Efavirenz Is Not Associated with an Increased Risk of Depressive Disorders in Patients Living with HIV: An 11-Year Population-Based Study in Taiwan
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
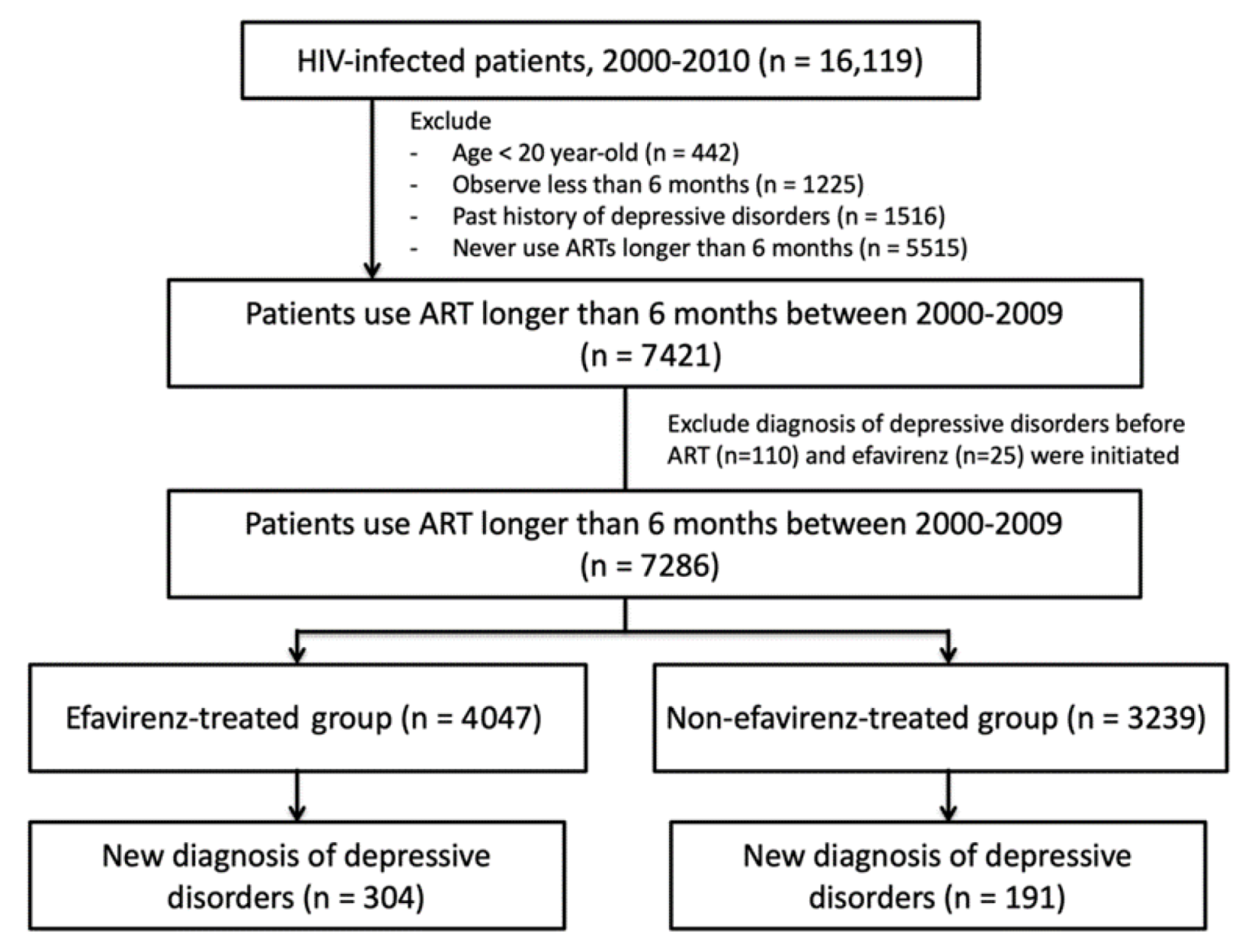
2.2. Study Population and Design
2.3. Research Variables
2.4. Statistical Analysis
2.5. Sensitivity Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beyer, J.L.; Taylor, L.; Gersing, K.R.; Krishnan, K.R. Prevalence of HIV infection in a general psychiatric outpatient population. Psychosomatics 2007, 48, 31–37. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lopes, M.; Olfson, M.; Rabkin, J.; Hasin, D.S.; Alegría, A.A.; Lin, K.H.; Grant, B.F.; Blanco, C. Gender, HIV status, and psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related conditions. J. Clin. Psychiatry 2012, 73, 384–391. [Google Scholar] [CrossRef]
- Chen, M.H.; Su, T.P.; Chen, T.J.; Cheng, J.Y.; Wei, H.T.; Bai, Y.M. Identification of psychiatric disorders among human immunodeficiency virus-infected individuals in Taiwan, a nine-year nationwide population-based study. AIDS Care 2012, 24, 1543–1549. [Google Scholar] [CrossRef] [PubMed]
- Wright, E.; Brew, B.; Arayawichanont, A.; Roberson, K.; Saintharapanya, K.; Kongsaengdao, S.; Lim, M.; Vonthanak, S.; Lal, L.; Sarim, C.; et al. Neurologic disorders are prevalent in HIV-positive outpatients in the Asia-Pacific region. Neurology 2008, 71, 50–56. [Google Scholar] [CrossRef]
- Kim, M.H.; Mazenga, A.C.; Yu, X.; Devandra, A.; Nguyen, C.; Ahmed, S.; Kazembe, P.N.; Sharp, C. Factors associated with depression among adolescents living with HIV in Malawi. BMC Psychiatry 2015, 15, 264. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.H.; Mazenga, A.C.; Devandra, A.; Ahmed, S.; Kazembe, P.N.; Yu, X.; Nguyen, C.; Sharp, C. Prevalence of depression and validation of the beck depression inventory-II and the children’s depression inventory-short amongst HIV-positive adolescents in Malawi. J. Int. AIDS Soc. 2014, 17, 18965. [Google Scholar] [CrossRef]
- Pao, M.; Lyon, M.; D’Angelo, L.J.; Schuman, W.B.; Tipnis, T.; Mrazek, D.A. Psychiatric diagnoses in adolescents seropositive for the human immunodeficiency virus. Arch. Pediatr. Adolesc. Med. 2000, 154, 240–244. [Google Scholar] [CrossRef]
- Wood, S.M.; Shah, S.S.; Steenhoff, A.P.; Rutstein, R.M. The impact of AIDS diagnoses on long-term neurocognitive and psychiatric outcomes of surviving adolescents with perinatally acquired HIV. AIDS 2009, 23, 1859–1865. [Google Scholar] [CrossRef]
