Nursing Students’ Informal Learning of Patient Safety Management Activities
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants and Data Collection
2.3. Ethics Approval
2.4. Research Instruments
2.4.1. Participant Characteristics
2.4.2. Nursing Competence
2.4.3. Informal Learning
2.4.4. Patient Safety Management
2.5. Data Analysis
3. Results
3.1. General Characteristics and Descriptive Statistics of Participants
3.2. Correlational and Validity Analysis
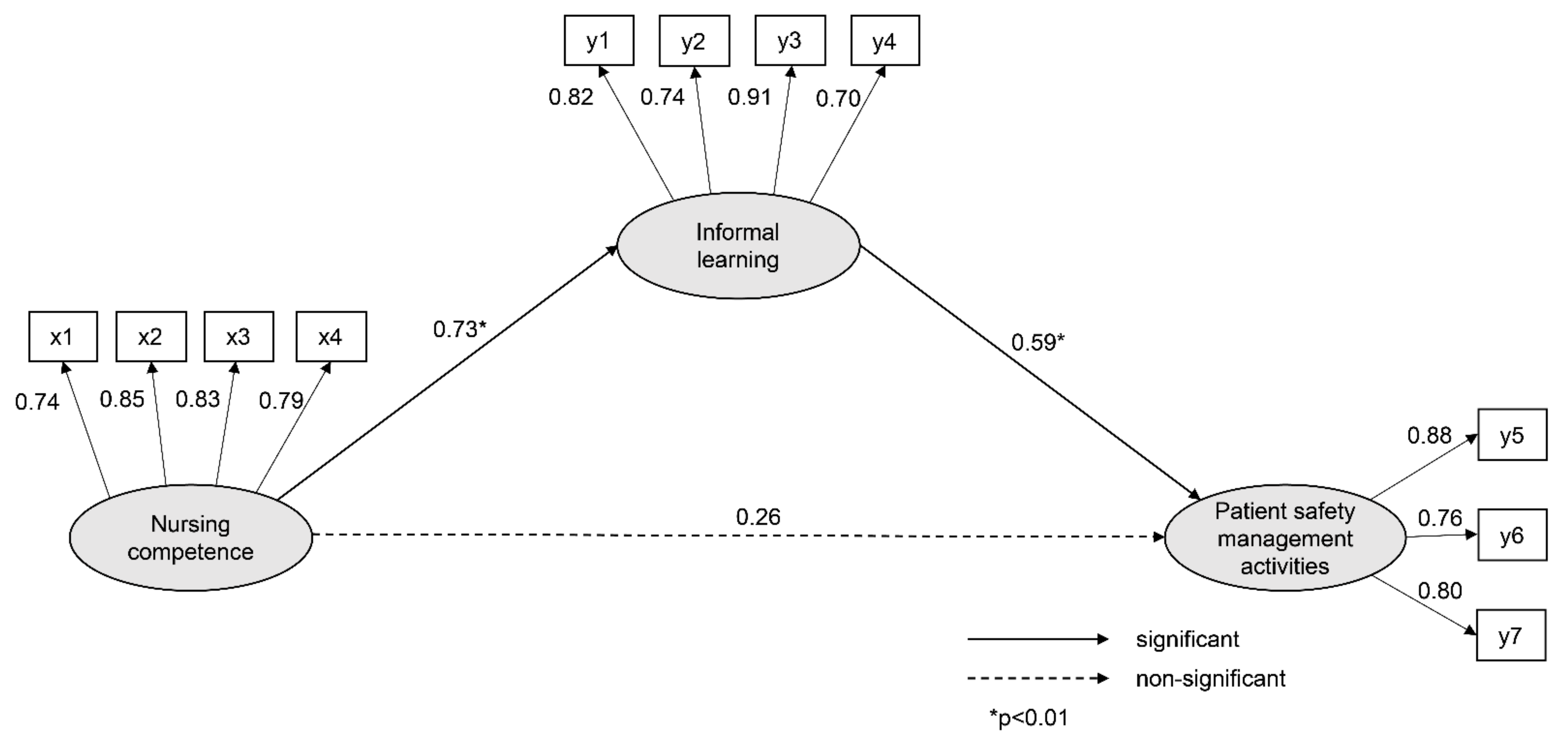
3.3. Fitness of the Hypothetical Model and Path Analysis
4. Discussion
5. Limitations
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, N.-Y. Analysis of patient safety incident in Korea. J. Korean Acad. Nurs Adm. 2020, 26, 151–159. [Google Scholar] [CrossRef]
- Buheji, M.; Buhaid, N. Nursing human factor during COVID-19 pandemic. Int. J. Nurs. Sci. 2020, 10, 12–24. [Google Scholar] [CrossRef]
- Vanhaecht, K.; Seys, D.; Schouten, L.; Bruyneel, L.; Coeckelberghs, E.; Panella, M.; Zeeman, G. Duration of second victim symptoms in the aftermath of a patient safety incident and association with the level of patient harm: A cross-sectional study in the Netherlands. BMJ Open 2019, 9, e029923. [Google Scholar] [CrossRef]
- Vogelsang, A.C.; Swenne, C.L.; Gustafsson, B.Å.; Falk Brynhildsen, K. Operating theatre nurse specialist competence to ensure patient safety in the operating theatre: A discursive paper. Nurs. Open 2020, 7, 495–502. [Google Scholar] [CrossRef]
- Nabizadeh, G.Z.; Alavi, N.M.; Ajorpaz, N.M. Clinical competence in nursing: A hybrid concept analysis. Nurse Educ. Today 2021, 97, 104728. [Google Scholar] [CrossRef]
- Kim, N.Y. Novice and advanced beginner nurses’ patient safety management activities: Mediating effects of informal learning. J. Korean Acad. Nurs. Adm. 2020, 26, 542–549. [Google Scholar] [CrossRef]
- Kim, M.J.; Kim, J.K. A study on the relationships among perception about patient safety culture, patient safety competence, and safety nursing activities of emergency room nurses. J. Korean Contents Soc. 2017, 17, 268–279. [Google Scholar]
- Song, M.O.; Mun, J.E. A study on the patient safety management activities of nursing students. J. Korean Soc. Converg. 2018, 9, 379–388. [Google Scholar]
- Yoo, H.N.; Lee, H.Y. The initial application of the patient safety management activity scale (PSM-A) for nursing students: Brief on reliability and validity. J. Korean Data Anal. Soc. 2014, 16, 3423–3436. [Google Scholar]
