Does Multidisciplinary Team Simulation-Based Training Improve Obstetric Emergencies Skills?
Abstract
1. Introduction
- Identify the training needs of the health professionals associated with obstetric emergencies.
- Design and validate a specific tool to measure the competencies in the training with obstetric simulations.
- Design and conduct simulation scenarios in obstetric emergencies with a multi-professional group.
- Compare the actions of the health professionals when faced with selected obstetric emergencies before and after simulation training.
- Describe the perception and level of satisfaction of the health professionals after the obstetric simulation training.
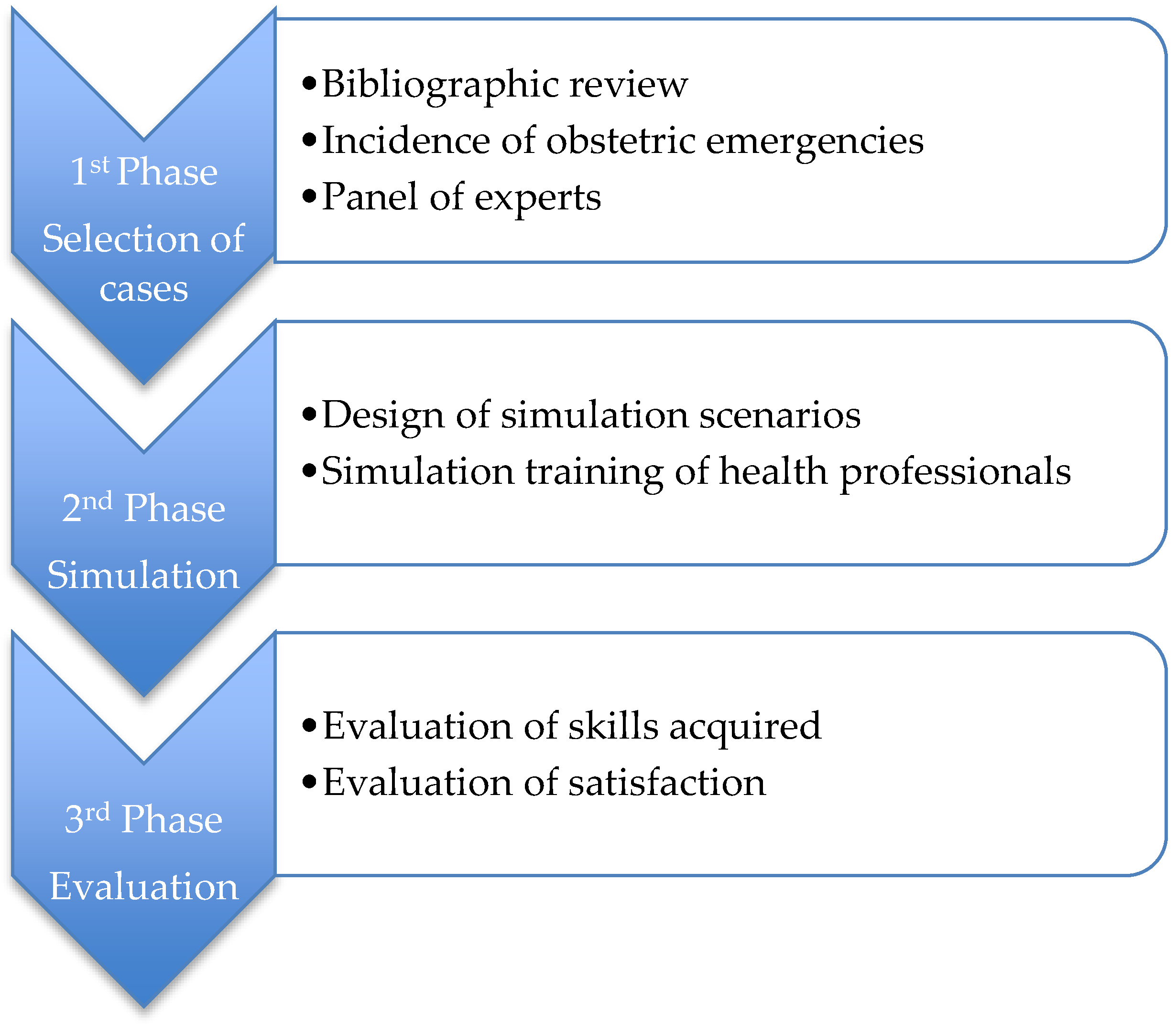
2. Materials and Methods
2.1. Methodology of the First Phase
2.1.1. Design of the Study and Sample
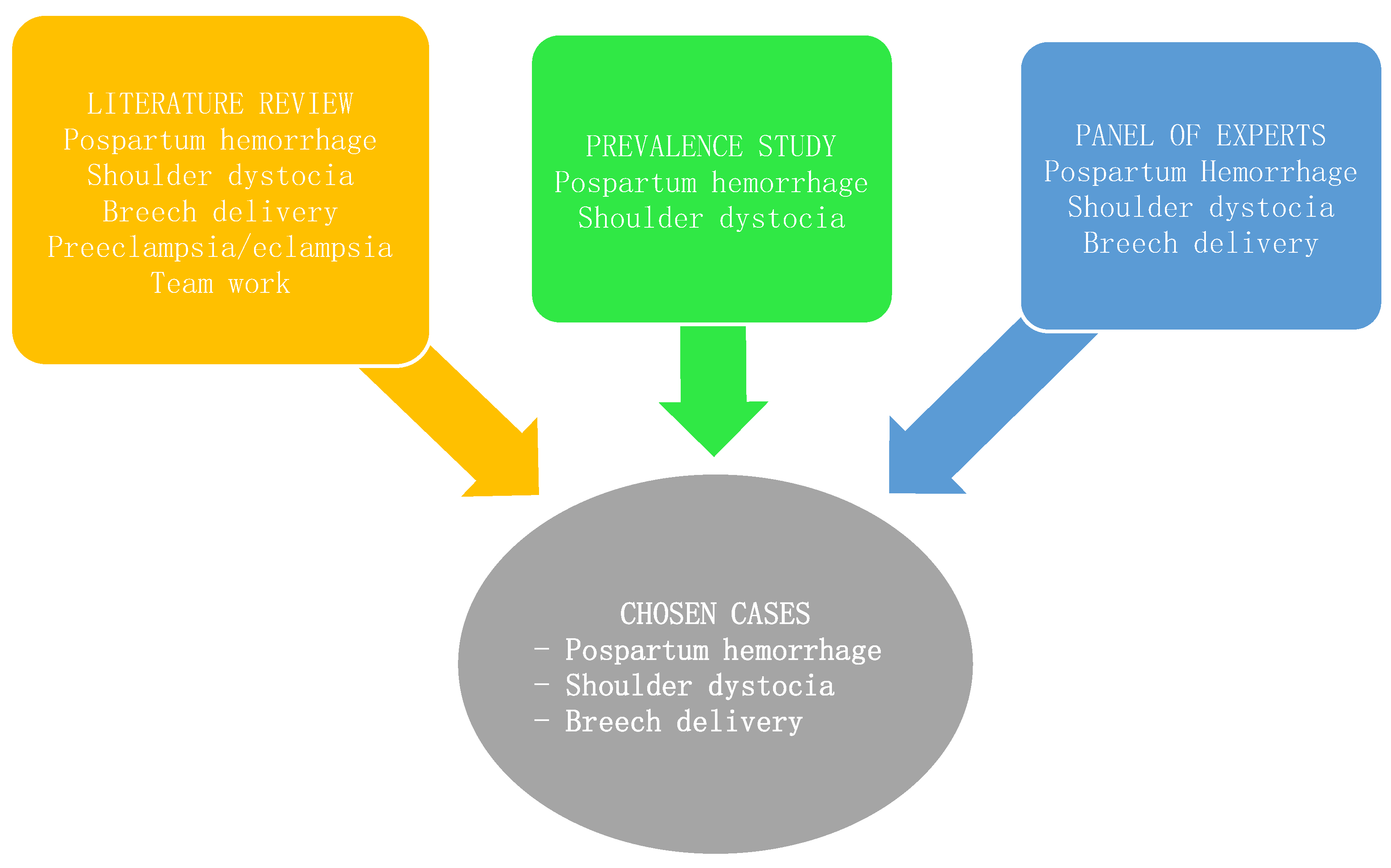
- Literature Review
- Prevalence Study at the Hospital of Torrevieja
- Expert Judgement
- Having more than six years of work experience in obstetrics.
