Clinical and Humanistic Outcomes of Community Pharmacy-Based Healthcare Interventions Regarding Medication Use in Older Adults: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
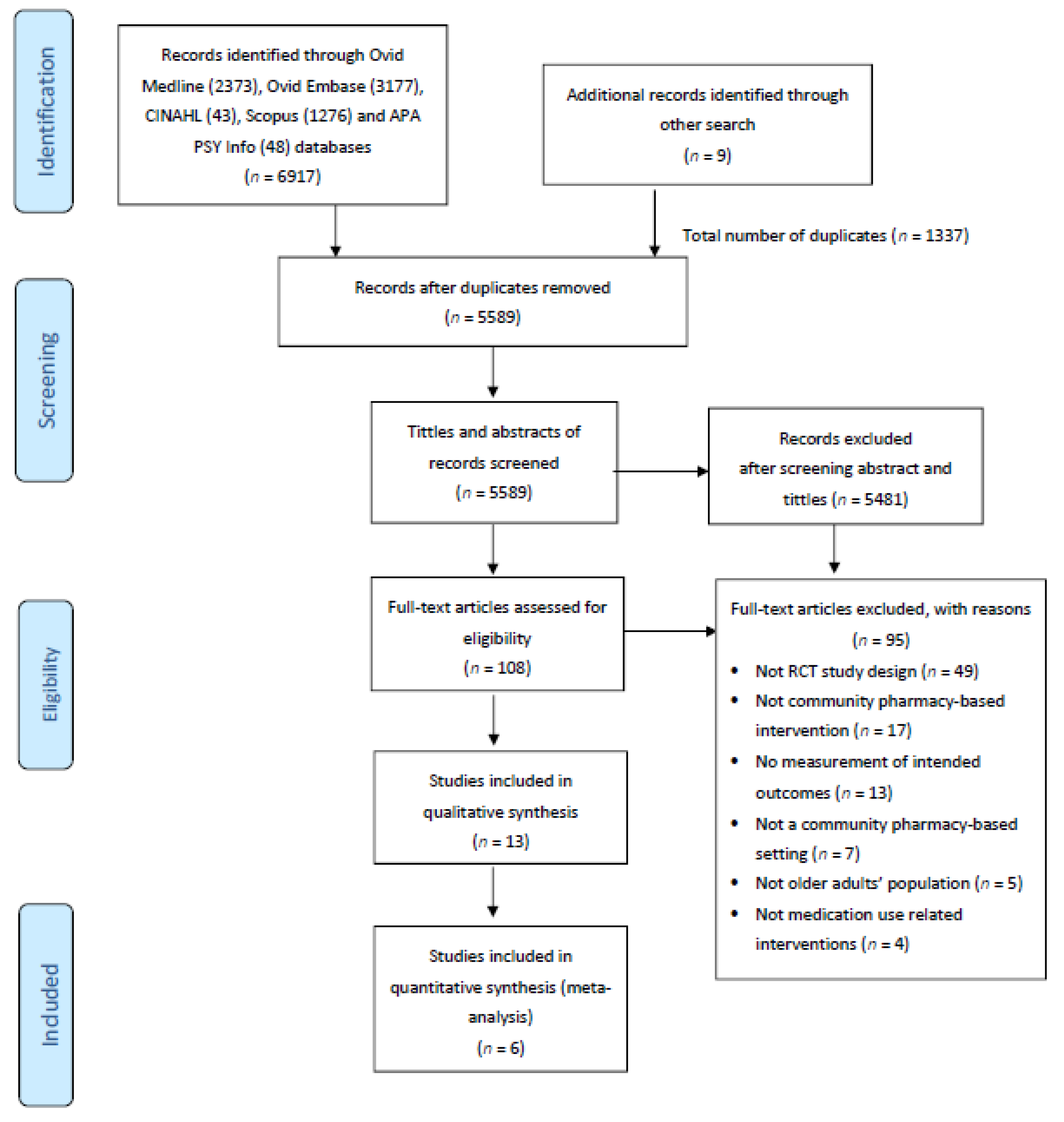
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Study Selection
2.4. Data Extraction
2.5. Risk of Bias (Quality Assessment)
2.6. Data Analysis
3. Results
3.1. Characteristics of Included Studies
3.2. Risk of Bias Assessment
3.3. Types of Community Pharmacists’ Interventions
3.3.1. Medication Review
3.3.2. Educational Intervention
3.3.3. Pharmaceutical Care
3.3.4. Electronic Reminder Device
3.4. The Outcomes of the Interventions
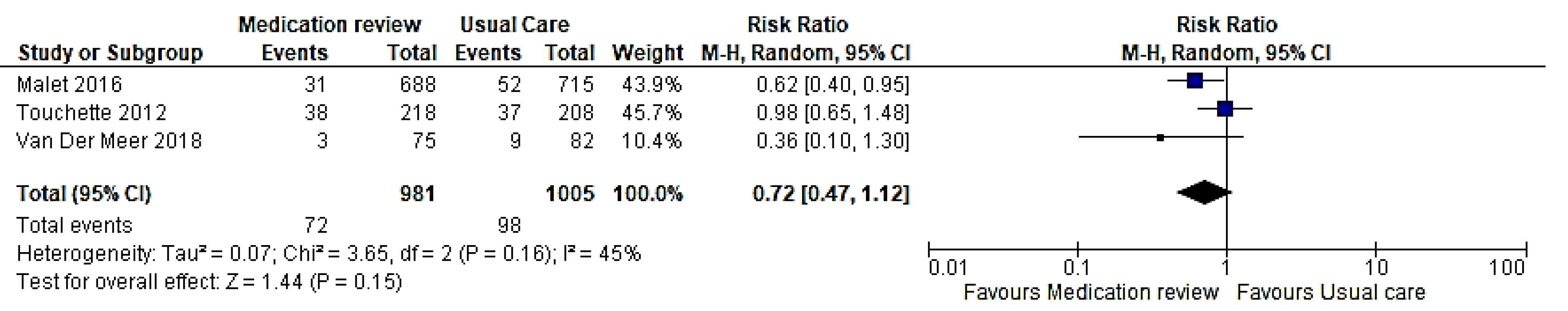
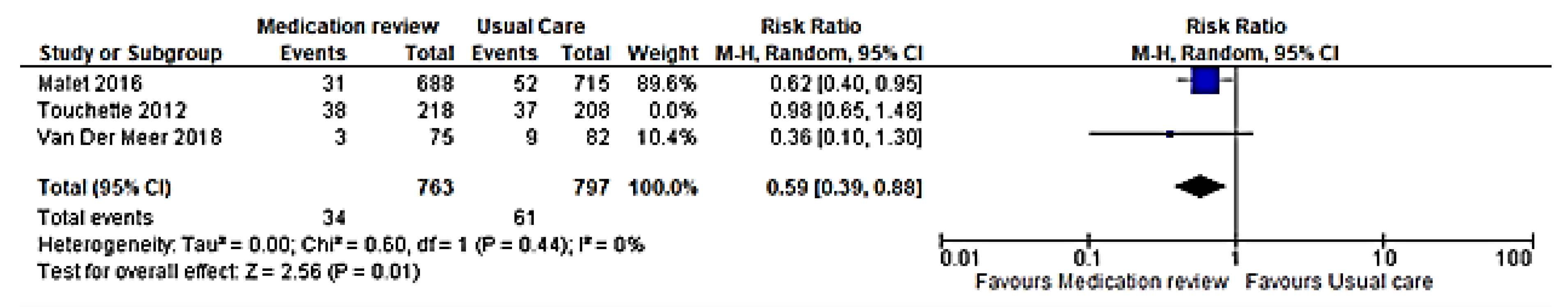
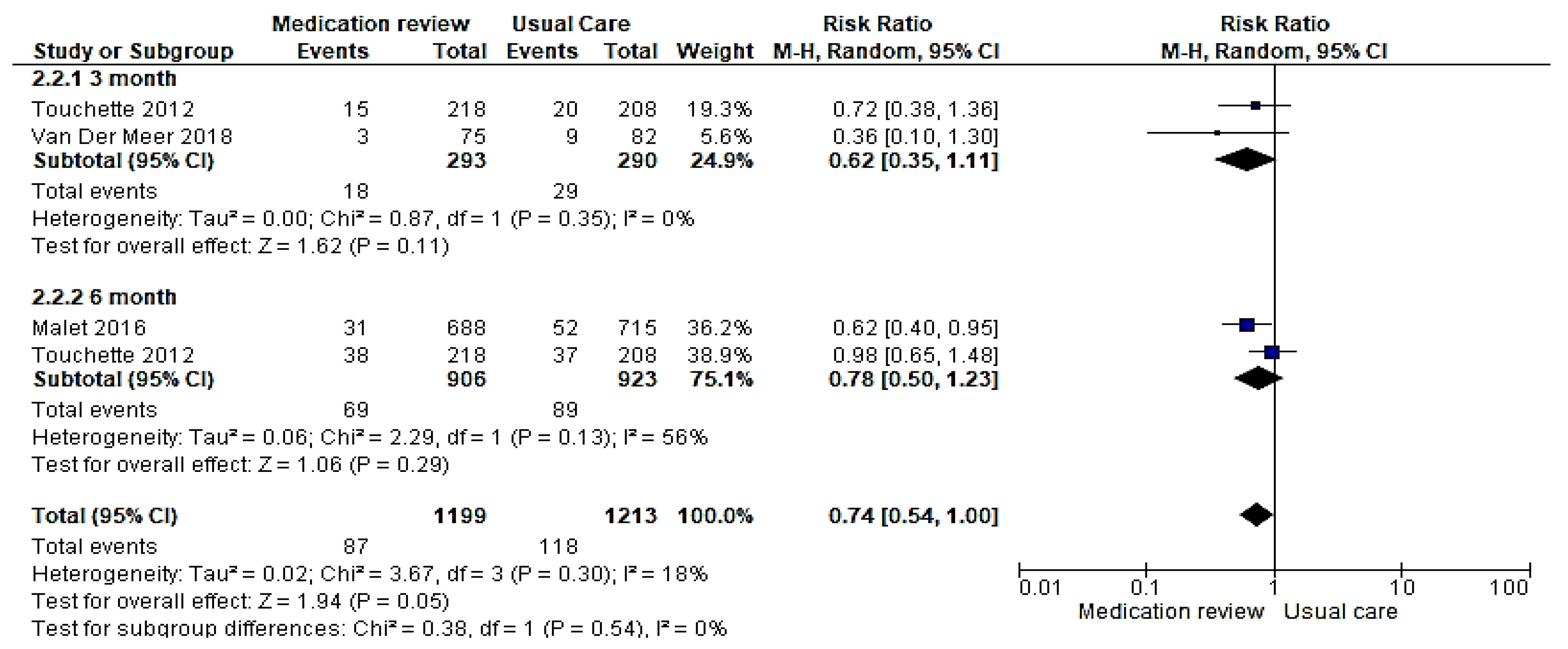
3.4.1. Hospitalization
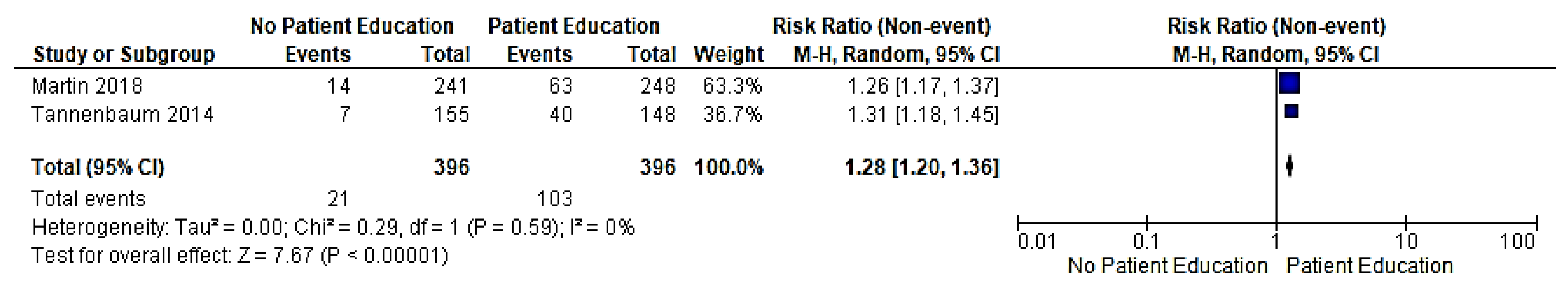
3.4.2. Sedative–Hypnotics Users
3.4.3. Number of Older Adults Who Fall
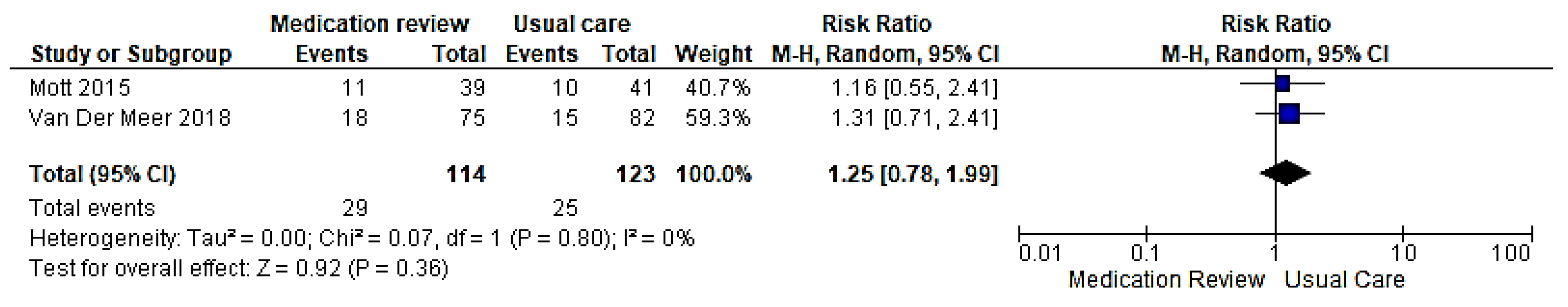
3.4.4. Potentially Inappropriate Medications
3.4.5. Medication Adherence
3.4.6. Adverse Drug Events
3.4.7. Other Outcomes
3.5. Sensitivity Analysis
3.6. Subgroup Analysis
3.7. Certainty of Evidence
4. Discussion
4.1. Strengths and Limitation
4.2. Implications for Research and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- He, W.; Goodkind, D.; Kowal, P.R. An Aging World, International Population Reports; U.S. Government Printing Office: Washington, DC, USA, 2015. [Google Scholar]
- Amoako, E.P.; Richardson-Campbell, L.; Kennedy-Malone, L. Self-Medication with Over-The-Counter Drugs Among Elderly Adults. J. Gerontol. Nurs. 2003, 29, 10–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.; Parish, A.L. Polypharmacy and Medication Management in Older Adults. Nurs. Clin. N. Am. 2017, 52, 457–468. [Google Scholar] [CrossRef] [PubMed]
- Scott, I.A.; Hilmer, S.N.; Reeve, E.; Potter, K.; Le Couteur, D.; Rigby, D.; Gnjidic, D.; Del Mar, C.B.; Roughead, E.E.; Page, A.; et al. Reducing Inappropriate Polypharmacy. JAMA Intern. Med. 2015, 175, 827–834. [Google Scholar] [CrossRef] [Green Version]
- Balbuena, F.R.; Aranda, A.B.; Figueras, A. Self-Medication in Older Urban Mexicans. Drugs Aging 2009, 26, 51–60. [Google Scholar] [CrossRef]
- Chiatti, C.; Bustacchini, S.; Furneri, G.; Mantovani, L.G.; Cristiani, M.; Misuraca, C.; Lattanzio, F. The Economic Burden of Inappropriate Drug Prescribing, Lack of Adherence and Compliance, Adverse Drug Events in Older People. Drug Saf. 2012, 35, 73–87. [Google Scholar] [CrossRef]
- Aparasu, R.R.; Mort, J.R. Prevalence, correlates, and associated outcomes of potentially inappropriate psychotropic use in the community-dwelling elderly. Am. J. Geriatr. Pharmacother. 2004, 2, 102–111. [Google Scholar] [CrossRef]
