New Rehabilitation Assessment Method of the End-Effector Finger Rehabilitation Robot Based on Multi-Sensor Source
Abstract
:1. Introduction
2. Materials and Methods
2.1. Mechanism Design of EFRR
2.2. Function Composition of EFRR
3. Results
3.1. Muscle Strength Assessment Based on Fingertip Pressure
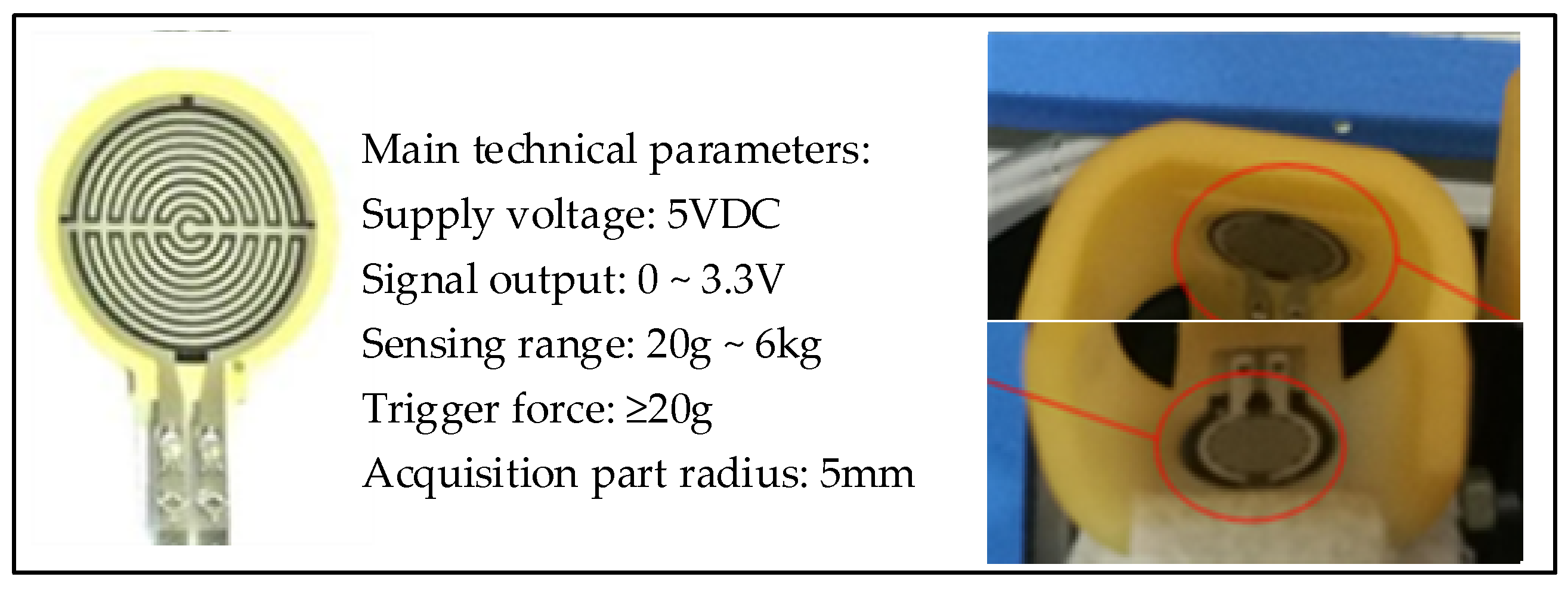
3.1.1. Pressure Detection of the Fingertip
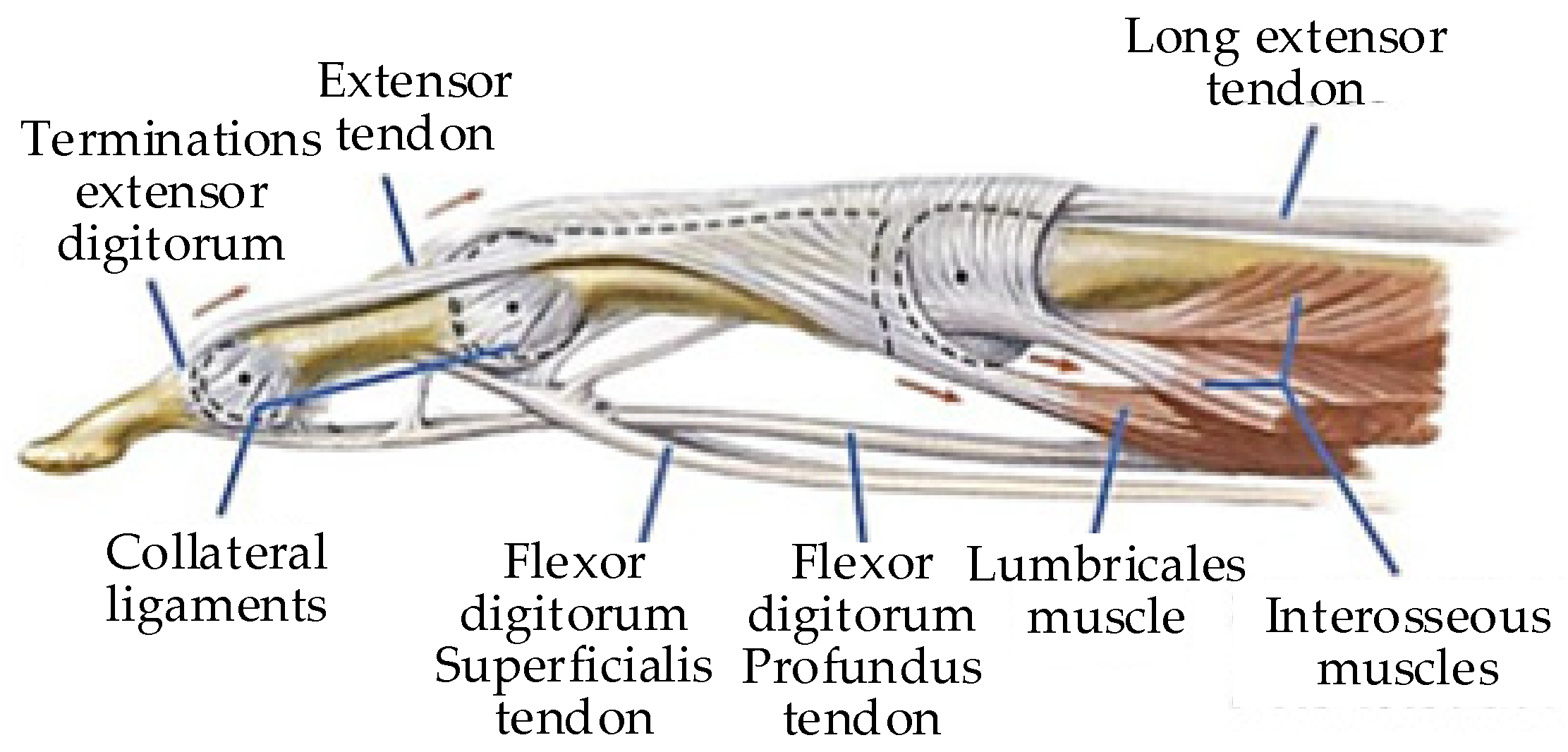
3.1.2. The Calculation of Finger Muscle Strength
3.1.3. Finger Strength Analysis
3.2. Fatigue Assessment Based on sEMG Signal
3.2.1. sEMG Signal Acquisition
3.2.2. Data Processing
3.2.3. Fatigue Degree Analysis
3.3. Assessment of Range of Motion Based on Motor Encoder
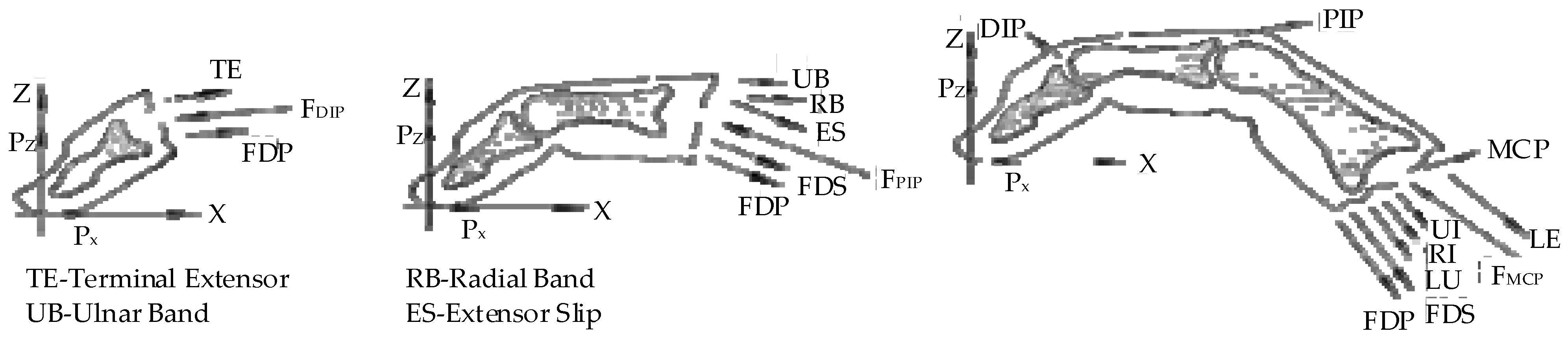
3.3.1. Human–Machine Motion Coupling Model
3.3.2. ROM Analysis
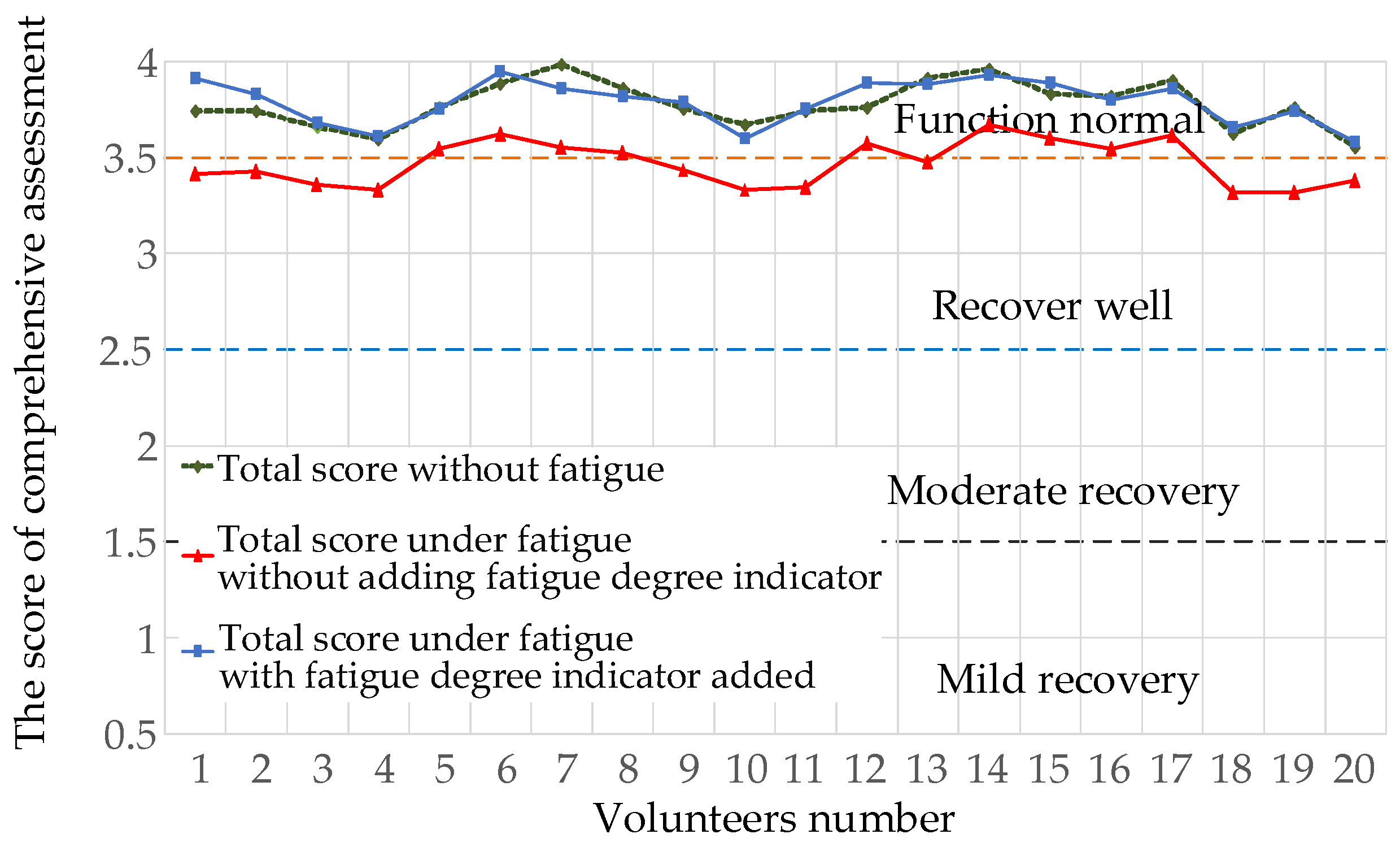
3.4. Comprehensive Assessment of Finger Rehabilitation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ji, S.R. Rehabilitation Medicine; Higher Education Press: Beijing, China, 2004; pp. 16–62. [Google Scholar]
- Sun, C.C.; Wang, C.F.; Ding, X.J. Effect of Upper Limb Rehabilitation Robot Assisted Training on Upper Limb Motor Function of Stroke Patients with Hemiplegia. Chin. J. Rehabil. Med. 2018, 33, 1162–1167. [Google Scholar]
- Xu, G.C.; Li, L.L. Assessment of Motion Function after Stroke. Clin. Rehabil. China 2002, 6, 1233–1235. [Google Scholar]
- Zhang, J.C. Development Process, Connotation and Theoretical Basis of Rehabilitation Engineering and Assistive Technology. Chin. Rehabil. Theory Pract. 2011, 17, 581–582. [Google Scholar]
- Wang, L.; Zhang, X.F.; Ma, Y. Review of Upper Limb Rehabilitation Robots and Assessment Methods for Stroke Patients. Beijing Biomed. Eng. 2015, 34, 526–532. [Google Scholar]
