Effect of the Abdominal Draw-In Maneuver and Bracing on Abdominal Muscle Thickness and the Associated Subjective Difficulty in Healthy Individuals
Abstract
1. Introduction
2. Materials and Methods
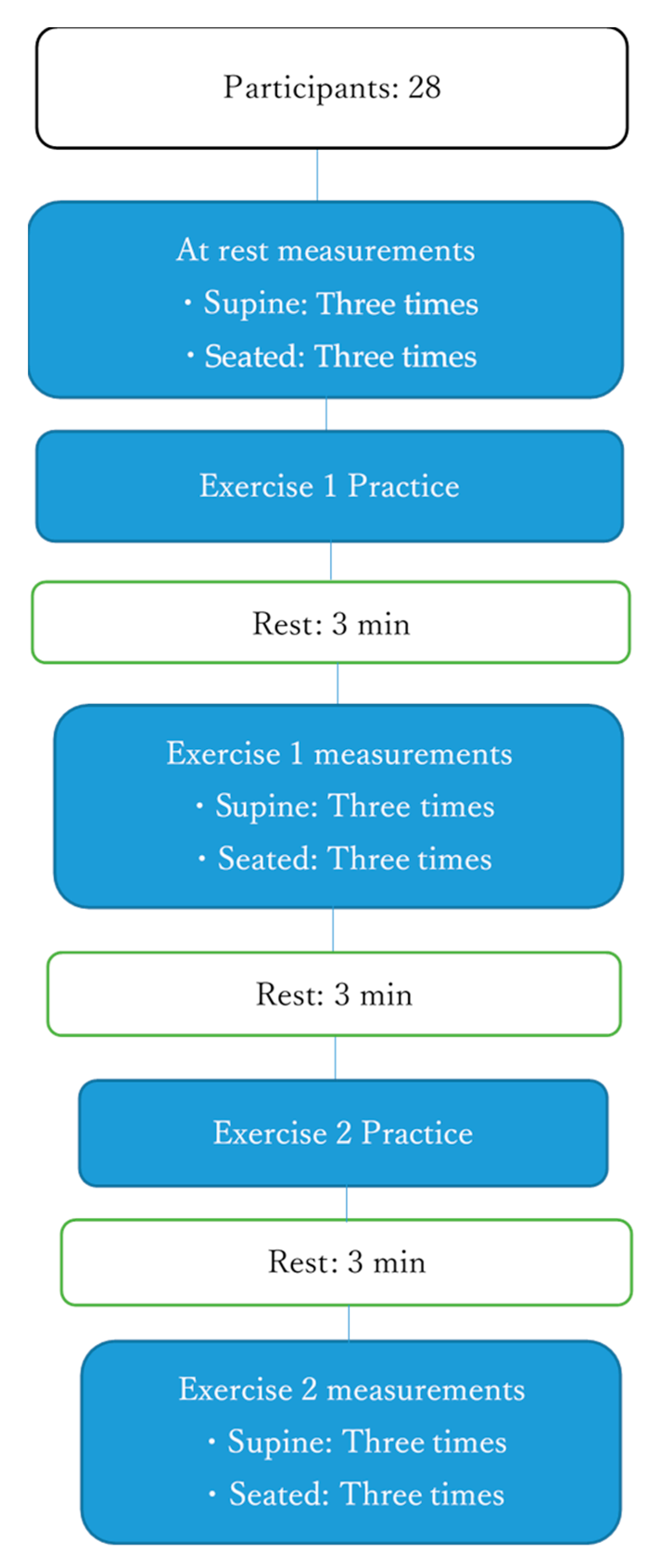
2.1. Study Design
2.2. Study Participants
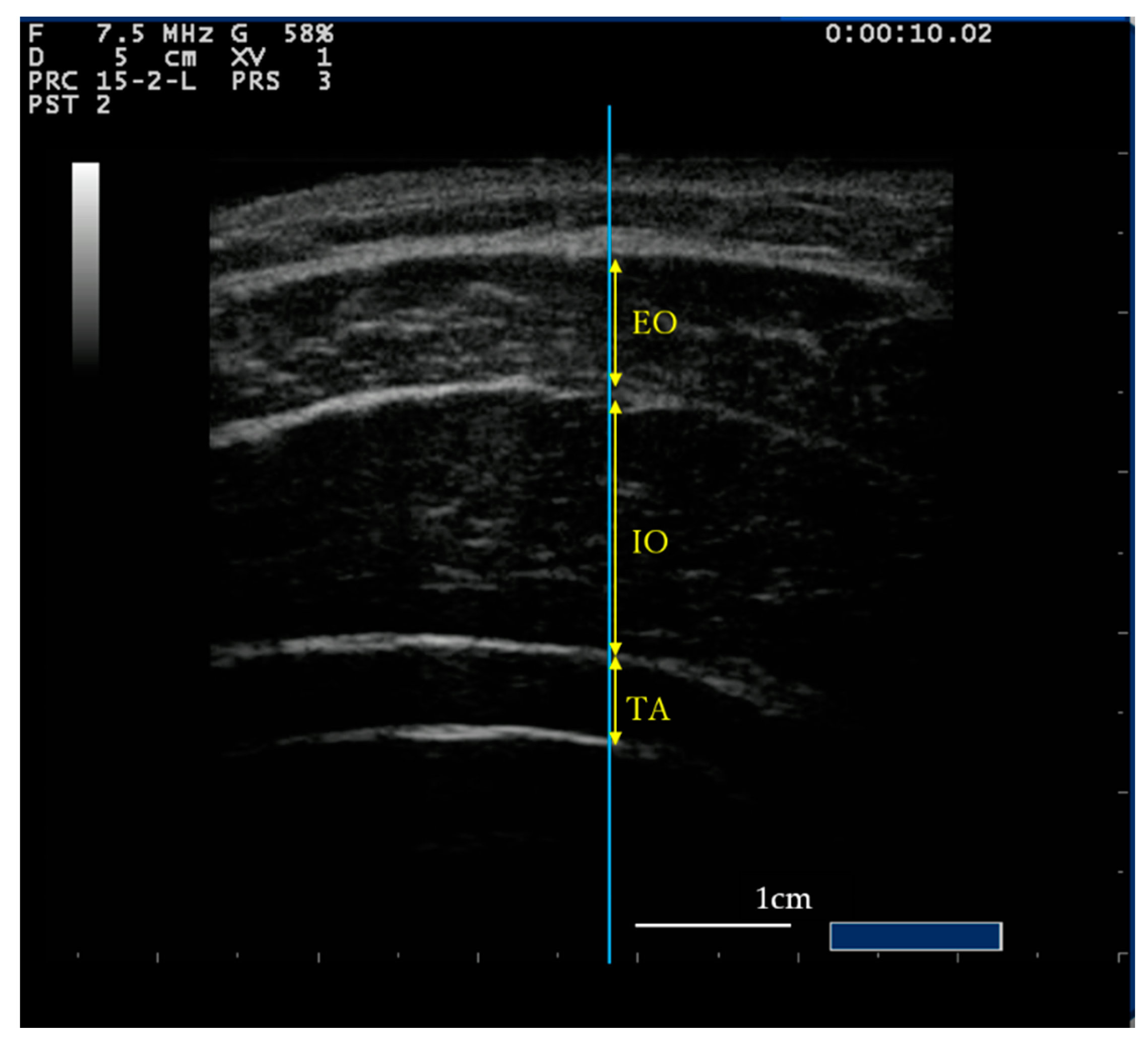
2.3. Measurement Procedure
2.4. Statistical Analysis
3. Results
3.1. Subjective Difficulty of Exercises
3.2. Intraclass Correlation Coefficients
3.3. Lateral Abdominal Muscle Thickness
3.4. Correlation of Subjective Difficulty and Muscle Thickness
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Richardson, C.; Jull, G. Muscle control–pain control. What exercises would you prescribe? Man. Ther. 1995, 1, 2–10. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, P. Masterclass. Lumbar segmental ‘instability’: Clinical presentation and specific stabilizing exercise management. Man. Ther. 2000, 5, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Gomes-Neto, M.; Lopes, J.M.; Conceição, C.S.; Araujo, A.; Brasileiro, A.; Sousa, C.; Carvalho, V.O.; Arcanjo, F.L. Stabilization exercise compared to general exercises or manual therapy for the management of low back pain: A systematic review and meta-analysis. Phys. Ther. Sport 2017, 23, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Searle, A.; Spink, M.; Ho, A.; Chuter, V. Exercise interventions for the treatment of chronic low back pain: A systematic review and meta-analysis of randomised controlled trials. Clin. Rehabil. 2015, 29, 1155–1167. [Google Scholar] [CrossRef] [PubMed]
- Richardson, C.A.; Jull, G.A.; Hides, J.; Hodges, P. Therapeutic Exercise for Spinal Segmental Stabilization in Low Back Pain; Churchill Livingstone: New York, NY, USA, 1999. [Google Scholar]
- Teyhen, D.S.; Bluemle, L.N.; Dolbeer, J.A.; Baker, S.E.; Molloy, J.M.; Whittaker, J.; Childs, J.D. Changes in Lateral Abdominal Muscle Thickness During the Abdominal Drawing-in Maneuver in Those With Lumbopelvic Pain. J. Orthop. Sports Phys. Ther. 2009, 39, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Hosseinifar, M.; Akbari, M.; Behtash, H.; Amiri, M.; Sarrafzadeh, J. The Effects of Stabilization and Mckenzie Exercises on Transverse Abdominis and Multifidus Muscle Thickness, Pain, and Disability: A Randomized Controlled Trial in NonSpecific Chronic Low Back Pain. J. Phys. Ther. Sci. 2013, 25, 1541–1545. [Google Scholar] [CrossRef] [PubMed]