- Bennett, J.A.; Flaherty-Robb, M.K. Issues affecting the health of older citizens: Meeting the challenge. Online J. Issues Nurs. 2003, 8, 2. [Google Scholar]
- Baillie, L.; Gallini, A.; Corser, R.; Elworthy, G.; Scotcher, A.; Barrand, A. Care transitions for frail, older people from acute hospital wards within an integrated healthcare system in England: A qualitative case study. Int. J. Integr. Care 2014, 14, e009. [Google Scholar] [CrossRef] [Green Version]
- Ramsbottom, H.; Rutter, P.; Fitzpatrick, R. Post discharge medicines use review (dMUR) service for older patients: Cost-savings from community pharmacist interventions. Res. Soc. Adm. Pharm. 2018, 14, 203–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramsbottom, H.F.; Fitzpatrick, R.; Rutter, P. Post discharge medicines use review service for older patients: Recruitment issues in a feasibility study. Int. J. Clin. Pharm. 2016, 38, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Rutter, P.; Ramsbottom, H.; Fitzpatrick, R. Community pharmacist perceptions of delivering post-hospital discharge Medicines Use Reviews for elderly patients. Int. J. Clin. Pharm. 2017, 39, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Kayyali, R.; Funnell, G.; Harrap, N.; Patel, A. Can community pharmacy successfully bridge the gap in care for housebound patients? Res. Soc. Adm. Pharm. 2019, 15, 425–439. [Google Scholar] [CrossRef] [Green Version]
- Foubert, K.; Mehuys, E.; Claes, L.; Abeele, D.V.D.; Haems, M.; Somers, A.; Petrovic, M.; Boussery, K. A shared medication scheme for community dwelling older patients with polypharmacy receiving home health care: Role of the community pharmacist. Acta Clin. Belg. 2018, 74, 326–333. [Google Scholar] [CrossRef]
- Kallio, S.E.; Kiiski, A.; Airaksinen, M.S.; Mäntylä, A.T.; Kumpusalo-Vauhkonen, A.E.; Järvensivu, T.P.; Pohjanoksa-Mäntylä, M.K. Community Pharmacists’ Contribution to Medication Reviews for Older Adults: A Systematic Review. J. Am. Geriatr. Soc. 2018, 66, 1613–1620. [Google Scholar] [CrossRef]
- Tasai, S.; Kumpat, N.; Dilokthornsakul, P.; Chaiyakunapruk, N.; Saini, B.; Dhippayom, T. Impact of Medication Reviews Delivered by Community Pharmacist to Elderly Patients on Polypharmacy: A Meta-analysis of Randomized Controlled Trials. J. Patient Saf. 2021, 17, 290–298. [Google Scholar] [CrossRef]
- Jokanovic, N.; Tan, E.; Sudhakaran, S.; Kirkpatrick, C.; Dooley, M.J.; Ryan-Atwood, T.E.; Bell, J.S. Pharmacist-led medication review in community settings: An overview of systematic reviews. Res. Soc. Adm. Pharm. 2017, 13, 661–685. [Google Scholar] [CrossRef] [PubMed]