- Tohmola, A.; Saarnio, R.; Mikkonen, K.; Kyngäs, H.; Elo, S. Development and psychometric testing of the Gerontological Nursing Competence (GeroNursingCom) instrument. J. Adv. Nurs. 2021, 77, 1070–1084. [Google Scholar] [CrossRef]
- Ginsburg, L.; Castel, E.; Tregunno, D.; Norton, P.G. The H-PEPSS: An instrument to measure health professionals’ perceptions of patient safety competence at entry into practice. BMJ Qual. Saf. 2012, 21, 676–684. [Google Scholar] [CrossRef]
- Moon, S.Y.; Na, S.I. Variables associated with informal learning of workers in small and medium-sized enterprises. Today 2011, 14, 111–138. [Google Scholar]
- Joynes, V.; Kerr, M.; Treasure, J.T. Exploring informal workplace learning in primary healthcare for continuous professional development. Educ. Prim. Care 2017, 28, 216–222. [Google Scholar] [CrossRef]
- Marsick, V.; Watkins, K. Informal and Incidental Learning in the Workplace; Routledge: London, UK, 2015; pp. 51–126. [Google Scholar]
- Cho, J.; Yoon, D.Y.; Han, S.H. The effects of informal learning on organizational commitment: The mediating effects of self-efficacy. Korean Acad. Assoc. Bus. Adm. 2018, 31, 1527–1547. [Google Scholar] [CrossRef]
- Kim, N.Y.; Woo, C.H. Mediating effect of self-efficacy in the relationship between informal learning, shared leadership and organizational socialization of beginner-advanced beginner nurses. J. Korean Acad. Nurs. Adm. 2018, 24, 1–9. [Google Scholar] [CrossRef]
- Park, J.H.; Park, M.H. Nursing students’ knowledge, attitudes, and confidence on patient safety of undergraduate nursing students. J. Korean Acad. Soc. Nurs. Educ. 2014, 20, 5–14. [Google Scholar] [CrossRef]
- Jeong, H.S.; Kong, J.H.; Jeon, M.Y. Factors influencing confidence in patient safety management in nursing students. J. Korean Soc. Converg. 2017, 8, 121–130. [Google Scholar] [CrossRef]
- Lee, J.Y.; Lee, S.H. The effect of nursing college students’ patient safety culture attitude and practice of patient safety management on satisfaction with clinical practice. Korean J. Saf. Manag. Sci. 2017, 19, 125–132. [Google Scholar]
- Bae, B.R. Amos 24 Structural Equation Modeling; Cheongram: Seoul, Korea, 2017; pp. 134–311. [Google Scholar]
- Scheiner, S.M. Path analysis. In Design and Analysis of Ecological Experiments.; Gurevitch, J., Mitchell, R.J., Eds.; Oxford University Press: Oxford, UK, 2001; pp. 217–234. [Google Scholar]
