The Impact of the COVID-19 Pandemic on Cancer Patient’s Management—Lithuanian Cancer Center Experience
Abstract
:1. Introduction
2. Materials and Methods
Statistics
3. Results
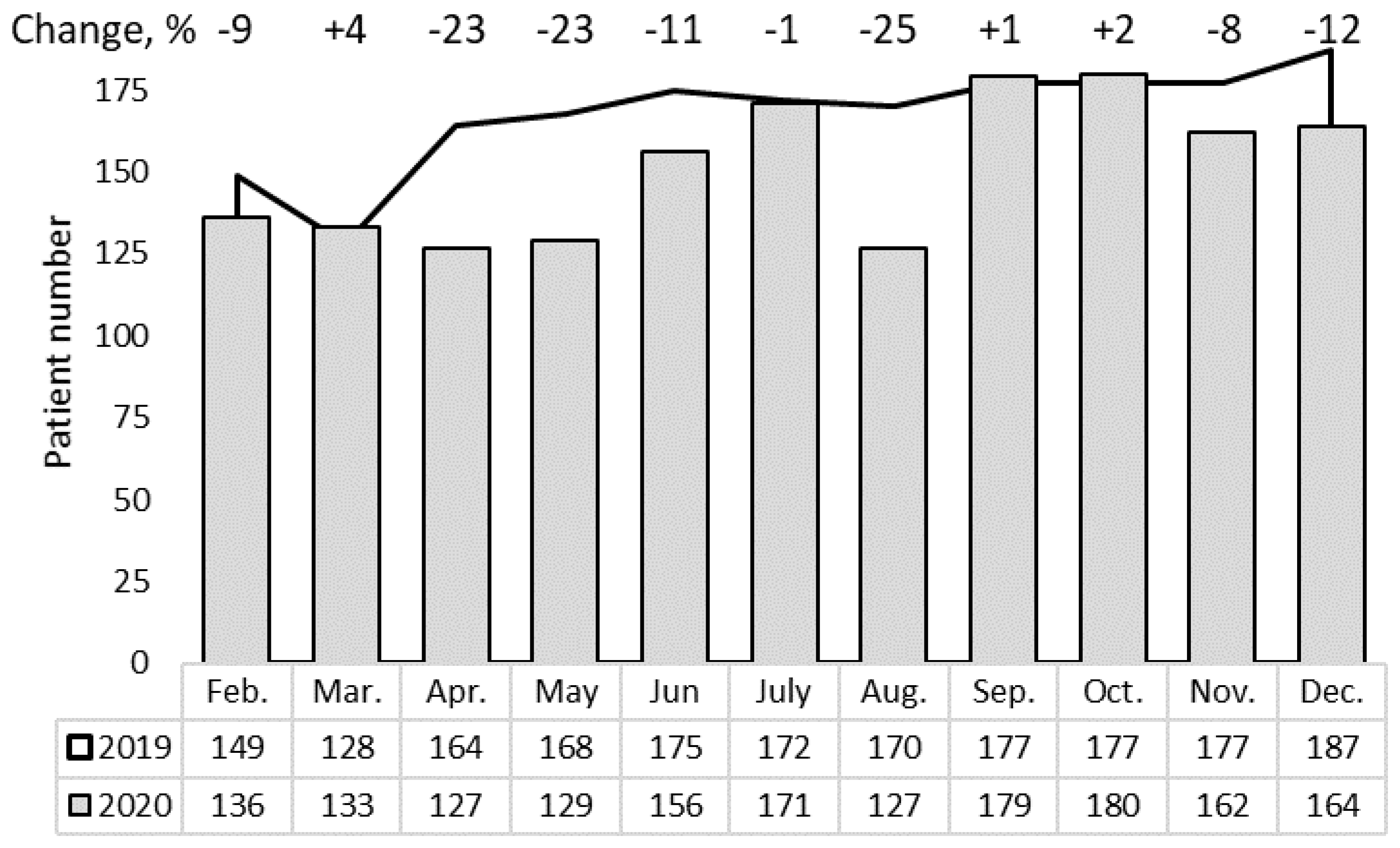
3.1. Out-Patient Cancer Services
3.2. The Services of Systemic Anticancer Therapy and Radiotherapy