- Banning, M. A review of interventions used to improve adherence to medication in older people. Int. J. Nurs. Stud. 2009, 46, 1505–1515. [Google Scholar] [CrossRef]
- Loganathan, M.; Singh, S.; Franklin, B.D.; Bottle, A.; Majeed, A. Interventions to optimise prescribing in care homes: Systematic review. Age Ageing 2011, 40, 150–162. [Google Scholar] [CrossRef] [Green Version]
- Cooper, J.A.; Cadogan, C.A.; Patterson, S.M.; Kerse, N.; Bradley, M.C.; Ryan, C.; Hughes, C.M. Interventions to improve the appropriate use of polypharmacy in older people: A Cochrane systematic review. BMJ Open 2015, 5, e009235. [Google Scholar] [CrossRef] [Green Version]
- Clyne, B.; Fitzgerald, C.; Quinlan, A.; Hardy, C.; Galvin, R.; Fahey, T.; Smith, S. Interventions to Address Potentially Inappropriate Prescribing in Community-Dwelling Older Adults: A Systematic Review of Randomized Controlled Trials. J. Am. Geriatr. Soc. 2016, 64, 1210–1222. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Bryant, L.J.; Coster, G.; Gamble, G.; McCormick, R.N. The General Practitioner–Pharmacist Collaboration (GPPC) study: A randomised controlled trial of clinical medication reviews in community pharmacy. Int. J. Pharm. Pract. 2011, 19, 94–105. [Google Scholar] [CrossRef]
- Falamić, S.; Lucijanic, M.; Ortner-Hadžiabdić, M.; Marušić, S.; Bačić-Vrca, V. Pharmacists’ influence on adverse reactions to warfarin: A randomised controlled trial in elderly rural patients. Int. J. Clin. Pharm. 2019, 41, 1166–1173. [Google Scholar] [CrossRef] [PubMed]
- Mott, D.A.; Martin, B.; Breslow, R.; Michaels, B.; Kirchner, J.; Mahoney, J.; Margolis, A. Impact of a medication therapy management intervention targeting medications associated with falling: Results of a pilot study. J. Am. Pharm. Assoc. 2016, 56, 22–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Touchette, D.R.; Masica, A.L.; Dolor, R.; Schumock, G.T.; Choi, Y.K.; Kim, Y.; Smith, S.R. Safety-focused medication therapy management: A randomized controlled trial. J. Am. Pharm. Assoc. 2012, 52, 603–612. [Google Scholar] [CrossRef]
- Varas-Doval, R.; Gastelurrutia, M.A.; Benrimoj, S.I.; García-Cárdenas, V.; Sáez-Benito, L.; Martinez-Martínez, F. Clinical impact of a pharmacist-led medication review with follow up for aged polypharmacy patients: A cluster randomized controlled trial. Pharm. Pract. 2020, 18, 2133. [Google Scholar] [CrossRef] [PubMed]
- Olesen, C.; Harbig, P.; Buus, K.M.; Barat, I.; Damsgaard, E.M. Impact of pharmaceutical care on adherence, hospitalisations and mortality in elderly patients. Int. J. Clin. Pharm. 2013, 36, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Toivo, T.; Airaksinen, M.; Dimitrow, M.; Savela, E.; Pelkonen, K.; Kiuru, V.; Suominen, T.; Uunimäki, M.; Kivelä, S.-L.; Leikola, S.; et al. Enhanced coordination of care to reduce medication risks in older home care clients in primary care: A randomized controlled trial. BMC Geriatr. 2019, 19, 332. [Google Scholar] [CrossRef] [PubMed]
