Blood Pressure Awareness and Knowledge of Cardio-Cerebrovascular Diseases in South Korean Women with Hypertension
Abstract
1. Introduction
2. Methods
2.1. Participants and Data Collection
2.2. Variables
2.2.1. Knowledge of CVDs’ Warning Signs and Awareness of Their Blood Pressure Level
2.2.2. Health-Related Quality of Life and Subjective Health Status
2.2.3. Depression
2.2.4. General Characteristics
2.3. Statistical Analysis
3. Results
3.1. General Characteristics According to AoBP
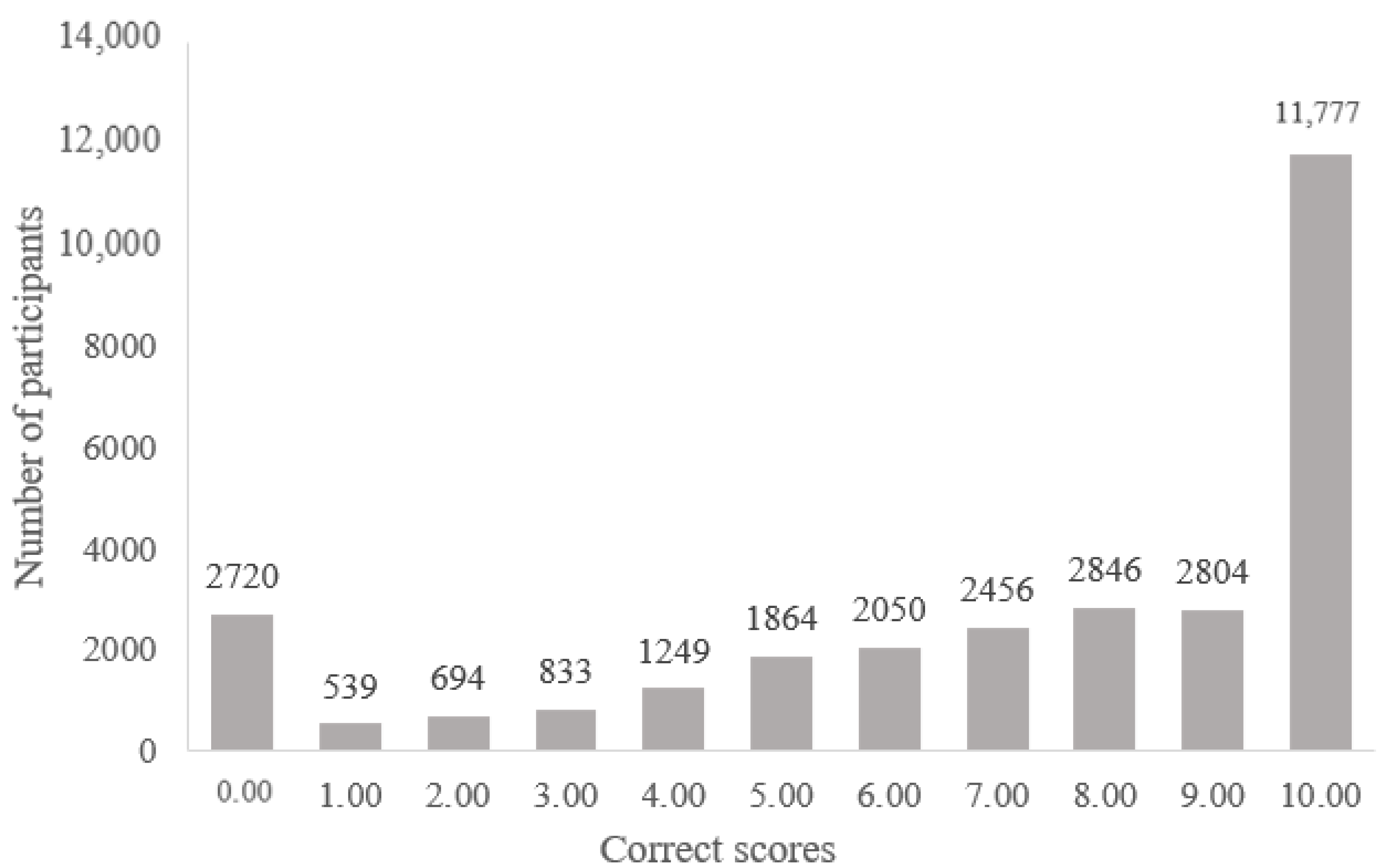
3.2. Level of KCVDs in Adult Women with Hypertension
3.3. Factors Associated with KCVDs and AoBP
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Keteepe-Arachi, T.; Sharma, S. Cardiovascular Disease in Women: Understanding Symptoms and Risk Factors. Eur. Cardiol. 2017, 12, 10–13. [Google Scholar] [CrossRef]
- Garcia, M.; Mulvagh, S.L.; Bairey Merz, C.N.; Buring, J.E.; Manson, J.E. Cardiovascular disease in women: Clinical perspectives. Circ. Res. 2016, 118, 1273–1293. [Google Scholar] [CrossRef]
- World Health Organization. Cardiovascular Disease (CVDs). Available online: https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1 (accessed on 21 December 2020).
