Evaluation of Pediatric Surgical Site Infections Associated with Colorectal Surgeries at an Academic Children’s Hospital
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population
2.3. Data Collection/Study Procedures
2.4. Definitions
2.5. Statistical Analysis
3. Results
3.1. Assessment of AP Compliance
3.2. Surgical Site Infections
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Berríos-Torres, S.I.; Umscheid, C.A.; Bratzle, D.W.; Leas, B.; Stone, E.C.; Kelz, R.R.; Reinke, C.E.; Morgan, S.; Solomkin, J.S.; Mazuski, J.E.; et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017, 152, 784. [Google Scholar]
- Ban, K.A.; Minei, J.P.; Laronga, C.; Harbrecht, B.G.; Jensen, E.H.; Fry, D.E.; Itani, K.M.; Dellinger, E.P.; Ko, C.Y.; Duane, T.M. American College of Surgeons and Surgical Infection Society: Surgical Site Infection Guidelines, 2016 Update. J. Am. Coll. Surg. 2017, 224, 59–74. [Google Scholar] [CrossRef] [PubMed]
- Rangel, S.J.; Islam, S.; Peter, S.D.S.; Goldin, A.B.; Abdullah, F.; Downard, C.D.; Saito, J.; Blakely, M.L.; Puligandla, P.S.; Dasgupta, R.; et al. Prevention of infectious complications after elective colorectal surgery in children: An American Pediatric Surgical Association Outcomes and Clinical Trials Committee comprehensive review. J. Pediatr. Surg. 2015, 50, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.L.; Bohl, J.K.; Mcelearney, S.T.; Friel, C.M.; Barclay, M.M.; Sawyer, R.G.; Foley, E.F. Wound Infection After Elective Colorectal Resection. Ann. Surg. 2004, 239, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Schilling, P.L.; Dimick, J.; Birkmeyer, J.D. Prioritizing Quality Improvement in General Surgery. J. Am. Coll. Surg. 2008, 207, 698–704. [Google Scholar] [CrossRef]
- Feng, C.; Sidhwa, F.; Cameron, D.B.; Glass, C.; Rangel, S. Rates and burden of surgical site infections associated with pediatric colorectal surgery: Insight from the National Surgery Quality Improvement Program. J. Pediatr. Surg. 2016, 51, 970–974. [Google Scholar] [CrossRef]
- Dornfeld, M.; Lovely, J.K.; Huebner, M.; Larson, D.W. Surgical Site Infection in Colorectal Surgery. Dis. Colon Rectum 2017, 60, 971–978. [Google Scholar] [CrossRef]
- McKibben, L.; Horan, T.; Tokars, J.I.; Fowler, G.; Cardo, D.M.; Pearson, M.L.; Brennan, P.J. Guidance on Public Reporting of Healthcare-Associated Infections: Recommendations of the Healthcare Infection Control Practices Advisory Committee. Am. J. Infect. Control. 2005, 33, 217–226. [Google Scholar] [CrossRef]
- Bratzle, D.W.; Dellinger, E.P.; Olsen, K.M.; Perl, T.M.; Auwaerter, P.G.; Bolon, M.K.; Fish, D.N.; Napolitano, L.M.; Sawyer, R.G.; Slain, D.; et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am. J. Heal. Pharm. 2013, 70, 195–283. [Google Scholar] [CrossRef]
- Anderson, D.J.; Podgorny, K.; Berríos-Torres, S.I.; Bratzle, D.W.; Dellinger, E.P.; Greene, L.; Nyquist, A.-C.; Saiman, L.; Yokoe, D.S.; Maragakis, L.L.; et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect. Control. Hosp. Epidemiol. 2014, 35, 605–627. [Google Scholar] [CrossRef]
- Global Guidelines for the Prevention of Surgical Site Infection. Available online: http://www.who.int/iris/handle/10665/250680 (accessed on 20 July 2017).
- Global Guidelines for the Prevention of Surgical Site Infection, 2nd ed. Available online: http://www.who.int/iris/handle/10665/277399 (accessed on 4 June 2019).