- Chang, W.H.; Kim, Y. Robot-Assisted Therapy in Stroke Rehabilitation. J. Stroke 2013, 15, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.H.; Zhang, C.; Ji, W. Rehabilitation Assessment Method of Upper Limb Rehabilitation Robot Based on AHP Fuzzy Comprehensive Assessment. J. Shenyang Univ. 2012, 13, 47–51. [Google Scholar]
- Mazzoleni, S.; Duret, C.; Grosmaire, A.G. Combining Upper Limb Robotic Rehabilitation with Other Therapeutic Approaches after Stroke: Current Status, Rationale, and Challenges. BioMed Res. Int. 2017, 2017, 8905637. [Google Scholar] [CrossRef]
- Mi, C.; Chen, Y.; Zou, L. Research on Muscle Fatigue Detection System Based on sEMG. Mod. Electron. 2018, 41, 86–90. [Google Scholar]
- Rong, J.F.; Ding, L.; Zhang, W. Effect of Rehabilitation Robot Combined with Mirror Therapy on Upper Limb Function of Stroke Patients with Hemiplegia. Chin. Rehabil. Theory Pract. 2019, 25, 709–713. [Google Scholar]
- Balasubramanian, S.; Colombo, R.; Sterpi, I. Robotic Assessment of Upper Limb Motion Function after Stroke. Am. J. Phys. Med. Rehabil. 2012, 91, S255–S269. [Google Scholar] [CrossRef] [PubMed]
- Hwang, C.H.; Seong, J.W.; Son, D. Individual Finger Synchronized Robot-Assisted Hand Rehabilitation in Subacute to Chronic Stroke: A Prospective Randomized Clinical Trial of Efficacy. Clin. Rehabil. 2012, 26, 696–704. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, S.; Klein, J.; Burdet, E. Robot-Assisted Rehabilitation of Hand Function. Curr. Opin. Neurol. 2010, 23, 661–670. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.Z.; Yu, H.L.; Fu, F.F.; Tang, X.P.; Zheng, L.D. Design of Robot Training and Rehabilitation Assessment System for Upper Limb Rehabilitation Training. Softw. Guide 2017, 16, 83–86. [Google Scholar]