- Currently working at the Hospital of Torrevieja obstetrics delivery room.
- Having teaching or research experience in the field of obstetrics/nursing.
- The panel of selected experts was composed of:
- One gynecologist doctor and supervisor of the Department of Obstetrics and Gynecology at the Hospital of Torrevieja and the Hospital of the Vinalopó in Elche
- One gynecologist from the Hospital of Torrevieja, a tutor of gynecology and obstetrics residents
- One midwife supervisor from the delivery and maternity service at the Hospital of Torrevieja and the Hospital of the Vinalopó, with teaching and research experience
- One midwife, researcher, and midwife residents tutor
- Two nursing assistants and tutors of nursing assistant students
- Knowledge about clinical simulation in obstetrics
- Previous participation in obstetric emergency simulations
- Interest in training on obstetric emergencies
- Needs of the multidisciplinary team in training
- Selection of cases for simulation training
2.1.2. Analysis of the First Phase Data
2.2. Methodology of the Second Phase
2.2.1. Study Design
2.2.2. Sample
2.2.3. Variables
2.2.4. Data Collection
2.3. Methodology of the Third Phase
Data Analysis of the Second and Third Phases
2.4. Ethical Considerations
3. Results
3.1. Results of the First Phase
3.2. Results of the Second Phase
3.2.1. Sample Data
3.2.2. Form Tool
3.2.3. The Overall Time to Resolution
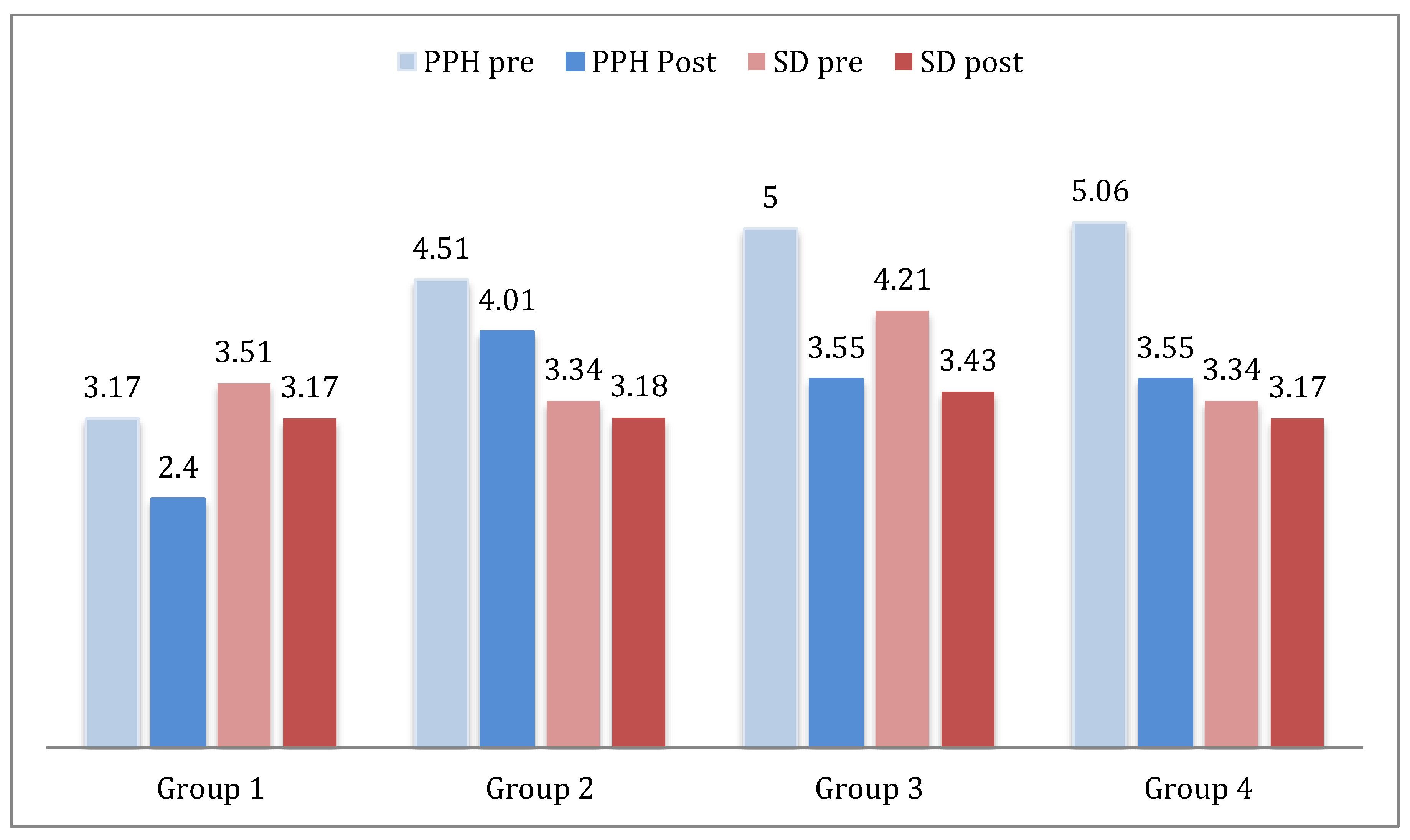
PPH: Postpartum Hemorrhage, SD: Shoulder Dystocia
3.2.4. Inter-observer Agreement
3.3. Results of the Third Phase
3.3.1. Acquisition of Competencies of the Health Professionals
- Postpartum Hemorrhage Scenario
- Shoulder Dystocia Scenario
- Breech Delivery Scenario
3.3.2. Satisfaction of the Health Professionals
4. Discussion
4.1. Discussion of the First and Second Phases
4.2. Discussion of the Third Phase
5. Implications
