Age-Standardized Breast Cancer Detection Rates of Breast Cancer Screening Program by Age Group in Korea; Comparison with Age-Standardized Incidence Rates from the Korea Central Cancer Registry
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Study Design
2.2. Study Subjects
2.3. Variables
2.4. Indicators
2.4.1. Participation Rate of Screening for Breast Cancer
2.4.2. Positivity Rate of Screening for Breast Cancer
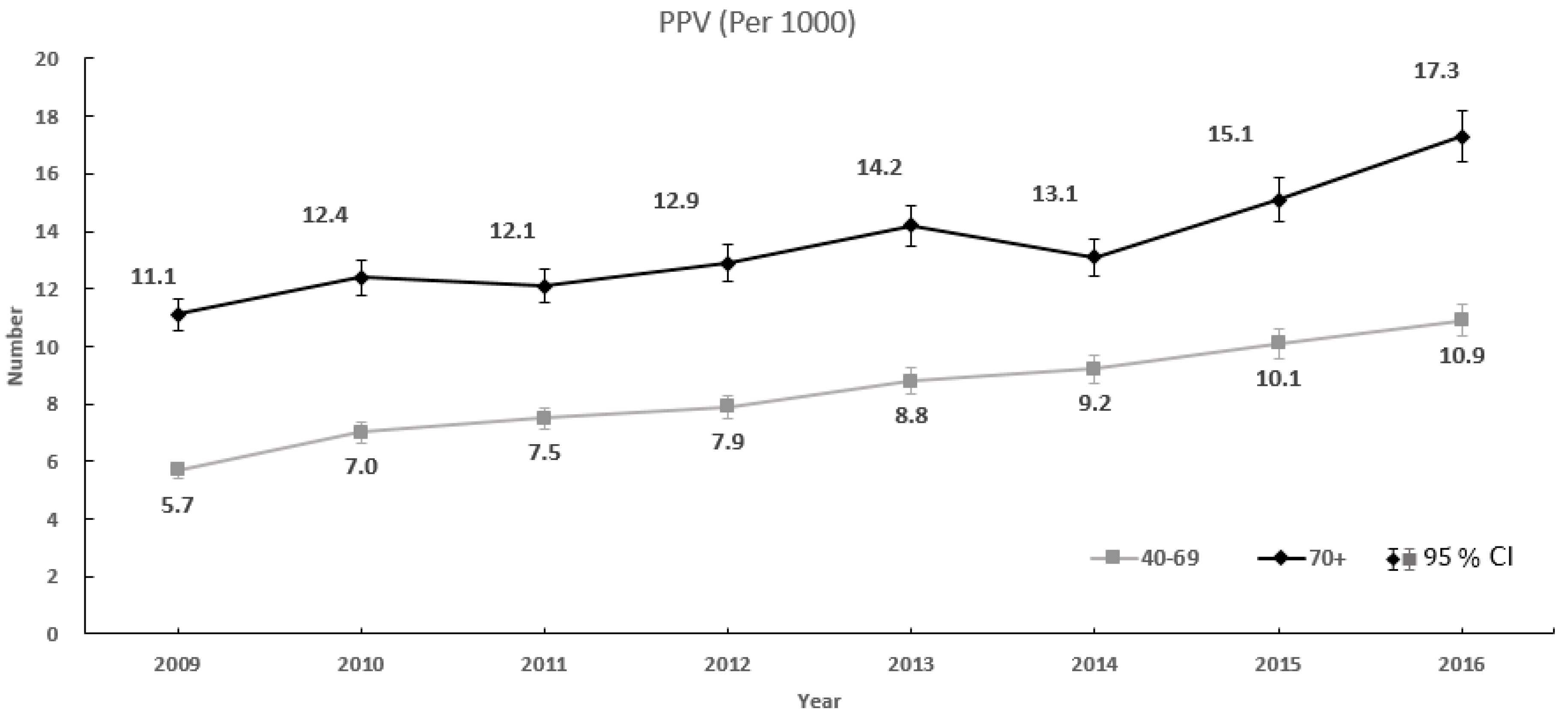
2.4.3. PPV of Screening for Breast Cancer
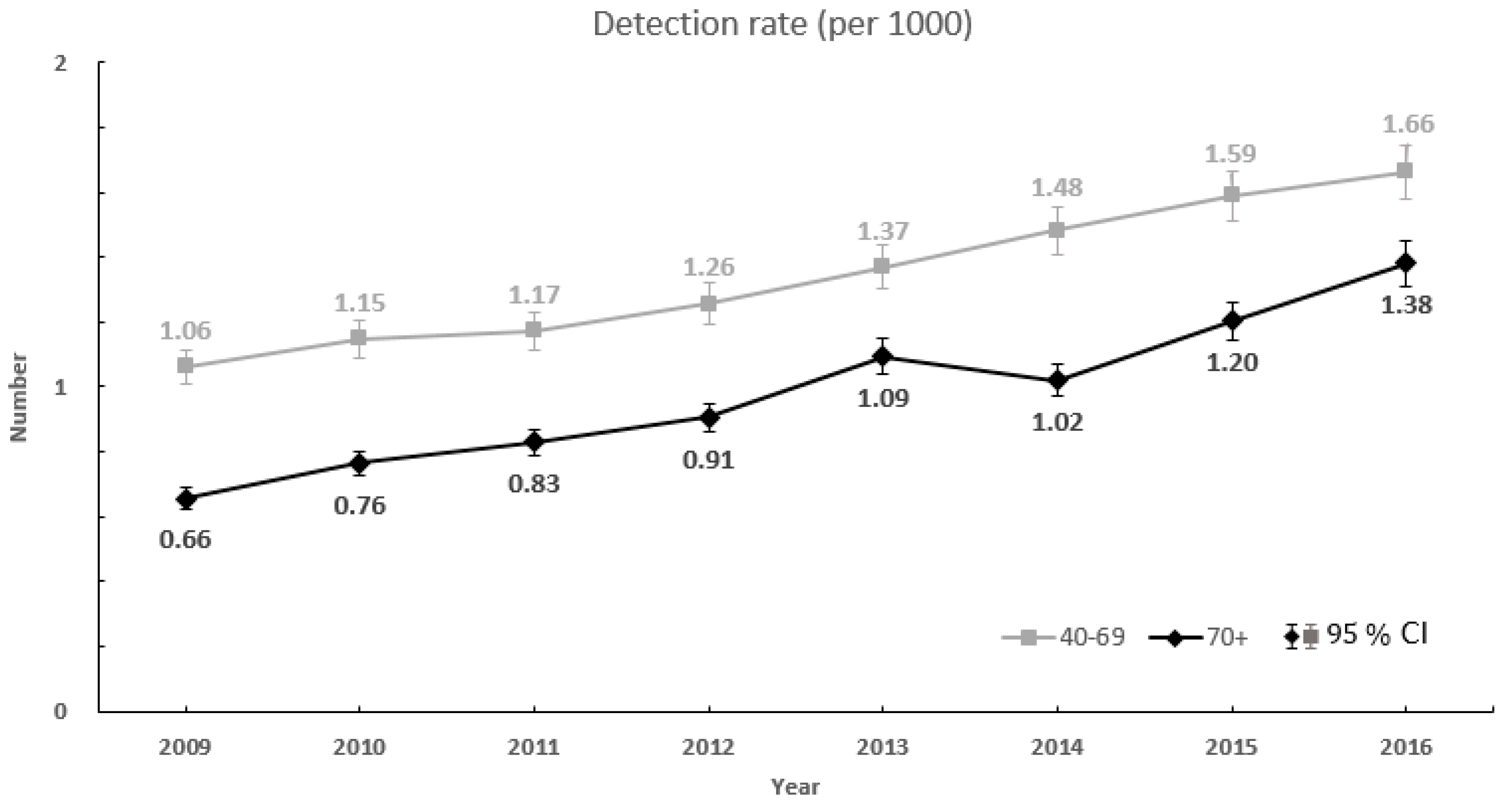
2.4.4. Detection Rate of Screening for Breast Cancer
2.5. Statistical Analyses
2.6. Ethics Statement
3. Results
3.1. Subjects and Participants; and Rates of Participation, Positivity
3.2. PPV and Detection Rate
3.3. Comparison Age-Standardized Detection Rate with Age-Standardized Incidence Rate
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Park, S.K. Epidemiological characteristics of breast cancer in Koreans. J. Korean. Med. Assoc. 2019, 62, 424–436. [Google Scholar] [CrossRef]
- National Cancer Information Center, Ministry of Health and Welfare. Available online: https://www.cancer.go.kr/lay1/S1T639C643/contents.do (accessed on 25 October 2018).
- Ministry of Health and Welfare. Cancer Registration Statistics. Available online: http://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=DT_117N_A00022&vw_cd=MT_ZTITLE&list_id=101_11744&seqNo=&lang_mode=ko&language=kor&obj_var_id=&itm_id=&conn_path=MT_ZTITLE (accessed on 22 January 2020).
- Ministry of Health and Welfare. Cancer Registration Statistics. Available online: http://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=DT_117N_A00023&conn_path=I2 (accessed on 25 October 2018).
- Cancer Facts & Figures 2017. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf (accessed on 25 October 2018).