- Ota, M.; Kaneoka, K.; Hangai, M.; Koizumi, K.; Murematsu, T. The effectiveness of lunbar stabilization exercise for chronic low back pain-thickness and asymmetry of abdominal muscles. J. Jpn. Soc. Clin. Sports Med. 2012, 20, 72–78. [Google Scholar]
- Gorbet, N.; Selkow, N.M.; Hart, J.M.; Saliba, S.A. No Difference in Transverse Abdominis Activation Ratio between Healthy and Asymptomatic Low Back Pain Patients during Therapeutic Exercise. Rehabil. Res. Pr. 2010, 2010, 1–6. [Google Scholar] [CrossRef]
- Kato, S.; Murakami, H.; Inaki, A.; Mochizuki, T.; Demura, S.; Nakase, J.; Yoshioka, K.; Yokogawa, N.; Igarashi, T.; Takahashi, N.; et al. Innovative exercise device for the abdominal trunk muscles: An early validation study. PLoS ONE 2017, 12, e0172934. [Google Scholar] [CrossRef]
- Grenier, S.G.; McGill, S.M. Quantification of Lumbar Stability by Using 2 Different Abdominal Activation Strategies. Arch. Phys. Med. Rehabil. 2007, 88, 54–62. [Google Scholar] [CrossRef]
- Tayashiki, K.; Takai, Y.; Maeo, S.; Kanehisa, H. Intra-abdominal Pressure and Trunk Muscular Activities during Abdominal Bracing and Hollowing. Int. J. Sports Med. 2015, 37, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Peek, K.; Sanson-Fisher, R.; MacKenzie, L.J.; Carey, M. Patient adherence to physiotherapist prescribed self-management strategies: A critical review. Int. J. Ther. Rehabil. 2015, 22, 535–543. [Google Scholar] [CrossRef]
- Saner, J.; Bergman, E.M.; De Bie, R.; Sieben, J.M. Low back pain patients’ perspectives on long-term adherence to home-based exercise programmes in physiotherapy. Musculoskelet. Sci. Pr. 2018, 38, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Beinart, N.; Goodchild, C.E.; Weinman, J.A.; Ayis, S.; Godfrey, E.L. Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: A systematic review. Spine J. 2013, 13, 1940–1950. [Google Scholar] [CrossRef]
- Escolar-Reina, P.; Medina-Mirapeix, F.; Gascón-Cánovas, J.J.; Montilla-Herrador, J.; Jimeno-Serrano, F.J.; Sousa, S.L.D.O.; Del Baño-Aledo, M.E.; Lomas-Vega, R. How do care-provider and home exercise program characteristics affect patient adherence in chronic neck and back pain: A qualitative study. BMC Health Serv. Res. 2010, 10, 60. [Google Scholar] [CrossRef]