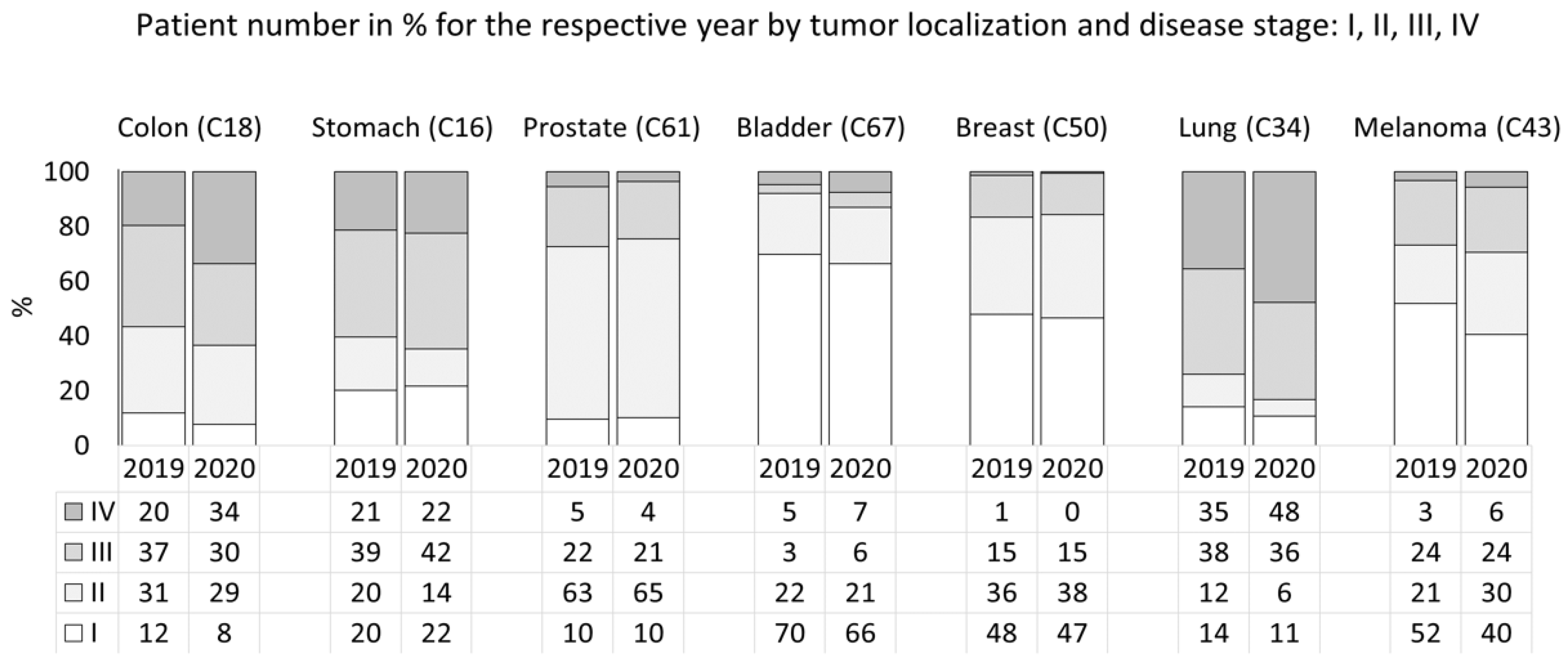
3.3. In-Patient Cancer Services
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Medicare & Medicaid Services. Available online: https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf (accessed on 20 July 2021).
