Developing an Innovative Medical Training Simulation Device for Peripheral Venous Access: A User-Centered Design Approach
Abstract
1. Introduction
2. Materials and Methods
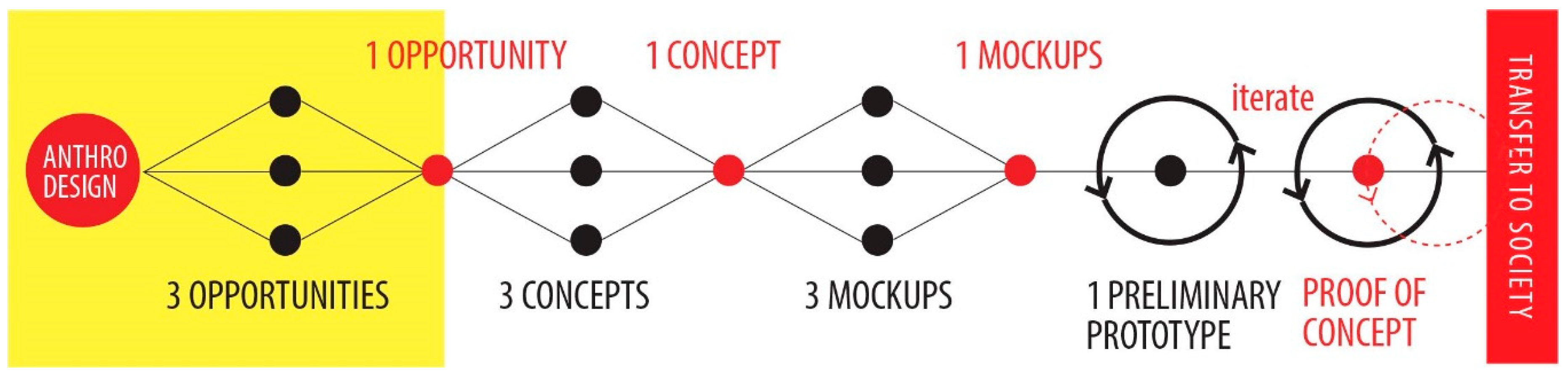
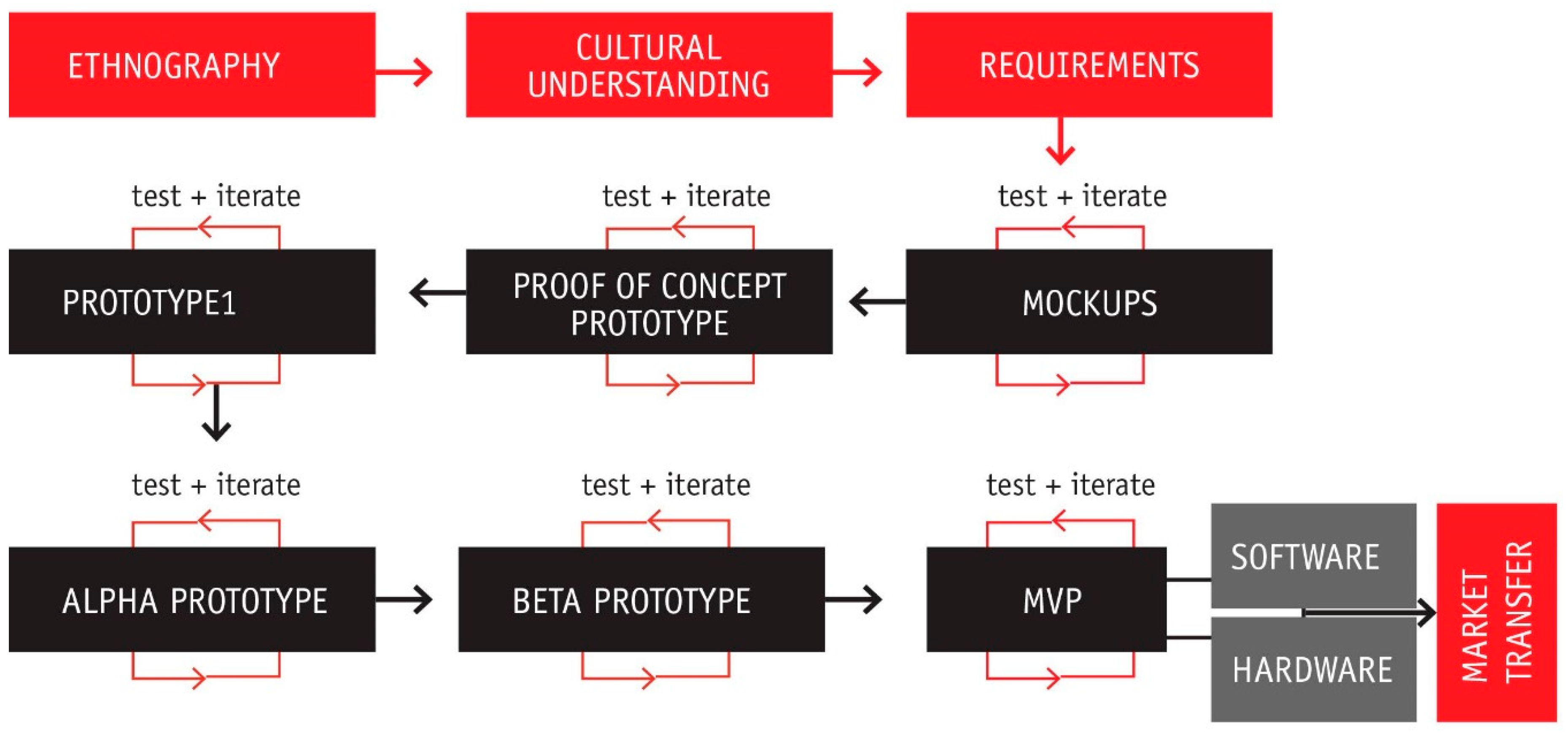
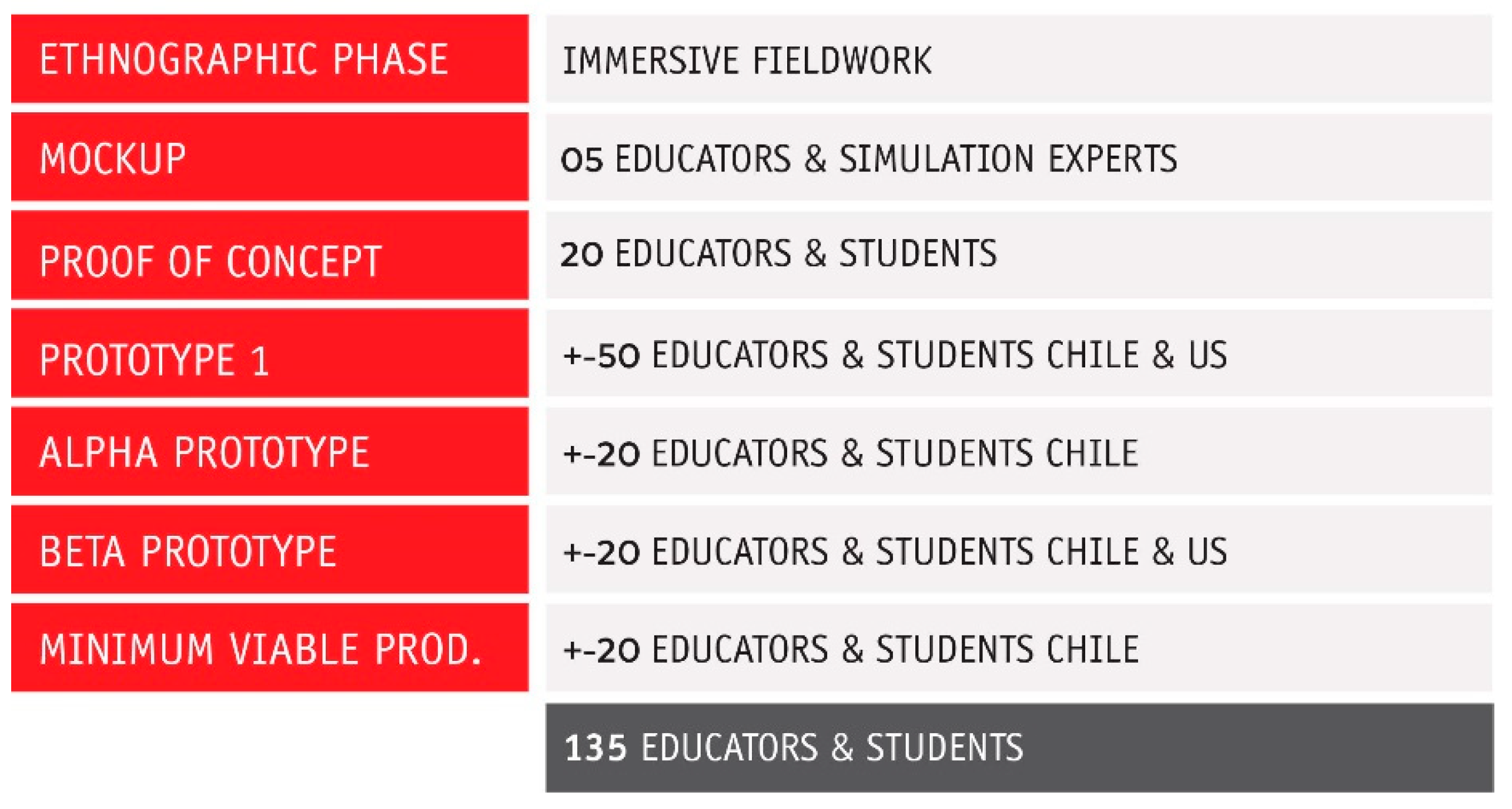
Methodology: An Anthro-Design Process Involving the Users
3. Results
3.1. Minimum Viable Product and User Centered Design Process
3.2. First Design Cycle: From Behaviors to Requirements, to Functional Prototypes
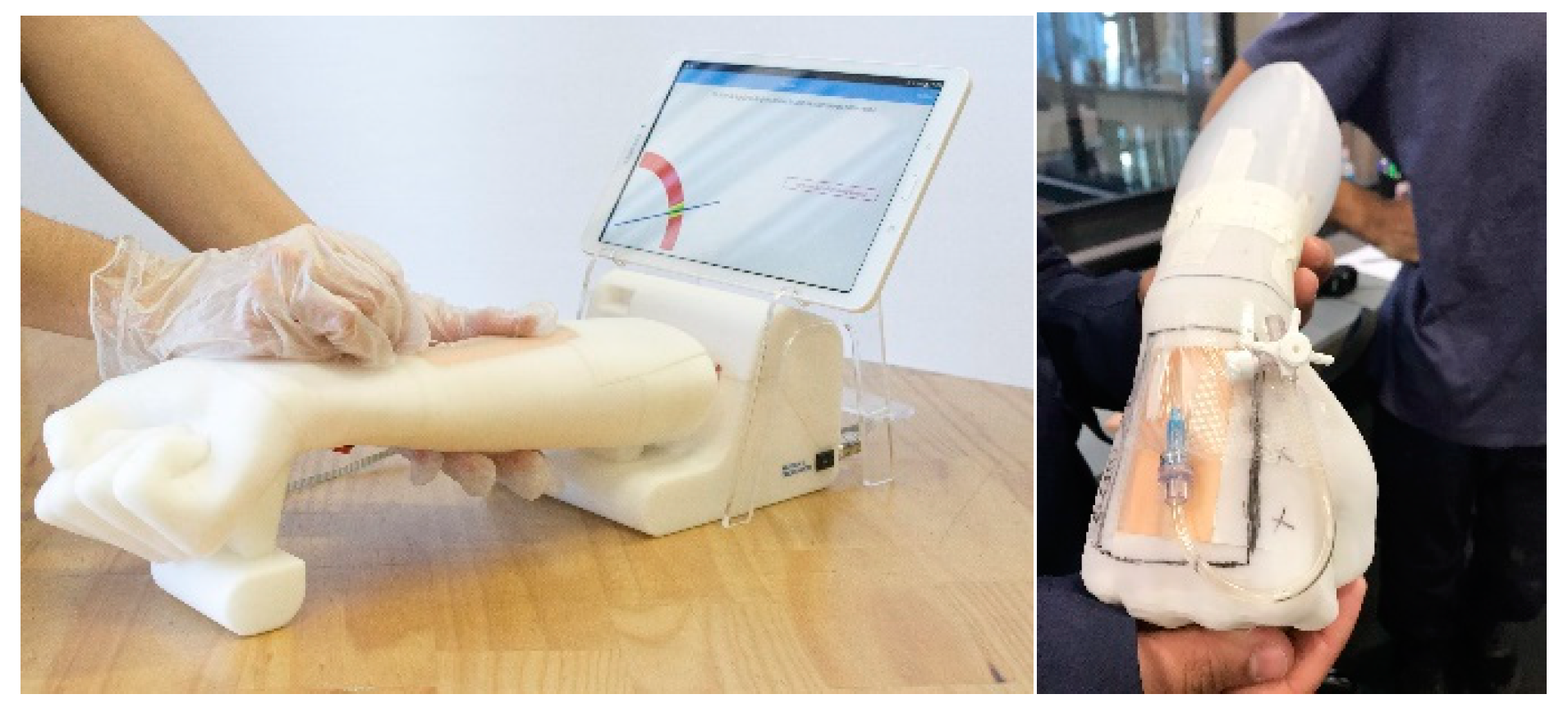
3.2.1. Mockups: Going from Behaviors to Requirements in Cheap Physical Prototypes
3.2.2. Consecutive Prototypes and User-Based Iterations