- Tourmousoglou, C.E.; Yiannakopoulou, E.C.; Bramis, J.; Papadopoulos, J.S.; Kalapothaki, V. Adherence to guidelines for antibiotic prophylaxis in general surgery: A critical appraisal. J. Antimicrob. Chemother. 2007, 61, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Kilan, R.; Moran, D.; Eid, I.; Okeahialam, C.; Quinn, C.; Binsaddiq, W.; Williams, T.; Johnson, M.H. Improving antibiotic prophylaxis in gastrointestinal surgery patients: A quality improvement project. Ann. Med. Surg. 2017, 20, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, M.; Macfarlane, G. Changes in predominant bacterial populations in human faeces with age and with Clostridium difficile infection. J. Med Microbiol. 2002, 51, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, M.; Sharp, R.; Macfarlane, G.T. Age and disease related changes in intestinal bacterial populations assessed by cell culture, 16S rRNA abundance, and community cellular fatty acid profiles. Gut 2001, 48, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Costs of Intimate Partner Violence against Women in the United States; CDC, National Center for Injury Prevention and Control: Atlanta, GA, USA, 2003. [Google Scholar]
- Bull, A.; Russo, P.; Friedman, N.; Bennett, N.; Boardman, C.; Richards, M. Compliance with surgical antibiotic prophylaxis–reporting from a statewide surveillance programme in Victoria, Australia. J. Hosp. Infect. 2006, 63, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Putnam, L.R.; Chang, C.M.; Rogers, N.B.; Podolnick, J.M.; Sakhuja, S.; Matusczcak, M.; Austin, M.T.; Kao, L.S.; Lally, K.P.; Tsao, K. Adherence to surgical antibiotic prophylaxis remains a challenge despite multifaceted interventions. Surgery 2015, 158, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Nemeth, T.A.; Beilman, G.J.; Hamlin, C.L.; Chipman, J. Preoperative Verification of Timely Antimicrobial Prophylaxis Does Not Improve Compliance with Guidelines. Surg. Infect. 2010, 11, 387–391. [Google Scholar] [CrossRef]
- Tan, J.A.; Naik, V.N.; Lingard, L. Exploring obstacles to proper timing of prophylactic antibiotics for surgical site infections. Qual. Saf. Heal. Care 2006, 15, 32–38. [Google Scholar] [CrossRef]
- Nair, B.G.; Newman, S.-F.; Peterson, G.N.; Wu, W.-Y.; Schwid, H.A. Feedback Mechanisms Including Real-Time Electronic Alerts to Achieve Near 100% Timely Prophylactic Antibiotic Administration in Surgical Cases. Anesth. Analg. 2010, 111, 1293–1300. [Google Scholar] [CrossRef]