- Cai, H.M. Design of an Upper Limb Rehabilitation Robotic Training and Evaluation System. Master’s Thesis, Tianjin University of Technology, Tianjin, China, 2021. [Google Scholar]
- Wu, Z.F. Stroke Assessment and Thinking Based on Artificial Neural Network in Tactile Virtual Environment. Master’s Thesis, East China University of Technology, Shanghai, China, 2016. [Google Scholar]
- Kurillo, G.; Chen, A.; Bajcsy, R. Assessment of Upper Extremity Reachable Workspace Using Kinect Camera. Technol. Health Care 2013, 21, 641–656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bai, J. Research on Key Technologies and Rehabilitation Assessment of Upper Limb Rehabilitation Robot. Master’s Thesis, Southeast University, Nanjing, China, 2019. [Google Scholar]
- Gao, B.F.; Wei, C.; Ma, H.D. Real-Time Evaluation of the Signal Processing of sEMG Used in Limb Exoskeleton Rehabilitation System. Appl. Bionics Biomech. 2018, 2018, 1391032. [Google Scholar] [CrossRef]
- Su, C.Q. Design of Upper Limb Rehabilitation Assessment System Based on sEMG-Inertia Information. Master’s Thesis, Yanshan University, Qinhuangdao, China, 2017. [Google Scholar]
- Alessandro, S.; Franco, M. Low-Cost Tracking Systems Allow Fine Biomechanical Evaluation of Upper-Limb Daily-Life Gestures in Healthy People and Post-Stroke Patients. Sensors 2019, 19, 1224. [Google Scholar] [CrossRef] [Green Version]
- Wang, Q.H.; Wei, Y.K.; Liu, L.M. Research and Application Progress of Rehabilitation Robot. Packag. Eng. 2018, 39, 95–101. [Google Scholar]
- Li, Y.Q.; Zeng, Q.; Huang, G.Z. Clinical Application Progress of Upper Limb Rehabilitation Robot in Stroke. Chin. Rehabil. Theory Pract. 2020, 26, 310–314. [Google Scholar]