- Kamau, J.W.; Kuria, W.; Mathai, M.; Atwoli, L.; Kangethe, R. Psychiatric morbidity among HIV-infected children and adolescents in a resource-poor Kenyan urban community. AIDS Care 2012, 24, 836–842. [Google Scholar] [CrossRef]
- Nomoto, S.H.; Longhi, R.M.; de Barros, B.P.; Croda, J.; Ziff, E.B.; Konkiewitz, E.C. Socioeconomic disadvantage increasing risk for depression among recently diagnosed HIV patients in an urban area in Brazil: Cross-sectional study. AIDS Care 2015, 27, 979–985. [Google Scholar] [CrossRef]
- Rasmussen, L.D.; Obel, D.; Kronborg, G.; Larsen, C.S.; Pedersen, C.; Gerstoft, J.; Obel, N. Utilization of psychotropic drugs prescribed to persons with and without HIV infection: A Danish nationwide population-based cohort study. HIV Med. 2014, 15, 458–469. [Google Scholar] [CrossRef] [PubMed]
- Gibbie, T.; Mijch, A.; Ellen, S.; Hoy, J.; Hutchison, C.; Wright, E.; Chua, P.; Judd, F. Depression and neurocognitive performance in individuals with HIV/AIDS: 2-year follow-up. HIV Med. 2006, 7, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Kacanek, D.; Jacobson, D.; Spiegelman, D.; Wanke, C.; Issac, R.; Wilson, I.B. Incident depression symptoms are associated with poorer HAART adherence: A longitudinal analysis from the Nutrition for Healthy Living study. J. Acquir. Immune Defic. Syndr. 2010, 53, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Serrão, R.; Piñero, C.; Velez, J.; Coutinho, D.; Maltez, F.; Lino, S.; Sarmento e Castro, R.; Tavares, A.P.; Pacheco, P.; Lopes, M.J.; et al. Non-AIDS-related comorbidities in people living with HIV-1 aged 50 years and older: The AGING POSITIVE study. Int. J. Infect Dis. 2019, 79, 94–100. [Google Scholar] [CrossRef]
- Gaida, R.; Truter, I.; Grobler, C.; Kotze, T.; Godman, B. A review of trials investigating efavirenz-induced neuropsychiatric side effects and the implications. Expert Rev. Anti-Infect. Ther. 2016, 14, 377–388. [Google Scholar] [CrossRef]
- Dalwadi, D.A.; Ozuna, L.; Harvey, B.H.; Viljoen, M.; Schetz, J.A. Adverse Neuropsychiatric Events and Recreational Use of Efavirenz and other HIV-1 antiretroviral drugs. Pharmocol. Rev. 2018, 70, 684–711. [Google Scholar] [CrossRef]
- Cavalcante, G.I.T.; Chaves Filho, A.J.; Linhares, M.I.; de Carvalho Lima, C.N.; Venãncio, E.T.; Rios, E.R.; de Souza, F.C.; Vasconcelos, S.M.; Macêdo, D.; de França Fonteles, M.M. HIV antiretroviral drug Efavirenz induces anxiety-like and depression-like behavior in rats: Evaluation of neurotransmitter alterations in the striatum. Eur. J. Pharmacol. 2017, 799, 7–15. [Google Scholar] [CrossRef]