- Jack, K.; McLean, S.; Moffett, J.K.; Gardiner, E. Barriers to treatment adherence in physiotherapy outpatient clinics: A systematic review. Man. Ther. 2010, 15, 220–228. [Google Scholar] [CrossRef]
- Slade, S.C.; Molloy, E.K.; Keating, J.L. ‘Listen to me, tell me’: A qualitative study of partnership in care for people with non-specific chronic low back pain. Clin. Rehabil. 2009, 23, 270–280. [Google Scholar] [CrossRef]
- Slade, S.C.; Patel, S.; Underwood, M.; Keating, J.L. What Are Patient Beliefs and Perceptions About Exercise for Nonspecific Chronic Low Back Pain? Clin. J. Pain 2014, 30, 995–1005. [Google Scholar] [CrossRef]
- Palazzo, C.; Klinger, E.; Dorner, V.; Kadri, A.; Thierry, O.; Boumenir, Y.; Martin, W.; Poiraudeau, S.; Ville, I. Barriers to home-based exercise program adherence with chronic low back pain: Patient expectations regarding new technologies. Ann. Phys. Rehabil. Med. 2016, 59, 107–113. [Google Scholar] [CrossRef]
- McMeeken, J.; Beith, I.; Newham, D.; Milligan, P.; Critchley, D.J. The relationship between EMG and change in thickness of transversus abdominis. Clin. Biomech. 2004, 19, 337–342. [Google Scholar] [CrossRef]
- Hodges, P.W.; Pengel, L.; Herbert, R.; Gandevia, S. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve 2003, 27, 682–692. [Google Scholar] [CrossRef]
- Hides, J.; Wilson, S.; Stanton, W.; McMahon, S.; Keto, H.; McMahon, K.; Bryant, M.; Richardson, C. An MRI Investigation into the Function of the Transversus Abdominis Muscle During “Drawing-In” of the Abdominal Wall. Spine 2006, 31, E175–E178. [Google Scholar] [CrossRef] [PubMed]
- Koppenhaver, S.L.; Hebert, J.J.; Parent, E.C.; Fritz, J.M. Rehabilitative ultrasound imaging is a valid measure of trunk muscle size and activation during most isometric sub-maximal contractions: A systematic review. Aust. J. Physiother. 2009, 55, 153–169. [Google Scholar] [CrossRef]
- Dooley, I.J.; O’Brien, P.D. Subjective difficulth of each stage of phacoemulsification cataract surgery performed by basic surgical trainees. J. Cataract. Refract. Surg. 2006, 33, 604–608. [Google Scholar] [CrossRef] [PubMed]
- Sakai, C.; Shimizu, T. Treatment focusing on subjective difficulty improved step-down movement; A case of trisomy 18. Phys. Ther. Hyogo 2019, 25, 45–48. [Google Scholar]
- Nagata, C.; Ido, M.; Shimizu, H.; Misao, A.; Matsuura, H. Choice of Response Scale for Health Measurement: Comparison of 4, 5, and 7-point Scales and Visual Analog Scale. J. Epidemiol. 1996, 6, 192–197. [Google Scholar] [CrossRef]