- Malet-Larrea, A.; Goyenechea, E.; García-Cárdenas, V.; Calvo, B.; Arteche, J.M.; Aranegui, P.; Zubeldia, J.J.; Gastelurrutia, M.A.; Martínez-Martínez, F.; Benrimoj, S. The impact of a medication review with follow-up service on hospital admissions in aged polypharmacy patients. Br. J. Clin. Pharmacol. 2016, 82, 831–838. [Google Scholar] [CrossRef] [Green Version]
- Tannenbaum, C.; Martin, P.; Tamblyn, R.; Benedetti, A.; Ahmed, S. Reduction of Inappropriate Benzodiazepine Prescriptions Among Older Adults Through Direct Patient Education. JAMA Intern. Med. 2014, 174, 890–898. [Google Scholar] [CrossRef] [Green Version]
- Van der Meer, H.; Wouters, H.; Pont, L.G.; Taxis, K. Reducing the anticholinergic and sedative load in older patients on polypharmacy by pharmacist-led medication review: A randomised controlled trial. BMJ Open 2018, 8, e019042. [Google Scholar] [CrossRef] [Green Version]
- Martin, P.; Tamblyn, R.; Benedetti, A.; Ahmed, S.; Tannenbaum, C. Effect of a pharmacist-led educational intervention on inap-propriate medication prescriptions in older adults: The D-PRESCRIBE randomized clinical trial. JAMA 2018, 320, 1889–1898. [Google Scholar] [CrossRef]
- Falamić, S.; Lucijanic, M.; Hadžiabdić, M.O.; Marušić, S.; Vrca, V.B. Pharmacist’s interventions improve time in therapeutic range of elderly rural patients on warfarin therapy: A randomized trial. Int. J. Clin. Pharm. 2018, 40, 1078–1085. [Google Scholar] [CrossRef]
- Kooy, M.; Van Wijk, B.L.; Heerdink, E.R.; De Boer, A.; Bouvy, M.L. Does the use of an electronic reminder device with or without counseling improve adherence to lipid-lowering treatment? The results of a randomized controlled trial. Front. Pharmacol. 2013, 4, 69. [Google Scholar] [CrossRef] [Green Version]
- Gudi, S.K.; Kashyap, A.; Chhabra, M.; Rashid, M.; Tiwari, K.K. Impact of pharmacist-led home medicines review services on drug-related problems among the elderly population: A systematic review. Epidemiol. Health 2019, 41, e2019020. [Google Scholar] [CrossRef] [PubMed]
- Tecklenborg, S.; Byrne, C.; Cahir, C.; Brown, L.; Bennett, K. Interventions to Reduce Adverse Drug Event-Related Outcomes in Older Adults: A Systematic Review and Meta-analysis. Drugs Aging 2020, 37, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Thiruchelvam, K.; Hasan, S.S.; Wong, P.S.; Kairuz, T. Residential Aged Care Medication Review to Improve the Quality of Medication Use: A Systematic Review. J. Am. Med. Dir. Assoc. 2017, 18, 87.e1–87.e14. [Google Scholar] [CrossRef]