- Yi, R.W. Design of Network Oriented Finger Rehabilitation Training and Assessment System. Master’s Thesis, Southeast University, Nanjing, China, 2016. [Google Scholar]
- Zhang, N.; Niu, B.S.; Wang, H.B.; Chen, F.; Yan, H.; Jin, Z.N. Structure and Control System Design of ADRC Finger Rehabilitation Robot. Sci. Technol. Eng. 2019, 19, 166–173. [Google Scholar]
- Gao, F.; Damsgaard, M.; Rasmussen, J.; Christensen, S.T. Computational Method for Muscle-Path Representation in Musculoskeletal Models. Biol. Cybern. 2002, 87, 199–210. [Google Scholar] [CrossRef]
- Yang, W.Z. Research on the Generation of Real Power Sense in Virtual Hand Interaction. Master’s Thesis, Zhejiang University, Hangzhou, China, 2007. [Google Scholar]
- Eyler, D.L.; Markee, J.E. The Anatomy and Function of the Intrinsic Musculature of the Fingers. J. Bone Jt. Surg. 1954, 36, 1–9. [Google Scholar] [CrossRef]
- Bullock, I.M.; Júlia, B.S.; Dollar, A.M. Assessing Assumptions in Kinematic Hand Models: A Review. In Proceedings of the 2012 4th IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), Rome, Italy, 24–27 June 2012; pp. 139–164. [Google Scholar]
- Zhang, L.L. Biomechanical Modeling of Human Upper Limb and Biomechanical Study of Typical Sports. Master’s Thesis, Shanghai Jiaotong University, Shanghai, China, 2009. [Google Scholar]
- Ueki, S.; Kawasaki, H.; Ito, S.; Nishimoto, Y.; Abe, M.; Aoki, T.; Ishigure, Y.; Ojika, T.; Mouri, T. Development of a Hand-Assist Robot with Multi-Degrees-of-Freedom for Rehabilitation Therapy. IEEE/ASME Trans. Mechatron. 2012, 17, 136–146. [Google Scholar] [CrossRef]
- Hu, D. Biomechanical Modeling of Driver’s Hand Skeletal Muscle. Master’s Thesis, Jilin University, Chang Chun, China, 2014. [Google Scholar]