- Park, M.R.; Kim, N.C. Development of a nursing competence measurement scale according to nurse’s clinical ladder in general wards. J. Korean Acad. Nurs. Adm. 2014, 20, 257–271. [Google Scholar] [CrossRef]
- Park, J.H. Nursing students’ patient safety competency and patient safety management behavior. J. Korean Acad. Ind. Soc. 2019, 20, 216–223. [Google Scholar]
- Kim, J.J.; Jung, H.M. Effect of patient safety culture and patient safety competence on safety nursing activity among nurses working in anesthetic and recovery rooms. J. Korean Clin. Nurs. Res. 2020, 26, 164–174. [Google Scholar] [CrossRef]
- Knebel, E.; Greiner, A.C. Health Professions Education: A Bridge. to Quality; National Academies Press: Washington, DC, USA, 2003; pp. 19–74. [Google Scholar]
- Kim, D.H.; Lee, Y.; Hwang, M.S.; Park, J.H.; Kim, H.S.; Cha, H.G. Effects of a simulation-based integrated clinical practice program (SICPP) on the problem solving process, clinical competence and critical thinking in a nursing student. J. Korean Acad. Soc. Nurs. Educ. 2012, 18, 499–509. [Google Scholar] [CrossRef][Green Version]
- Kim, E.J.; Nam, K.A. Effects of Team-based Simulation Training on Patient Safety Confidence and Nursing Competency among Nursing Students. J. East. West. Nurs. Res. 2020, 26, 130–138. [Google Scholar]
- Kim, E.J. Nursing students’ error and recovery in transfusion simulation for safety competency. J. Korean Acad. Fundam. Nurs. 2015, 22, 180–189. [Google Scholar] [CrossRef][Green Version]
- Kim, Y.M.; Yu, J.Y. Influences of simulation-based education of postpartum hemorrhage care on nursing college students’ critical thinking tendency, communication confidence, and problem solving process. AJMAHS 2019, 9, 399–409. [Google Scholar]
- Hung, C.C.; Kao, H.F.S.; Liu, H.C.; Liang, H.F.; Chu, T.P.; Lee, B.O. Effects of simulation-based learning on nursing students’ perceived competence, self-efficacy, and learning satisfaction: A repeat measurement method. Nurse Educ. Today 2021, 97, 104725. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Lee, N.J.; Jang, H. Patient safety teaching competency of nursing faculty. J. Korean Acad. Nurs. 2018, 48, 720–730. [Google Scholar] [CrossRef]
- Tregunno, D.; Ginsburg, L.; Clarke, B.; Norton, P. Integrating patient safety into health professionals’ curricula: A qualitative study of medical, nursing and pharmacy faculty perspectives. BMJ Qual. Saf. 2014, 23, 257–264. [Google Scholar] [CrossRef]