- Yuan, C.; Ding, Y.; Zhou, K.; Huang, Y.; Xi, X. Clinical outcomes of community pharmacy services: A systematic review and meta-analysis. Health Soc. Care Community 2019, 27, e567–e587. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Babtain, B.; Cheema, E.; Hadi, M.A. Impact of community-pharmacist-led medication review programmes on patient outcomes: A systematic review and meta-analysis of randomised controlled trials. Res. Soc. Adm. Pharm. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Dawoud, D.M.; Haines, A.; Wonderling, D.; Ashe, J.; Hill, J.; Varia, M.; Dyer, P.; Bion, J. Cost Effectiveness of Advanced Pharmacy Services Provided in the Community and Primary Care Settings: A Systematic Review. PharmacoEconomics 2019, 37, 1241–1260. [Google Scholar] [CrossRef] [PubMed]
- Milosavljevic, A.; Aspden, T.; Harrison, J. Community pharmacist-led interventions and their impact on patients’ medication adherence and other health outcomes: A systematic review. Int. J. Pharm. Pract. 2018, 26, 387–397. [Google Scholar] [CrossRef]
- Varas-Doval, R.; Saéz-Benito, L.; Gastelurrutia, M.A.; Benrimoj, S.I.; Garcia-Cardenas, V.; Martinez-Martínez, F. Systematic review of pragmatic randomised control trials assessing the effectiveness of professional pharmacy services in community pharmacies. BMC Health Serv. Res. 2021, 21, 156. [Google Scholar] [CrossRef] [PubMed]
- Dou, C.; Rebane, J.; Bardal, S. Interventions to improve benzodiazepine tapering success in the elderly: A systematic review. Aging Ment. Health 2018, 23, 411–416. [Google Scholar] [CrossRef]
- Reeve, E.; Ong, M.; Wu, A.; Jansen, J.; Petrovic, M.; Gnjidic, D. A systematic review of interventions to deprescribe benzodiazepines and other hypnotics among older people. Eur. J. Clin. Pharmacol. 2017, 73, 927–935. [Google Scholar] [CrossRef]
- Huiskes, V.J.B.; Burger, D.M.; van den Ende, C.H.M.; van den Bemt, B.J.F. Effectiveness of medication review: A systematic review and meta-analysis of randomized controlled trials. BMC Fam. Pract. 2017, 18, 5. [Google Scholar] [CrossRef] [Green Version]
- Holland, R.; Desborough, J.; Goodyer, L.; Hall, S.; Wright, D.; Loke, Y.K. Does pharmacist-led medication review help to reduce hospital admissions and deaths in older people? A systematic review and meta-analysis. Br. J. Clin. Pharmacol. 2008, 65, 303–316. [Google Scholar] [CrossRef] [Green Version]
