Impact of Self-Reported Sitting Time and Transtheoretical Model Based on Exercise Behavior Change on Glycemic and Weight Control in Japanese Adults with Type 1 Diabetes: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
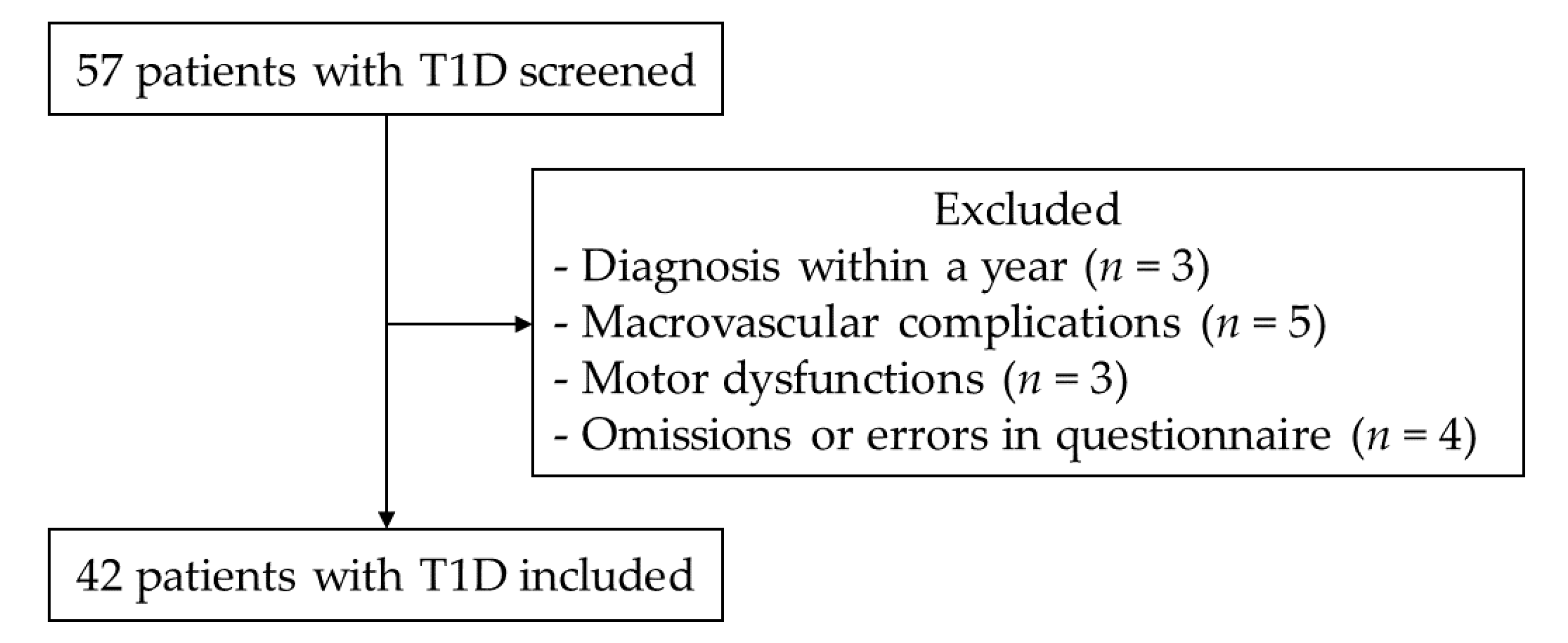
2.2. Participants
2.3. Measurements
2.4. Statistical Analysis
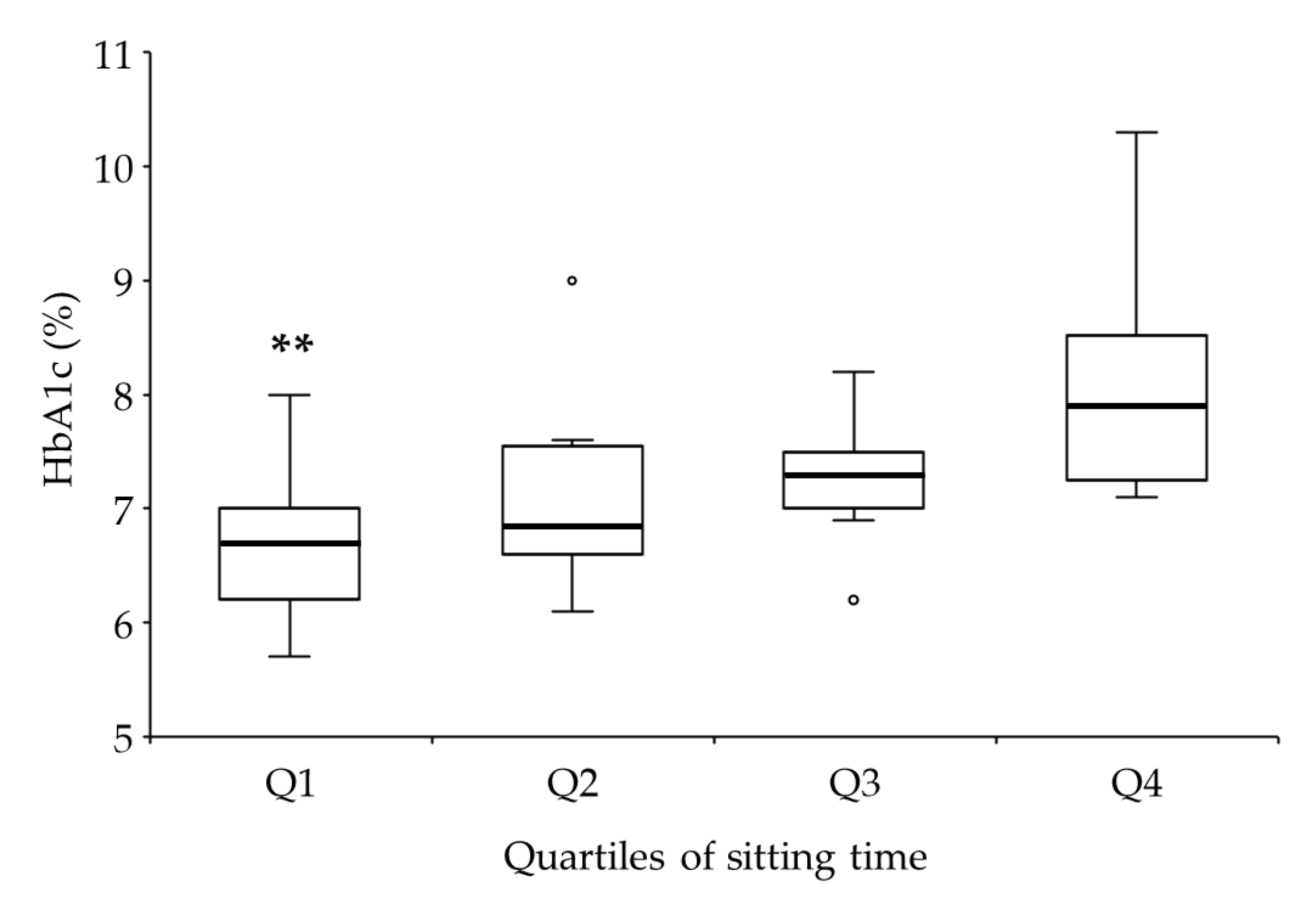
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar] [CrossRef]
- Barone Gibbs, B.; Pettee Gabriel, K.; Reis, J.P.; Jakicic, J.M.; Carnethon, M.R.; Sternfeld, B. Cross-sectional and longitudinal associations between objectively measured sedentary time and metabolic disease: The Coronary Artery Risk Development in Young Adults (CARDIA) study. Diabetes Care 2015, 38, 1835–1843. [Google Scholar] [CrossRef]
- Van der Ploeg, H.P.; Chey, T.; Korda, R.J.; Banks, E.; Bauman, A. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch. Intern. Med. 2012, 172, 494–500. [Google Scholar] [CrossRef]
- Mikus, C.R.; Oberlin, D.J.; Libla, J.L.; Taylor, A.M.; Booth, F.W.; Thyfault, J.P. Lowering physical activity impairs glycemic control in healthy volunteers. Med. Sci. Sports Exerc. 2012, 44, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B.; Leitzmann, M.F.; Stampfer, M.J.; Colditz, G.A.; Willett, W.C.; Rimm, E.B. Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Arch. Intern. Med. 2001, 161, 1542–1548. [Google Scholar] [CrossRef] [PubMed]
- Sardinha, L.B.; Magalhaes, J.P.; Santos, D.A.; Judice, P.B. Sedentary Patterns, Physical Activity, and Cardiorespiratory Fitness in Association to Glycemic Control in Type 2 Diabetes Patients. Front. Physiol. 2017, 8, 262. [Google Scholar] [CrossRef] [PubMed]
- Bohn, B.; Herbst, A.; Pfeifer, M.; Krakow, D.; Zimny, S.; Kopp, F.; Melmer, A.; Steinacker, J.M.; Holl, R.W. Impact of Physical Activity on Glycemic Control and Prevalence of Cardiovascular Risk Factors in Adults With Type 1 Diabetes: A Cross-sectional Multicenter Study of 18,028 Patients. Diabetes Care 2015, 38, 1536–1543. [Google Scholar] [CrossRef]
- MacMillan, F.; Kirk, A.; Mutrie, N.; Matthews, L.; Robertson, K.; Saunders, D.H. A systematic review of physical activity and sedentary behavior intervention studies in youth with type 1 diabetes: Study characteristics, intervention design, and efficacy. Pediatr. Diabetes 2014, 15, 175–189. [Google Scholar] [CrossRef]
- Miculis, C.P.; De Campos, W.; da Silva Boguszweski, M.C. Correlation between glycemic control and physical activity level in adolescents and children with type 1 diabetes. J. Phys. Act. Health 2015, 12, 232–237. [Google Scholar] [CrossRef]
