lancet 2014, 384, 189–205. [Google Scholar] [CrossRef]
- Varela, M.M.; Nohr, E.A.; Llopis-González, A.; Andersen, A.M.; Olsen, J. Socio-occupational status and congenital anomalies. Eur. J. Public Health 2009, 19, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Laisk, T.; Soares, A.; Ferreira, T.; Painter, J.N.; Censin, J.C.; Laber, S.; Bacelis, J.; Chen, C.Y.; Lepamets, M.; Lin, K.; et al. The genetic architecture of sporadic and multiple consecutive miscarriage. Nat. Commun. 2020, 11, 5980. [Google Scholar] [CrossRef]
- Jarvis, G.E. Misjudging early embryo mortality in natural human reproduction. F1000Research 2020, 9, 702. [Google Scholar] [CrossRef]
- Țarcă, E.; Criscov, I.G.; Murgu, A.M.; Duceac, L.D.; Savu, B. Psychological effects and ethical implications of the prenatal diagnosis of severe malformation in the fetus. Med. Surg. J. 2019, 123, 166–174. [Google Scholar]
- Ţarcă, E.; Ciongradi, I.; Aprodu, S.G. Birth Weight, Compromised Bowel and Sepsis are the Main Variables Significantly Influencing Outcome in Gastroschisis. Chirurgia 2015, 110, 151–156. [Google Scholar]
- Rajangam, S.; Devi, R. Consagunity and chromosomal abnormality in mental retardation and or multiple congenital anomalies. J. Anat. Soc. India 2007, 56, 30–33. [Google Scholar]
- Yang, Q.; Wen, S.W.; Leader, A.; Chen, X.K.; Lipson, J.; Walker, M. Paternal age and birth defects: How strong is the association? Hum. Reprod. 2007, 22, 696–701. [Google Scholar] [CrossRef] [PubMed]
- Calzolari, E.; Bianchi, F.; Dolk, H.; Milan, M.; EUROCAT Group. Omphalocele and gastroschisis in Europe: A survey of 3 million births 1980–1990. Am. J. Med. Genet. 1995, 58, 187–194. [Google Scholar] [CrossRef]
- Reefhuis, J.; Honein, M.A. Maternal age and non-chromosomal birth defects, Atlanta-1968-2000: Teenager or thirty-something, who is at risk? Birth Defects Res. Part A Clin. Mol. Teratol. 2004, 70, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Stoll, W.C.; Alembik, Y.; Dott, B.; Roth, M.P. Risk factors in abdominal wall defects (omphalocele and gastroschisis): A study in a series of 265 858 consecutive birth. Ann. Genet. 2001, 44, 201–208. [Google Scholar] [CrossRef]
- Kaleche, K.D.; Bierlich, A.; Hammer, H.; Bollmann, R. Is unexplained third trimester intrauterine death of fetuses with gastroschisis caused by umbilical cord compression due to acute extra-abdominal bowel dilatation? Prenat. Diagn. 2002, 22, 715–717. [Google Scholar] [CrossRef] [PubMed]
- Ramiro-Cortijo, D.; Herrera, T.; Rodríguez-Rodríguez, P.; López De Pablo, Á.L.; De La Calle, M.; López-Giménez, M.R.; Mora-Urda, A.I.; Gutiérrez-Arzapalo, P.Y.; Gómez-Rioja, R.; Aguilera, Y.; et al. Maternal plasma antioxidant status in the first trimester of pregnancy and development of obstetric complications. Placenta 2016, 47, 37–45. [Google Scholar] [CrossRef]
- Reutter, H.; Boyadjiev, S.A.; Gambhir, L.; Ebert, A.K.; Rosch, W.H.; Stein, R.; Schroder, A.; Boemers, T.M.; Bartels, E.; Vogt, H.; et al. Phenotype severity in the bladder exstrophy-epispadias complex: Analysis of genetic and nongenetic contributing factors in 441 families from North America and Europe. J. Pediatr. 2011, 15, 825–831. [Google Scholar] [CrossRef]
- Wood, H.M.; Babineau, D.; Gearhart, J.P. In vitro fertilization and the cloacal/bladder exstrophy-epispadias complex: A continuing association. J. Pediatr. Urol. 2007, 3, 305–310. [Google Scholar] [CrossRef]
- Ebert, A.K.; Reutter, H.; Ludwig, M.; Rosch, W.H. The exstrophy-epispadias complex. Orphanet J. Rare Dis. 2009, 4, 23. [Google Scholar] [CrossRef]
- Murray, J.C. Face facts: Genes, environment, and clefts. Am. J. Hum. Genet. 1995, 57, 227–232. [Google Scholar]
- Vargesson, N. Thalidomide-induced teratogenesis: History and mechanisms. Birth Defects Res. C Embryo Today 2015, 105, 140–156. [Google Scholar] [CrossRef] [PubMed]