- Wei, G.F. Study on Overall Biomechanical Modeling and Simulation Analysis of Human Bone and Muscle System. Master’s Thesis, Shanghai Jiaotong University, Shanghai, China, 2010. [Google Scholar]
- Fang, Z.; Lv, J.; Fang, L.; Xu, S.X.; Fang, M. Biomechanical Modeling and Analysis of Hand Force of Traditional Chinese Medicine Massage and Health Method. Prog. Biomed. Eng. 2010, 31, 191–194. [Google Scholar]
- Geng, H.Y. Biomechanical Modeling and Simulation of Human Skeletal Muscle. Master’s Thesis, Harbin University of Technology, Harbin, China, 2019. [Google Scholar]
- Yan, Z.X. Human Upper Limb Movement Recognition and Muscle Fatigue Detection Based on sEMG Signal. Master’s Thesis, Beijing University of Technology, Beijing, China, 2018. [Google Scholar]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of Recommendations for sEMG Sensors and Sensor Placement Procedures. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Leonardis, D.; Barsotti, M.; Loconsole, C.; Solazzi, M.; Troncossi, M.; Mazzotti, C.; Castelli, V.P.; Procopio, C.; Lamola, G.; Chisari, C.; et al. An EMG-Controlled Robotic Hand Exoskeleton for Bilateral Rehabilitation. IEEE Trans. Haptics 2015, 8, 140–151. [Google Scholar] [CrossRef]
- Ren, L.Y.; Shao, Z.M.; Xu, D.L. Time Frequency Domain Feature Extraction of Human sEMG Signal. J. Chang. Univ. 2019, 29, 10–12. [Google Scholar]
- Niu, B.S. Mechanical Structure and Control System Design of Finger Rehabilitation Robot. Master’s Thesis, Yanshan University, Qinhuangdao, China, 2020. [Google Scholar]
- Zhong, Y. Randomized Controlled Study on Clinical Pathway of Early Rehabilitation of Ischemic Stroke. Electron. J. Clin. Med. Lit. 2018, 5, 85–86. [Google Scholar]

















| Muscle Group | FDP | FDS | LE | LU | UI | RI |
|---|---|---|---|---|---|---|