- Galler, A.; Lindau, M.; Ernert, A.; Thalemann, R.; Raile, K. Associations between media consumption habits, physical activity, socioeconomic status, and glycemic control in children, adolescents, and young adults with type 1 diabetes. Diabetes Care 2011, 34, 2356–2359. [Google Scholar] [CrossRef]
- Ligtenberg, P.C.; Blans, M.; Hoekstra, J.B.; van der Tweel, I.; Erkelens, D.W. No effect of long-term physical activity on the glycemic control in type 1 diabetes patients: A cross-sectional study. Neth. J. Med. 1999, 55, 59–63. [Google Scholar] [CrossRef]
- American Diabetes Association. 5. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020, 43, S48–S65. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, A.; Nishimura, R.; Tajima, N. Trends in the Epidemiology of Patients with Diabetes in Japan. JMAJ 2010, 53, 36–40. [Google Scholar]
- Shojaeian, A.; Mehri-Ghahfarrokhi, A. An overview of the Epidemiology of Type 1 Diabetes Mellitus. Int. J. Metab. Syndr. 2018, 2, 1–4. [Google Scholar]
- Snouffer, E. An inexplicable upsurge: The rise in type 1 diabetes. Diabetes Res. Clin. Pract. 2018, 137, 242–244. [Google Scholar] [CrossRef]
- Bandura, A.; Adams, N.E. Analysis of Self-Efficacy Theory of Behavioral Change. Cognit. Ther. Res. 1977, 1, 287–310. [Google Scholar] [CrossRef]
- Selcuk-Tosun, A.; Zincir, H. The effect of a transtheoretical model-based motivational interview on self-efficacy, metabolic control, and health behaviour in adults with type 2 diabetes mellitus: A randomized controlled trial. Int. J. Nurs. Pract. 2019, 25, e12742. [Google Scholar] [CrossRef]
- Wakui, S.; Shimomitsu, T.; Odagiri, Y.; Inoue, S.; Takamiya, T.; Ohya, Y. Relation of the stages of change for exercise behaviors, self-efficacy, decisional-balance, and diet-related psycho-behavioral factors in young Japanese women. J. Sports Med. Phys. Fit. 2002, 42, 224–232. [Google Scholar]
- Selcuk-Tosun, A.; Zincir, H. The Effect on Health Outcomes of Post-Intervention Transtheoretical Model-Based Motivational Interview in Adults with Type 2 Diabetes Mellitus: Follow up a Cross-Sectional Study. J. Caring Sci. 2019, 8, 1–8. [Google Scholar] [CrossRef]
- Tseng, H.M.; Liao, S.F.; Wen, Y.P.; Chuang, Y.J. Stages of change concept of the transtheoretical model for healthy eating links health literacy and diabetes knowledge to glycemic control in people with type 2 diabetes. Prim. Care Diabetes 2017, 11, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Van Poppel, M.N.; Chinapaw, M.J.; Mokkink, L.B.; van Mechelen, W.; Terwee, C.B. Physical activity questionnaires for adults: A systematic review of measurement properties. Sports Med. 2010, 40, 565–600. [Google Scholar] [CrossRef]