- Donà, D.; Luise, D.; La Pergola, E.; Montemezzo, G.; Frigo, A.C.; Lundin, R.; Zaoutis, T.E.; Gamba, P.; Giaquinto, C. Effects of an antimicrobial stewardship intervention on perioperative antibiotic prophylaxis in pediatrics. Antimicrob. Resist. Infect. Control. 2019, 8, 13. [Google Scholar] [CrossRef]
- Sandora, T.J.; Fung, M.; Melvin, P.; Graham, D.A.; Rangel, S.J. National Variability and Appropriateness of Surgical Antibiotic Prophylaxis in US Children’s Hospitals. JAMA Pediatr. 2016, 170, 570. [Google Scholar] [CrossRef] [PubMed]
- Gaufin, T.; Tobin, N.H.; Aldrovandi, G. The importance of the microbiome in pediatrics and pediatric infectious diseases. Curr. Opin. Pediatr. 2018, 30, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Hollister, E.B.; Riehle, K.; Luna, R.A.; Weidler, E.M.; Rubio-Gonzales, M.; Mistretta, T.-A.; Raza, S.; Doddapaneni, H.V.; Metcalf, G.A.; Muzny, N.M.; et al. Structure and function of the healthy pre-adolescent pediatric gut microbiome. Microbiome 2015, 3, 36. [Google Scholar] [CrossRef] [PubMed]
- Staude, B.; Oehmke, F.; Lauer, T.; Behnke, J.; Göpel, W.; Schloter, M.; Schulz, H.; Krauss-Etschmann, S.; Ehrhardt, H. The Microbiome and Preterm Birth: A Change in Paradigm with Profound Implications for Pathophysiologic Concepts and Novel Therapeutic Strategies. BioMed Res. Int. 2018, 2018, 1–12. [Google Scholar] [CrossRef]
- Kao, A.M.; Arnold, M.R.; Prasad, T.; Schulman, A.M. The impact of abnormal BMI on surgical complications after pediatric colorectal surgery. J. Pediatr. Surg. 2019, 54, 2300–2304. [Google Scholar] [CrossRef]

| Variable | Patient (N = 192) | Patient (%) | SSI (N = 12) | SSI (%) | p-value |
|---|---|---|---|---|---|
| Age (range) | 4.7 mo (0–17.7 yr) | 3.0 yr (1.8 mo−17.1 yr) | 0.009 | ||
| Male | 113 | 59 | 9 | 75 | 0.365 |
| Race | 0.0592 | ||||
| White | 128 | 67 | 5 | 42 | 0.058 |
| Black | 37 | 19 | 4 | 34 | 0.251 |
| Hispanic | 18 | 9 | 2 | 17 | 0.312 |
| Asian | 2 | 1 | 1 | 8 | 0.121 |
| Other | 7 | 4 | 0 | 0 | 1.000 |
| Co-morbidities/Exposures | |||||
| Proton Pump Inhibitor | 37 | 19 | 3 | 25 | 0.704 |
| Hyperglycemia | 37 | 19 | 5 | 42 | 0.042 |
| Immunocompromised | 14 | 7 | 1 | 8 | 1.000 |
| Steroids | 19 | 10 | 2 | 17 | 0.337 |
| Prematurity | 90 | 47 | 3 | 25 | 0.143 |
| Obese (BMI >30) | 7 | 4 | 2 | 17 | 0.063 |
| Beta-Lactam Allergy Reported | 10 | 5 | 1 | 8 | 0.484 |
| Previous hospitalizations within the year | 62 | 32 | 5 | 42 | 0.473 |
| Median Duration of Surgical Hospitalization | 13 (1–511) days | 19 (3–92) days | 0.526 | ||
| Median Surgery Duration (range) | 92 (20–579) min | 112.5 (76–206) min | 0.037 | ||