- Statistics Korea. 2018 Annual Report on the Cause of Death Statistics; Statistics Korea: Deajeon, Korea, 2019; pp. 1–40. [Google Scholar]
- Ministry of Health and Welfare. Korea Health Statistic 2019: Korea National Health and Nutrition Examination Survey (KNHANES VIII-1), 1st ed.; Ministry of Health and Welfare, & Korea Disease Control and Prevention Agency: Sejong, Korea, 2020; pp. 1–326. [Google Scholar]
- Statistics Korea. Cause of Death Statistics. Available online: http://kostat.go.kr/portal/eng/pressReleases/8/10/index.board?bmode=read&bSeq=&aSeq=385629&pageNo=1&rowNum=10&navCount=10&currPg=&searchInfo=&sTarget=title&sTxt= (accessed on 22 December 2020).
- Smith, S.C., Jr.; Collins, A.; Ferrari, R.; Holmes, D.R., Jr.; Logstrup, S.; McGhie, D.V.; Ralston, J.; Sacco, R.L.; Stam, H. Our time: A call to save preventable death from cardiovascular disease (heart disease and stroke). Eur. Heart J. 2012, 33, 2910–2916. [Google Scholar] [CrossRef] [PubMed]
- Woodward, M. Cardiovascular disease and the female disadvantage. Int. J. Environ. Res. Public Health 2019, 16, 1165. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-T.; Fonarow, G.C.; Smith, E.E.; Reeves, M.J.; Navalkele, D.D.; Grotta, J.C.; Grau-Sepulveda, M.V.; Hernandez, A.F.; Peterson, E.D.; Schwamm, L.H. Treatment with tissue plasminogen activator in the golden hour and the shape of the 4.5-hour time-benefit curve in the national United States Get With The Guidelines-Stroke population. Circulation 2017, 135, 128–139. [Google Scholar] [CrossRef] [PubMed]
- Arrebola-Moreno, M.; Petrova, D.; Garrido, D.; Ramírez-Hernández, J.A.; Catena, A.; Garcia-Retamero, R. Psychosocial markers of pre-hospital decision delay and psychological distress in acute coronary syndrome patients. Br. J. Health Psychol. 2020, 25, 305–323. [Google Scholar] [CrossRef] [PubMed]
- Kimura, K.; Kimura, T.; Ishihara, M.; Nakagawa, Y.; Nakao, K.; Miyauchi, K.; Sakamoto, T.; Tsujita, K.; Hagiwara, N.; Miyazaki, S. JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ. J. 2019, 83, 1085–1196. [Google Scholar] [CrossRef]
- Ahn, H.M.; Kim, H.; Lee, K.S.; Lee, J.H.; Jeong, H.S.; Chang, S.H.; Lee, K.R.; Kim, S.H.; Shin, E.Y. Hospital Arrival Rate within Golden Time and Factors Influencing Prehospital Delays among Patients with Acute Myocardial Infarction. J. Korean Acad. Nurs. 2016, 46, 804–812. [Google Scholar] [CrossRef]
- Won, M.-S.; Shin, N.-M.; Kim, E. Gender Differences in Delay Seeking Treatment and Related Experiences in Patients with Acute Myocardial Infarction. Korean J. Adult Nurs. 2016, 28, 459–469. [Google Scholar] [CrossRef]
- Banharak, S.; Prasankok, C.; Lach, H.W. Factors Related to a Delay in Seeking Treatment for Acute Myocardial Infarction in Older Adults: An Integrative Review. Pac. Rim Int. J. Nurs. Res. 2020, 24, 553–568. Available online: https://he02.tci-haijo.org/index.php/PRIJNR/article/view/237531 (accessed on 23 December 2020).