- Murano, I.; Asakawa, Y.; Mizukami, M.; Takihara, J. Examination of the Validity of the Japanese Version of the IPA Questionnaire for the Evaluation of the Physical Activity of Diabetes Patients (in Japanese). Rigakuryoho Kagaku 2013, 28, 101–104. [Google Scholar] [CrossRef][Green Version]
- Prochaska, J.O.; DiClemente, C.C. Stages and processes of self-change of smoking: Toward an integrative model of change. J. Consult. Clin. Psychol. 1983, 51, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Oka, K. Reliability and validity of the stages of change for exercise behavior scale among middle-aged adults. Jpn. J. Health Promot. 2003, 5, 15–22. [Google Scholar]
- Oka, K.; Takenaka, K.; Miyazaki, Y. Assessing the stages of change for exercise behavior among young adults: The relationship with self-reported physical activity and exercise behavior. Jpn. Health Psychol. 2000, 8, 17–23. [Google Scholar]
- Araki, E.; Haneda, M.; Kasuga, M.; Nishikawa, T.; Kondo, T.; Ueki, K.; Kadowaki, T. New glycemic targets for patients with diabetes from the Japan Diabetes Society. J. Diabetes Investig. 2017, 8, 123–125. [Google Scholar] [CrossRef]
- Li, J.; Chattopadhyay, K.; Xu, M.; Chen, Y.; Hu, F.; Chu, J.; Li, L. Glycaemic control in type 2 diabetes patients and its predictors: A retrospective database study at a tertiary care diabetes centre in Ningbo, China. BMJ Open 2018, 8, e019697. [Google Scholar] [CrossRef]
- Dempsey, P.C.; Larsen, R.N.; Sethi, P.; Sacre, J.W.; Straznicky, N.E.; Cohen, N.D.; Cerin, E.; Lambert, G.W.; Owen, N.; Kingwell, B.A.; et al. Benefits for Type 2 Diabetes of Interrupting Prolonged Sitting With Brief Bouts of Light Walking or Simple Resistance Activities. Diabetes Care 2016, 39, 964–972. [Google Scholar] [CrossRef]
- Dunstan, D.W.; Kingwell, B.A.; Larsen, R.; Healy, G.N.; Cerin, E.; Hamilton, M.T.; Shaw, J.E.; Bertovic, D.A.; Zimmet, P.Z.; Salmon, J.; et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care 2012, 35, 976–983. [Google Scholar] [CrossRef] [PubMed]
- Peddie, M.C.; Bone, J.L.; Rehrer, N.J.; Skeaff, C.M.; Gray, A.R.; Perry, T.L. Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: A randomized crossover trial. Am. J. Clin. Nutr. 2013, 98, 358–366. [Google Scholar] [CrossRef]
- Hamilton, M.T.; Hamilton, D.G.; Zderic, T.W. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes 2007, 56, 2655–2667. [Google Scholar] [CrossRef] [PubMed]
- Basu, R.; Johnson, M.L.; Kudva, Y.C.; Basu, A. Exercise, hypoglycemia, and type 1 diabetes. Diabetes Technol. Ther. 2014, 16, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016, 39, 2065–2079. [Google Scholar] [CrossRef] [PubMed]
