Identifying Predictive Characteristics of Opioid Medication Use among a Nationally Representative Sample of United States Older Adults with Pain and Comorbid Hypertension or Hypercholesterolemia
Abstract
1. Introduction
2. Materials and Methods
2.1. Medical Expenditure Panel Survey (MEPS) Study Design
2.2. Eligibility Criteria
2.3. Predictor Variables
2.4. Dependent Variable
2.5. Data Analysis
3. Results
3.1. Selection of Study Subjects
3.2. Prevalence of Opioid Medication Use among Study Subjects
3.3. Characteristics of Study Subjects
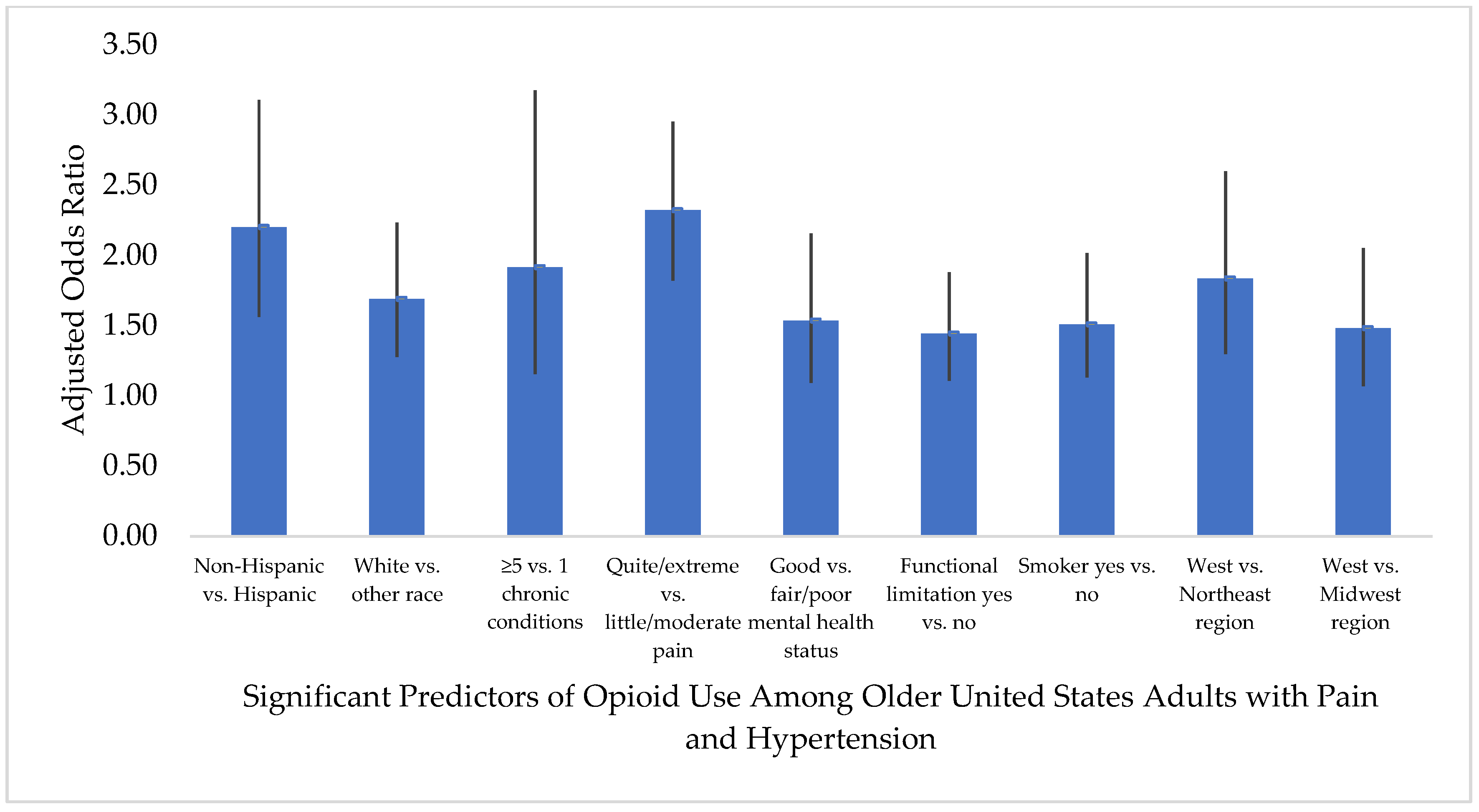
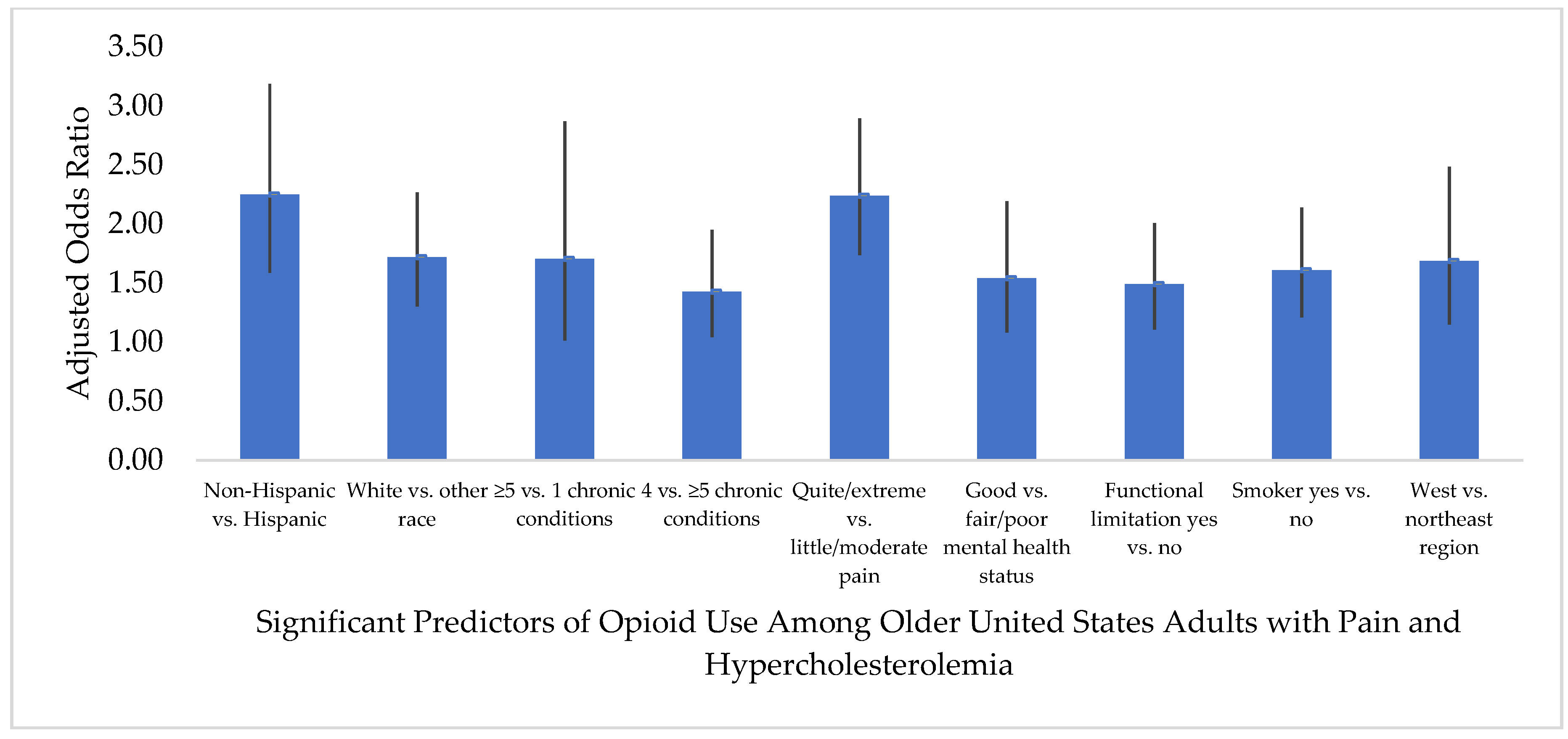
3.4. Predictors of Opioid Medication Use
4. Discussion
4.1. Predisposing Factors
4.2. Need Factors
4.3. Personal Health Practice Factors
4.4. External Environmental Factors
4.5. Prevalence of Opioid Use
4.6. Implications for Clinical Care
4.7. Limitations and Future Work
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dahlhamer, J.; Lucas, J.; Zelaya, C.; Nahin, R.; Mackey, S.; DeBar, L.; Kerns, R.; Von Korff, M.; Porter, L.; Helmick, C. Prevalence of Chronic Pain and High-Impact Chornic Pain among Adults—United States. 2016. Available online: https://www.cdc.gov/mmwr/volumes/67/wr/mm6736a2.htm?s_cid=mm6736a2_w (accessed on 26 June 2020).