- Aminde, L.N.; Takah, N.; Ngwasiri, C.; Noubiap, J.J.; Tindong, M.; Dzudie, A.; Veerman, J.L. Population awareness of cardiovascular disease and its risk factors in Buea, Cameroon. BMC Public Health 2017, 17, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.; Al-Nafisi, H. Public knowledge of cardiovascular disease and its risk factors in Kuwait: A cross-sectional survey. BMC Public Health 2014, 14, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Jo, M.; Oh, H.; Jang, S.-Y.; Jo, A. Factors Influencing Unawareness of Warning Signs of Stroke among Hypertensive Diabetic Patients at a High Risk for Stroke: The 2017 Nationwide Community Health Survey in Korea. Korean J. Adult Nurs. 2019, 31, 403–413. [Google Scholar] [CrossRef]
- Park, K.S. Factors affecting awareness of myocardial infarction symptoms among the general public in Korea. Epidemiol. Health 2020, 42, e2020032. [Google Scholar] [CrossRef]
- Oh, J.; Kim, H.Y.; Kim, Y.S.; Kim, S.H. Variation in Knowledge of Stroke Warning Signs by Age and Presence of Conventional Risk Factors: A Community Health Survey in Korea. J. Cardiovasc. Nurs. 2020. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhou, Z.; Gao, J.; Wang, D.; Zhang, Q.; Zhou, Z.; Su, M.; Li, D. Health-related quality of life and its influencing factors for patients with hypertension: Evidence from the urban and rural areas of Shaanxi Province, China. BMC Health Serv. Res. 2016, 16, 1–9. [Google Scholar] [CrossRef]
- Bergantin, L.B. Depression rises the risk of hypertension incidence: Discussing the link through the Ca2+/cAMP signalling. Curr. Hypertens. Rev. 2020, 16, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.-Y.; Shin, M.-H.; Rhee, J.-A. Gender differences in the association between self-rated health and hypertension in a Korean adult population. BMC Public Health 2012, 12, 1–6. [Google Scholar] [CrossRef]
- Yu, Y.; Liu, L.; Huang, J.; Shen, G.; Chen, C.; Huang, Y.; Zhang, B.; Tang, S.; Feng, Y. Association between systolic blood pressure and first ischemic stroke in the Chinese older hypertensive population. J. Int. Med. Res. 2020, 48. [Google Scholar] [CrossRef]
- O’Donnell, M.; Hankey, G.J.; Rangarajan, S.; Chin, S.L.; Rao-Melacini, P.; Ferguson, J.; Xavier, D.; Lisheng, L.; Zhang, H.; Pais, P. Variations in knowledge, awareness and treatment of hypertension and stroke risk by country income level. Heart 2021, 107, 282–289. [Google Scholar] [CrossRef]
- Rahman, A.R.A.; Wang, J.-G.; Kwong, G.M.Y.; Morales, D.D.; Sritara, P.; Sukmawan, R. Perception of hypertension management by patients and doctors in Asia: Potential to improve blood pressure control. Asia Pac. Fam. Med. 2015, 14, 1–11. [Google Scholar] [CrossRef]
- Han, C.H.; Kim, H.; Lee, S.; Chung, J.H. Knowledge and poor understanding factors of stroke and heart attack symptoms. Int. J. Environ. Res. Public Health 2019, 16, 3665. [Google Scholar] [CrossRef] [PubMed]
- Korea Diseases Control and Prevention Agency. Community Health Survey 2018, 1st ed.; Korea Diseases Control and Prevention Agency: Cheongju, Korea, 2020; pp. 1–209. [Google Scholar]
- Korea Diseases Control and Prevention Agency. Community Health Survy. Available online: https://chs.cdc.go.kr/chs/index.do (accessed on 19 January 2021).