- Journot, V.; Chene, G.; De Castro, N.; Rancinan, C.; Cassuto, J.; Allard, C.; Vildé, J.L.; Sobel, A.; Carré, M.; Molina, J.M.; et al. Use of efavirenz is not associated with a higher risk of depressive disorders: A substudy of the randomized clinical trial ALIZE-ANRS 099. Clin. Infect. Dis. 2006, 42, 1790–1799. [Google Scholar] [CrossRef]
- Mollan, K.R.; Smurzynski, M.; Eron, J.J.; Daar, E.S.; Campbell, T.B.; Sax, P.E.; Gulick, R.M.; Na, L.; O’Keefe, L.; Robertson, K.R.; et al. Association between efavirenz as initial therapy for HIV-1 infection and increased risk for suicidal ideation or attempted or completed suicide an analysis of trial data. Ann. Intern. Med. 2014, 161, 1–10. [Google Scholar] [CrossRef]
- Gutiérrez, F.; García, L.; Padilla, S.; Alvarez, D.; Moreno, S.; Navarro, G.; Gómez-Sirvent, J.; Vidal, F.; Asensi, V.; Masiá, M.; et al. Risk of clinically significant depression in HIV-infected patients: Effect of antiretroviral drugs. HIV Med. 2014, 15, 213–223. [Google Scholar] [CrossRef]
- Chiang, T. Taiwan’s 1995 healthcare reform. Health Policy 1997, 39, 225–239. [Google Scholar] [CrossRef]
- Lévesque, L.E.; Hanley, J.A.; Kezouh, A.; Suissa, S. Problem of immortal time bias in cohort studies: Example using statins for preventing progression of diabetes. BMJ 2010, 340, b5087. [Google Scholar] [CrossRef] [PubMed]
- Eaton, E.F.; Gravett, R.M.; Tamhane, A.R.; Mugavero, M.J. Antiretroviral therapy initiation and changes in self-reported depression. Clin. Infect. Dis. 2017, 64, 1791–1794. [Google Scholar] [CrossRef] [PubMed]
- Nanni, M.G.; Caruso RMitchell, A.J.; Meggiolaro, E.; Grassi, L. Depression in HIV infected patients: A review. Curr. Psychiatry Rep. 2015, 17, 530. [Google Scholar] [CrossRef]
- Danzter, R.; O’Connor, J.C.; Freund, G.G.; Johnson, R.W.; Kelly, K.W. From inflmmation to sickness and depression: When the immune system subjugates the brain. Nat. Rev. Neurosci. 2008, 9, 46–56. [Google Scholar]
- Prasad, A.; Kulkarni, R.; Shrivastava, A.; Jiang, S.; Lawson, K.; Groopman, J.E. Methamphetamine functions as a novel CD4(+) T-cell activator via the sigma-1 receptor to enhance HIV-1 infection. Sci. Rep. 2019, 9, 958. [Google Scholar] [CrossRef]
- Yao, H.; Kim, K.; Duan, M.; Hayashi, T.; Guo, M.; Morgello, S.; Prat, A.; Wang, J.; Su, T.P.; Buch, S. Cocain hijacks σ1 receptor to initiate induction of activated leukocyte cell adhesion molecule: Implication for increased monocyte adhesion and migration in the CNS. J. Neurosci. 2011, 31, 5942–5955. [Google Scholar] [CrossRef]