- Chimen, M.; Kennedy, A.; Nirantharakumar, K.; Pang, T.T.; Andrews, R.; Narendran, P. What are the health benefits of physical activity in type 1 diabetes mellitus? A literature review. Diabetologia 2012, 55, 542–551. [Google Scholar] [CrossRef] [PubMed]
- Balducci, S.; Sacchetti, M.; Orlando, G.; Salvi, L.; Pugliese, L.; Salerno, G.; D’Errico, V.; Iacobini, C.; Conti, F.G.; Zanuso, S.; et al. Correlates of muscle strength in diabetes: The study on the assessment of determinants of muscle and bone strength abnormalities in diabetes (SAMBA). Nutr. Metab. Cardiovasc. Dis. 2014, 24, 18–26. [Google Scholar] [CrossRef]
- Bauman, A.; Ainsworth, B.E.; Sallis, J.F.; Hagstromer, M.; Craig, C.L.; Bull, F.C.; Pratt, M.; Venugopal, K.; Chau, J.; Sjostrom, M.; et al. The descriptive epidemiology of sitting. A 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am. J. Prev. Med. 2011, 41, 228–235. [Google Scholar] [CrossRef]
- Nakanishi, S.; Hirukawa, H.; Shimoda, M.; Tatsumi, F.; Kohara, K.; Obata, A.; Okauchi, S.; Katakura, Y.; Sanada, J.; Fushimi, Y.; et al. Impact of physical activity and sedentary time on glycated hemoglobin levels and body composition: Cross-sectional study using outpatient clinical data of Japanese patients with type 2 diabetes. J. Diabetes Investig. 2019. [Google Scholar] [CrossRef]
- American Diabetes Association. 6. Glycemic Targets: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020, 43, S66–S76. [Google Scholar] [CrossRef]
- Cleland, C.; Ferguson, S.; Ellis, G.; Hunter, R.F. Validity of the International Physical Activity Questionnaire (IPAQ) for assessing moderate-to-vigorous physical activity and sedentary behaviour of older adults in the United Kingdom. BMC Med. Res. Methodol. 2018, 18, 176. [Google Scholar] [CrossRef] [PubMed]
- Brazeau, A.S.; Rabasa-Lhoret, R.; Strychar, I.; Mircescu, H. Barriers to physical activity among patients with type 1 diabetes. Diabetes Care 2008, 31, 2108–2109. [Google Scholar] [CrossRef]
- Lascar, N.; Kennedy, A.; Hancock, B.; Jenkins, D.; Andrews, R.C.; Greenfield, S.; Narendran, P. Attitudes and barriers to exercise in adults with type 1 diabetes (T1DM) and how best to address them: A qualitative study. PLoS ONE 2014, 9, e108019. [Google Scholar] [CrossRef] [PubMed]
- Yardley, J.; Mollard, R.; MacIntosh, A.; MacMillan, F.; Wicklow, B.; Berard, L.; Hurd, C.; Marks, S.; McGavock, J. Vigorous intensity exercise for glycemic control in patients with type 1 diabetes. Can. J. Diabetes 2013, 37, 427–432. [Google Scholar] [CrossRef]