3.3. Second Development Stage: Prototype Iterations with the Users
“We have three IV trainers that serve 100 students, we understand the gap. There is a need for this to be scalable. We need it to be used in multiple sites for multiple students. We have 5 campuses for nurse programs.”(Director Health Science Simulation Center at the Nursing School).
“You are breaking the barrier between the user and the product!”(Simulation Specialist at the Health Science Simulation Center at the Nursing School)
“My job is to get the technology out of the way of the educators”. “There are so many different levels: equipment and the actual operations. The SIM technology is not very well designed, it is not very fancy technology. I want the technology to be invisible, so reliable that there isn’t that uncertainty if it will work or not. In my ideal world, there isn’t a need for an operator.”(Simulation Technician, Nursing School)
4. Discussion
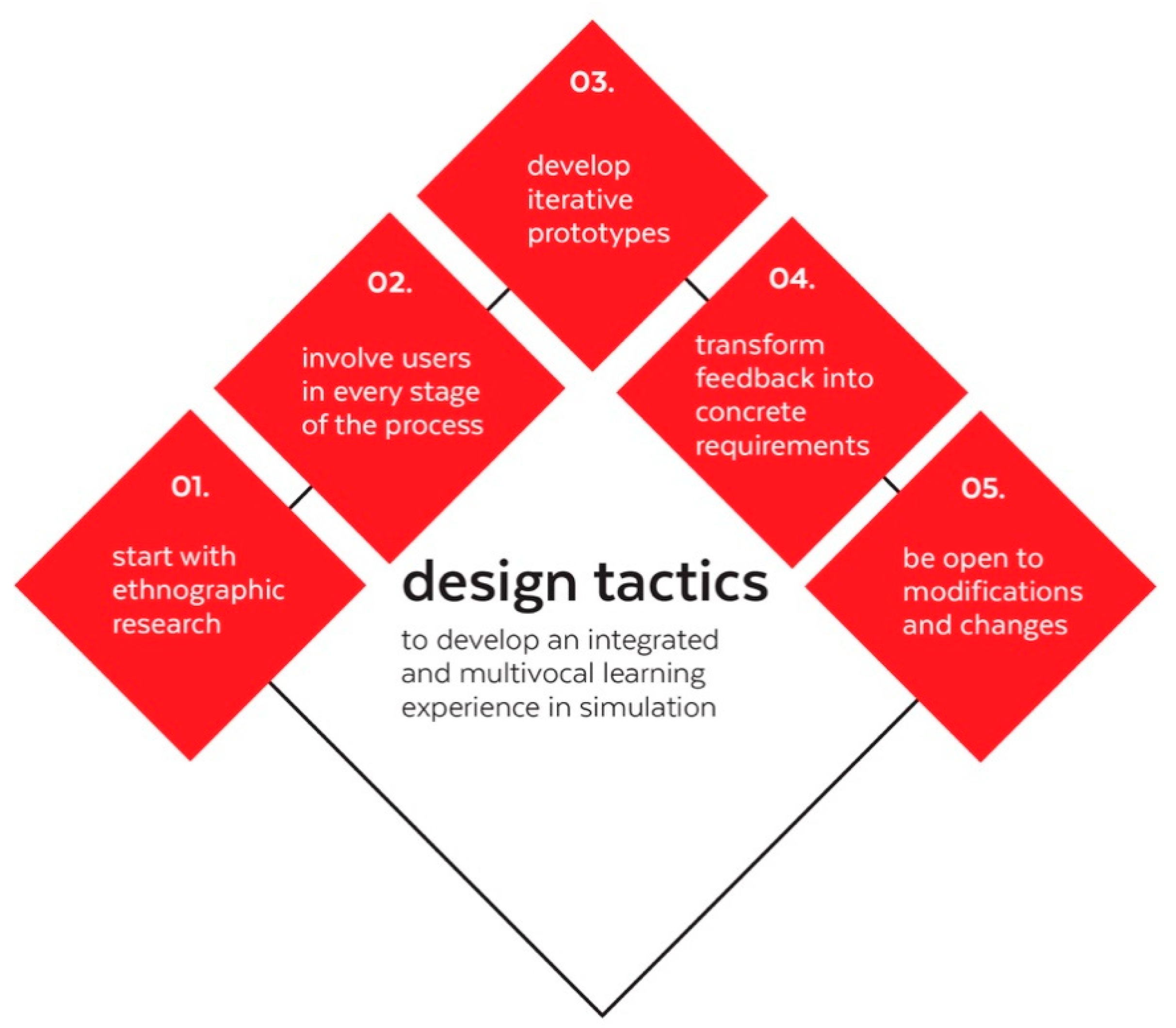
Design Tactics for Future Developments That Resonate with Educators and Students
- Start with ethnographic research: Start talking to your users in their field: Anthro Design works wonders because it involves going in the field and understanding their day-to-day activities. In turn, this means that future simulation designers and practitioners would benefit from learning the basics of qualitative research and some of the fundamental tools (and theoretical foundations of those tools), such as observation, semi structured interviews and field notes.
- Involve users in every stage of the process: Co-creating instead of convincing. Involve the user from the beginning and empower them to tell you about their ideas. People want to be heard. Additionally, we found that “snowball sampling” is key to testing with diverse institutions and individuals. When your participants are your allies, they can lead you to more participants.
- Develop iterative prototypes: Start with cheap prototypes like mockups before investing in packaging a full technology. Prototyping several times to receive continuous feedback can be cheaper than developing and getting to the users with something that does not resonate with them. Forecast and plan for incremental development cycles and not just one field research and not just one development stage. It may seem expensive and time consuming to address it that way, but it is much cheaper than producing a final product that will not appeal to user or will not have a meaningful impact
- Transform feedback into concrete requirements: Exercise translating qualitative information into design requirements. Sometimes it will not be too obvious, mostly because users do not think in terms of requirements (they think in terms of experience). However, creating requirements from data is a skill that can be developed over time.