- Centers for Disease Control and Prevention. Summary Health Statistics for U.S. Adults: National Health Interview Survey. 2012. Available online: https://www.cdc.gov/nchs/data/series/sr_10/sr10_260.pdf (accessed on 15 August 2020).
- Patel, K.V.; Guralnik, J.M.; Dansie, E.J.; Turk, D.C. Prevalence and impact of pain among older adults in the United states: Findings from the 2011 National Health and Aging Trends Study. Pain 2013, 154, 2649–2657. [Google Scholar] [CrossRef]
- Cochran, G.; Rosen, D.; McCarthy, R.M.; Engel, R.J. Risk Factors for Symptoms of Prescription Opioid Misuse: Do Older Adults Differ from Younger Adult Patients? J. Gerontol. Soc. Work 2017, 60, 443–457. [Google Scholar] [CrossRef] [PubMed]
- James, S.L.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef]
- Nahin, R.L.; Sayer, B.; Stussman, B.J.; Feinberg, T.M. Eighteen-year trends in the prevalence of, and health care use for, noncancer pain in the United States: Data from the Medical Expenditure Panel Survey. J. Pain 2019, 20, 796–809. [Google Scholar] [CrossRef]
- Axon, D.R.; Patel, M.J.; Martin, J.R.; Slack, M.K. Use of multidomain management strategies by community dwelling adults with chronic pain: Evidence from a systematic review. Scand J. Pain 2019, 19, 9–23. [Google Scholar] [CrossRef]
- Chau, D.L.; Walker, V.; Pai, L.; Cho, L.M. Opiates and elderly: Use and side effects. Clin. Interv. Aging 2008, 3, 273–278. [Google Scholar] [CrossRef]
- National Institute on Drug Abuse. Commonly Used Drugs. Available online: https://www.drugabuse.gov/sites/default/files/Commonly-Used-Drugs-Charts_final_June_2020_optimized.pdf (accessed on 15 August 2020).
- Papaleontiou, M.; Henderson, C.R., Jr.; Turner, B.J.; Moore, A.A.; Olkhovskaya, Y.; Amanfo, L.; Reid, M.C. Outcomes associated with opioid use in the treatment of chronic noncancer pain in older adults: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 2010, 58, 1353–1369. [Google Scholar] [CrossRef]
- Cavalieri, T.A. Management of pain in older adults. J. Am. Osteopa. Assoc. 2005, 105, S12–S17. [Google Scholar]
- Agency for Healthcare Research and Quality. Evidence-Based Practice Center Technical Brief Protocol. Prevention, Diagnosis, and Management of Opioids, Opioid Misuse and Opioid Use Disorder in Older Adults. Available online: https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/opioids-oa-protocol.pdf (accessed on 26 June 2020).