- Freer, P.E. The Impact of the COVID-19 Pandemic on Breast Imaging. Radiol. Clin. North Am. 2021, 59, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Blanco, G.D.V.; Calabrese, E.; Biancone, L.; Monteleone, G.; Paoluzi, O.A. The impact of COVID-19 pandemic in the colorectal cancer prevention. Int. J. Color. Dis. 2020, 35, 1–4. [Google Scholar] [CrossRef]
- ElGohary, G.M.; Hashmi, S.; Styczynski, J.; Kharfan-Dabaja, M.A.; Alblooshi, R.M.; de la Cámara, R.; Mohamed, S.; Alshaibani, A.; Cesaro, S.; El-Aziz, N.A.; et al. The risk and prognosis of COVID-19 infection in cancer patients: A systematic review and meta-analysis. Hematol. Stem Cell Ther. 2020, 30, 1658. [Google Scholar] [CrossRef] [PubMed]
- Kutikov, A.; Weinberg, D.S.; Edelman, M.; Horwitz, E.M.; Uzzo, R.G.; Fisher, R.I. A War on Two Fronts: Cancer Care in the Time of COVID-19. Ann. Intern. Med. 2020, 172, 756–758. [Google Scholar] [CrossRef] [Green Version]
- Wilkinson, E. How cancer services are fighting to counter COVID-19′s impact. BMJ 2020, 370, m2747. [Google Scholar] [CrossRef]
- Hanna, T.P.; King, W.D.; Thibodeau, S.; Jalink, M.; Paulin, G.A.; Harvey-Jones, E.; O’Sullivan, D.E.; Booth, C.M.; Sullivan, R.; Aggarwal, A. Mortality due to cancer treatment delay: Systematic review and meta-analysis. BMJ 2020, 371, m4087. [Google Scholar] [CrossRef]
- Khorana, A.A.; Tullio, K.; Elson, P.; Pennell, N.; Grobmyer, S.R.; Kalady, M.F.; Raymond, D.; Abraham, J.; Klein, E.A.; Walsh, R.M.; et al. Time to initial cancer treatment in the United States and association with survival over time: An observational study. PLoS ONE 2019, 14, e0213209. [Google Scholar] [CrossRef] [Green Version]
- Visit to Physicians in 1998-Health Information Centre, Institute of Hygiene. Available online: https://hi.lt/php/spiv1.php?dat_file=spiv1en.txt (accessed on 30 October 2021).
- Yang, E.A.L.; Chai, P.; Yu, J.; Fan, X. Effects of cancer on patients with COVID-19: A systematic review and meta-analysis of 63,019 participants. Cancer Biol. Med. 2021, 18, 298–307. [Google Scholar] [CrossRef]
- Liang, W.; Guan, W.; Chen, R.; Wang, W.; Li, J.; Xu, K.; Li, C.; Ai, Q.; Lu, W.; Liang, H.; et al. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020, 21, 335–337. [Google Scholar] [CrossRef]
- Curigliano, G.; Banerjee, S.; Cervantes, A.; Garassino, M.C.; Garrido, P.; Girard, N.; Haanen, J.; Jordan, K.; Lordick, F.; Machiels, J.P.; et al. Managing cancer patients during the COVID-19 pandemic: An ESMO multidisciplinary expert consensus. Ann. Oncol. 2020, 31, 1320–1335. [Google Scholar] [CrossRef]
- Coles, C.; Aristei, C.; Bliss, J.; Boersma, L.; Brunt, A.; Chatterjee, S.; Hanna, G.; Jagsi, R.; Person, O.K.; Kirby, A.; et al. International Guidelines on Radiation Therapy for Breast Cancer During the COVID-19 Pandemic. Clin. Oncol. 2020, 32, 279–281. [Google Scholar] [CrossRef] [PubMed]
- Zaorsky, N.G.; Yu, J.B.; McBride, S.M.; Dess, R.T.; Jackson, W.C.; Mahal, B.A.; Chen, R.; Choudhury, A.; Henry, A.; Syndikus, I.; et al. Prostate Cancer Radiotherapy Recommendations in Response to COVID-19. Adv. Radiat. Oncol. 2020, 5, 26–32. [Google Scholar] [CrossRef]
- Guckenberger, M.; Belka, C.; Bezjak, A.; Bradley, J.; Daly, M.E.; DeRuysscher, D.; Dziadziuszko, R.; Faivre-Finn, C.; Flentje, M.; Gore, E.; et al. Practice Recommendations for Lung Cancer Radiotherapy During the COVID-19 Pandemic: An ESTRO-ASTRO Consensus Statement. Int. J. Radiat. Oncol. 2020, 107, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Burki, T.K. Cancer guidelines during the COVID-19 pandemic. Lancet Oncol. 2020, 21, 629–630. [Google Scholar] [CrossRef]