- Be open to modifications and changes: Do not impose your solutions. Perhaps one of the more challenging aspects of adopting an ethnographic approach is to suspend your previous judgments when entering the field. Under an anthro-design methodology it is equally important not to grow infatuated with your current ideas. Be open to learning and making mistakes. Do not start the process with a solution and do not rush to one once you get a little data. Trust the process and maintain an open mind.
5. Conclusions
6. Patents
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wigton, R. See one, do one, teach one. Acad. Med. 1992, 67, 743. [Google Scholar]
- Vozenilek, J.; Huff, J.S.; Reznek, M.; Gordon, J.A. See one, do one, teach one: Advanced technology in medical education. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2004, 11, 1149–1154. [Google Scholar] [CrossRef] [PubMed]
- Rohrich, R.J. “See one, do one, teach one”: An old adage with a new twist. Plast. Reconstr. Surg. 2006, 118, 257–258. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, K.S.; Chen, A.; Standfield, N.J.; Gupte, C.M. The role of simulation in developing surgical skills. Curr. Rev. Musculoskelet. Med. 2014, 7, 155–160. [Google Scholar] [CrossRef]
- Duncan, J.R.; Henderson, K.; Street, M.; Richmond, A.; Klingensmith, M.; Beta, E.; Vannucci, A.; Murray, D. Creating and evaluating a data-driven curriculum for central venous catheter placement. J. Grad. Med Educ. 2010, 2, 389–397. [Google Scholar] [CrossRef]
- Cook, D.A.; Hatala, R.; Brydges, R.; Zendejas, B.; Szostek, J.H.; Wang, A.T.; Erwin, P.J.; Hamstra, S.J. Technology-enhanced simulation for health professions education: A systematic review and meta-analysis. JAMA 2011, 306, 978–988. [Google Scholar] [CrossRef]
- Aggarwal, R.; Mytton, O.T.; Derbrew, M.; Hananel, D.; Heydenburg, M.; Issenberg, B.; MacAulay, C.; Mancini, M.E.; Morimoto, T.; Soper, N.; et al. Training and simulation for patient safety. Qual. Saf. Health Care 2010, 19 (Suppl. 2), i34–i43. [Google Scholar] [CrossRef]
- Ma, I.W.Y.; Brindle, M.E.; Ronksley, P.E.; Lorenzetti, D.L.; Sauve, R.S.; Ghali, W.A. Use of Simulation-Based Education to Improve Outcomes of Central Venous Catheterization: A Systematic Review and Meta-Analysis. Acad. Med. 2011, 86, 1137–1147. [Google Scholar] [CrossRef] [PubMed]
- Haydn, J.; Smiley, R.; Alexander, M.; Kardong-edgren, S.; Jeffries, P. The NCSBN National Simulation Study: A Longitudinal, Randomized, Controlled Study Replacing Clinical Hours with Simulation in Prelicensure Nursing Education. J. Nurs. Regul. 2014, 5, S3–S40. [Google Scholar] [CrossRef]
- Ahlin, C.; Klang-Söderkvist, B.; Johansson, E.; Björkholm, M.; Löfmark, A. Assessing nursing students’ knowledge and skills in performing venepuncture and inserting peripheral venous catheters. Nurse Educ. Pract. 2017, 23, 8–14. [Google Scholar] [CrossRef]
- Liau, D.W. Injuries and Liability Related to Peripheral Catheters: A Closed Claims Analysis. ASA Newsl. 2006, 70, 11–13. [Google Scholar]
- Tagalakis, V.; Kahn, S.R.; Libman, M.; Blostein, M. The epidemiology of peripheral vein infusion thrombophlebitis: A critical review. Am. J. Med. 2002, 113, 146–151. [Google Scholar] [CrossRef]