- CDC Guideline for Prescribing Opioids for Chronic Pain—United States. 2016. Available online: https://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fmmwr%2Fvolumes%2F65%2Frr%2Frr6501e1er.htm (accessed on 26 June 2020).
- Schneider, V.; Lévesque, L.E.; Zhang, B.; Hutchinson, T.; Brophy, J.M. Association of selective and conventional nonsteroidal antiinflammatory drugs with acute renal failure: A population-based, nested case-control analysis. Am. J. Epidemiol. 2006, 164, 881–889. [Google Scholar] [CrossRef]
- Gislason, G.H.; Rasmussen, J.N.; Abildstrom, S.Z.; Schramm, T.K.; Hansen, M.L.; Fosbøl, E.L.; Sørensen, R.; Folke, F.; Buch, P.; Gadsbøll, N.; et al. Increased mortality and cardiovascular morbidity associated with use of nonsteroidal anti-inflammatory drugs in chronic heart failure. Arch. Intern. Med. 2009, 169, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Haag, M.D.M.; Bos, M.J.; Hofman, A.; Koudstaal, P.J.; Breteler, M.M.B.; Stricker, B.H.C. Cyclooxygenase selectivity of nonsteroidal anti-inflammatory drugs and risk of stroke. Arch. Intern. Med. 2008, 168, 1219–1224. [Google Scholar] [CrossRef] [PubMed]
- Griffin, M.R. Epidemiology of nonsteroidal anti-inflammatory drug–associated gastrointestinal injury. Am. J. Med. 1998, 104, 23S–29S. [Google Scholar] [CrossRef]
- Weiss, A.J.; Heslin, K.C.; Barrett, M.L.; Izar, R.; Bierman, A.S. Opioid-Related Inpatient Stays and Emergency Department Visits among Patients Aged 65 Years and Older, 2010 and 2015: Statistical Brief #244. Available online: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb244-Opioid-Inpatient-Stays-ED-Visits-Older-Adults.pdf (accessed on 26 June 2020).
- Singh, J.A.; Cleveland, J.D. National U.S. time-trends in opioid use disorder hospitalizations and associated healthcare utilization and mortality. PLoS ONE 2020, 15, e0229174. [Google Scholar] [CrossRef] [PubMed]
- Axon, D.R.; Slack, M.; Barraza, L.; Lee, J.K.; Warholak, T. Nationally representative health care expenditures of community-based older adults with pain in the United States prescribed opioids vs those not prescribed opioids. Pain Med. 2020, 114. [Google Scholar] [CrossRef]
- Chou, R.; Turner, J.A.; Devine, E.B.; Hansen, R.N.; Sullivan, S.D.; Blazina, I.; Dana, T.; Bougatsos, C.; Deyo, R.A. The effectiveness and risks of long-term opioid therapy for chronic pain: A systematic review for a National Institutes of Health pathways to prevention workshop. Ann. Intern. Med. 2015, 162, 276–286. [Google Scholar] [CrossRef]
- Oh, G.; Abner, E.L.; Fardo, D.W.; Freeman, P.R.; Moga, D.C. Patterns and predictors of chronic opioid use in older adults: A retrospective cohort study. PLoS ONE 2019, 14, e0210341. [Google Scholar] [CrossRef]
- Thielke, S.M.; Shortreed, S.M.; Saunders, K.; Turner, J.A.; LeResche, L.; Von Korff, M. A prospective study of predictors of long-term opioid use among patients with chronic noncancer pain. Clin. J. Pain 2017, 33, 198–204. [Google Scholar] [CrossRef]
- Fryar, C.D.; Ostchega, Y.; Hales, C.M.; Zhang, G.; Kruszon-Moran, D. NCHS Data Brief No. 289 October 2017. Hypertension Prevalence and Control among Adults: United States, 2015–2016. Available online: https://www.cdc.gov/nchs/data/databriefs/db289.pdf (accessed on 15 August 2020).