- Teyhen, D.S.; Miltenberger, C.E.; Deiters, H.M.; Del Toro, Y.M.; Pulliam, J.N.; Childs, J.D.; Boyles, R.E.; Flynn, T. The Use of Ultrasound Imaging of the Abdominal Drawing-in Maneuver in Subjects with Low Back Pain. J. Orthop. Sports Phys. Ther. 2005, 35, 346–355. [Google Scholar] [CrossRef]
- Springer, B.A.; Mielcarek, B.J.; Nesfield, T.K.; Teyhen, D.S. Relationships among Lateral Abdominal Muscles, Gender, Body Mass Index, and Hand Dominance. J. Orthop. Sports Phys. Ther. 2006, 36, 289–297. [Google Scholar] [CrossRef]
- Rankin, G.; Stokes, M.; Newham, D.J. Abdominal muscle size and symmetry in normal subjects. Muscle Nerve 2006, 34, 320–326. [Google Scholar] [CrossRef]
- Aboufazeli, M.; Afshar-Mohajer, N. Within-day and between-day reliability of thickness measurements of abdominal muscles using ultrasound during abdominal hollowing and bracing maneuvers. J. Bodyw. Mov. Ther. 2018, 22, 122–128. [Google Scholar] [CrossRef]
- Koh, H.-W.; Cho, S.-H.; Kim, C.-Y. Comparison of the Effects of Hollowing and Bracing Exercises on Cross-sectional Areas of Abdominal Muscles in Middle-aged Women. J. Phys. Ther. Sci. 2014, 26, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Tayashiki, K.; Maeo, S.; Usui, S.; Miyamoto, N.; Kanehisa, H. Effect of abdominal bracing training on strength and power of trunk and lower limb muscles. Graefe’s Arch. Clin. Exp. Ophthalmol. 2016, 116, 1703–1713. [Google Scholar] [CrossRef] [PubMed]
- Maeo, S.; Takahashi, T.; Takai, Y.; Kanehisa, H. Trunk Muscle Activities During Abdominal Bracing: Comparison Among Muscles and Exercises. J. Sports Sci. Med. 2013, 12, 467–474. [Google Scholar] [PubMed]
- Storheim, K.; Holm, I.; Gunderson, R.; Brox, J.I.; Bø, K. The Effect of Comprehensive Group Training on Cross-sectional Area, Density, and Strength of Paraspinal Muscles in Patients Sick-Listed for Subacute Low Back Pain. J. Spinal Disord. Tech. 2003, 16, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Tsao, H.; Hodges, P.W. Immediate changes in feedforward postural adjustments following voluntary motor training. Exp. Brain Res. 2007, 181, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kim, Y.; Oh, S.; Suh, D.; Eun, S.-D.; Yoon, B. Abdominal hollowing and bracing strategies increase joint stability in the trunk region during sudden support surface translation but not in the lower extremities. J. Back Musculoskelet. Rehabil. 