- Yardley, J.E.; Kenny, G.P.; Perkins, B.A.; Riddell, M.C.; Balaa, N.; Malcolm, J.; Boulay, P.; Khandwala, F.; Sigal, R.J. Resistance versus aerobic exercise: Acute effects on glycemia in type 1 diabetes. Diabetes Care 2013, 36, 537–542. [Google Scholar] [CrossRef]
- Colberg, S.R.; Laan, R.; Dassau, E.; Kerr, D. Physical activity and type 1 diabetes: Time for a rewire? J. Diabetes Sci. Technol. 2015, 9, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Spencer, L.; Adams, T.B.; Malone, S.; Roy, L.; Yost, E. Applying the transtheoretical model to exercise: A systematic and comprehensive review of the literature. Health Promot. Pract. 2006, 7, 428–443. [Google Scholar] [CrossRef] [PubMed]
- Tappy, L.; Binnert, C.; Schneiter, P. Energy expenditure, physical activity and body-weight control. Proc. Nutr. Soc. 2003, 62, 663–666. [Google Scholar] [CrossRef] [PubMed]
- Holmen, H.; Wahl, A.; Torbjornsen, A.; Jenum, A.K.; Smastuen, M.C.; Ribu, L. Stages of change for physical activity and dietary habits in persons with type 2 diabetes included in a mobile health intervention: The Norwegian study in RENEWING HEALTH. BMJ Open Diabetes Res. Care 2016, 4, e000193. [Google Scholar] [CrossRef]
- Chau, J.Y.; Grunseit, A.C.; Chey, T.; Stamatakis, E.; Brown, W.J.; Matthews, C.E.; Bauman, A.E.; van der Ploeg, H.P. Daily sitting time and all-cause mortality: A meta-analysis. PLoS ONE 2013, 8, e80000. [Google Scholar] [CrossRef]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.M.; Lancet Physical Activity Series 2 Executive Committe; Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef]
- Suliga, E.; Ciesla, E.; Rebak, D.; Koziel, D.; Gluszek, S. Relationship between Sitting Time, Physical Activity, and Metabolic Syndrome among Adults Depending on Body Mass Index (BMI). Med. Sci. Monit. 2018, 24, 7633–7645. [Google Scholar] [CrossRef] [PubMed]
- Virtuoso Junior, J.S.; Roza, L.B.; Tribess, S.; Meneguci, J.; Mendes, E.L.; Pegorari, M.S.; Dias, F.A.; Dos Santos Tavares, D.M.; Sasaki, J.E. Time Spent Sitting Is Associated with Changes in Biomarkers of Frailty in Hospitalized Older Adults: A Cross Sectional Study. Front. Physiol. 2017, 8, 505. [Google Scholar] [CrossRef]
- Hashemzadeh, M.; Rahimi, A.; Zare-Farashbandi, F.; Alavi-Naeini, A.M.; Daei, A. Transtheoretical Model of Health Behavioral Change: A Systematic Review. Iran. J. Nurs. Midwifery Res. 2019, 24, 83–90. [Google Scholar] [CrossRef]
- Columb, M.; Atkinson, M. Statistical analysis: Sample size and power estimations. BJA Educ. 2015, 16, 159–161. [Google Scholar] [CrossRef]