- Danzter, R.; O’Connor, J.C.; Lawson, M.A.; Kelley, K.W. Inflammation-associated depression: From serotonin to kynurenine. Psychoneuroendocrinology 2011, 36, 426–436. [Google Scholar]
- Cavalcante, G.I.T.; Capistrano, V.L.M.; Cavalcante, F.S.D.; Macedo, D.S.; Sousa, F.C.F.; Woods, D.J.; Fonteles, M.M.F. Implications of efavirenz for neuropsychiatry: A review. Int. J. Neurosci. 2010, 120, 739–745. [Google Scholar] [CrossRef]
- Nguyen, L.; Thomas, K.L.; Lucke-Wold, B.P.; Cavendish, J.Z.; Crowe, M.S.; Matsumoto, R.R. Dextromethorphan: An update on its utility for neurological and neuropsyhciatric disorders. Pharmacol. Ther. 2016, 159, 1–22. [Google Scholar] [CrossRef]
- Nguyen, L.; Lucke-Wold, B.P.; Logsdon, A.F.; Scandinaro, A.L.; Huber, J.D.; Matsumoto, R.R. Behavioral and biochemial effects of ketamine and dextromethorphan relative to its antidepressant-like effects in Swiss Webster mice. Neuroreport 2016, 27, 1004–1011. [Google Scholar] [CrossRef] [PubMed]
- Glynn, T.R.; Llabre, M.M.; Lee, J.S.; Bedoya, C.A.; Pinkston, M.M.; O’Cleirigh, C.; Safren, S.A. Pathways to health: An examination of HIV-related stigma, life stressors, depression, and substance use. Int. J. Behav. Med. 2019, 26, 286–296. [Google Scholar] [CrossRef] [PubMed]
- Boyd, S. Management of HIV infection in treatment- naïve patients: A review of the most current recommendations. Am. J. Health Syst. Pharm. 2011, 68, 991–1001. [Google Scholar] [CrossRef] [PubMed]
- Churchill, D.; Waters, L.; Ahmed, N.; Angus, B.; Boffito, M.; Bower, M.; Dunn, D.; Edwards, S.; Emerson, C.; Fidler, S.; et al. British HIV Association guidelines for the treatment of HIV-1-positive adults with antriretroviral therapy 2015. HIV Med. 2016, 17, s2–s104. [Google Scholar] [CrossRef]
| Variables | Efavirenz-Treated Group (n = 4047) | Non-Efavirenz Treated Group (n = 3239) | p Value |
|---|---|---|---|
| Gender | 0.282 | ||
| Male | 3777 (93.3) | 3043 (93.9) | |
| Female | 270 (6.7) | 196 (6.1) | |
| Age of HIV diagnosis, years | 35.0 (20–81, 10.4) | 35.1 (20–81, 10.6) | 0.658 |
| 20–29 | 1453 (35.9) | 1209 (37.3) | 0.554 |
| 30–39 | 1561 (38.6) | 1191 (36.8) | |
| 40–49 | 654 (16.2) | 521 (16.1) | |
| 50–59 | 257 (6.3) | 219 (6.7) | |
| ≥60 | 122 (3.0) | 99 (3.1) | |
| Residence area | <0.001 | ||
| North | 2109 (52.1) | 2037 (62.9) | |
| Central | 667 (16.5) | 455 (14.0) | |
| South | 1121 (27.7) | 628 (19.4) | |
| East and outer islands | 150 (3.7) | 119 (3.7) | |
| Insurance premium based monthly income, NTD | 0.005 | ||
| ≤17,280 | 1940 (47.9) | 1488 (45.9) | |
| 17,281–26,400 | 1058 (26.2) | 790 (24.4) | |