- O’Grady, N.P.; Alexander, M.; Burns, L.A.; Dellinger, E.P.; Garland, J.; Heard, S.O.; Lipsett, P.A.; Masur, H.; Mermel, L.A.; Pearson, M.L.; et al. Guidelines for the prevention of intravascular catheter-related infections. Clin. Infect. Dis. 2011, 52, e162–e193. [Google Scholar] [CrossRef] [PubMed]
- Carlson, J.N.; Das, S.; De la Torre, F.; Callaway, C.W.; Phrampus, P.E.; Hodgins, J. Motion capture measures variability in laryngoscopic movement during endotracheal intubation: A preliminary report. Simul. Healthc. J. Soc. Simul. Healthc. 2012, 7, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Rohrer, C.; Au, I.; Darnell, E.; Dickenson, N.; Evenson, S.; Kaasgaard, K. Design, marketing, strategy? Where does user research belong? In Proceedings of the Conference on Human Factors in Computing Systems, Florence, Italy, 5–10 April 2008; pp. 2241–2244. [Google Scholar] [CrossRef]
- Partala, T.; Saari, T. Understanding the most influential user experiences in successful and unsuccessful technology adoptions. Comput. Hum. Behav. 2015, 53, 381–395. [Google Scholar] [CrossRef]
- Miranda, C. Crash-Course de Antro-Diseño; Ediciones UC: Santiago, Chile, 2019. [Google Scholar]
- Lavoie, P.; Clarke, S.P. Simulation in nursing education. Nurs. Manag. 2017, 48, 16–17. [Google Scholar] [CrossRef]
- Maloney, S.; Haines, T. Issues of cost-benefit and cost-effectiveness for simulation in health professions education. Adv. Simul. 2016, 1, 13. [Google Scholar] [CrossRef]
- Vanderbeeken, M. Taking a broader view of the human experience. Interactions 2009, 16, 54–57. [Google Scholar] [CrossRef]
- Cant, R.P.; Cooper, S.J. Use of simulation-based learning in undergraduate nurse education: An umbrella systematic review. Nurse Educ. Today 2017, 49, 63–71. [Google Scholar] [CrossRef]
- Kaakinen, J.; Arwood, E. Systematic review of nursing simulation literature for use of learning theory. Int. J. Nurs. Educ. Sch. 2009, 6. [Google Scholar] [CrossRef]
- Lavoie, P.; Michaud, C.; Bélisle, M.; Boyer, L.; Gosselin, É.; Grondin, M.; Larue, C.; Lavoie, S.; Pepin, J. Learning theories and tools for the assessment of core nursing competencies in simulation: A theoretical review. J. Adv. Nurs. 2018, 74, 239–250. [Google Scholar] [CrossRef] [PubMed]
- Hennig, K.; Kirova, A. The role of cultural artefacts in play as tools to mediate learning in an intercultural preschool programme. Contemp. Issues Early Child. 2012, 13, 226–241. [Google Scholar] [CrossRef]
- Varga-Atkins, T.; McIsaac, J.; Willis, I. Focus Group meets Nominal Group Technique: An effective combination for student evaluation? Innov. Educ. Teach. 2017, 54, 289–300. [Google Scholar] [CrossRef]
- Healey, M.; Flint, A.; Harrington, K. Students as partners: Reflections on a conceptual model. Teach. Learn. Inq. 2016, 4, 1–13. [Google Scholar]
- Cooper, A.; Reimann, R. About Face 2.0. The Essentials of Interaction Design; Wiley: Indianapolis, IN, USA, 2003. [Google Scholar]
- Garrett, J.J. The Elements of User Experience: User-Centered Design for the Web and Beyond; New Riders: Berkeley, CA, USA, 2010. [Google Scholar]
- Goodwin, K. Designing for the Digital Age: How to Create Human-Centered Products and Services; John Wiley & Sons: Indianapolis, IN, USA, 2011. [Google Scholar]
- Wasson, C. Ethnography in the field of design. Hum. Organ. 2000, 59, 377–388. [Google Scholar] [CrossRef]