- Carroll, M.D.; Fryar, C.D.; Nguyen, D.T. NCHS Data Brief No. 290 October 2017. Total and High-Density Lipoprotein Cholesterol in Adults: United States, 2015–2016. Available online: https://www.cdc.gov/nchs/data/databriefs/db290.pdf (accessed on 15 August 2020).
- Agency for Healthcare Research and Quality. Survey Background. Available online: https://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp (accessed on 26 June 2020).
- Agency for Healthcare Research and Quality. MEPS HC-201 2017 Full Year Consolidated Data File. Available online: https://meps.ahrq.gov/data_stats/download_data/pufs/h201/h201doc.pdf (accessed on 26 June 2020).
- Agency for Healthcare Research and Quality. MEPS HC-201 2017 Full Year Consolidated Data Codebook. Available online: https://meps.ahrq.gov/data_stats/download_data/pufs/h201/h201cb.pdf (accessed on 26 June 2020).
- Agency for Healthcare Research and Quality. Download Data Files, Documentation, and Codebooks. Available online: https://meps.ahrq.gov/mepsweb/data_stats/download_data_files.jsp (accessed on 26 June 2020).
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality. MEPS HC-197A 2017 Prescribed Medicines. Available online: https://meps.ahrq.gov/data_stats/download_data/pufs/h197a/h197adoc.pdf (accessed on 26 June 2020).
- Agency for Healthcare Research and Quality. MEPS HC-197A Codebook 2017 Prescribed Medicines. Available online: https://meps.ahrq.gov/data_stats/download_data/pufs/h197a/h197acb.pdf (accessed on 26 June 2020).
- Chen, I.; Kurz, J.; Pasanen, M.; Faselis, C.; Panda, M.; Staton, L.J.; O’Rorke, J.; Menon, M.; Genao, I.; Wood, J.; et al. Racial differences in opioid use for chronic nonmalignant pain. J. Gen. Intern Med. 2005, 20, 593–598. [Google Scholar] [CrossRef]
- Harrison, J.M.; Lagisetty, P.; Sites, B.D.; Guo, C.; Davis, M.A. Trends in prescription pain medication use by race/ethnicity among US adults with noncancer pain, 2000–2015. Am. J. Public Health 2018, 108, 788–790. [Google Scholar] [CrossRef]
- Davis, M.A.; Lin, L.A.; Liu, H.; Sites, B.D. Prescription opioid use among adults with mental health disorders in the United States. J. Am. Board. Fam. Med. 2017, 30, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Richardson, L.P.; Russo, J.E.; Katon, W.; McCarty, C.A.; DeVries, A.; Edlund, M.J.; Martin, B.C.; Sullivan, M.D. Mental health disorders and chronic opioid use among adolescents and young adults with chronic pain. J. Adolesc. Health 2012, 50, 553–558. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Clarke, D.M.; Currie, K.C. Depression, anxiety and their relationship with chronic diseases: A review of the epidemiology, risk and treatment evidence. Med. J. Aust. 2009, 190, S54–S60. [Google Scholar] [CrossRef]
- Valkanoff, T.A.; Kline-Simon, A.H.; Sterling, S.; Campbell, C. Functional disability among chronic pain patients receiving long-term opioid treatment. J. Soc. Work Disabil. Rehabil. 2012, 11, 128–142. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heydari, G.; Hosseini, M.; Yousefifard, M.; Asady, H.; Baikpour, M.; Barat, A. Smoking and physical activity in healthy adults: A cross-sectional study in Tehran. Tanaffos 2015, 14, 238–245. [Google Scholar]
- Unick, G.J.; Ciccarone, D. US regional and demographic differences in prescription opioid and heroin-related overdose hospitalizations. Int. J. Drug Policy 2017, 46, 112–119. [Google Scholar] [CrossRef]
- Keyes, K.M.; Cerdá, M.; Brady, J.E.; Havens, J.R.; Galea, S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am. J. Public Health 2014, 104, e52–e59. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention National Center for Injury Prevention and Control. 2018 Annual Surveillance Report of Drug-Related Risks and Outcomes. Available online: https://www.cdc.gov/drugoverdose/pdf/pubs/2018-cdc-drug-surveillance-report.pdf (accessed on 15 August 2020).