| PCSA | 10.67 | 8.89 | 4.15 | 0.52 | 1.45 | 4.30 |
| Muscle Group | FDP | FDS | LE | INT |
|---|---|---|---|---|
| Muscle strength |
| ROM | ||||
|---|---|---|---|---|
| Score | 1 | 2 | 3 | 4 |
| Weight | ||||
|---|---|---|---|---|
| 1 | 1.93 | 3.15 | 0.55 | |
| 0.52 | 1 | 1.66 | 0.28 | |
| 0.32 | 0.6 | 1 | 0.17 |
| ROM | Muscle Strength | Fatigue Degree | Weight | |
|---|---|---|---|---|
| ROM | 1 | 1.44 | 0.23 | 0.45 |
| Muscle strength | 1.44 | 1 | 0.16 | 0.46 |
| Fatigue degree | 5 | 6.33 | 1 | 0.09 |
| The Score of Comprehensive Assessment | ||||
|---|---|---|---|---|
| Degree | Mild recovery | Moderate recovery | Good recovery | Normal function |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Chen, P.; Li, Y.; Sun, B.; Liao, Z.; Niu, B.; Niu, J. New Rehabilitation Assessment Method of the End-Effector Finger Rehabilitation Robot Based on Multi-Sensor Source. Healthcare 2021, 9, 1251. https://doi.org/10.3390/healthcare9101251
Wang H, Chen P, Li Y, Sun B, Liao Z, Niu B, Niu J. New Rehabilitation Assessment Method of the End-Effector Finger Rehabilitation Robot Based on Multi-Sensor Source. Healthcare. 2021; 9(10):1251. https://doi.org/10.3390/healthcare9101251
Chicago/Turabian StyleWang, Hongbo, Peng Chen, Yungui Li, Bowen Sun, Ziyu Liao, Baoshan Niu, and Jianye Niu. 2021. "New Rehabilitation Assessment Method of the End-Effector Finger Rehabilitation Robot Based on Multi-Sensor Source" Healthcare 9, no. 10: 1251. https://doi.org/10.3390/healthcare9101251
APA StyleWang, H., Chen, P., Li, Y., Sun, B., Liao, Z., Niu, B., & Niu, J. (2021). New Rehabilitation Assessment Method of the End-Effector Finger Rehabilitation Robot Based on Multi-Sensor Source. Healthcare, 9(10), 1251. https://doi.org/10.3390/healthcare9101251