- Lee, J.H.; Yim, S.H.; Won, Y.J.; Jung, K.W.; Son, B.H.; Lee, H.D.; Lee, E.S.; Yoo, K.Y.; Ahn, S.H.; Shin, H.R. Population-based breast cancer statistics in Korea during 1993–2002: Incidence, mortality, and survival. J. Korean Med. Sci. 2007, 22, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.S.; Chang, H.S.; Lee, S.M.; Park, E.C. Economic burden of cancer in Korea during 2000–2010. Cancer Res. Treat. 2015, 47, 387–398. [Google Scholar] [CrossRef]
- Lee, E.H.; Park, B.; Kim, N.S.; Seo, H.J.; Ko, K.L.; Min, J.W.; Shin, M.H.; Lee, K.; Lee, S.; Choi, N.; et al. The Korean guideline for breast cancer screening. J. Korean Med. Assoc. 2015, 58, 408–419. [Google Scholar] [CrossRef]
- Smith, R.A. The value of modern mammography screening in the control of breast cancer: Understanding the underpinnings of the current debates. Cancer Epidemiol. Biomarkers Prev. 2014, 23, 1139–1146. [Google Scholar] [CrossRef][Green Version]
- Pace, L.E.; Keating, N.L. A systematic assessment of benefits and risks to guide breast cancer screening decisions. JAMA 2014, 311, 1327–1335. [Google Scholar] [CrossRef]
- Shah, T.A.; Guraya, S.S. Breast cancer screening programs: Review of merits, demerits, and recent recommendations practiced across the world. J. Microsc. Ultrastruct. 2017, 5, 59–69. [Google Scholar] [CrossRef]
- U.S. Preventive Services Task Force. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann. Intern. Med. 2016, 164, 279–296. [Google Scholar] [CrossRef]
- Tonelli, M.; Connor, G.S.; Joffres, M.; Dickinson, J.; Singh, H.; Lewin, G.; Birtwhistle, R.; Fitzpatrick-Lewis, D.; Hodgson, N.; Ciliska, D.; et al. Recommendations on screening for breast cancer in average-risk women aged 40–74 years. Can. Med. Assoc. J. 2011, 183, 2147. [Google Scholar] [CrossRef]
- Hamashima, C.C.; Hattori, M.; Honjo, S.; Kasahara, Y.; Katayama, T.; Nakai, M.; Nakayama, T.; Morita, T.; Ohta, K.; Ohnuki, K.; et al. The Japanese Guidelines for Breast Cancer Screening. Jpn. J. Clin. Oncol. 2016, 46, 482–492. [Google Scholar] [CrossRef] [PubMed]
- Evaluation of the Validity of Current National Health Screening Program and Plan to Improve the System. Available online: https://www.scienceopen.com/document?vid=d0b8c597-fce9-49cc-8084-da4a94358dd2 (accessed on 11 May 2020).
- Lee, K.; Kim, H.; Lee, J.H.; Jeong, H.; Shin, S.A.; Han, T.; Seo, Y.L.; Yoo, Y.; Nam, S.E.; Park, J.H.; et al. Retrospective observation on contribution and limitations of screening for breast cancer with mammography in Korea: Detection rate of breast cancer and incidence rate of interval cancer of the breast. BMC Women’s Health 2016, 16, 72. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Jeong, S.H.; Kim, J.; Jung, S.H.; Song, K.B.; Nam, C.M. Scheduling mammography screening for the early detection of breast cancer in Korean women. J. Med. Screen. 2007, 14, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Michielutte, R.; Sharp, P.C.; Foley, K.L.; Cunningham, L.E.; Spangler, J.G.; Paskett, E.D.; Case, L.D. Intervention to increase screening mammography among women 65 and older, Health Education Research. Health Educ. Res. 2005, 20, 149–162. [Google Scholar] [CrossRef][Green Version]
- Jung, K.W.; Won, Y.J.; Kong, H.J.; Lee, E.S.; Community of Population-Based Regional Cancer Registries. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2015. Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2018, 50, 303–316. [Google Scholar] [CrossRef]
- Domingo, L.; Hofvind, S.; Hubbard, R.A.; Román, M.; Benkeser, D.; Sala, M.; Castells, X. Cross-national comparison of screening mammography accuracy measures in U.S., Norway, and Spain. Eur. Radiol. 2016, 26, 2520–2528. [Google Scholar] [CrossRef]