- Waden, J.; Forsblom, C.; Thorn, L.M.; Saraheimo, M.; Rosengard-Barlund, M.; Heikkila, O.; Lakka, T.A.; Tikkanen, H.; Groop, P.H.; FinnDiane Study Group. Physical activity and diabetes complications in patients with type 1 diabetes: The Finnish Diabetic Nephropathy (FinnDiane) Study. Diabetes Care 2008, 31, 230–232. [Google Scholar] [CrossRef] [PubMed]
- Prince, S.A.; Cardilli, L.; Reed, J.L.; Saunders, T.J.; Kite, C.; Douillette, K.; Fournier, K.; Buckley, J.P. A comparison of self-reported and device measured sedentary behaviour in adults: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 31. [Google Scholar] [CrossRef]
| Variables | Values |
|---|---|
| Male/Female (frequency) (percentage) | 14/28 (33.3/66.7) |
| Age (years) | 44.0 (33.3–56.8) |
| Duration of T1D (years) | 11.0 (3.1–18.8) |
| BMI (kg/m2) | 22.1 (20.9–23.2) |
| HbA1c (%) | 7.2 (6.7–7.8) |
| Sitting time (hours/day) | 6.0 (4.6–8.0) |
| Use of CSII (frequency) (percentage) | 11 (26.2) |
| Cigarette smoking (frequency) (percentage) | 10 (23.8) |
| Alcohol drinking (frequency) (percentage) | 18 (42.9) |
| Use of car (frequency) (percentage) | 21 (50.0) |
| Employed (frequency) (percentage) | 26 (61.9) |
| Living with family (frequency) (percentage) | 30 (71.4) |
| TTM based on exercise behavior change (frequency) (percentage) | |
| Precontemplation | 18 (42.9) |
| Contemplation | 3 (7.1) |
| Preparation | 6 (14.3) |
| Action | 1 (2.4) |
| Maintenance | 14 (33.3) |
| Variables | HbA1c | BMI | ||||
|---|---|---|---|---|---|---|
| r | p-Value | Power | r | p-Value | Power | |
| Gender | –0.20 | 0.21 | 0.25 | 0.14 | 0.39 | 0.14 |
| Age | 0.35 | 0.02 * | 0.64 | 0.23 | 0.14 | 0.31 |
| Duration of T1D | 0.22 | 0.16 | 0.29 | 0.39 | 0.01 * | 0.74 |
| BMI | 0.20 | 0.20 | 0.25 | - | - | - |
| HbA1c | - | - | - | 0.20 | 0.20 | 0.25 |
| Sitting time | 0.60 | <0.01 ** | 0.99 | <0.01 | 0.99 | 0.05 |
| Use of CSII | –0.30 | 0.05 | 0.50 | –0.07 | 0.65 | 0.07 |
| Cigarette smoking | –0.23 | 0.15 | 0.31 | 0.10 | 0.54 | 0.10 |
| Alcohol drinking | –0.27 | 0.08 | 0.42 | 0.03 | 0.83 | 0.05 |
| Use of car | –0.03 | 0.87 | 0.05 | –0.06 | 0.73 | 0.07 |
| Employed | –0.19 | 0.22 | 0.23 | 0.09 | 0.56 | 0.09 |
| Living with family | –0.27 | 0.08 | 0.42 | –0.06 | 0.72 | 0.07 |
| TTM | –0.26 | 0.09 | 0.39 | –0.40 | <0.01 ** | 0.76 |
| Variables | HbA1c | p-Value | Effect Size (r, Cramer’s V) | Power | |
|---|---|---|---|---|---|
| ≤7% (n = 16) | >7% (n = 26) | ||||
| Male/Female (frequency) (percentage) | 7/9 (43.8/56.2) | 7/19 (26.9/73.1) | 0.32 | 0.12 | 0.11 |
| Age (years) | 38.5 (33.8–47.5) | 45.5 (33.8–61.8) | 0.22 | 0.50 | 0.32 |
| Duration of T1D (years) | 6.0 (2.0–18.3) | 13.0 (5.5–18.8) | 0.17 | 0.22 | 0.10 |
| BMI (kg/m2) | 21.4 (20.0–23.0) | 22.8 (21.1–23.5) | 0.09 | 0.63 | 0.48 |