| Urgency | <0.001 | ||||
| Elective | 175 | 91 | 7 | 58 | <0.001 |
| Emergent | 17 | 9 | 5 | 42 | <0.001 |
| Surgery Type | |||||
| Appendectomy | 11 | 6 | 0 | 0 | 1.000 |
| Small Bowel Resection | 33 | 17 | 5 | 42 | 0.020 |
| Colon/Rectal resection | 84 | 44 | 8 | 67 | 0.134 |
| Chait Cecostomy | 7 | 4 | 0 | 0 | 1.000 |
| Soave | 5 | 3 | 0 | 0 | 1.000 |
| Duodenal atresia repair | 16 | 8 | 0 | 0 | 0.604 |
| Ostomy formation/revision | 67 | 35 | 4 | 33 | 1.000 |
| Ostomy closure | 66 | 34 | 3 | 25 | 0.550 |
| Exploratory laparotomy | 54 | 28 | 8 | 67 | 0.005 |
| Gastrostomy tube placement/Revision | 14 | 7 | 1 | 8 | 1.000 |
| Other | 43 | 22 | 3 | 25 | 0.733 |
| Wound Classification | 0.0005 | ||||
| Clean-contaminated | 130 | 68 | 3 | 25 | 0.002 |
| Contaminated | 33 | 17 | 2 | 17 | 1.000 |
| Dirty | 29 | 15 | 7 | 58 | 0.000016 |
| ASA Class | 0.549 | ||||
| I | 8 | 4 | 1 | 8 | 0.409 |
| II | 80 | 42 | 5 | 42 | 1.000 |
| III | 84 | 44 | 6 | 50 | 0.652 |
| IV | 20 | 10 | 0 | 0 | 0.618 |
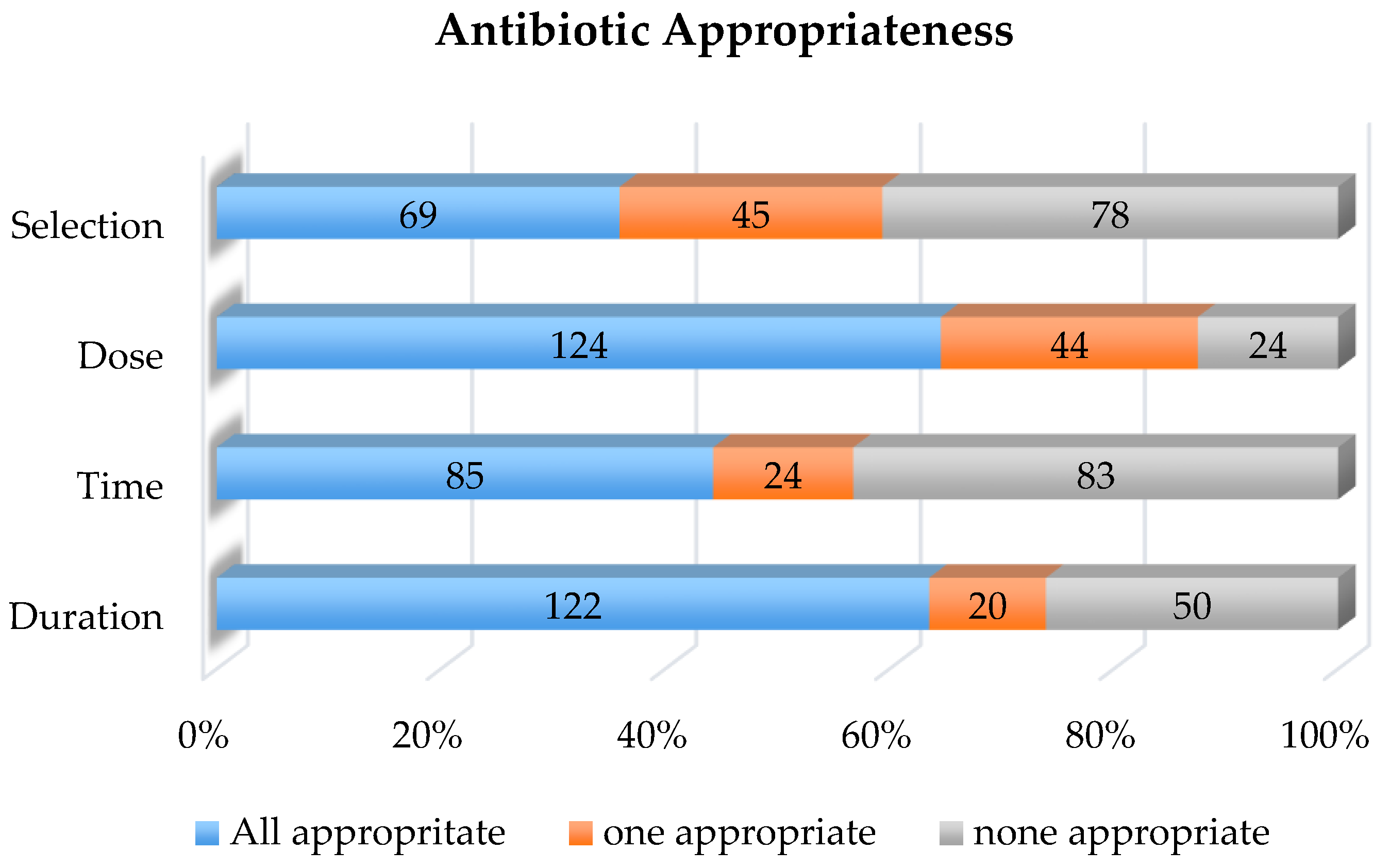
| Appropriate | Inappropriate | SSI Appropriate | SSI Inappropriate | |
|---|---|---|---|---|
| N = 192 (%) | N = 192 (%) | N = 12 (%) | N = 12(%) | |
| Antibiotic Selection | 69 (36) | 123 (64) | 8 (67) | 4 (33) |
| Antibiotic Dose | 124 (65) | 68 (35) | 6 (50) | 6 (50) |
| Antibiotic Timing | 85 (44) | 107 (56) | 7 (58) | 5 (42) |
| Antibiotic Duration | 122 (64) | 70 (36) | 10 (83) | 2 (17) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pough, K.; Bhakta, R.; Maples, H.; Honeycutt, M.; Vijayan, V. Evaluation of Pediatric Surgical Site Infections Associated with Colorectal Surgeries at an Academic Children’s Hospital. Healthcare 2020, 8, 91. https://doi.org/10.3390/healthcare8020091
Pough K, Bhakta R, Maples H, Honeycutt M, Vijayan V. Evaluation of Pediatric Surgical Site Infections Associated with Colorectal Surgeries at an Academic Children’s Hospital. Healthcare. 2020; 8(2):91. https://doi.org/10.3390/healthcare8020091
Chicago/Turabian StylePough, Kimberly, Rima Bhakta, Holly Maples, Michele Honeycutt, and Vini Vijayan. 2020. "Evaluation of Pediatric Surgical Site Infections Associated with Colorectal Surgeries at an Academic Children’s Hospital" Healthcare 8, no. 2: 91. https://doi.org/10.3390/healthcare8020091
APA StylePough, K., Bhakta, R., Maples, H., Honeycutt, M., & Vijayan, V. (2020). Evaluation of Pediatric Surgical Site Infections Associated with Colorectal Surgeries at an Academic Children’s Hospital. Healthcare, 8(2), 91. https://doi.org/10.3390/healthcare8020091