- Smith, E.L.; Cronenwett, L.; Sherwood, G. Current assessments of quality and safety education in nursing. Nurs. Outlook 2007, 55, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.Y.; Jeong, S.Y. Patient safety management activities of clinical nurse: A modified theory of planned behavior. J. Korean Acad. Nurs. Adm. 2019, 25, 384–392. [Google Scholar] [CrossRef]
| Variable | Category | n (%) | Mean ± SD | Skewness | Kurtosis |
|---|---|---|---|---|---|
| Age (years) | 22.10 ± 1.97 | ||||
| University grade | 3rd year | 67 (49.3) | |||
| 4th year | 69 (50.7) | ||||
| Safety education (hospital) | Yes | 111 (81.6) | 1.46 ± 1.78 | ||
| No | 25 (18.4) | ||||
| Safety education (college) | Yes | 95 (69.9) | 0.96 ± 1.18 | ||
| No | 41 (30.1) | ||||
| Observation of patient safety accident | Yes | 77 (56.6) | 0.72 ± 1.42 | ||
| No | 59 (43.4) | ||||
| Nursing competence | 3.23 ± 0.36 | 0.41 | −0.31 | ||
| Informal learning | 3.97 ± 0.49 | −0.08 | −0.01 | ||
| Patient safety management activities | 4.18 ± 0.48 | −0.08 | −0.21 |
| Variable | NC | IL | PSMA | AVE | CR |
|---|---|---|---|---|---|
| R | r | r | |||
| (p) | (p) | (p) | |||
| Nursing competence | 1 | 0.65 | 0.88 | ||
| Informal learning | 0.64 | 1 | 0.63 | 0.87 | |
| (<0.001) | |||||
| Patient safety management activities | 0.60 | 0.66 | 1 | 0.67 | 0.86 |
| (<0.001) | (<0.001) |
| Endogenous Variable | Exogenous Variable | SE | CR | P | SRW | SMC | Direct Β (p) | Indirect Β (p) |
|---|---|---|---|---|---|---|---|---|
| IL | NC | 1.08 | 7.12 | 0.73 | 0.53 | 0.73 (0.005) | ||
| PSMA | NC | 0.37 | 2.27 | 0.023 | 0.26 | 0.63 | 0.26 (0.114) | 0.43 (0.005) |
| IL | 0.57 | 5.00 | <0.001 | 0.59 | 0.59 (0.009) | |||
| Goodness-of-fit statistics | χ2/DF(p) = 1.73(.003), GFI = 0.91, NFI = 0.93, TLI = 0.97, CFI = 0.97, SRMR = 0.05, RMSEA = 0.06 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, N.-Y. Nursing Students’ Informal Learning of Patient Safety Management Activities. Healthcare 2021, 9, 1635. https://doi.org/10.3390/healthcare9121635
Kim N-Y. Nursing Students’ Informal Learning of Patient Safety Management Activities. Healthcare. 2021; 9(12):1635. https://doi.org/10.3390/healthcare9121635
Chicago/Turabian StyleKim, Nam-Yi. 2021. "Nursing Students’ Informal Learning of Patient Safety Management Activities" Healthcare 9, no. 12: 1635. https://doi.org/10.3390/healthcare9121635
APA StyleKim, N.-Y. (2021). Nursing Students’ Informal Learning of Patient Safety Management Activities. Healthcare, 9(12), 1635. https://doi.org/10.3390/healthcare9121635