- Torfs, C.P.; Katz, E.A.; Bateson, T.F.; Lam, P.K.; Curry, C.J. Maternal medications and environmental exposures as risk factors for gastroschisis. Teratology 1996, 54, 84–92. [Google Scholar] [CrossRef]
- Eros, E.; Czeizel, A.E.; Rockenbauer, M.; Sorensen, H.T.; Olsen, J. A population-based case-control teratologic study of nitrazepam, medazepam, tofisopam, alprazolum and clonazepam treatment during pregnancy. Eur. J. Obs. Gynecol. Reprod. Biol. 2002, 101, 147–154. [Google Scholar] [CrossRef]
- Waller, D.K.; Gallaway, M.S.; Taylor, L.G.; Ramadhani, T.A.; Canfield, M.A.; Scheuerle, A.; Hernandez-Diaz, S.; Louik, C.; Correa, A.; National Birth Defects Prevention Study. Use of oral contraceptives in pregnancy and major structural birth defects in offspring. Epidemiology 2010, 21, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Materna-Kiryluk, A.; Więckowska, B.; Wiśniewska, K.; Czyżewska, M.; Godula-Stuglik, U.; Baumert, M.; Margol, R.; Latos-Bielenska, A. Geospatial clustering of gastroschisis in Poland: Data from the Polish Registry of Congenital Malformations (PRCM). Int. J. Occup. Med. Environ. Health 2016, 29, 461–470. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Elliott, P.; Briggs, D.; Morris, S.; de Hoogh, C.; Hurt, C.; Jensen, T.K.; Maitland, I.; Richardson, S.; Wakefield, J.; Jarup, L. Risk of adverse birth outcomes in populations living near landfill sites. BMJ 2001, 323, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Ritz, B.; Yu, F.; Fruin, S.; Chapa, G.; Shaw, G.M.; Harris, J.A. Ambient air pollution and risk of birth defects in southern California. Am. J. Epidemiol. 2002, 155, 17–25. [Google Scholar] [CrossRef]
- Bhutta, A.Z.; Hafeez, A. What can Pakistan do to address maternal and child health over the next decade? Health Res. Policy Syst. 2015, 13, 49. [Google Scholar] [CrossRef]
- Enweronu-Laryea, C.; Dickson, K.E.; Moxon, S.G.; Simen-Kapeu, A.; Nyange, C.; Niermeyer, S.; Begin, F.; Sobel, H.L.; Lee, A.C.C.; von Xylander, S.; et al. Basic newborn care and neonatal resuscitation: A multi-country analysis of health system bottlenecks and potential solutions. BMC Pregnancy Childbirth 2015, 15, 4. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.C.; Cousens, S.; Wall, S.N.; Niermeyer, S.; Darmstadt, G.L.; Carlo, W.A.; Keenan, W.J.; Bhutta, Z.A.; Gill, C.; Lawn, J.E. Neonatal resuscitation and immediate newborn assessment and stimulation for the prevention of neonatal deaths: A systematic review, meta-analysis and Delphi estimation of mortality effect. BMC Public Health 2011, 11, S12. [Google Scholar] [CrossRef] [PubMed]
- Bang, A.; Bang, R.; Baitule, S.; Reddy, H.; Deshmukh, M. Effect of home-based neonatal care and management of sepsis on neonatal mortality: Field trial in rural India. Lancet 1999, 354, 1955–1961. [Google Scholar] [CrossRef]
- Draper, E.S.; Rankin, J.; Tonks, A.M.; Abrams, K.R.; Field, D.J.; Clarke, M.; Kurinczuk, J.J. Recreational drug use: A major risk factor for gastroschisis? Am. J. Epidemiol. 2008, 167, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Forrester, M.B.; Merz, R.D. Comparison of trends in gastroschisis and prenatal illicit drug use rates. J.Toxicol. Environ. Health A 2006, 69, 1253–1259. [Google Scholar] [CrossRef]
- Werler, M.M.; Sheehan, J.E.; Mitchell, A.A. Maternal medication use and risks of Gastroschisis and small intestinal atresia. Am. J. Epidemiol. 2002, 155, 26–31. [Google Scholar] [CrossRef]
- Feldkamp, M.L.; Carmichael, S.L.; Shaw, G.M.; Panichello, J.D.; Moore, C.A.; Botto, L.D. Maternal nutrition and gastroschisis: Findings from the National Birth Defects Prevention Study. Am. J. Obs. Gynecol. 2011, 204, e401–e404. [Google Scholar] [CrossRef]
- Botto, L.D.; Mulinare, J.; Erickson, J.D. Occurrence of omphalocele in relation to maternal multivitamin use: A population-based study. Pediatrics 2002, 109, 904–908. [Google Scholar] [CrossRef]