- Center for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Questionnaire. Available online: https://www.cdc.gov/brfss/index.html (accessed on 19 January 2021).
- Kim, K.A.; Hwang, S.Y. Knowledge on cardio-cerebrovascular disease and health behaviors among middle-aged postmenopausal women at risk. Korean J. Adult Nurs. 2016, 28, 424–435. [Google Scholar] [CrossRef]
- Kim, M.-H.; Cho, Y.-S.; Uhm, W.-S.; Kim, S.; Bae, S.-C. Cross-cultural adaptation and validation of the Korean version of the EQ-5D in patients with rheumatic diseases. Qual. Life Res. 2005, 14, 1401–1406. [Google Scholar] [CrossRef]
- Rabin, R.; Charro, F.D. EQ-SD: A measure of health status from the EuroQol Group. Ann. Med. 2001, 33, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-K.; Nam, H.-S.; Chuang, L.-H.; Kim, K.-Y.; Yang, H.-K.; Kwon, I.-S.; Kind, P.; Kweon, S.-S.; Kim, Y.-T. South Korean time trade-off values for EQ-5D health states: Modeling with observed values for 101 health states. Value Health 2009, 12, 1187–1193. [Google Scholar] [CrossRef]
- Wu, S.; Wang, R.; Zhao, Y.; Ma, X.; Wu, M.; Yan, X.; He, J. The relationship between self-rated health and objective health status: A population-based study. BMC Public Health 2013, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.S.; Choi, J.H.; Park, K.H.; Joo, K.J.; Ga, H.; Ko, H.J.; Kim, S.R. Standardization of the Korean Version of Patient Health Questionnaire-9 as a Screening Instrument for Major Depressive Disorder. J. Korean Acad. Fam. Med. 2007, 28, 114–119. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Patient Health Questionnaire Primary Care Study Group; Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef]
- Mahajan, S.; Valero-Elizondo, J.; Khera, R.; Desai, N.R.; Blankstein, R.; Blaha, M.J.; Virani, S.S.; Kash, B.A.; Zoghbi, W.A.; Krumholz, H.M. Variation and disparities in awareness of myocardial infarction symptoms among adults in the United States. JAMA Netw. Open 2019, 2, e1917885. [Google Scholar] [CrossRef]
- World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Available online: http://www.wpro.who.int/nutrition/documents/docs/Redefiningobesity.pdf (accessed on 21 January 2021).
- Jang, M.H.; Park, C.G. Risk Factors Influencing Probability and Severity of Elder Abuse in Community-dwelling Older Adults: Applying Zero-inflated Negative Binomial Modeling of Abuse Count Data. J. Korean Acad. Nurs. 2012, 42. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Ullah, S.; Nitz, J. Statistical modelling of falls count data with excess zeros. Inj. Prev. 2011, 17, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Luan, S.; Yang, Y.; Huang, Y.; McDowell, M. Public knowledge of stroke and heart attack symptoms in China: A cross-sectional survey. BMJ Open 2021, 11, e043220. [Google Scholar] [CrossRef]
- Mata, J.; Frank, R.; Gigerenzer, G. Symptom recognition of heart attack and stroke in nine European countries: A representative survey. Health Expect. 2014, 17, 376–387. [Google Scholar] [CrossRef]
- Hwang, S.Y.; Jeong, M.H. Cognitive factors that influence delayed decision to seek treatment among older patients with acute myocardial infarction in Korea. Eur. J. Cardiov. Nurs. 2012, 11, 154–159. [Google Scholar] [CrossRef]
- Shi, H.; Li, W.; Zhou, X.; Liu, X.; Liu, J.; Fan, S.; Wang, H.; An, L. Sex differences in prodromal symptoms and individual responses to acute coronary syndrome. J. Cardiov. Nurs. 2020, 35, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.-J.; Moon, J.-D. An analysis of the causes of prehospital delays in patients with suspected acute stroke. Korean J. Emerg. Med. Serv. 2020, 24, 27–38. [Google Scholar]