| Sitting time (hours/day) | 4.0 (3.0–5.5) | 7.3 (6.0–8.0) | <0.01 ** | 1.56 | 0.97 |
| Use of CSII (frequency) (percentage) | 6 (37.5) | 5 (19.2) | 0.28 | 0.15 | 0.15 |
| Cigarette smoking (frequency) (percentage) | 5 (31.3) | 5 (19.2) | 0.47 | 0.08 | 0.06 |
| Alcohol drinking (frequency) (percentage) | 9 (56.3) | 9 (34.6) | 0.21 | 0.16 | 0.17 |
| Use of car (frequency) (percentage) | 8 (50.0) | 13 (50.0) | 1.00 | 0.00 | 0.00 |
| Employed (frequency) (percentage) | 10 (62.5) | 16 (61.5) | 1.00 | 0.00 | 0.00 |
| Living with family (frequency) (percentage) | 13 (81.3) | 17 (65.4) | 0.32 | 0.12 | 0.08 |
| TTM based on exercise behavior change (frequency) (percentage) | 0.04 * | 0.46 | 0.69 | ||
| Precontemplation | 4 (25.0) | 14 (53.8) | |||
| Contemplation | 0 (0.0) | 3 (11.5) | |||
| Preparation | 3 (18.8) | 3 (11.5) | |||
| Action | 0 (0.0) | 1 (3.8) | |||
| Maintenance | 9 (56.3) | 5 (19.2) | |||
| Variables | Odds Ratio | 95% CI | p-Value | VIF |
|---|---|---|---|---|
| BMI (per 1-kg/m2 increase) | 1.52 | 0.86–2.69 | 0.15 | 1.18 |
| Sitting time (per 1-hour increase) | 3.53 | 1.54–8.11 | <0.01 ** | 1.55 |
| TTM based on exercise behavior change (per 1-stage increase) | 0.52 | 0.27–1.01 | 0.07 | 1.43 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Honda, H.; Igaki, M.; Tanaka, S.-i.; Ono, K.; Hirota, Y. Impact of Self-Reported Sitting Time and Transtheoretical Model Based on Exercise Behavior Change on Glycemic and Weight Control in Japanese Adults with Type 1 Diabetes: A Cross-Sectional Study. Healthcare 2020, 8, 105. https://doi.org/10.3390/healthcare8020105
Honda H, Igaki M, Tanaka S-i, Ono K, Hirota Y. Impact of Self-Reported Sitting Time and Transtheoretical Model Based on Exercise Behavior Change on Glycemic and Weight Control in Japanese Adults with Type 1 Diabetes: A Cross-Sectional Study. Healthcare. 2020; 8(2):105. https://doi.org/10.3390/healthcare8020105
Chicago/Turabian StyleHonda, Hiroto, Makoto Igaki, Shin-ichiro Tanaka, Kumiko Ono, and Yushi Hirota. 2020. "Impact of Self-Reported Sitting Time and Transtheoretical Model Based on Exercise Behavior Change on Glycemic and Weight Control in Japanese Adults with Type 1 Diabetes: A Cross-Sectional Study" Healthcare 8, no. 2: 105. https://doi.org/10.3390/healthcare8020105
APA StyleHonda, H., Igaki, M., Tanaka, S.-i., Ono, K., & Hirota, Y. (2020). Impact of Self-Reported Sitting Time and Transtheoretical Model Based on Exercise Behavior Change on Glycemic and Weight Control in Japanese Adults with Type 1 Diabetes: A Cross-Sectional Study. Healthcare, 8(2), 105. https://doi.org/10.3390/healthcare8020105