- Lehman, C.; White, E.; Peacock, S.; Drucker, M.; Urban, N. Effect of age and breast density on screening mammograms with false-positive findings. AJR Am. J. Roentgenol. 1999, 173, 1651–1655. [Google Scholar] [CrossRef]
- Checka, C.M.; Chun, J.E.; Schnabel, F.R.; Lee, J.; Toth, H. The Relationship of Mammographic Density and Age: Implications for Breast Cancer Screening. AJR Am. J. Roentgenol. 2012, 198, W292–W295. [Google Scholar] [CrossRef]
- Rafia, R.; Brennan, A.; Madan, J.; Collins, K.; Reed, M.W.; Lawrence, G.; Robinson, T.; Greenberg, D.; Wyld, L. Modeling the Cost-Effectiveness of Alternative Upper Age Limits for Breast Cancer Screening in England and Wales. Value Health 2016, 19, 404–412. [Google Scholar] [CrossRef]
- Cindy, S.L.; Linda, M.; Bonnie, N.J.; Edward, A.S.; Bethany, L.N. Screening for Breast Cancer in Women Age 75 Years and Older. AJR Am. J. Roentgenol. 2018, 210, 256–263. [Google Scholar] [CrossRef]
- Ng, Z.X.; Ong, M.S.; Jegadeesan, T.; Deng, S.; Yap, C.T. Breast Cancer: Exploring the Facts and Holistic Needs during and beyond Treatment. Healthcare 2017, 5, 26. [Google Scholar] [CrossRef] [PubMed]

| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | ||
|---|---|---|---|---|---|---|---|---|---|
| Subjects for Screening | 40–69 | 4,963,914 | 4,482,903 | 5,171,907 | 4,563,574 | 4,713,451 | 4,765,409 | 4,945,719 | 5,072,341 |
| ≥70 | 948,517 | 918,220 | 1,129,966 | 1,012,101 | 1,049,574 | 1,083,725 | 1,111,346 | 1,175,298 | |
| Total | 5,912,431 | 5,401,123 | 6,301,873 | 5,575,675 | 5,763,025 | 5,849,134 | 6,057,065 | 6,247,639 | |
| Participants | 40–69 | 2,597,693 | 2,525,167 | 2,909,618 | 2,858,449 | 2,918,093 | 3,031,223 | 3,222,881 | 3,432,426 |
| ≥70 | 377,662 | 381,887 | 458,570 | 483,923 | 497,824 | 538,924 | 551,969 | 606,112 | |
| Total | 2,975,355 | 2,907,054 | 3,368,188 | 3,342,372 | 3,415,917 | 3,570,147 | 3,774,850 | 4,038,538 | |
| Participation Rate (%) | 40–69 | 52.3 | 56.3 | 56.3 | 62.6 | 61.9 | 63.6 | 65.2 | 67.7 |
| ≥70 | 39.8 | 41.6 | 40.6 | 47.8 | 47.4 | 49.7 | 49.7 | 51.6 | |
| Total | 50.3 | 53.8 | 53.4 | 59.9 | 59.3 | 61 | 62.3 | 64.6 | |
| Positivity Rate (%) | 40–69 | 18.7 | 16.3 | 15.7 | 15.9 | 15.6 | 16.1 | 15.7 | 15.2 |
| ≥70 | 5.9 | 6.2 | 6.8 | 7.0 | 7.7 | 7.8 | 8.0 | 8.0 | |
| Total | 17.0 | 15.0 | 14.5 | 14.6 | 14.5 | 14.9 | 14.6 | 14.2 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.; Kim, H.; Choi, H.; Son, M.; Lee, K.-S.; Han, T.-H.; Kim, S. Age-Standardized Breast Cancer Detection Rates of Breast Cancer Screening Program by Age Group in Korea; Comparison with Age-Standardized Incidence Rates from the Korea Central Cancer Registry. Healthcare 2020, 8, 132. https://doi.org/10.3390/healthcare8020132
Kim M, Kim H, Choi H, Son M, Lee K-S, Han T-H, Kim S. Age-Standardized Breast Cancer Detection Rates of Breast Cancer Screening Program by Age Group in Korea; Comparison with Age-Standardized Incidence Rates from the Korea Central Cancer Registry. Healthcare. 2020; 8(2):132. https://doi.org/10.3390/healthcare8020132
Chicago/Turabian StyleKim, Miye, Hyeongsu Kim, Heejung Choi, MiSeon Son, Kun-Sei Lee, Tae-Hwa Han, and Sollip Kim. 2020. "Age-Standardized Breast Cancer Detection Rates of Breast Cancer Screening Program by Age Group in Korea; Comparison with Age-Standardized Incidence Rates from the Korea Central Cancer Registry" Healthcare 8, no. 2: 132. https://doi.org/10.3390/healthcare8020132
APA StyleKim, M., Kim, H., Choi, H., Son, M., Lee, K.-S., Han, T.-H., & Kim, S. (2020). Age-Standardized Breast Cancer Detection Rates of Breast Cancer Screening Program by Age Group in Korea; Comparison with Age-Standardized Incidence Rates from the Korea Central Cancer Registry. Healthcare, 8(2), 132. https://doi.org/10.3390/healthcare8020132