- Jones, A.; Smakowski, A.; O’Connell, N.; Chalder, T.; David, A.S. Functional stroke symptoms: A prospective observational case series. J. Psychosom. Res. 2020, 132, 109972. [Google Scholar] [CrossRef]
- Colsch, R.; Lindseth, G. Unique stroke symptoms in women: A review. J. Neurosci. Nurs. 2018, 50, 336–342. [Google Scholar] [CrossRef]
- Berglund, A.; Schenck-Gustafsson, K.; von Euler, M. Sex differences in the presentation of stroke. Maturitas 2017, 99, 47–50. [Google Scholar] [CrossRef]
- Schaefer, C. Quality of life and self-monitoring: CVD prevention in practice. The role of patient organizations in CVD prevention. Eur. Heart J. Suppl. 2007, 9, B42–B44. [Google Scholar] [CrossRef]
- Saint Onge, J.M.; Krueger, P.M. Health lifestyle behaviors among U.S. adults. SSM Popul. Health. 2017, 3, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Christensen, V.T.; Carpiano, R.M. Social class differences in BMI among Danish women: Applying Cockerham’s health lifestyles approach and Bourdieu’s theory of lifestyle. Soc. Sci. Med. 2014, 112, 12–21. [Google Scholar] [CrossRef]
- Margolis, R. Educational differences in healthy behavior changes and adherence among middle-aged Americans. J. Health Soc. Behav. 2013, 54, 353–368. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, B.R.; Hinton, L.; Hartmann-Boyce, J.; Roberts, N.W.; Bobrovitz, N.; McManus, R.J. Self-monitoring blood pressure in hypertension, patient and provider perspectives: A systematic review and thematic synthesis. Patient Educ. Couns. 2016, 99, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Bancej, C.M.; Campbell, N.; McKay, D.W.; Nichol, M.; Walker, R.L.; Kaczorowski, J. Home blood pressure monitoring among Canadian adults with hypertension: Results from the 2009 Survey on Living with Chronic Diseases in Canada. Can. J. Cardiol. 2010, 26, e152–e157. [Google Scholar] [CrossRef]
- Ostchega, Y.; Zhang, G.; Kit, B.K.; Nwankwo, T. Factors Associated With Home Blood Pressure Monitoring Among US Adults: National Health and Nutrition Examination Survey, 2011–2014. Am. J. Hypertens. 2017, 30, 1126–1132. [Google Scholar] [CrossRef]
- Ovaisi, S.; Ibison, J.; Leontowitsch, M.; Cloud, G.; Oakeshott, P.; Kerry, S. Stroke patients’ perceptions of home blood pressure monitoring: A qualitative study. Br. J. Gen. Pract. 2011, 61, e604–e610. [Google Scholar] [CrossRef]
- Yan, R.; Gu, H.-Q.; Wang, W.; Ma, L.; Li, W. Health-related quality of life in blood pressure control and blood lipid-lowering therapies: Results from the CHIEF randomized controlled trial. Hypertens. Res. 2019, 42, 1561–1571. [Google Scholar] [CrossRef]
- Shin, H.-G.; Kim, J.-H.; Kwon, H.-W.; Hong, A.; Youn, J.-H.; Han, Y.-J.; Kim, Y.-I. The relationship of blood pressure with subjective health awareness and health related quality of life. Korean J. Fam. Pract. 2016, 6, 660–667. [Google Scholar] [CrossRef]
- Rubio-Guerra, A.F.; Rodriguez-Lopez, L.; Vargas-Ayala, G.; Huerta-Ramirez, S.; Serna, D.C.; Lozano-Nuevo, J.J. Depression increases the risk for uncontrolled hypertension. Exp. Clin. Cardiol. 2013, 18, 10–12. [Google Scholar] [PubMed]
- Disease Policy Division. Creating a Healthy Society without Worrying about Cardiovascular Disease. Available online: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=345946&SEARCHKEY=TITLE&SEARCHVALUE=%EC%8B%AC%EB%87%8C%ED%98%88%EA%B4%80%EC%A7%88%ED%99%98 (accessed on 3 March 2021).