- Axon, D.R.; Bhattacharjee, S.; Warholak, T.L.; Slack, M.K. Xm2 scores for estimating total exposure to multimodal strategies identified by pharmacists for managing pain: Validity testing and clinical relevance. Pain Res. Manag. 2018, 2018, 1–11. [Google Scholar] [CrossRef]
- Polónia, J. Interaction of antihypertensive drugs with anti-inflammatory drugs. Cardiology 1997, 88, 47–51. [Google Scholar] [CrossRef]
- Moore, N.; Pollack, C.; Butkerait, P. Adverse drug reactions and drug–drug interactions with over-the-counter NSAIDs. Ther. Clin. Risk Manag. 2015, 11, 1061–1075. [Google Scholar] [CrossRef]
- Aljadhey, H.; Tu, W.; Hansen, R.A.; Blalock, S.J.; Brater, D.C.; Murray, M.D. Comparative effects of non-steroidal anti-inflammatory drugs (NSAIDs) on blood pressure in patients with hypertension. BMC Cardiovasc. Disord. 2012, 12, 93. [Google Scholar] [CrossRef] [PubMed]
- Varga, Z.; Sabzwari, S.R.A.; Vargova, V. Cardiovascular risk of nonsteroidal anti-inflammatory drugs: An under-recognized public health issue. Cureus 2017, 9, e1144. [Google Scholar] [CrossRef] [PubMed]
| Pain-Hypertension Group | Pain-Hypercholesterolemia Group | |||||
|---|---|---|---|---|---|---|
| Factors | Opioid User wt.% (95% CI) | Non-User wt.% (95% CI) | p | Opioid User wt.% (95% CI) | Non-User wt.% (95% CI) | p |
| Predisposing factors: | ||||||
| Age ≥65 years | 55.9 (52.0–59.8) | 59.6 (56.5–62.7) | 0.1279 | 56.6 (52.5–60.8) | 60.6 (57.4–63.7) | 0.1246 |
| Non-Hispanic | 94.5 (93.1–95.9) | 89.9 (88.2–91.7) | <0.0001 | 94.7 (93.1–96.2) | 89.5 (87.8–91.3) | <0.0001 |
| White | 81.1 (77.7–84.5) | 76.5 (74.0–79.0) | 0.0270 | 84.1 (81.1–87.1) | 80.3 (78.0–82.5) | 0.0383 |
| Female | 57.0 (53.1–61.0) | 52.4 (49.8–55.0) | 0.0456 | 53.7 (49.2–58.2) | 52.6 (49.9–55.3) | 0.6975 |
| Enabling factors: | ||||||
| >High school education | 44.2 (39.3–49.1) | 50.7 (47.6–53.8) | 0.0161 | 45.0 (40.3–49.7) | 50.5 (47.7–53.3) | 0.0754 |
| Unemployed | 76.3 (72.3–80.3) | 68.8 (65.7–72.0) | 0.0030 | 73.6 (69.3–77.6) | 67.7 (64.4–71.0) | 0.0261 |
| Married | 49.8 (45.6–54.0) | 56.0 (53.2–58.8) | 0.0086 | 52.6 (47.9–57.3) | 57.7 (55.0–60.4) | 0.0401 |
| Private health insurance | 53.8 (49.4–58.1) | 59.2 (56.3–62.2) | 0.0581 | 55.9 (51.5–60.3) | 60.1 (56.9–63.3) | 0.1626 |
| Middle/high income | 59.7 (55.2–64.2) | 65.6 (62.8–68.3) | 0.0137 | 61.7 (57.0–66.5) | 66.9 (64.2–69.7) | 0.0348 |
| Need factors: | ||||||
| ≥5 chronic conditions | 41.0 (36.9–45.1) | 31.2 (28.6–33.9) | <0.0001 | 39.6 (35.5–43.6) | 32.0 (29.3–34.7) | <0.0001 |