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Miguel Sesmero, J.R.; Cacho, P.M.; Solano, A.M.; Feu, J.M.; Gómez, M.G.; Prieto, A.P.; González, N.L.; Vicens, J.M. Mortalidad materna en España en el periodo 2010–2012: Resultados de la encuesta de la Sociedad Española de Ginecología (SEGO). Progr. Obstet. Ginecol. 2016, 5, 342–349. [Google Scholar] [CrossRef]
- Deering, S.; Rowland, J. Obstetric emergency simulation. Semin. Perinatol. 2013, 37, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Kainer, F. Simulation-based training in obstetrics. Arch. Gynecol. Obstet. 2014, 4, 703–704. [Google Scholar] [CrossRef]
- Riley, W.; Davis, S.; Miller, K.; Hansen, H.; Sainfort, F.; Sweet, R. Didactic and simulation nontechnical skills team training to improve perinatal patient outcomes in a community hospital. Jt. Comm. J. Qual. Patient. Saf. 2011, 8, 357–364. [Google Scholar] [CrossRef]
- Lavelle, M.; Abthorpe, J.; Simpson, T.; Reedy, G.; Little, F.; Banerjee, A. MBRRACE in simulation: An evaluation of a multi-disciplinary simulation training for medical emergencies in obstetrics (MEmO). J. Obs. Gynaecol. 2018, 6, 781–788. [Google Scholar] [CrossRef]
- Robertson, B.; Schumacher, L.; Gosman, G.; Kanfer, R.; Kelley, M.; De Vita, M. Simulation-based crisis team training for multidisciplinary obstetric providers. Simul. Healthc. 2009, 2, 77–83. [Google Scholar] [CrossRef]
- Amatullah, A.F. Using interprofessional simulation-based training to improve management of obstetric emergencies: A systematic review. Clin. Simul. Nurs. 2018, 14, 45–53. [Google Scholar] [CrossRef]
- Al-Yateem Sami, R.N.; Al-Yateem Nabeel, R.N.; Amatullah, A.F. Simulation-based training to improve obstetric/perinatal nurses competency in managing obstetric emergencies in Saudi Arabia (KSA). Int. J. Caring. Sci. 2019, 3, 1788–1795. [Google Scholar]
- OMS. Objetivo de Desarrollo del Milenio 5: Mejorar la Salud Materna. Available online: http://www.who.int/maternal_child_adolescent/topics/maternal/mdg/es/ (accessed on 3 April 2017).