| Variables | Categories | Awareness Group (n = 17,039) | Non-Awareness Group (n = 12,793) |
|---|---|---|---|
| n (Column %) or M ± SD | n (Column %) or M ± SD | ||
| Age | 65.99 ± 10.441 | 72.84 ± 10.483 | |
| 19–39 | 155 (0.9) | 65 (0.5) | |
| 40–64 | 7230 (42.4) | 2526 (19.7) | |
| Over 65 years old | 9564 (56.7) | 10,202 (79.7) | |
| Education | <High school | 11,518 (67.7) | 11,240 (88.0) |
| High school or higher | 5491 (32.3) | 1538 (12.0) | |
| Monthly income (Korean won) | <2 million | 8512 (51.6) | 8556 (69.0) |
| ≥2 million | 7999 (48.4) | 3843 (31.0) | |
| Employed | Yes | 7369 (43.3) | 4263 (33.3) |
| No | 9653 (56.7) | 8522 (66.7) | |
| Residence location | Rural (town, township) | 8168 (47.9) | 8221 (64.3) |
| Urban (city) | 8871 (52.1) | 4572 (35.7) | |
| Marital status | Married and living with a spouse | 11,087 (65.2) | 5902 (46.2) |
| Other * | 5930 (34.8) | 6885 (53.8) | |
| Smoking status | Non-smoker | 16,708 (98.1) | 12,455(97.4) |
| Current smoker | 331 (1.9) | 338 (2.6) | |
| Alcohol (during the last year) | Yes | 7971 (46.8) | 4580 (35.8) |
| No | 9068 (53.2) | 8212 (64.2) | |
| BMI | Normal | 6882 (40.4) | 5953 (46.5) |
| Obese | 10,157 (59.6) | 6840 (53.5) | |
| Walking exercise | <30 min, 1 day per week or less | 5010 (29.4) | 5486 (42.9) |
| >30 min, 2–4 days per week | 3517 (20.6) | 2584 (20.2) | |
| >30 min, 5 days per week or more | 8512 (50.5) | 4723 (36.9) | |
| HTN medication | Yes | 16,428 (96.4) | 12,351 (96.6) |
| No | 610 (3.6) | 440 (3.4) | |
| Diabetes Mellitus | Yes | 3895 (22.9) | 3233 (25.3) |
| No | 13,140 (77.1) | 9558 (74.7) |
| Variables | Awareness Group (n = 17,039) | Non-Awareness Group (n = 12,793) | t or χ2 | p | Cohen’s d or Cramer’s V |
|---|---|---|---|---|---|
| M ± SD or n (%) | M ± SD or n (%) | ||||
| Subjective health status | 2.76 ± 0.85 | 2.50 ± 0.90 | −15.443 | <0.001 | 0.29 |
| Depression | 2.69 ± 3.65 | 3.42 ± 4.28 | −9.752 | <0.001 | −0.19 |
| HRQoL | 0.88 ± 0.152 | 0.82 ± 0.196 | 24.700 | <0.001 | 0.35 |
| Good KCVDs | 10,140 (64.3) | 5635 (35.7) | 701.172 | <0.001 | 0.15 |
| Poor KCVDs | 6899 (49.1) | 7158 (50.98) |
| Variables | Categories | OR | 95% CI | p | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Age | 19–39 | 0.976 | 0.840 | 1.133 | 0.747 |
| 40–64 | 1.046 | 1.012 | 1.081 | 0.008 | |
| 65–79 | ref. | ||||
| Education | <High school | 0.931 | 0.899 | 0.964 | 0.000 |
| High school or higher | ref. | ||||
| Monthly income (Korean won) | <2 million | 0.989 | 0.961 | 1.019 | 0.464 |
| ≥2 million | ref. | ||||
| Employed | Yes | 1.034 | 1.006 | 1.063 | 0.017 |
| No | ref. | ||||
| Residence location | Rural (town, township) | 1.005 | 0.978 | 1.033 | 0.714 |
| Urban (city) | ref. | ||||
| Marital status | Married and living with a spouse | 1.068 | 1.039 | 1.097 | 0.000 |
| Other * | ref. | ||||
| Smoking status | Non-smoker | 0.993 | 0.914 | 1.080 | 0.875 |
| Current smoker | ref. | ||||
| Alcohol (during the last year) | No | 0.983 | 0.957 | 1.009 | 0.196 |
| Yes | ref. | ||||
