Orthodontic Treatment and Healthcare Goals: Evaluation of Multibrackets Treatment Results Using PAR Index (Peer Assessment Rating)
Abstract
1. Introduction
- (1)
- To evaluate the quality of the orthodontic treatment performed by students of a postgraduate orthodontic program, using the weighted PAR.
- (2)
- To determine whether the outcome of treatment (in terms of change in PAR) is related to the following factors: gender, treatment technique, dental extractions.
2. Material and Methods
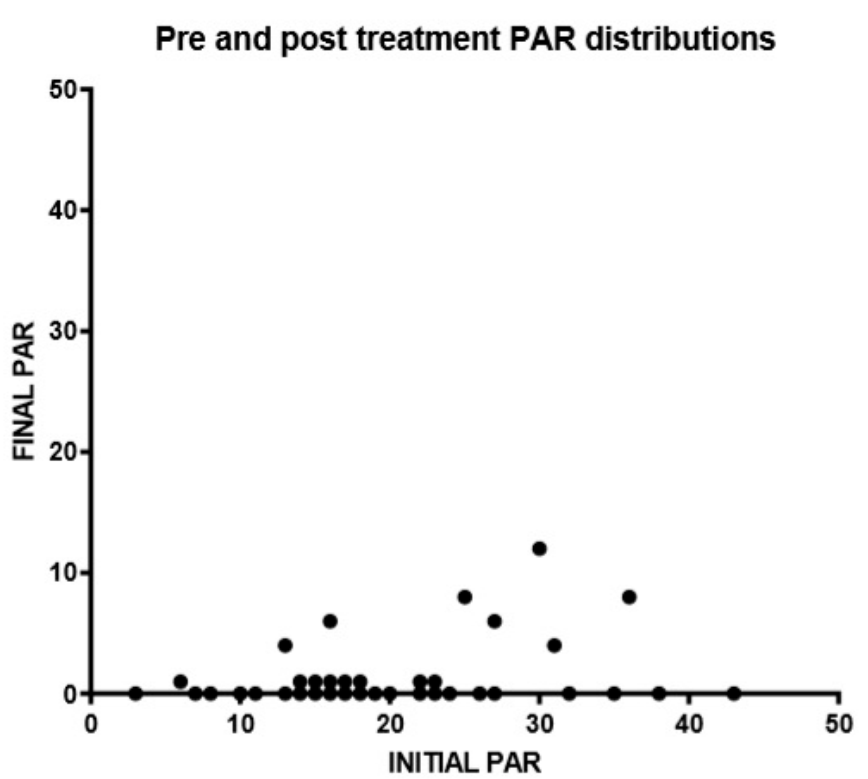
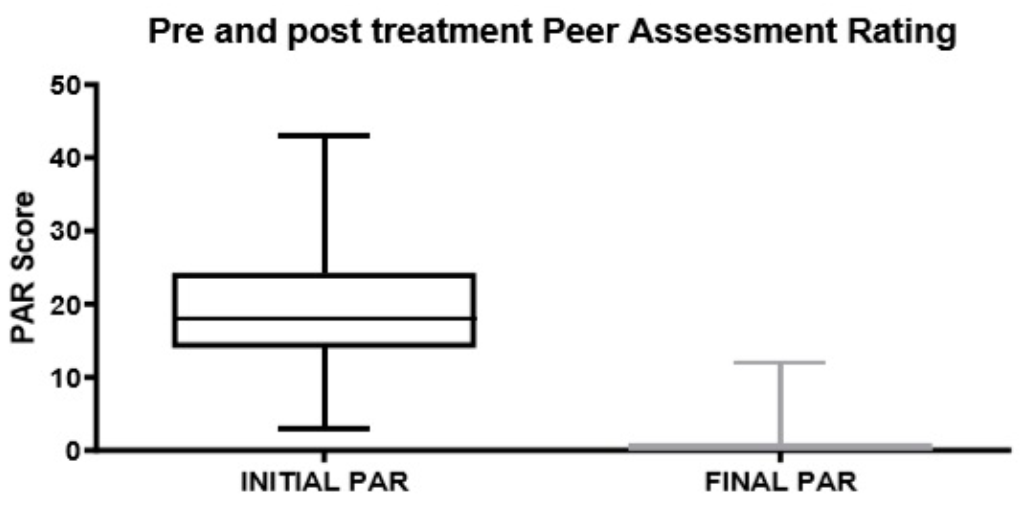
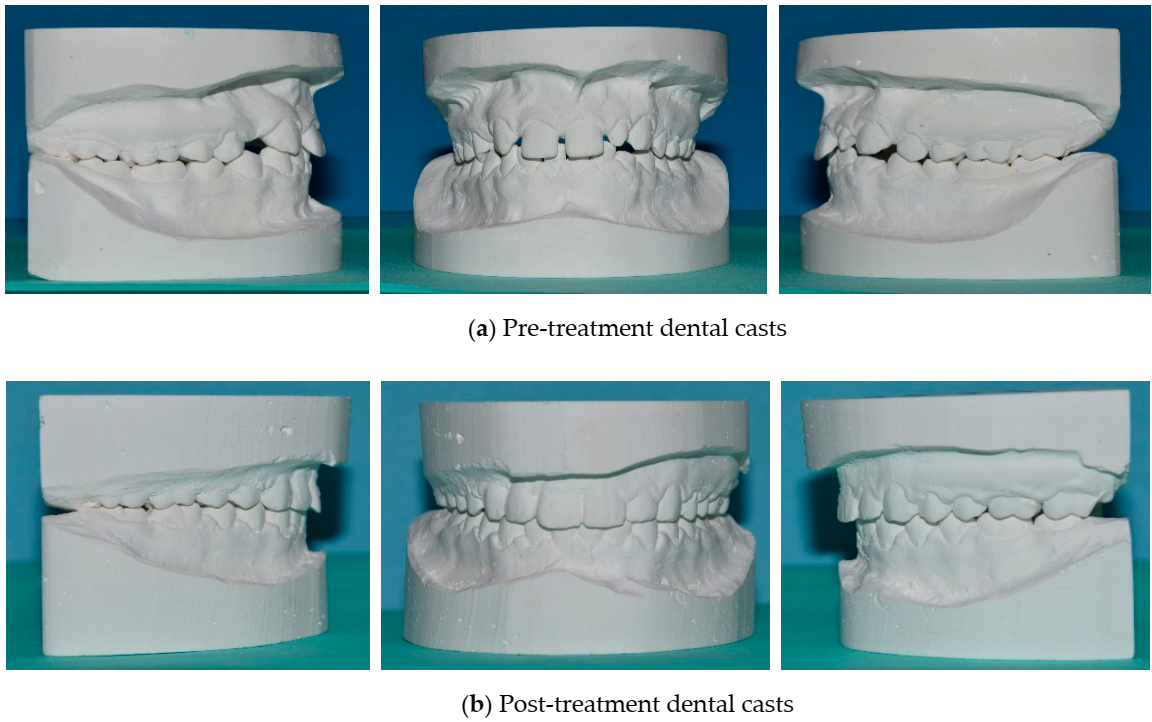
3. Results
- Worsening or no difference: 0% of patients.
- Improvement: 8% of patients.
- Great improvement: 92% of patients.