- Bajaj, K.; Rivera-Chiauzzi, E.Y.; Lee, C.; Shepard, C.; Bernstein, P.S.; Moore-Murray, T.; Smith, H.; Nathan, L.; Walker, K.; Chazotte, C.; et al. Validating obstetric emergency checklists using simulation: A randomized controlled trial. Am. J. Perinatol. 2016, 12, 1182–1190. [Google Scholar]
- SEGO Sociedad Española de Obstetricia y Ginecología. Distocia de Hombros, Protocolos Asistenciales en Obstetricia. Available online: http://www.sego.es//Guias_de_Asistencia_Practica#perinatal/Distocia-de-hombros-2015-.pdf (accessed on 5 May 2017).
- Crofts, J.F.; Bartlett, C.; Ellis, D.; Hunt, L.P.; Fox, R.; Draycott, T.J. Management of Shoulder Dystocia: Skill Retention 6 and 12 Months After Training. Obstet. Gynecol. 2007, 5, 1069–1074. [Google Scholar] [CrossRef]
- Jordan, A.; Antomarchi, J.; Bongain, A.; Tran, A.; Delotte, J. Development and validation of an objective structured assessment of technical skill tool for the practice of breech presentation delivery. Arch. Gynecol. Obs. 2016, 2, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Deering, S.; Brown, J.; Hodor, J.; Satin, A.J. Simulation training and resident performance of singleton vaginal breech delivery. Obs. Gynecol. 2006, 1, 86–89. [Google Scholar] [CrossRef]
- De la Horra Gutiérrez, I. La simulación clínica como herramienta de evaluación de competencias en la formación de enfermería. Reduca Enfermería Fisioterapia Podología 2010, 1, 549–580. [Google Scholar]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice; F. A. Davis Company: Philadelphia, PA, USA, 2009. [Google Scholar]
- Deering, S. Emergencies in Clinical Obstetrics Course Introduction. Available online: https://www.acog.org/Education-and-Events/ECO-Course (accessed on 3 April 2017).