| BMI | Normal | 0.987 | 0.962 | 1.012 | 0.302 |
| Obese | ref. | ||||
| Walking exercise | <30 min, 1 day per week or less | 0.964 | 0.936 | 0.993 | 0.015 |
| >30 min, 2–4 days per week | 0.987 | 0.955 | 1.021 | 0.454 | |
| >30 min, 5 days per week or more | ref. | ||||
| HTN medication | Yes | 0.974 | 0.910 | 1.042 | 0.442 |
| No | ref | ||||
| Diabetes Mellitus | Yes | 1.010 | 0.981 | 1.041 | 0.488 |
| No | ref. | ||||
| AoBP | Yes | 1.121 | 1.091 | 1.151 | 0.000 |
| No | ref. | ||||
| Subjective health status | 1.000 | 0.983 | 1.016 | 0.972 | |
| Depression | 1.000 | 0.997 | 1.004 | 0.799 | |
| HRQoL | 1.073 | 0.979 | 1.175 | 0.132 | |
| Variables | Categories | OR | 95% CI | p | |
|---|---|---|---|---|---|
| LL | UL | ||||
| Age | 19–39 | 1.092 | 0.795 | 1.500 | 0.587 |
| 40–64 | 1.595 | 1.491 | 1.706 | <0.001 | |
| 65–79 | 1 | ||||
| Education | <High school | 0.542 | 0.503 | 0.584 | <0.001 |
| High school or higher | 1 | ||||
| Monthly income (Korean won) | <2 million | 0.969 | 0.914 | 1.028 | 0.297 |
| ≥2 million | 1 | ||||
| Employed | Yes | 1.111 | 1.050 | 1.176 | <0.001 |
| No | 1 | ||||
| Residence location | Rural (town, township) | 0.637 | 0.603 | 0.673 | <0.001 |
| Urban (city) | 1 | ||||
| Marital status | Married and living with a spouse | 1.496 | 1.418 | 1.578 | <0.001 |
| Other * | 1 | ||||
| Smoking status | Non-smoker | 1.162 | 0.984 | 1.373 | 0.078 |
| Current smoker | 1 | ||||
| Alcohol (during the last year) | No | 0.956 | 0.905 | 1.008 | 0.097 |
| Yes | 1 | ||||
| BMI | Normal | 0.832 | 0.790 | 0.875 | <0.001 |
| Obese | 1 | ||||
| Walking exercise | <30 min, 1 day per week or less | 0.736 | 0.693 | 0.781 | <0.001 |
| >30 min, 2–4 days per week | 0.898 | 0.839 | 0.960 | 0.002 | |
| >30 min, 5 days per week or more | 1 | ||||
| HTN medication | Yes | 1.437 | 1.249 | 1.653 | <0.001 |
| No | 1 | ||||
| Diabetes Mellitus | Yes | 1.024 | 0.965 | 1.087 | 0.426 |
| No | 1 | ||||
| Subjective health status | 1.095 | 1.059 | 1.132 | <0.001 | |
| Depression | 0.994 | 0.987 | 1.001 | 0.088 | |
| HRQoL | 2.048 | 1.704 | 2.462 | <0.001 | |
| Knowledge of CVDs | 1.076 | 1.068 | 1.085 | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, Y.W. Blood Pressure Awareness and Knowledge of Cardio-Cerebrovascular Diseases in South Korean Women with Hypertension. Healthcare 2021, 9, 360. https://doi.org/10.3390/healthcare9030360
Jeong YW. Blood Pressure Awareness and Knowledge of Cardio-Cerebrovascular Diseases in South Korean Women with Hypertension. Healthcare. 2021; 9(3):360. https://doi.org/10.3390/healthcare9030360
Chicago/Turabian StyleJeong, Yeo Won. 2021. "Blood Pressure Awareness and Knowledge of Cardio-Cerebrovascular Diseases in South Korean Women with Hypertension" Healthcare 9, no. 3: 360. https://doi.org/10.3390/healthcare9030360
APA StyleJeong, Y. W. (2021). Blood Pressure Awareness and Knowledge of Cardio-Cerebrovascular Diseases in South Korean Women with Hypertension. Healthcare, 9(3), 360. https://doi.org/10.3390/healthcare9030360