- Ionescu-Ittu, R.; Marelli, A.J.; Mackie, A.S.; Pilote, L. Prevalence of severe congenital heart disease after folic acid fortification of grain products: Time trend analysis in Quebec, Canada. BMJ 2009, 338, b1673. [Google Scholar] [CrossRef]
- Van Allen, M.I.; McCourt, C.; Lee, N.S. Preconception Health: Folic Acid for the Primary Prevention of Neural Tube Defects. A Resource Document for Health Professionals; Cat. Number H39-607/ 2002E; Minister of Public Works and Government Services Canada: Ottawa, ON, Canada, 2002. [Google Scholar]
- Blencowe, H.; Cousens, S.; Modell, B.; Lawn, J. Folic acid to reduce neonatal mortality from neural tube disorders. Int. J. Epidemiol. 2010, 39, i110–i121. [Google Scholar] [CrossRef]
- Koletzko, B.; Godfrey, K.M.; Poston, L.; Szajewska, H.; van Goudoever, J.B.; de Waard, M.; Brands, B.; Grivell, R.M.; Deussen, A.R.; Dodd, J.M.; et al. Nutrition During Pregnancy, Lactation and Early Childhood and its Implications for Maternal and Long-Term Child Health: The Early Nutrition Project Recommendations. Ann. Nutr. Metab. 2019, 74, 93–106. [Google Scholar] [CrossRef]
- Cooper, C.; Harvey, N.C.; Bishop, N.J.; Kennedy, S.; Papageorghiou, A.T.; Schoenmakers, I.; Fraser, R.; Gandhi, S.V.; Carr, A.; D’Angelo, S.; et al. Maternal gestational vitamin D supplementation and offspring bone health (MAVIDOS): A multicentre, double-blind, randomised placebo-controlled trial. Lancet. Diabetes Endocrinol. 2016, 4, 393–402. [Google Scholar]
- Aite, L.; Trucchi, A.; Nahom, A.; Spina, V.; Bilancioni, E.; Bagolan, P. Multidisciplinary management of fetal surgical anomalies: The impact on maternal anxiety. Eur. J. Pediatr. Surg. 2002, 12, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Czeizel, A.; Intody, Z.; Modell, B. What proportion of congenital abnormalities can be prevented. BMJ 1993, 306, 499–503. [Google Scholar] [CrossRef] [PubMed]
- Correa-Villasenor, A.; Cragan, J.; Kucik, J.; O’Leary, L.; Siffel, C.; Williams, L. The metropolitan atlanta congenital defects program: 35 years of birth defects surveillance at the centers for disease control and prevention. Birth Defects Res. A Clin. Mol. Teratol. 2003, 67, 617–624. [Google Scholar] [CrossRef]
- Requejo, J.; Merialdi, M.; Althabe, F.; Keller, M.; Katz, J.; Menon, R. Born too soon: Care during pregnancy and childbirth to reduce preterm deliveries and improve health outcomes of the preterm baby. Reprod. Health 2013, 10, S4. [Google Scholar] [CrossRef] [PubMed]
- Mwansa-Kambafwile, J.; Cousens, S.; Hansen, T.; Lawn, J.E. Antenatal steroids in preterm labour for the prevention of neonatal deaths due to complications of preterm birth. Int. J. Epidemiol. 2010, 39, i122–i133. [Google Scholar] [CrossRef]
- Rubens, C.E.; Gravett, M.G.; Victora, C.G.; Nunes, T.M.; GAPPS Review Group. Global report on preterm birth and stillbirth (7 of 7): Mobilizing resources to accelerate innovative solutions (Global Action Agenda). BMC Pregnancy Childbirth 2010, 10, S7. [Google Scholar] [CrossRef] [PubMed]
- Kochhar, S.; Edwards, K.M.; Ropero Alvarez, A.M.; Moro, P.L.; Ortiz, J.R. Introduction of new vaccines for immunization in pregnancy—Programmatic, regulatory, safety and ethical considerations. Vaccine 2019, 37, 3267–3277. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Guo, L.; Li, B.X.; Deng, M.; Wen, F.; Jiang, J.H.; Tan, Y.Q.; Song, Y.Z.; Liu, Z.H.; Zhang, C.H.; Kobayashi, K.; et al. Etiological analysis of neurodevelopmental disabilities: Single-center eight-year clinical experience in south China. J. Biomed. Biotechnol. 2011, 2011, 318616. [Google Scholar] [CrossRef] [PubMed]
- Wiley, V.; Webster, D.; Loeber, G. Screening Pathways through China, the Asia Pacific Region, the World. Int. J. Neonatal Screen 2019, 5, 26. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Public Health. Romania. Available online: https://cnsisp.insp.gov.ro/wp-content/uploads/2019/01/MORTALITATEA-INFANTILA-2017.pdf (accessed on 17 March 2021).