2016, 29, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kim, M.; Oh, S.; Yoon, B. The Effectiveness of Hollowing and Bracing Strategies with Lumbar Stabilization Exercise in Older Adult Women With Nonspecific Low Back Pain: A Quasi-Experimental Study on a Community-based Rehabilitation. J. Manip. Physiol. Ther. 2018, 41, 1–9. [Google Scholar] [CrossRef]
- Nakao, T.; Tsujita, J.; Yamashita, Y.; Masuda, K.; Kanai, S.; Hirakawa, K. Influences on motor function caused by the lower trunk muscular contraction. J. Jpn. Soc. Physiol. Anthropol. 2005, 20, 135–145. [Google Scholar]
- Tayanaka, M. Approaches to trunk dysfunction: Voiding problems. J. Clin. Phys. Ther. 2009, 12, 1–6. [Google Scholar]
- Reeve, A.; Dilley, A. Effects of posture on the thickness of transversus abdominis in pain-free subjects. Man. Ther. 2009, 14, 679–684. [Google Scholar] [CrossRef]
- O’Sullivan, P.B.; Dankaerts, W.; Burnett, A.F.; Farrell, G.T.; Jefford, E.; Naylor, C.S.; O’Sullivan, K.J. Effect of Different Upright Sitting Postures on Spinal-Pelvic Curvature and Trunk Muscle Activation in a Pain-Free Population. Spine 2006, 31, E707–E712. [Google Scholar] [CrossRef] [PubMed]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Different Ways to Balance the Spine. Spine 2009, 34, E208–E214. [Google Scholar] [CrossRef] [PubMed]
| Posture | Supine | Sitting | ||
|---|---|---|---|---|
| ADIM | AB | ADIM | AB | |
| Difficulty | 2.0 ± 1.0 | 3.26 ± 0.9 *,† | 2.15 ± 0.91 | 3.19 ± 0.83 *,† |
| Posture | Supine | Sitting | ||||
|---|---|---|---|---|---|---|
| Muscle | Rest | ADIM | AB | Rest | ADIM | AB |
| TA | 0.95 (0.90–0.98) | 0.95 (0.91–0.98) | 0.96 (0.93–0.98) | 0.94 (0.89–0.97) | 0.96 (0.93–0.98) | 0.87 (0.75–0.93) |
| IO | 0.98 (0.96–0.99) | 0.91 (0.84–0.96) | 0.94 (0.89–0.97) | 0.97 (0.94–0.98) | 0.97 (0.95–0.98) | 0.96 (0.93–0.98) |
| EO | 0.97 (0.95–0.99) | 0.88 (0.78–0.94) | 0.95 (0.91–0.98) | 0.95 (0.91–0.98) | 0.90 (0.80–0.95) | 0.92 (0.85–0.96) |
| Posture | Supine | Sitting | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Rest | ADIM | AB | Comparison | p | Rest | ADIM | AB | Comparison | p | |
| TA | 4.0 ± 0.8 | 6.9 ± 1.7 | 4.9 ± 2.0 | Rest-ADIM | <0.01 | 4.3 ± 1.3 | 6.7 ± 2.4 | 4.7 ± 1.8 | Rest-ADIM | <0.01 |
| Rest-AB | 0.14 | Rest-AB | 1.00 | |||||||
| ADIM-AB | <0.01 | ADIM-AB | <0.01 | |||||||