| 26,401–43,900 | 649 (16.0) | 591 (18.3) | |
| ≥43,901 | 400 (9.9) | 370 (11.4) | |
| Comorbidities | |||
| Opportunistic infections | 2268 (56.0) | 1675 (51.7) | <0.001 |
| Hypertension | 147 (3.6) | 129 (4.0) | 0.436 |
| Diabetes mellitus | 93 (2.3) | 84 (2.6) | 0.416 |
| Cardiovascular diseases | 26 (0.6) | 32 (0.9) | 0.099 |
| Psychiatric disorders (other than depressive disorders) | 239 (5.9) | 208 (6.4) | 0.362 |
| Observation time, mean (range, SD), years | 6.1 (0–11, 3.9) | 4.7 (0–11, 3.16) | <0.001 |
| Depressive disorders | 304 (7.5) | 191 (5.9) | <0.001 |
| No. of Depressive Disorders/Total No. | Crude | Adjusted | |||
|---|---|---|---|---|---|
| RR (95% CI) | p Value | HR (95% CI) | p Value | ||
| Efavirenz use | |||||
| Yes | 304/4047 | 1.25 (1.05–1.50) | 0.011 | 0.92 (0.76–1.10) | 0.353 |
| No | 191/3239 | 1.00 | 1.00 | ||
| Gender | |||||
| Male | 459/6820 | 1.00 | 1.00 | ||
| Female | 36/466 | 1.14 (0.82–1.58) | 0.441 | 0.81 (0.57–1.14) | 0.222 |
| Age of HIV diagnosis, years | |||||
| 20–29 | 189/2662 | 1.00 | 1.00 | ||
| 30–39 | 190/2752 | 0.97 (0.80–1.18) | 0.792 | 0.88 (0.72–1.08) | 0.225 |
| 40–49 | 65/1175 | 0.79 (0.60–1.04) | 0.093 | 0.79 (0.60–1.06) | 0.113 |
| 50–59 | 37/476 | 1.09 (0.77–1.53) | 0.627 | 0.85 (0.59–1.23) | 0.738 |
| ≥60 | 14/221 | 0.90 (0.53–1.52) | 0.691 | 0.58 (0.33–1.02) | 0.056 |
| Insurance premium-based monthly income, NTD | |||||
| ≤17,280 | 304/3428 | 2.04 (1.43–2.92) | <0.001 | 2.59 (1.79–3.76) | <0.001 |
| 17,281–26,400 | 114/1848 | 1.46 (0.99–2.14) | 0.054 | 1.55 (1.04–2.31) | 0.030 |
| 26,401–43,900 | 45/1240 | 0.88 (0.56–1.37) | 0.565 | 0.94 (0.59–1.48) | 0.774 |
| ≥43,901 | 32/770 | 1.00 | 1.00 | ||
| Residence area | |||||
| Northern | 259/4146 | 1.00 | 1.00 | ||
| Central | 81/1122 | 1.15 (0.90–1.46) | 0.271 | 1.24 (0.96–1.59) | 0.101 |
| Southern | 139/1770 | 1.24 (1.02–1.51) | 0.035 | 1.49 (1.21–1.84) | <0.001 |
| Eastern and outer islands | 16/248 | 1.03 (0.63–1.68) | 0.903 | 0.99 (0.60–1.64) | 0.966 |
| Comorbidities | |||||
| Opportunistic infections | 245/3943 | 0.85 (0.71–0.99) | 0.046 | 0.80 (0.67–0.95) | 0.011 |
| Hypertension | 18/276 | 0.96 (0.61–1.52) | 0.864 | 1.21 (0.72–2.02) | 0.476 |
| Diabetes mellitus | 10/177 | 0.84 (0.46–1.54) | 0.568 | 1.03 (0.54–1.97) | 0.926 |
| Cardiovascular diseases | 3/58 | 0.77 (0.26–2.33) | 0.646 | 1.29 (0.40–4.14) | 0.669 |
| Psychiatric disorders (other than depressive disorders) | 67/447 | 2.21 (1.74–2.82) | <0.001 | 4.59 (3.51–6.01) | <0.001 |
| Scenario 1 a | Scenario 2 b | Scenario 3 c | |||||||