- The Society of Obstetricians and Gynaecologists of Canada. Advances in Labour and Risk Management Course Manual, 22nd ed.; The Society of Obstetricians and Gynaecologists of Canada: Otawa, ON, Canada, 2002. [Google Scholar]
- Walker, D.M.; Cohen, S.R.; Estrada, F.; Monterroso, M.E.; Jenny, A.; Fritz, J.; Fahey, J.O. Pronto training for obstetric and neonatal emergencies in Mexico. Int. J. Gynecol. Obstet. 2012, 2, 128–133. [Google Scholar] [CrossRef]
- Winter, C.; Crofts, J.; Laxton, C.; Barnfield, S.; Draycott, T. PROMPT: Practical Obstetric Multi-Professional Training: Practical Locally Based Training for Obstetric Emergencies; Cambridge University Press: Cambridge, UK, 2008. [Google Scholar]
- Hernández Pinto, P.P.H.; Feu, J.M.O.; Alonso, J.M.M.; Sánchez, M.L.; Mazariegos, I.D.M.V.; Sesmero, J.R.D.M. Entrenamiento de equipos interdisciplinares en urgencias obstétricas mediante simulación clínica. Progr. Obstet. Ginecol. 2011, 54, 618–624. [Google Scholar] [CrossRef]
- Marshall, N.E.; Vanderhoeven, J.; Eden, K.B.; Segel, S.Y.; Guise, J.M. Impact of simulation and team training on postpartum hemorrhage management in non-academic centers. J. Matern. Fetal. Neo. Med. 2015, 5, 495–499. [Google Scholar] [CrossRef] [PubMed]
- Kato, C.; Kataoka, Y. Simulation training program for midwives to manage postpartum hemorrhage: A randomized controlled trial. Nurse Educ. Today 2017, 51, 88–95. [Google Scholar] [CrossRef]
- Gum, L.; Greenhill, J.; Dix, K. Clinical simulation in maternity (CSiM): Interprofessional learning through simulation team training. BMJ Qual. Saf. 2010, 5, e19. [Google Scholar] [CrossRef]
- Maslovitz, S.; Barkai, G.; Lessing, J.B.; Ziv, A.; Many, A. Recurrent obstetric management mistakes identified by simulation. Obs. Gynecol. 2007, 6, 1295–1300. [Google Scholar] [CrossRef] [PubMed]
- SEGO Sociedad Española de Obstetricia y Ginecología. Parto en La Presentación de Nalgas a Término: Protocolos Asistenciales en Obstetricia. Available online: http://www.sego.es//Guias_de_Asistencia_Practica#perinatal/47-Parto-en-la-presentacion-de-nalgas-a-t--rmino.pdf (accessed on 4 May 2016).
- Lansac, J.; Crenn-Hebert, C.; Rivière, O.; Vendittelli, F. How singleton breech babies at term are born in France: A survey of data from the AUDIPOG network. Eur. J. Obs. Gynecol. Reprod. Biol. 2015, 188, 79–82. [Google Scholar] [CrossRef]
- Calton, E.; Essex, J.; Bowman, D.; Barrett, C. Ethics teaching for clinical practice: A student perspective. Clin. Teach 2008, 4, 222–225. [Google Scholar] [CrossRef]
| Variables 2nd Phase | ||
|---|---|---|
| Independent var. | Dependent var. | |
| Age | Non-technical | Technical |
| Sex | Coordination of tasks | 39 variables Techniques from the three specific scenarios |
| Profession | Working in teams | |
| Previous simulation experience | Communication with patient | |
| Experience in obstetrics | Communication with team | |
| Nationality | Communication with family | |
| Observer | Perception of professionals | |
| Name of scenario | Obstetric Emergency to Simulate |
|---|---|
| Patient data | Relevant data |
| Health status of the pregnant woman | |