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Data Availability Statement
References
- Dyken, R.A.; Sadowsky, P.L.; Hurst, D. Orthodontic outcomes assessment using the peer assessment rating index. Angle Orthod. 2001, 71, 164–169. [Google Scholar] [PubMed]
- Richmond, S.; Shaw, W.C.; O’Brien, K.D.; Buchanan, I.B.; Jones, R.; Stephens, C.D.; Roberts, C.T.; Andrews, M. The development of the PAR Index (Peer Assessment Rating): Reliability and validity. Eur. J. Orthod. 1992, 14, 125–139. [Google Scholar] [CrossRef] [PubMed]
- Onyeaso, C.O.; BeGole, E.A. Associations between pretreatment age and treatment time with orthodontic treatment outcome: A comparison by means of two orthodontic indices. Hell Orthod. Rev. 2008, 11, 9–20. [Google Scholar]
- Hickman, J.H. Directional edgewise orthodontic approach. J. Clin. Orthod. 1975, 9, 143–154. [Google Scholar]
- Firestone, A.R.; Häsler, R.U.; Ingervall, B. Treatment results in dental school orthodontic patients in 1983 and 1993. Angle Orthod. 1999, 69, 19–26. [Google Scholar]
- Cook, D.R.; Harris, E.F.; Vaden, J.L. Comparison of university and private- practice orthodontic treatment outcomes with the American Board of Orthodontics objective grading system. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 707–712. [Google Scholar] [CrossRef]
- Ramanathan, C. PAR index in the evaluation of the stability of the orthodontic treatment results. A Review. Acta Med. 2006, 49, 203–207. [Google Scholar] [CrossRef][Green Version]
- Pangrazio-Kulbersh, V.; Kaczynski, R.; Shunock, M. Early treatment outcome assessed by the Peer Assessment Rating index. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 544–550. [Google Scholar] [CrossRef]
- Templeton, K.M.; Powell, R.; Moore, M.B.; Williams, A.C.; Sandy, R. Are the Peer Assessment Rating Index and the Index of Treatment Complexity, Outcome, and Need suitable measures for orthognathic outcomes? Eur. J. Orthod. 2006, 28, 462–466. [Google Scholar] [CrossRef]
- Gonzales-Gil-de-Bernabé, P.; Bellot-Arcis, C.; Montiel-Company, J.M.; Gandia-Franco, J.L. Evaluation of treament outcomes in a 3 years post-graduate orthodontic program using the peer assessment rating (par). J. Clin. Exp. Dent. 2014, 6, 364–368. [Google Scholar] [CrossRef]
- Richmond, S.; Shaw, W.C.; Roberts, C.T.; Andrews, M. The PAR Index (Peer Assessment Rating): Methods to determine outcome of orthodontic treatment in terms of improvement and standards. Eur. J. Orthod. 1992, 14, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Bernas, A.J.; Banting, D.W.; Short, L.L. Effectiveness of phase I orthodontic treatment in an undergraduate teaching clinic. J. Dent. Educ. 2007, 71, 1179–1186. [Google Scholar] [CrossRef] [PubMed]
- Campbell, C.L.; Roberts, W.E.; Hartsfield, J.K., Jr.; Qi, R. Treatment outcomes in a graduate orthodontic clinic for cases defined by the American Board of Orthodontics malocclusion categories. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 822–829. [Google Scholar] [CrossRef] [PubMed]
- Yang-Powers, L.C.; Sadowsky, C.; Rosenstein, S.; BeGole, E.A. Treatment outcome in a graduate orthodontic clinic using the American Board of Orthodontics grading system. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Pinskaya, Y.B.; Hsieh, T.J.; Roberts, W.E.; Hartsfield, J.K. Comprehensive clinical evaluation as an outcome assessment for a graduate orthodontics program. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 533–543. [Google Scholar] [CrossRef]
- Onyeaso, C.O.; Begole, E.A. Orthodontic Treatment—Improvement and Standards using the Peer Assessment Rating Index. Angle Orthod. 2006, 76, 260–264. [Google Scholar]