| IO | 10.1 ± 1.9 | 12.1 ± 2.5 | 10.5 ± 2.6 | Rest-ADIM | <0.01 | 10.9 ± 3.0 | 15.0 ± 3.6 | 11.8 ± 4.2 | Rest-ADIM | <0.01 |
| Rest-AB | 1.00 | Rest-AB | 0.96 | |||||||
| ADIM-AB | 0.03 | ADIM-AB | <0.01 | |||||||
| EO | 7.0 ± 1.3 | 7.8 ± 1.4 | 6.9 ± 1.6 | Rest-ADIM | 0.12 | 7.3 ± 1.4 | 7.5 ± 1.2 | 7.4 ± 1.4 | Rest-ADIM | 1.00 |
| Rest-AB | 1.00 | Rest-AB | 1.00 | |||||||
| ADIM-AB | 0.04 | ADIM-AB | 1.00 | |||||||
| Muscle | Exercise | Supine | Sitting | p |
|---|---|---|---|---|
| TA | Rest | 4.0 ± 0.8 | 4.3 ± 1.3 | 0.08 |
| ADIM | 6.9 ± 1.7 | 6.7 ± 2.4 | 0.78 | |
| AB | 4.9 ± 2.0 | 4.7 ± 1.8 | 0.52 | |
| IO | Rest | 10.1 ± 1.9 | 10.9 ± 3.0 | 0.06 |
| ADIM | 12.1 ± 2.5 | 15.0 ± 3.6 | <0.01 | |
| AB | 10.5 ± 2.6 | 11.8 ± 4.2 | 0.02 | |
| EO | Rest | 7.0 ± 1.3 | 7.3 ± 1.4 | 0.13 |
| ADIM | 7.8 ± 1.4 | 7.5 ± 1.2 | 0.19 | |
| AB | 6.9 ± 1.6 | 7.4 ± 1.4 | 0.02 |
| Posture | Supine | Sitting | |||
|---|---|---|---|---|---|
| All (p) | ADIM (p) | AB (p) | ADIM (p) | AB (p) | |
| TA | −0.400 (<0.01) | −0.373 (0.05) | −0.223 (0.25) | −0.051 (0.80) | −0.275 (0.16) |
| IO | −0.284 (<0.01) | −0.054 (0.79) | −0.050 (0.80) | −0.078 (0.69) | −0.313 (0.11) |
| EO | −0.110 (0.25) | 0.39 (0.84) | −0.050 (0.80) | −0.51 (0.80) | −0.126 (0.52) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Madokoro, S.; Yokogawa, M.; Miaki, H. Effect of the Abdominal Draw-In Maneuver and Bracing on Abdominal Muscle Thickness and the Associated Subjective Difficulty in Healthy Individuals. Healthcare 2020, 8, 496. https://doi.org/10.3390/healthcare8040496
Madokoro S, Yokogawa M, Miaki H. Effect of the Abdominal Draw-In Maneuver and Bracing on Abdominal Muscle Thickness and the Associated Subjective Difficulty in Healthy Individuals. Healthcare. 2020; 8(4):496. https://doi.org/10.3390/healthcare8040496
Chicago/Turabian StyleMadokoro, Sachiko, Masami Yokogawa, and Hiroichi Miaki. 2020. "Effect of the Abdominal Draw-In Maneuver and Bracing on Abdominal Muscle Thickness and the Associated Subjective Difficulty in Healthy Individuals" Healthcare 8, no. 4: 496. https://doi.org/10.3390/healthcare8040496
APA StyleMadokoro, S., Yokogawa, M., & Miaki, H. (2020). Effect of the Abdominal Draw-In Maneuver and Bracing on Abdominal Muscle Thickness and the Associated Subjective Difficulty in Healthy Individuals. Healthcare, 8(4), 496. https://doi.org/10.3390/healthcare8040496