| Summary of the scenario | |
| Objectives to be met in the simulation | Evaluation of the patient |
| Activities/techniques to be performed | |
| Coordination, teamwork | |
| Professional involved | Gynecologist, midwife, nursing assistant |
| OTR | Overall resolution time of the emergency |
| S.C. | Specific competencies to be trained on/evaluated in each scenario |
| Country | UK, New Zealand, and Australia | Latin America, Africa, and India | United States | Canada |
|---|---|---|---|---|
| Course | PROMPT | PRONTO | ECO | ALARM |
| Obstetric cases | Shoulder dystocia | Shoulder dystocia | Shoulder dystocia | Shoulder dystocia |
| Severe pre-eclampsia and eclampsia | Postpartum hemorrhage | Postpartum hemorrhage | Pre-eclampsia and eclampsia | |
| Postpartum hemorrhage | Pre-eclampsia and eclampsia | Cord prolapse | Postpartum hemorrhage | |
| Breech delivery | Neonatal resuscitation | Breech delivery | Breech delivery | |
| Uterine inversion | Choriamnionitis | Maternal sepsis | ||
| Cord prolapse | Teamwork | Instrumental delivery | ||
| Maternal sepsis | Communication | |||
| CPR | ||||
| Maternal anesthetic emergencies | ||||
| Intrapartum fetal monitoring | ||||
| Teamwork | ||||
| Caregiving to the second twin | ||||
| Neonatal resuscitation |
| Obstetric Emergency | Number of Cases (2016) |
|---|---|
| Eclampsia | 1 |
| Shoulder dystocia | 6 |
| Postpartum hemorrhage | 11 |
| Obstetric trauma (third and fourth degree tears) | 7 |
| Emergency obstetric hysterectomy | 0 |
| Uterine rupture | 0 |
| Postpartum curettage | 11 |
| Postpartum thromboembolic disease | 0 |
| Blood or blood products transfusion | 4 |
| OTR | Pre | Post | Pre-Post | |
|---|---|---|---|---|
| M/SD | M/SD | t-Test (gl) | p | |
| PPH | 4.48/0.70 | 3.50/0.52 | 11.24 (29) | 0.000 |
| SD | 3.57/0.33 | 3.22/0.10 | 8.12 (29) | 0.000 |
| Pre-Test | Postest | |||||||
|---|---|---|---|---|---|---|---|---|
| ICC | Confidence Interval 95% | p | ICC | Confidence Interval 95% | p | |||
| PPH | Lower | Upper | Lower | Upper | ||||
| S.C.8 | 0.981 | 0.966 | 0.990 | 0.000 | 0.700 | 0.449 | 0.847 | 0.000 |
| S.C.13 | 0.549 | 0.173 | 0.770 | 0.005 | 0.970 | 0.944 | 0.985 | 0.000 |
| S.C.14 | 0.865 | 0.753 | 0.931 | 0.000 | 0.900 | 0.817 | 0.949 | 0.000 |
| S.C.33 | 0.777 | 0.592 | 0.887 | 0.000 | 0.833 | 0.693 | 0.915 | 0.000 |
| DH | ||||||||
| S.C.8 | 0.745 | 0.533 | 0.870 | 0.000 | 0.808 | 0.649 | 0.902 | 0.000 |
| S.C.13 | 0.600 | 0.267 | 0.796 | 0.001 | 0.917 | 0.849 | 0.958 | 0.000 |
| S.C.33 | 0.812 | 0.654 | 0.904 | 0.000 | 0.574 | 0.219 | 0.783 | 0.003 |
| BD | ||||||||
| S.C.8 | 0.875 | 0.771 | 0.936 | 0.000 | 0.819 | 0.669 | 0.908 | 0.000 |
| S.C.13 | 0.568 | 0.208 | 0.780 | 0.003 | 0.643 | 0.345 | 0.818 | 0.000 |
| S.C.14 | 0.921 | 0.854 | 0.960 | 0.000 | 0.844 | 0.714 | 0.920 | 0.000 |
| S.C.33 | 0.819 | 0.668 | 0.908 | 0.000 | 0.810 | 0.652 | 0.903 | 0.000 |
| Pre-Test | Postest | Pre-Test/Postest | ||||
|---|---|---|---|---|---|---|
| PPT | M | SD | M | SD | t(gl) | p |
| Diagnosis (S.C.8) | 4.66 | 1.09 | 6.6 | 0.49 | 15.314 (29) | 0.000 |
| Management (S.C.13) | 2.33 | 0.47 | 5.13 | 1.16 | 15.38 (29) | 0.000 |