|---|---|---|---|---|---|---|---|---|---|
| aHR | 95% CI | p Value | aHR | 95% CI | p Value | aHR | 95% CI | p Value | |
| Efavirenz use | 0.83 | 0.68–1.01 | 0.068 | 0.97 | 0.81–1.17 | 0.744 | 0.76 | 0.61–0.96 | 0.018 |
| Monthly insurance premium, NTD | |||||||||
| ≤17,280 | 2.93 | 1.93–4.44 | <0.001 | 2.93 | 1.93–4.44 | <0.001 | 2.53 | 1.62–3.97 | <0.001 |
| 17,281–26,400 | 1.71 | 1.09–2.67 | 0.020 | 1.72 | 1.10–2.68 | 0.018 | 1.63 | 1.01–2.64 | 0.045 |
| 26,401–43,900 | 0.96 | 0.57–1.61 | 0.867 | 0.96 | 0.57–1.61 | 0.870 | 0.94 | 0.54–1.63 | 0.812 |
| ≥43,901 | 1.00 | 1.00 | 1.00 | ||||||
| Residence area | |||||||||
| Northern | 1.00 | 1.00 | 1.00 | ||||||
| Central | 1.14 | 0.86–1.52 | 0.366 | 1.14 | 0.86–1.52 | 0.365 | 1.14 | 0.82–1.58 | 0.451 |
| Southern | 1.36 | 1.07–1.73 | 0.014 | 1.36 | 1.06–1.73 | 0.014 | 1.54 | 1.17–2.02 | 0.002 |
| Eastern and outer islands | 0.92 | 0.51–1.64 | 0.765 | 0.94 | 0.53–1.69 | 0.844 | 1.15 | 0.62–2.13 | 0.650 |
| Opportunistic infections | 0.88 | 0.72–1.07 | 0.204 | 0.88 | 0.72–1.07 | 0.187 | 0.89 | 0.71–1.11 | 0.292 |
| Psychiatric disorders other than depression | 4.07 | 2.96–6.00 | <0.001 | 4.08 | 2.97–5.61 | <0.001 | 4.89 | 4.47–6.89 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, C.-W.; Chen, Y.-C.; Lee, N.-Y.; Chen, P.-L.; Li, M.-C.; Li, C.-Y.; Ko, W.-C.; Ko, N.-Y. Efavirenz Is Not Associated with an Increased Risk of Depressive Disorders in Patients Living with HIV: An 11-Year Population-Based Study in Taiwan. Healthcare 2021, 9, 1625. https://doi.org/10.3390/healthcare9121625
Li C-W, Chen Y-C, Lee N-Y, Chen P-L, Li M-C, Li C-Y, Ko W-C, Ko N-Y. Efavirenz Is Not Associated with an Increased Risk of Depressive Disorders in Patients Living with HIV: An 11-Year Population-Based Study in Taiwan. Healthcare. 2021; 9(12):1625. https://doi.org/10.3390/healthcare9121625
Chicago/Turabian StyleLi, Chia-Wen, Yen-Chin Chen, Nan-Yao Lee, Po-Lin Chen, Ming-Chi Li, Chung-Yi Li, Wen-Chien Ko, and Nai-Ying Ko. 2021. "Efavirenz Is Not Associated with an Increased Risk of Depressive Disorders in Patients Living with HIV: An 11-Year Population-Based Study in Taiwan" Healthcare 9, no. 12: 1625. https://doi.org/10.3390/healthcare9121625
APA StyleLi, C.-W., Chen, Y.-C., Lee, N.-Y., Chen, P.-L., Li, M.-C., Li, C.-Y., Ko, W.-C., & Ko, N.-Y. (2021). Efavirenz Is Not Associated with an Increased Risk of Depressive Disorders in Patients Living with HIV: An 11-Year Population-Based Study in Taiwan. Healthcare, 9(12), 1625. https://doi.org/10.3390/healthcare9121625