- National Institute for Statistics. Romania 1998–2018. TEMPO-Online Database. Available online: http://statistici.insse.ro:8077/tempo-online/#/pages/tables/insse-table (accessed on 12 March 2021).
- Pop, T.L.; Burlea, M.; Falup-Pecurariu, O.; Borzan, C.; Gabor-Harosa, F.; Herdea, V.; Pop, C.F.; Rajka, D.; Ognean, M.L.; Căinap, S.S. Overview of the pediatric healthcare system in Romania. Turk. Pediatri. Ars. 2020, 55, 69–84. [Google Scholar] [CrossRef]
- Țarcă, V. Specific Approaches to the Methodology of the Industrial Production Index Calculation at County Level. Rom. Stat. Rev. 2017, 65, 31–46. [Google Scholar]
- Iacob, A.I.; Cristache, S.E.; Ungureanu, D. The analysis of the main macroeconomic indicators which characterize the Romanian health system. Procedia Econ. Financ. 2015, 26, 522–527. [Google Scholar] [CrossRef]
- Ţarcă, E.; Aprodu, S. Past and present in omphalocele treatment in Romania. Chirurgia 2014, 109, 507–513. [Google Scholar]
- Sitkin, N.A.; Ozgediz, D.; Donkor, P.; Farmer, D.L. Congenital anomalies in low- and middle-income countries: The unborn child of global surgery. World J. Surg. 2015, 39, 36–40. [Google Scholar] [CrossRef]
| Key Factors of Neonatal Morbidity and Mortality | Lack of Sexual Education and Primary Care Education | Parents’ Socio-Occupational Status | Chromosomal Abnormalities, Birth Defects, and Metabolic Diseases | Miscarriage and Intrauterine Deaths | Perinatal Infections |
|---|---|---|---|---|---|
| Possible preventive health measures | - sexual education and family planning - primary education, where children learn what a healthy and balanced life means, with long-term consequences - promoting a healthy lifestyle, starting with the primary education of children and continuing with the involvement of the church and the media | - reducing the pollution specific to residential areas - implementation of simple but essential requirements for hygiene and newborn survival - educating women in rural areas on minimal healthcare for at-home deliveries - social and financial support for disadvantaged mothers | - proper family planning - avoiding the consumption of toxic foods, alcohol, tobacco, and drugs - periconceptional supplementation of folic acid, vitamin B12, and other vitamins - maintaining a normal body mass index - neonatal screening for metabolic diseases - improving access to medical services and improving the rate of the antenatal diagnosis of malformations | - careful monitoring of problematic pregnancies - home monitoring and frequent ultrasound scans - administration of antenatal corticosteroids to pregnant women at high risk of preterm birth - emergency caesarean section if necessary | - antibiotic treatment for preterm premature rupture of the membranes - screening for and treatment of sexually transmitted diseases including HIV and other infections - immunization during pregnancy |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ţarcă, E.; Roșu, S.T.; Cojocaru, E.; Trandafir, L.; Luca, A.C.; Rusu, D.; Ţarcă, V. Socio-Epidemiological Factors with Negative Impact on Infant Morbidity, Mortality Rates, and the Occurrence of Birth Defects. Healthcare 2021, 9, 384. https://doi.org/10.3390/healthcare9040384
Ţarcă E, Roșu ST, Cojocaru E, Trandafir L, Luca AC, Rusu D, Ţarcă V. Socio-Epidemiological Factors with Negative Impact on Infant Morbidity, Mortality Rates, and the Occurrence of Birth Defects. Healthcare. 2021; 9(4):384. https://doi.org/10.3390/healthcare9040384
Chicago/Turabian StyleŢarcă, Elena, Solange Tamara Roșu, Elena Cojocaru, Laura Trandafir, Alina Costina Luca, Daniela Rusu, and Viorel Ţarcă. 2021. "Socio-Epidemiological Factors with Negative Impact on Infant Morbidity, Mortality Rates, and the Occurrence of Birth Defects" Healthcare 9, no. 4: 384. https://doi.org/10.3390/healthcare9040384
APA StyleŢarcă, E., Roșu, S. T., Cojocaru, E., Trandafir, L., Luca, A. C., Rusu, D., & Ţarcă, V. (2021). Socio-Epidemiological Factors with Negative Impact on Infant Morbidity, Mortality Rates, and the Occurrence of Birth Defects. Healthcare, 9(4), 384. https://doi.org/10.3390/healthcare9040384