- Wallerstedt, S.M.; Kindblom, J.; Nylén, K.; Samuelsson, O.; Strandell, A. Medication reviews for nursing home residents to reduce mortality and hospitalization: Systematic review and meta-analysis. Br. J. Clin. Pharmacol. 2014, 78, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Hart, L.A.; Phelan, E.A.; Yi, J.Y.; Marcum, Z.A.; Gray, S.L. Use of Fall Risk–Increasing Drugs Around a Fall-Related Injury in Older Adults: A Systematic Review. J. Am. Geriatr. Soc. 2020, 68, 1334–1343. [Google Scholar] [CrossRef] [PubMed]
- Crilly, P.; Kayyali, R. A Systematic Review of Randomized Controlled Trials of Telehealth and Digital Technology Use by Community Pharmacists to Improve Public Health. Pharmarcy 2020, 8, 137. [Google Scholar] [CrossRef] [PubMed]
- Barton, S. Which clinical studies provide the best evidence? The best RCT still trumps the best observational study. BMJ 2000, 321, 255–256. [Google Scholar] [CrossRef] [PubMed]

| Author, Year, Country | Study Design, Settings | Interventions | Control Sample Size | Intervention Sample Size | Follow-Up Period | Outcomes | Conclusion |
|---|---|---|---|---|---|---|---|
| Bryant et al. [28] (2010) New Zealand | Randomized, controlled trial, Community pharmacy | IG: Medication review was completed with the access of medical records from GP. A care plan was prepared, and discussions were completed among CP and GP. Follow-up consultations with patients were completed after taking action on the care plan. CG: Usual care | 143 | 207 | 6 months and 12 months | Quality of Life (SF-36) and Medication Inappropriateness Index (MAI), number of inappropriate medications | Medication review improved MAI and reduced the number of potentially inappropriate medicines at 6 months follow-up. However, this intervention did not produce a significant improvement in quality of life. |
| Falamic et al. [29] (2019) Croatia | Randomized, controlled trial, Community pharmacy | IG: Education with follow-up plan (given pillbox and plan form) CG: Standard GP-managed care | 66 | 65 | 6 months | The incidence and type of adverse drug reactions caused by warfarin | The cumulative incidence of adverse drug reactions was significantly lower in the intervention group. |
| Mott et al. [30] (2016) United States | Cluster-randomized, controlled trial, Community pharmacy | IG: Medication therapy management with follow-up CG: Received mailed pamphlet describing medication use and falls | 41 | 39 | 6 months | Rate of discontinuing the fall-risk inducing drug | Medication review significantly improved the rate of discontinuation of fall-risk-inducing drugs among older adults and reduced the number of falls. |