- Patt, D.; Gordan, L.; Diaz, M.; Okon, T.; Grady, L.; Harmison, M.; Markward, N.; Sullivan, M.; Peng, J.; Zhou, A. Impact of COVID-19 on Cancer Care: How the Pandemic Is Delaying Cancer Diagnosis and Treatment for American Seniors. JCO Clin. Cancer Inform. 2020, 4, 1059–1071. [Google Scholar] [CrossRef]
- Blay, J.; Boucher, S.; Le Vu, B.; Cropet, C.; Chabaud, S.; Perol, D.; Barranger, E.; Campone, M.; Conroy, T.; Coutant, C.; et al. Delayed care for patients with newly diagnosed cancer due to COVID-19 and estimated impact on cancer mortality in France. ESMO Open 2021, 6, 100134. [Google Scholar] [CrossRef]
- Whitaker, K.L.; Scott, S.E.; Winstanley, K.; MacLeod, U.; Wardle, J. Attributions of Cancer ‘Alarm’ Symptoms in a Community Sample. PLoS ONE 2014, 9, e114028. [Google Scholar] [CrossRef] [Green Version]
- Maringe, C.; Spicer, J.; Morris, M.; Purushotham, A.; Nolte, E.; Sullivan, R.; Rachet, B.; Aggarwal, A. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: A national, population-based, modelling study. Lancet Oncol. 2020, 21, 1023–1034. [Google Scholar] [CrossRef]
- Limb, M. COVID-19: Early stage cancer diagnoses fell by third in first lockdown. BMJ 2021, 373, n1179. [Google Scholar] [CrossRef]
- Minami, C.A.; Kantor, O.; Weiss, A.; Nakhlis, F.; King, T.A.; Mittendorf, E.A. Association Between Time to Operation and Pathologic Stage in Ductal Carcinoma in Situ and Early-Stage Hormone Receptor-Positive Breast Cancer. J. Am. Coll. Surg. 2020, 231, 434–447.e2. [Google Scholar] [CrossRef]
- Dee, E.C.; Mahal, B.A.; Arega, M.A.; D’Amico, A.V.; Mouw, K.W.; Nguyen, P.L.; Muralidhar, V. Relative Timing of Radiotherapy and Androgen Deprivation for Prostate Cancer and Implications for Treatment During the COVID-19 Pandemic. JAMA Oncol. 2020, 6, 1630–1632. [Google Scholar] [CrossRef] [PubMed]
- O’Hea, E.; Kroll-Desrosiers, A.; Cutillo, A.S.; Michalak, H.R.; Barton, B.A.; Harralson, T.; Carmack, C.; McMahon, C.; Boudreaux, E.D. Impact of the mental health and dynamic referral for oncology (MHADRO) program on oncology patient outcomes, health care utilization, and health provider behaviors: A multi-site randomized control trial. Patient Educ. Couns. 2019, 103, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Bäuerle, A.; Musche, V.; Schmidt, K.; Schweda, A.; Fink, M.; Weismüller, B.; Kohler, H.; Herrmann, K.; Tewes, M.; Schadendorf, D.; et al. Mental Health Burden of German Cancer Patients before and after the Outbreak of COVID-19: Predictors of Mental Health Impairment. Int. J. Environ. Res. Public Health 2021, 18, 2318. [Google Scholar] [CrossRef] [PubMed]

| Services | 2019, (N) | 2020 (N) | Change, (%) |
|---|---|---|---|
| Medical consultations | 110. 510 | 94. 709 | −14 |
| Mental health (psychological and psychiatric services) | 537 | 597 | 11 |
| Systemic anticancer therapy | 21.623 | 22.502 | 4 |
| Radiation therapy | 31.854 | 29.542 | −7 |
| Radiology (inc. Rx, MRI, CT, US *) | 108.473 | 90.981 | −16 |
| Day surgery | 6403 | 4827 | −25 |
| Endoscopic procedures | 2627 | 1853 | −29 |
| Disease follow-up visits | 16.894 | 14.205 | −16 |
| Preventive programs: | |||
| Mammography | 9704 | 3653 | −62 |
| Prostate cancer | 259 | 112 | −57 |
| Colonoscopy | 780 | 587 | −25 |
| Solid Tumors | SACT | Radiotherapy/Brachytherapy | ||||
|---|---|---|---|---|---|---|
| The Number of Patients | Changes, % | The Number of Patients | Changes, (%) | |||