- Plattner, H.; Meinel, C.; Leifer, L. Design Thinking: Understand Improve Apply (Understanding Innovation), 1st ed.; Springer: Berlin, Germany, 2010. [Google Scholar]
- Lawson, B. How Designers Think: The Design Process Demystified, 4th ed.; Architectural Press: Burlington, NJ, USA, 2005. [Google Scholar]
- Agar, M. Speaking of Ethnography, 1st ed.; Sage Publications: Beverly Hills, CA, USA, 1986. [Google Scholar]
- Clifford, J. Anthropology and/as Travel. Etnofoor 1996, 9, 5–15. [Google Scholar]
- Wolcott, H.F. Ethnography Lessons: A Primer; Left Coast Press: Walnut Creek, CA, USA, 2010. [Google Scholar]
- Newell, A.; Shaw, J.; Simon, H. “The Process of Creative Thinking”. In Contemporary Approaches to Creative Thinking; Gruber, H., Terrel, G., Wertheimer, M., Eds.; Literary Licensing: New York, NY, USA, 1967; pp. 63–119. [Google Scholar]
- Lassiter, L.E. Invitation to Anthropology, 3rd ed.; Altamira Press: Lanham, MD, USA, 2006. [Google Scholar]
- Schensul, S.; Schensul, J.; LeCompte, M. Essential Ethnographic Methods: Observations, Interviews, and Questionnaires; Alta Mira: Walnut Creek, CA, USA, 1999. [Google Scholar]
- Britten, N. Qualitative interviews in medical research. BMJ 1995, 311, 251–253. [Google Scholar] [CrossRef]
- Weiss, R.S. In their own words: Making the most of qualitative interviews. Contexts 2004, 3, 44–51. [Google Scholar] [CrossRef]
- Bernard, R.H. Research Methods in Anthropology: Qualitative and Quantitative Methods; AltaMira Press: Walnut Creek, CA, USA, 2002. [Google Scholar]
- Wolcott, H.F. Ethnography: A Way of Seeing, 2nd ed.; AltaMira Press: Lanham, MD, USA, 2008. [Google Scholar]
- Strauss, A.; Corbin, J. Basics of Qualitative Research, 2nd ed.; Sage Publications: Thousand Oakes, CA, USA, 1998. [Google Scholar]
- Bryant, A.; Charmaz, K.C. The SAGE Handbook of Grounded Theory; SAGE Publications: Thousand Oaks, CA, USA, 2007. [Google Scholar]
- Norman, D.A.; Verganti, R. Incremental and Radical Innovation: Design Research vs. Technology and Meaning Change. Design Issues 2014, 30, 78–96. [Google Scholar] [CrossRef]
- Koivisto, J.-M.; Haavisto, E.; Niemi, H.; Haho, P.; Nylund, S.; Multisilta, J. Design principles for simulation games for learning clinical reasoning: A design-based research approach. Nurse Educ. Today 2018, 60, 114–120. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miranda, C.; Altermatt, F.; Villagrán, I.; Goñi, J. Developing an Innovative Medical Training Simulation Device for Peripheral Venous Access: A User-Centered Design Approach. Healthcare 2020, 8, 420. https://doi.org/10.3390/healthcare8040420
Miranda C, Altermatt F, Villagrán I, Goñi J. Developing an Innovative Medical Training Simulation Device for Peripheral Venous Access: A User-Centered Design Approach. Healthcare. 2020; 8(4):420. https://doi.org/10.3390/healthcare8040420
Chicago/Turabian StyleMiranda, Constanza, Fernando Altermatt, Ignacio Villagrán, and Julián Goñi. 2020. "Developing an Innovative Medical Training Simulation Device for Peripheral Venous Access: A User-Centered Design Approach" Healthcare 8, no. 4: 420. https://doi.org/10.3390/healthcare8040420
APA StyleMiranda, C., Altermatt, F., Villagrán, I., & Goñi, J. (2020). Developing an Innovative Medical Training Simulation Device for Peripheral Venous Access: A User-Centered Design Approach. Healthcare, 8(4), 420. https://doi.org/10.3390/healthcare8040420