| Touchette et al. [31] (2012) United States | Randomized, controlled trial, Academic medical center, community pharmacies, and family medicine clinics | IG: Medication therapy management (MTM) with follow-up (enhanced MTM) CG: Usual care | 208 | Basic MTM = 211 Enhanced MTM = 218 | 6 months | Frequency of adverse drug events and hospitalization | Medication review did not have a beneficial impact on adverse drug events and hospitalization. |
| Varas–Doval et al. [32] (2020) Spain | Open-label, multi-center, cluster-randomized, controlled trial, Community pharmacy | IG: Medication review with follow-up CG: Usual care | 715 | 688 | 6 months | Uncontrolled health problems | Medication review benefited, with a significant reduction in the number of uncontrolled health problems. |
| Olesen et al. [33] (2014) Denmark | Cluster-randomized, controlled trial, Patient’s home | IG: Pharmaceutical care (examining medication list of older adults, answering any questions on their medications, providing leaflets and motivational adherence support) CG: Usual care | 264 | 253 | 3, 6, 9, and 24 months | Medication adherence, hospitalization, and mortality | Pharmaceutical care did not bring a beneficial impact on medication adherence, hospitalization, and mortality among older adults. |
| Toivo et al. [34] (2019) Finland | Cluster-randomized, controlled trial, Community pharmacy, homecare units, public health care center | IG: Collaborative coordination of care (medication review and triage meeting) CG: Standard home care | 87 | 104 | 12 months | Potentially inappropriate medication | No significant findings were found on the impact of coordination of care on outcomes of older adults’ health. |
| Malet-Larrea et al. [35] (2016) Spain | Cluster-randomized, controlled trial, Community pharmacy | IG: Medication review with follow-up CG: Usual care | 715 | 688 | 6 months | Hospitalization | The probability of being hospitalized was 3.7 times higher in the non-intervention group. Thus, medication review had reduced the number of older adults hospitalized. |
| Tannenbaum et al. [36] (2014) Canada | Cluster-randomized, controlled trial. Community pharmacy | IG: Patient education (materials which also contained benzodiazepine safety and tapering dose) CG: Usual care | 155 | 148 | 6 months | Benzodiazepine therapy discontinuation | Patient education improved the benzodiazepine discontinuation rate among older adults. |
| Van Der Meer et al. [37] (2018) Netherlands | Single-blind, randomized, controlled trial, Community pharmacy | IG: Medication review with follow-up CG: Usual care | 82 | 75 | 3 months | Drug burden index, hospitalization | Medication review did not have significant effects on the number of falls and hospitalization. Moreover, it did not produce an impact on the difference in drug burden index between groups. |