- Egolf, R.J.; BeGole, E.A.; Upshaw, H.S. Factors associated with orthodontic patient compliance with intraoral elastic and headgear wear. Am. J. Orthod. Dentofac. Orthop. 1990, 97, 336–348. [Google Scholar] [CrossRef]
- Ngan, P.; Kess, B.; Wilson, S. Perception of discomfort by patients undergoing orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1989, 96, 47–53. [Google Scholar] [CrossRef]
- Sergl, H.G.; Klages, U.; Zentner, A. Pain and discomfort during orthodontic treatment: Causative factors and effects on compliance. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 684–691. [Google Scholar] [CrossRef]
- Blanck-Lubarsch, M.; Hohoff, A.; Wiechmann, D.; Stamm, T. Orthodontic treatment of children/adolescents with special health care needs: An analysis of treatment lenght and clinical outcomes. BMC Oral Health 2014, 14, 67. [Google Scholar] [CrossRef]
- Vu, C.Q.; Roberts, W.E.; Hartsfield, J.K., Jr.; Ofner, S. Treatment complexity index for assessing the relationship of treatment duration and outcomes in a graduate orthodontics clinic. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.N.; Kulbersh, R.; Kaczynski, R. Clinical outcomes assessment of consecutively finished patients in a 24-month orthodontic residency: A 5-year perspective. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 665–668. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Gandini, P.; Castroflorio, T.; Garino, F.; Mergati, L.; D’Anca, K.; Trovati, F.; Scribante, A. Buccolingual Inclination Control of Upper Central Incisors of Aligners: A Comparison with Conventional and Self-Ligating Brackets. Biomed Res. Int. 2018, 2018, 9341821. [Google Scholar] [CrossRef] [PubMed]
- Holman, J.K.; Hans, M.G.; Nelson, S.; Powers, M.P. An assessment of extraction versus nonextraction orthodontic treatment using the peer assessment rating (PAR) index. Angle Orthod. 1998, 68, 527–534. [Google Scholar] [PubMed]
- Beckwith, F.R.; Ackerman, R.J., Jr.; Cobb, C.M.; Tira, D.E. An evaluation of factors affecting duration of orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 439–447. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Debiaggi, M.; Zara, F.; Brerra, R.; Comelli, M.; Bianchi, M.; Pollone, S.R.; Scribante, A. Influence of lingual bracket position on microbial and periodontal parameters in vivo. J. Appl. Oral Sci. 2012, 20, 357–361. [Google Scholar] [CrossRef]
- Tervonen, M.M.; Pirttiniemi, P.; Lahti, S. Development of a measure for orthodontists to evaluate patient compliance. Am. J. Orthod. Dentofacial. Orthop. 2011, 139, 791–796. [Google Scholar] [CrossRef]
- Karasiunok, A.Y.; Smahliuk, L.V. The role of parents in motivation for orthodontic treatment for children. Wiad. Lek. 2018, 71, 529–533. [Google Scholar]
- Scribante, A.; Contreras-Bulnes, R.; Montasser, M.A.; Vallittu, P.K. Orthodontics: Bracket Materials, Adhesives Systems, and Their Bond Strength. Biomed Res. Int. 2016, 2016, 1329814. [Google Scholar] [CrossRef]
- Willems, G.; Heidbüchel, R.; Verdonck, A.; Carels, C. Treatment and standard evaluation using the Peer Assessment Rating Index. Clin. Oral Investig. 2001, 5, 57–62. [Google Scholar] [CrossRef]
- Al Yami, E.A.; Kuijpers-Jagtman, A.M.; Van’t Hof, M.A. Occlusal outcome of orthodontic treatment. Angle Orthod. 1998, 68, 439–444. [Google Scholar] [PubMed]
- Barenghi, L.; Barenghi, A.; Cadeo, C.; Di Blasio, A. Innovation by Computer-Aided Design/Computer-Aided Manufacturing Technology: A Look at Infection Prevention in Dental Settings. Biomed Res. Int. 2019, 2019, 6092018. [Google Scholar] [CrossRef] [PubMed]