| Little/moderate pain | 51.4 (47.3–55.5) | 75.8 (73.3–78.3) | <0.0001 | 55.2 (50.9–59.4) | 77.9 (75.4–80.4) | <0.0001 |
| Ex/VG physical health | 21.2 (17.8–24.5) | 30.0 (27.4–32.7) | <0.0001 | 24.8 (21.3–28.2) | 32.2 (29.7–34.7) | <0.0001 |
| Ex/VG mental health | 40.1 (35.9–44.3) | 49.9 (46.9–52.9) | 0.0004 | 41.9 (37.8–46.0) | 50.4 (47.3–53.4) | 0.0024 |
| ADL limitation | 9.9 (7.7–12.1) | 5.8 (4.5–7.1) | 0.0005 | 8.1 (6.1–10.0) | 5.0 (3.8–6.2) | 0.0070 |
| IADL limitation | 16.5 (13.5–19.4) | 10.0 (8.4–11.6) | <0.0001 | 14.0 (11.2–16.9) | 8.9 (7.3–10.5) | 0.0011 |
| Functional limitation | 63.3 (59.3–67.3) | 42.1 (39.6–44.7) | <0.0001 | 60.3 (56.1–64.5) | 39.8 (37.2–42.5) | <0.0001 |
| Work limitation | 47.8 (43.5–52.1) | 28.5 (26.1–30.9) | <0.0001 | 44.9 (40.6–49.1) | 26.9 (24.3–29.4) | <0.0001 |
| Personal health practices: | ||||||
| Frequent exercise | 32.5 (28.8–36.2) | 37.8 (35.0–40.6) | 0.0199 | 35.3 (31.5–39.2) | 39.8 (37.2–42.5) | 0.0459 |
| Smoker | 19.4 (16.2–22.6) | 12.0 (10.5–13.6) | <0.0001 | 19.7 (16.6–22.7) | 11.2 (9.7–12.7) | <0.0001 |
| External environmental: | ||||||
| South region | 44.1 (39.5–48.6) | 38.1 (35.0–41.3) | 0.0096 | 43.3 (38.7–47.9) | 37.6 (34.6–40.5) | 0.0386 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Axon, D.R.; Vaffis, S.; Marupuru, S. Identifying Predictive Characteristics of Opioid Medication Use among a Nationally Representative Sample of United States Older Adults with Pain and Comorbid Hypertension or Hypercholesterolemia. Healthcare 2020, 8, 341. https://doi.org/10.3390/healthcare8030341
Axon DR, Vaffis S, Marupuru S. Identifying Predictive Characteristics of Opioid Medication Use among a Nationally Representative Sample of United States Older Adults with Pain and Comorbid Hypertension or Hypercholesterolemia. Healthcare. 2020; 8(3):341. https://doi.org/10.3390/healthcare8030341
Chicago/Turabian StyleAxon, David R., Shannon Vaffis, and Srujitha Marupuru. 2020. "Identifying Predictive Characteristics of Opioid Medication Use among a Nationally Representative Sample of United States Older Adults with Pain and Comorbid Hypertension or Hypercholesterolemia" Healthcare 8, no. 3: 341. https://doi.org/10.3390/healthcare8030341
APA StyleAxon, D. R., Vaffis, S., & Marupuru, S. (2020). Identifying Predictive Characteristics of Opioid Medication Use among a Nationally Representative Sample of United States Older Adults with Pain and Comorbid Hypertension or Hypercholesterolemia. Healthcare, 8(3), 341. https://doi.org/10.3390/healthcare8030341