| Drugs (S.C.14) | 1 | 0 | 1.4 | 0.49 | 4.39 (29) | 0.000 |
| Recording and communication (S.C.33) | 2 | 0.26 | 3.9 | 0.30 | 34.10 (29) | 0.000 |
| SD | ||||||
| Diagnosis (C.E.8) | 3.26 | 0.44 | 3.46 | 0.50 | 2.69 (29) | 0.012 |
| Management (C.E.13) | 3 | 0 | 6.2 | 0.40 | 43.08 (29) | 0.000 |
| Recording and communication (S.C.33) | 2.06 | 2.06 | 3.93 | 3.93 | 23.54 (29) | 0.000 |
| BD | ||||||
| Diagnosis (S.C.8) | 2.83 | 0.379 | 2.866 | 0.345 | 1.0 (29) | 0.326 |
| Management (S.C.13) | 2.40 | 0.813 | 9.733 | 0.691 | 41.88 (29) | 0.000 |
| Specific techniques (S.C.14) | 1.00 | 0.262 | 1.400 | 0.498 | 3.89 (29) | 0.001 |
| Recording and communication (S.C.33) | 2.50 | 0.508 | 2.700 | 0.466 | 2.69 (29) | 0.012 |
| ITEMS | n (%) | M (SD) | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |||
| 1. | The scenarios were real | 0 (0%) | 0 (0%) | 0 (0%) | 7 (23.33%) | 23 (76.66%) | 4.7 (0.4) |
| 2. | The experience has improved my technical skills | 0 (0%) | 0 (0%) | 0 (0%) | 2 (6.66%) | 28 (93.33%) | 4.9 (0.2) |
| 3. | It helps with the development of critical thinking and decision making | 0 (0%) | 0 (0%) | 0 (0%) | 1 (3.33%) | 29 (96.66%) | 4.9 (0.1) |
| 4. | The prioritization skills taught using simulation are valuable | 0 (0%) | 0 (0%) | 0 (0%) | 1 (3.33%) | 29 (96.66%) | 4.9 (0.1) |
| 5. | The experience with the simulation has increased my security | 0 (0%) | 0 (0%) | 0 (0%) | 2 (6.66%) | 28 (93.33%) | 4.9 (0.2) |
| 6. | The interaction with the simulation has improved my clinical competence | 0 (0%) | 0 (0%) | 0 (0%) | 1 (3.33%) | 29 (96.66%) | 4.9 (0.1) |
| 7. | The simulation has helped me to integrate theory and practice | 0 (0%) | 0 (0%) | 0 (0%) | 1 (3.33%) | 29 (96.66%) | 4.9 (0.1) |
| 8. | In general, the experience of working with clinical simulation has been satisfactory | 0 (0%) | 0 (0%) | 0 (0%) | 1 (3.33%) | 29 (96.66%) | 4.9 (0.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández, E.; Camacho, M.; Leal-Costa, C.; Ruzafa-Martínez, M.; Ramos-Morcillo, A.J.; Cazorla, E.; Díaz-Agea, J.L. Does Multidisciplinary Team Simulation-Based Training Improve Obstetric Emergencies Skills? Healthcare 2021, 9, 170. https://doi.org/10.3390/healthcare9020170
Hernández E, Camacho M, Leal-Costa C, Ruzafa-Martínez M, Ramos-Morcillo AJ, Cazorla E, Díaz-Agea JL. Does Multidisciplinary Team Simulation-Based Training Improve Obstetric Emergencies Skills? Healthcare. 2021; 9(2):170. https://doi.org/10.3390/healthcare9020170
Chicago/Turabian StyleHernández, Encarna, Marcos Camacho, César Leal-Costa, María Ruzafa-Martínez, Antonio Jesús Ramos-Morcillo, Eduardo Cazorla, and José Luis Díaz-Agea. 2021. "Does Multidisciplinary Team Simulation-Based Training Improve Obstetric Emergencies Skills?" Healthcare 9, no. 2: 170. https://doi.org/10.3390/healthcare9020170
APA StyleHernández, E., Camacho, M., Leal-Costa, C., Ruzafa-Martínez, M., Ramos-Morcillo, A. J., Cazorla, E., & Díaz-Agea, J. L. (2021). Does Multidisciplinary Team Simulation-Based Training Improve Obstetric Emergencies Skills? Healthcare, 9(2), 170. https://doi.org/10.3390/healthcare9020170