| Martin et al. [38] (2018) Canada | Cluster-randomized, controlled trial, Community pharmacy | IG: Patient education (education materials were distributed), and education materials were given to prescribers CG: Usual care | 241 | 248 | 6 months | Sedative-hypnotics (benzodiazepine therapy discontinuation) and potentially inappropriate medication | Patient education reduced the number of benzodiazepine users and reduced the number of inappropriate medications among older adults. |
| Falamic et al. [39] (2018) Croatia | Prospective, double-blind, randomized, controlled trial, Community pharmacy | IG: Education and follow-up plan with medication review (given a form containing lab values, INR, and pillbox. CG: Usual GP care | 66 | 65 | 6 months | Time in therapeutic range of warfarin | Patient education improved time in the therapeutic range of warfarin. |
| Outcome | Number of Studies | Number of Participants | Statistical Method | Effect Size 95% (CI) |
|---|---|---|---|---|
| Hospitalization | 3 [31,35,37] | 1986 | Risk ratio (M–H, random, 95% CI) | 0.74 (0.54,1.00) |
| 3 months | 2 [31,35] | 583 | Risk ratio (M–H, random, 95% CI) | 0.62 (0.35,1.11) |
| 6 months | 2 [31,37] | 190 | Risk ratio (M–H, random, 95% CI) | 0.78 (0.50,1.23) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Christopher, C.M.; KC, B.; Blebil, A.; Alex, D.; Ibrahim, M.I.M.; Ismail, N.; Alrasheedy, A.A. Clinical and Humanistic Outcomes of Community Pharmacy-Based Healthcare Interventions Regarding Medication Use in Older Adults: A Systematic Review and Meta-Analysis. Healthcare 2021, 9, 1577. https://doi.org/10.3390/healthcare9111577
Christopher CM, KC B, Blebil A, Alex D, Ibrahim MIM, Ismail N, Alrasheedy AA. Clinical and Humanistic Outcomes of Community Pharmacy-Based Healthcare Interventions Regarding Medication Use in Older Adults: A Systematic Review and Meta-Analysis. Healthcare. 2021; 9(11):1577. https://doi.org/10.3390/healthcare9111577
Chicago/Turabian StyleChristopher, Christina Malini, Bhuvan KC, Ali Blebil, Deepa Alex, Mohamed Izham Mohamed Ibrahim, Norhasimah Ismail, and Alian A. Alrasheedy. 2021. "Clinical and Humanistic Outcomes of Community Pharmacy-Based Healthcare Interventions Regarding Medication Use in Older Adults: A Systematic Review and Meta-Analysis" Healthcare 9, no. 11: 1577. https://doi.org/10.3390/healthcare9111577
APA StyleChristopher, C. M., KC, B., Blebil, A., Alex, D., Ibrahim, M. I. M., Ismail, N., & Alrasheedy, A. A. (2021). Clinical and Humanistic Outcomes of Community Pharmacy-Based Healthcare Interventions Regarding Medication Use in Older Adults: A Systematic Review and Meta-Analysis. Healthcare, 9(11), 1577. https://doi.org/10.3390/healthcare9111577