| 2019 | 2020 | 2019 | 2020 | |||
| Head-and neck (C00–C14, C30–C32 *) | 276 | 292 | 6 | 74 | 67 | _ |
| Digestive system (C15–C21, C22–C25) | 2478 | 582 | −77 | 95 | 91 | _ |
| Respiratory system (C33–C39) | 186 | 223 | 20 | 87 | 94 | _ |
| Melanoma and non-melanoma skin (C43, C44) | 56 | 49 | _ | 33 | 25 | _ |
| Breast (C50) | 1025 | 1414 | 38 | 405 | 418 | 3 |
| Gynecological (C51–C56) | 574 | 498 | −13 | 242 | 184 | -24 |
| Prostate (C61) | 264 | 342 | 30 | 195 | 181 | -7 |
| Summary | 4859 | 3400 | −30 | 1131 | 1060 | -6 |
| Solid Tumors | Year | Stage | Summary | Change, % | |||||
|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | p-Value for ch2 | p-Value for rsANOVA | ||||
| Colon (C18 *) | 2019 | 15 | 40 | 47 | 25 | 0.099 | 0.32 | 127 | −18 |
| 2020 | 8 | 30 | 31 | 35 | 104 | ||||
| Stomach (C16) | 2019 | 36 | 35 | 70 | 38 | 0.56 | 0.046 | 179 | −18 |
| 2020 | 32 | 20 | 62 | 33 | 147 | ||||
| Prostate (C61) | 2019 | 36 | 234 | 82 | 20 | 0.67 | >0.99 | 372 | 3 |
| 2020 | 39 | 250 | 80 | 14 | 383 | ||||
| Bladder (C67) | 2019 | 88 | 28 | 4 | 6 | 0.64 | >0.99 | 126 | −15 |
| 2020 | 71 | 22 | 6 | 8 | 107 | ||||
| Kidney (C64) | 2019 | 37 | 1 | 34 | 7 | 0.52 | 0.56 | 79 | _ |
| 2020 | 40 | 1 | 26 | 3 | 70 | ||||
| Breast (C50) | 2019 | 313 | 233 | 99 | 9 | 0.38 | 0.046 | 654 | −8 |
| 2020 | 281 | 229 | 91 | 3 | 604 | ||||
| Lung (C34) | 2019 | 33 | 28 | 90 | 83 | 0.053 | 0.046 | 234 | −36 |
| 2020 | 16 | 9 | 53 | 71 | 149 | ||||
| Thyroid (C73) | 2019 | 16 | 4 | 1 | 2 | 0.45 | 0.56 | 23 | _ |
| 2020 | 22 | 1 | 1 | 3 | 27 | ||||
| Melanoma (C43) | 2019 | 66 | 27 | 30 | 4 | 0.20 | 0.56 | 127 | −1 |
| 2020 | 51 | 38 | 30 | 7 | 126 | ||||
| Larynx (C32) | 2019 | 3 | 7 | 25 | 25 | 0.24 | >0.99 | 60 | _ |
| 2020 | 7 | 6 | 17 | 33 | 63 | ||||
| Summary | 2019 | 643 | 637 | 482 | 219 | 0.36 | 0.046 | 1981 | −10 |
| 2020 | 567 | 606 | 397 | 210 | 1780 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dabkeviciene, D.; Vincerzevskiene, I.; Urbonas, V.; Venius, J.; Dulskas, A.; Brasiuniene, B.; Janulionis, E.; Burneckis, A.; Zileviciene, A.; Tiskevicius, S.; et al. The Impact of the COVID-19 Pandemic on Cancer Patient’s Management—Lithuanian Cancer Center Experience. Healthcare 2021, 9, 1522. https://doi.org/10.3390/healthcare9111522
Dabkeviciene D, Vincerzevskiene I, Urbonas V, Venius J, Dulskas A, Brasiuniene B, Janulionis E, Burneckis A, Zileviciene A, Tiskevicius S, et al. The Impact of the COVID-19 Pandemic on Cancer Patient’s Management—Lithuanian Cancer Center Experience. Healthcare. 2021; 9(11):1522. https://doi.org/10.3390/healthcare9111522
Chicago/Turabian StyleDabkeviciene, Daiva, Ieva Vincerzevskiene, Vincas Urbonas, Jonas Venius, Audrius Dulskas, Birute Brasiuniene, Ernestas Janulionis, Arvydas Burneckis, Asta Zileviciene, Sigitas Tiskevicius, and et al. 2021. "The Impact of the COVID-19 Pandemic on Cancer Patient’s Management—Lithuanian Cancer Center Experience" Healthcare 9, no. 11: 1522. https://doi.org/10.3390/healthcare9111522
APA StyleDabkeviciene, D., Vincerzevskiene, I., Urbonas, V., Venius, J., Dulskas, A., Brasiuniene, B., Janulionis, E., Burneckis, A., Zileviciene, A., Tiskevicius, S., Vanseviciute-Petkeviciene, R., Usinskiene, J., Briediene, R., Bulotiene, G., Stratilatovas, E., Ostapenko, V., Gibaviciene, J., Karnas, I., Kekstaite, S., ... Jarmalaite, S. (2021). The Impact of the COVID-19 Pandemic on Cancer Patient’s Management—Lithuanian Cancer Center Experience. Healthcare, 9(11), 1522. https://doi.org/10.3390/healthcare9111522