- Hosseinzadeh Nik, T.; Gholamrezaei, E.; Keshvad, M.A. Facial asymmetry correction: From conventional orthognathic treatment to surgery-first approach. J. Dent. Res. Dent. Clin. Dent. Prospects. 2019, 13, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Sfondrini, M.F.; Gatti, S.; Gandini, P. Disinclusion of unerupted teeth by mean of self-ligating brackets: Effect of blood contamination on shear bond strength. Med. Oral Patol. Oral Cir. Bucal 2013, 18, e162–e167. [Google Scholar] [CrossRef] [PubMed]
- Lorente, C.; Lorente, P.; Perez-Vela, M.; Esquinas, C.; Lorente, T. Orthodontic management of a complete and an incomplete maxillary canine-first premolar transposition. Angle Orthod. 2019. [CrossRef]
- Sfondrini, M.F.; Gandini, P.; Malfatto, M.; Di Corato, F.; Trovati, F.; Scribante, A. Computerized Casts for Orthodontic Purpose Using Powder-Free Intraoral Scanners: Accuracy, Execution Time, and Patient Feedback. Biomed Res. Int. 2018, 2018, 4103232. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, M.; Briguglio, F.; Grassia, V.; Picciolo, G.; Fiorillo, L.; Matarese, G. Effectiveness of Low-Level Laser Therapy during Tooth Movement: A Randomized Clinical Trial. Materials 2019, 12, 2187. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Gandini, P.; Alcozer, R.; Vallittu, P.K.; Scribante, A. Failure load and stress analysis of orthodontic miniscrews with different transmucosal collar diameter. J. Mech. Behav. Biomed. Mater. 2018, 87, 132–137. [Google Scholar] [CrossRef]
- Sha, H.N.; Choi, S.H.; Yu, H.S.; Hwang, C.J.; Cha, J.Y.; Kim, K.M. Debonding force and shear bond strength of an array of CAD/CAM-based customized orthodontic brackets, placed by indirect bonding- An In Vitro study. PLoS ONE 2018, 13, e0202952. [Google Scholar] [CrossRef]







| Initial PAR Mean (CI 95%) | Final PAR Mean (CI 95%) | Change in PAR Score Mean (CI 95%) | Mann–Whitney U Test (p Value) | Change in PAR % Mean (CI 95%) | Mann–Whitney U Test (p Value) | ||
|---|---|---|---|---|---|---|---|
| Gender | Male (n = 28) | 21.29 (18.06–24.52) | 1.36 (0.27–2.45) | 19.93 (16.71–23.15) | p = 0.4691 | 94.13 (89.77–98.49) | p = 0.6599 |
| Female (n = 22) | 18.09 (14.92–21.26) | 0.86 (0.03–1.69) | 17.23 (14.38–20.08) | 95.64 (92.04–99.24) | |||
| Technique | Straight wire (n = 43) | 19.44 (17.08–21.80) | 1.05 (0.31–1.79) | 18.40 (16.128–20.68) | p = 0.2481 | 95.18 (92.18–98.18) | p = 0.9656 |
| Self ligating (n = 7) | 24.43 (16.84–32.02) | 1.71 (−0.62–4.05) | 22.71 (15.33–30.09) | 92.43 (82.68–102.18) | |||
| Extractions | Yes (n = 5) | 26.60 (18.53–34.67) | 2.40 (−0.74–5.54) | 24.20 (17.93–30.47) | p = 0.0989 | 92.98 (84.06–101.89) | p = 0.5680 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sfondrini, M.F.; Zampetti, P.; Luscher, G.; Gandini, P.; Gandía-Franco, J.L.; Scribante, A. Orthodontic Treatment and Healthcare Goals: Evaluation of Multibrackets Treatment Results Using PAR Index (Peer Assessment Rating). Healthcare 2020, 8, 473. https://doi.org/10.3390/healthcare8040473
Sfondrini MF, Zampetti P, Luscher G, Gandini P, Gandía-Franco JL, Scribante A. Orthodontic Treatment and Healthcare Goals: Evaluation of Multibrackets Treatment Results Using PAR Index (Peer Assessment Rating). Healthcare. 2020; 8(4):473. https://doi.org/10.3390/healthcare8040473
Chicago/Turabian StyleSfondrini, Maria Francesca, Paolo Zampetti, Giulia Luscher, Paola Gandini, José Luís Gandía-Franco, and Andrea Scribante. 2020. "Orthodontic Treatment and Healthcare Goals: Evaluation of Multibrackets Treatment Results Using PAR Index (Peer Assessment Rating)" Healthcare 8, no. 4: 473. https://doi.org/10.3390/healthcare8040473
APA StyleSfondrini, M. F., Zampetti, P., Luscher, G., Gandini, P., Gandía-Franco, J. L., & Scribante, A. (2020). Orthodontic Treatment and Healthcare Goals: Evaluation of Multibrackets Treatment Results Using PAR Index (Peer Assessment Rating). Healthcare, 8(4), 473. https://doi.org/10.3390/healthcare8040473








